Beruflich Dokumente
Kultur Dokumente
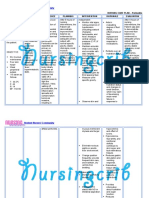
Nursing Care Plan: Epidural Hematoma Post Craniotomy
Hochgeladen von
TepperoniCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Care Plan: Epidural Hematoma Post Craniotomy
Hochgeladen von
TepperoniCopyright:
Verfügbare Formate
NURSING CARE PLAN Patients Name/Bed #: Mr.
A SICU0 Medical Diagnosis: epidural hematoma, right FTP area, S/P craniotomy, evacuation of subdural hematoma, right FTP (0/0/0); S/P repeat craniotomy, evacuation of epidural and subdural hematoma, JP drain (0/0/0) Subjective/Objective cues: Subjective cues: None-with ET tube attached to mechanical ventilator Objective cues: With pupillary size of 4 mm on right eye, 2 mm on left eye, both eyes with negative reaction to light Muscle grade of 1/5 for slight muscle contraction on all extremities, no joint motion. With GCS of 6 (best eye opening-opens to pain; verbal response-1 with ET attached to VR; motor response-3, flexes arms and extension of legs Nursing Diagnosis with Etiology Ineffective Cerebral Tissue Perfusion related to the interruption of the blood flow to the brain. Goals of Care Interventions General/Specific General: Independent: Within 2 weeks of medical Assessment and nursing interventions, Assess mental client will be able to status and improve level of changes in the consciousness. level of consciousness Specific: Within 1 day of medical and nursing interventions, client will be able to Therapeutic manifest: Position client in Improve/Stable low-fowlers level of position (30 consciousness degrees) Improve/Stable GCS score Avoid extreme No pupillary rotation of the changes, seizures, neck widening of pulse pressure, irregular respirations, hypotension and bradycardia. Avoid extreme hip flexion Rationale Evaluation
To check for affected cranial nerve functions in the brain (for GCS); check for cerebral hypoperfusion and hypoxia. Help venous drainage from the brain and promote brain expansion. This will compress the jugular veins leading to an increased intracranial pressure. Increase in intraabdominal and intra-thoracic pressure leading to increased intracranial
GCS of 5 (best eye opening-1, none; verbal response-1 with ET attached to VR; motor response-3, flexes arms and extension of legs to pain)
Patient is placed in lowFowlers position; made comfortable in bed and adjusted pillows Patient is monitored frequently; positioned head and neck cautiously and placed a pillow on side for support Patient is repositioned cautiously and provided with pillows for support
to pain) Babinski reflexpositive, and oculocephalic reflex-negative
pressure. Maintain airway patent Prevents build up of secretions leading to increase in carbon dioxide and intracranial pressure. ET tube placement is monitored if securely attached to patient at the appropriate level of 21 cm; suctioned frequently for secretions
Dependent: Administer medications such as diuretics (e.g. Mannitol) and anticonvulsants (e.g. Amlodipine, Verapamil) Diuretics are used and needed to decrease cerebral edema and anticonvulsant medications Mannitol 75 cc was given intravenously to patient; antihypertensives such Amlodipine 20 mg per tablet and Verapamil 10 mg per tablet was also given to patient
Collaborative: Review oximetry pulse saturation Hypoxia is Oxygen associated with patient ranges 98-99% reduced cerebral tissue perfusion. It maximizes cardiac output and prevents decreased cerebral perfusion associated with hypovolemia. With IV fluid of PNSS 1L x 63 cc per hour, patent and infusing well at left metacarpal vein of patient, with a rate of 21 drops per minute
Restore maintain balance
or fluid
Patients Name/Bed #: Mr. A SICU0 Medical Diagnosis: epidural hematoma, right FTP area, S/P craniotomy, evacuation of subdural hematoma, right FTP (0/0/0); S/P repeat craniotomy, evacuation of epidural and subdural hematoma, JP drain (0/0/0) Subjective/Objective cues: Subjective cues: None- with ET tube attached on mechanical ventilator Objective cues: Adventitious breath sounds heard at left anterior lung such as ronchi and wheezing Presence of whitish, tenacious secretions approximately 20 cc Decreased level of consciousness (GCS of 6: best eye openingopens to pain; verbal response1 with ET attached to VR; motor response3, flexes arms and extension of legs to pain) Nursing Diagnosis with Etiology Ineffective airway clearance maybe related to hypoventilation secondary to brain stem injury Goals of Care Interventions General/Specific General Independent Within 1 week of medical Assessment and nursing intervention, Assess client will be able to respiration and mobilize secretions. breath sounds, noting rate and Specific sounds (e.g. Within 1 day of medical tachypnea, and nursing stridor, crackles, interventions, client will wheezes) be able to manifest: Clear breath Evaluate sounds cough/gag reflex Decreased and swallowing secretions ability Assess airway for patency Rationale Evaluation
Respirations range between 16-21 breaths per minute, regular in rate and rhythm; adventitious breath sounds heard over left anterior lung, including ronchi and wheezing sounds exhibits To determine Patient swallowing and gag ability to protect reflexes; with absent own airway cough reflex These signs and symptoms are indicative of respiratory distress and/or accumulation of secretions. Placement of ET tube on patient is monitored frequently at the appropriate level of 21 cm; suctioned frequently for presence of secretions. Lethargy and Patient is GCS 5 (no eye somnolence are opening-1, with ET tube attached-1, and flexes late signs arms and extends legs to painful stimuli-3) Maintaining the airway is always first priority, especially in cases of trauma.
Assess changes in mental status
Note presence of sputum, assess quality, color, amount, odor and consistency.
Therapeutic Elevate head of bed and reposition every 2 hours and as needed.
Abnormalities maybe a result of infection. A sign of infection is discolored sputum. To take advantage of gravity decreasing pressure on the diaphragm and enhancing drainage of/ventilation to different lung segments. This prevents abdominal contents from pushing upward and inhibiting lung expansion. This loosens secretions and facilitates the removal.
with whitish, tenacious secretions noted upon suctioning of the mouth and ET tube, approximately 20 cc Patient was repositioned every two hours, made comfortable in bed while adjusting pillows; provided with chest physiotherapy upon change of position
Routinely check the patients position so he does not slide down in bed.
Patient is monitored frequently; with slight elevation of the foot part to prevent sliding down the bed.
Use humidifier.
Patients VR set-up cmes with a humidifier; monitored frequently from getting used up
Institute suctioning of the airway.
is suctioned Helps clear Patient frequently for presence secretions. of secretions
Dependent Administer medications (e.g. antibioticsLevofloxacin, Vigocid; mucolytic agents, bronchodilatorsSalbutamol) as ordered, noting effectiveness and side effects. Collaborative Check and monitor VR setup and patients response.
These promote clearance of airway secretions and bronchodilation decreases airway resistance.
Patient was given ILN Salbutamol 1 nebule via face mask; with respiratory rate of 17-21 breaths per minute, regular, non-labored; with no side effects such as hypotension or bradycardia.
The basis for setting every parameter of the ventilator depends on the patient. Maintaining the correct settings for every parameter ensures the proper ventilation to the patient.
With ET tube at 21 cm attached to patient connected to a functional ventilator; with VR set-up of: tidal volume-450 ml, peak flow-50, back up rate-16 breaths per minute, FIO2-30%, and assist-control mode; weaned to T-piece at 40% and 8 liters of oxygen
Patients Name/Bed #: Mr. A SICU0 Medical Diagnosis: epidural hematoma, right FTP area, S/P craniotomy, evacuation of subdural hematoma, right FTP (0/0/0); S/P repeat craniotomy, evacuation of epidural and subdural hematoma, JP drain (0/0/0) Subjective/Objective cues: Objective cues: GCS 5 best motor response is in decorticate position graded as 3 Unable to perform active range of motion exercises on all extremities Grade 1/5 in the muscle grading scale (slight muscle contraction on all extremities, no joint motion) Hand grasp of 0/3-none on both hands Nursing Diagnosis with Etiology Impaired physical mobility related to limitation in independent purposeful physical movement of the body secondary to motor never compression on frontal lobe Goals of Care Interventions General/Specific General: Independent: Within 2 weeks of Assessment: medical and nursing Assess for interventions, client will developing be able to maintain or thrombophlebitis increase strength of the (calf pain, body and extremities. Homans sign, redness, Specific: localized Within 1 week of medical swelling, and and nursing hyperthermia) interventions, client will be able to: Assess skin Improve muscle integrity strength on all extremities Perform passive exercises on all extremities Rationale Evaluation
Bed rest immobility promotes formation
or Patient displays no signs of calf pain, redness and on lower clot swelling extremities, or hyperthermia.
Regular examination of the skin especially on bony prominences will allow for prevention or early recognition and treatment of pressure sores.
Skin is dry, wrinkled, and rebounds instantly; with no signs of pressure sores or redness over bony prominences.
Therapeutic Keep side rails up and bed in low position
This promotes a Patient is frequently secured safe environment monitored; raised side rails at all times; placed in low or semi-Fowlers position
Turn patient every two hours
Turning position optimizes circulation to all tissues and relieves pressure.
Patient is repositioned every 2 hours, massaged bony prominences, and placed pillows or rolled cloth for limbs and body support. Patient was provided with pillows and properly rolled cloth to maintain alignment and support on all limbs. Passive range of motion exercises was provided to patient on all extremities with proper support and execution.
Maintain limbs in functional alignment
Maintaining proper alignment pf extremities prevents contractures. Exercise promotes increased venous return, prevents stiffness, and maintains muscle strength. This prevents tissue breakdown
Perform passive ROM exercises on all extremities
Use pressurerelieving devices as indicated
Placement of pillows or rolled cloth to prevent pressure of skin contact to surface; gentle massage on bony prominences was provided
Dependent: Administer medications as ordered such as antispasmodic drugs (e.g. Vitamin B complex)
Vitamin B complex Antispasmodic (Polynerv) 500 mg was medications may reduce muscle given to patient spasms that interfere with mobility.
Collaborative: Set-up a bowel program (e.g. adequate fluid, foods high in bulk, physical activity, stool softeners, laxatives) as needed. Record bowel activity level.
Prolonged bed rest, lack of exercise, and physical inactivity contribute to constipation. A variety of interventions will promote normal eliminations.
IV fluid of PNSS 1L x 63 cc per hour, patent and infusing well at left metacarpal vein of patient, adjusted at a rate of 21 drops per minute; nutrition given through osteorized tube feeding of 1, 800 kcal in 6 equal feedings plus 6 egg whites; patient was also ordered with Lactulose 30 cc; no bowel movement noted since last week
Patients Name/Bed #: Mr. A SICU0 Medical Diagnosis: epidural hematoma, right FTP area, S/P craniotomy, evacuation of subdural hematoma, right FTP (0/0/0); S/P repeat craniotomy, evacuation of epidural and subdural hematoma, JP drain (0/0/0) Subjective/Objective cues: Objective cues: presence of surgical wound stitched across the right part of the head about 12 inches, vertical; with dry, intact 2 x 3 inches dressing Nursing Diagnosis with Etiology Risk for infection related to tissue destruction susceptible for invasion of pathogens. Goals of Care Interventions General/Specific General: Independent: Within 2 weeks of Assessment: medical and nursing Observe for interventions, client will localized signs of be able to infection at prevent/reduce risk for surgical incision infection. wound. Note signs and Specific: symptoms of Within 1 week of medical sepsis; fever, Rationale Evaluation
To check for any Signs of infection were signs of infection not noted; no visible signs of redness or pus around surgical site. To check for the With normal temperature presence of ranges from 35.6 C to infection and give 37. 1 C taken at left
on right parietal part of head increased WBC (laboratory result of 14. 6 meq/L on January 7, 2013 ) Presence of an indwelling catheter and endotracheal tube
and nursing chills, interventions, client will diaphoresis. be able to manifest: Therapeutic: Absence of Change serosanguinous surgical/wound drainage from the dressings, as surgical site. indicated, using aseptic technique for changing/ Decrease or disposing of normal WBC contaminated value. materials. Health Teachings: Teach family how to clean incision site daily and remind them to change dressings as needed. Dependent: Administer or monitor medication regimen (e.g. antibiioticsLevofloxacin 750 mg, Vigocid 2.25 gm) and note patients response. Collaborative: Note and report laboratory values
necessary interventions. To facilitate wound healing and prevent infection by minimizing growth and spread of microorganisms.
axilla; chills and diaphoresis not noted Staff nurse on duty performed changing of surgical dressing, as indicated.
To educate the family about the right procedure to clean and change dressings.
Significant other was instructed to follow correct hand washing and aseptic technique whenever in contact with a surgical wound.
To determine Medications as directed effectiveness of follows the treatment duration for a certain therapy. number of days; completed the treatment regimen; temperature is within normal level of 35.6 C 37 C;
To provide a Latest lab values for global view of the WBC was not checked patients immune by student nurses function and nutritional status.
Subjective/Objective cues: Objective cues: Unable to pass stool since last week; with diet of osteorized tube feeding of 1, 800 kcal in 6 equal feeding plus 6 egg whites Inactivity, GCS 5 best motor response is in decorticate position graded as 3 muscle grade of 1/5 (muscle contraction on all extremities but no joint motion
Nursing Diagnosis with Etiology Constipation related to inhibited defecation reflex secondary to compression of the pudendal nerve on the medial prefrontal lobe of the brain
Goals of Care General/Specific General: Within 3 weeks of medical and nursing interventions, client will be able to pass out soft, formed stool Specific: Within 1 day of medical and nursing interventions, client will be able to: maintain normal bowel sounds within the range of 5-32 gurgling or clicking sounds perform passive ROM exercises on all extremities
Interventions Independent Assessment assess usual pattern of elimination; compare with present pattern, include size, frequency, color, and quality
Rationale
Evaluation
evaluate laxative use, type, and frequency
assess level
activity
evaluate current medication usage that may contribute to
normal frequency of passing stool varies from twice daily to once every third or fourth day. It is important to ascertain what is normal for each individual chronic use of laxatives causes the muscles and nerves of the colon to function inadequately in producing an urge to defecate. Over time, the colon becomes atonic and distended. Prolonged bed rest, lack of exercise, and inactivity causes constipation Drugs that can cause constipation include the
constipation
following: narcotics, antacids, antidepressants, anticholinergics, antihypertensive, general anesthetics, hypnotics, and iron and calcium supplements Patients, especially older patients, may have cardiovascular limitations that require that less fluid be taken Ambulation and/or abdominal exercises strengthen abdominal muscles that facilitates defecation These steps lead to reestablishing regular bowel habits Twenty grams of fiber per day is
Therapeutic provide fluid intake of 2000 to 3000 mL/day, if not contraindicated medically
provide passive ROM exercises on all extremities
Health Teachings reinforce to caregiver the importance of the following: a balanced diet consisting of
adequate fiber, fresh fruits, vegetables and grains adequate fluid intake (20003000 mL/day) regular exercise and activity
recommended
regular meals
Increased hydration promotes softer fecal mass Exercise strengthen abdominal muscles and stimulate peristalsis Successful bowel training relies on routine
Dependent administer drugs such as Lactulose, as ordered This laxative is characterized by a shorter colon transit time and accelerated bowel movement.
Collaborative Health teachings teach use of medications as ordered, as in the following: bulk fiber (Metamucil)
This fluid,
increase gaseous,
stool softeners (Colace) chemical irritants (castor oil, cascara, milk of magnesia)
suppositories
oil retention enema
and solid bulk of intestinal contents Softens stool and lubricates intestinal mucosa These irritate the bowel mucosa and cause rapid propulsion of contents and small intestine Softens stool and stimulates rectal mucosa Softens stool
Subjective/Objective cues: Objective cues:
Nursing Diagnosis with Etiology Risk for Aspiration related to decreased GCS of 6 (best level of consciousness eye opening- secondary to cerebral opens to pain; hypoperfusion verbal response1 with ET attached to VR; motor response3, flexes arms and extension of legs to pain)
Goals of Care General/Specific General: Within 1 week of medical and nursing intervention, patients risk will decrease as a result of ongoing assessment and early interventions Specific: Within 1 day of medical
Interventions
Rationale
Evaluation
Absent cough reflex Presence of endotracheal, and nasogastric tubes attached to patient
and nursing interventions, patient will be able to: Maintain a patent airway
Subjective/Objective cues: Objective cues: GCS of 6 (best eye openingopens to pain; verbal response1 with ET attached to VR; motor response3, flexes arms and extension of legs to pain) Grade 1/5 in the muscle grading scale (slight muscle contraction on all extremities, no joint motion) Hand grasp of 0/3-none on both hands
Nursing Diagnosis with Etiology Self-Care Deficit related to decreased level of consciousness secondary to cerebral hypoperfusion and compression of the motor nerve on the frontal lobe
Goals of Care General/Specific General: Within 3 weeks of medical and nursing interventions, patient will be able to safely perform (to maximum ability) selfcare activities Specific: Within 1 day of medical and nursing interventions, patient will be able to: Exhibit hygiene grooming good and
Interventions
Rationale
Evaluation
Das könnte Ihnen auch gefallen
- NCP For Subarachnoid HemorrhageDokument4 SeitenNCP For Subarachnoid HemorrhageJoan Rose Rendon-Hung78% (18)
- Craniotomy Nursing Care PlanDokument5 SeitenCraniotomy Nursing Care PlanNikko Dela Cruz94% (17)
- Nursing Care Plans - Ineffective Cerebral Tissue PerfusionDokument3 SeitenNursing Care Plans - Ineffective Cerebral Tissue PerfusionKate Cruz75% (8)
- 6 Pleural Effusion Nursing Care PlansDokument7 Seiten6 Pleural Effusion Nursing Care PlansjamieboyRN87% (62)
- Nursing Diagnoses For PT With Altered Level of ConsciousnessDokument5 SeitenNursing Diagnoses For PT With Altered Level of Consciousnessmikaela_pascua95% (40)
- Ineffective Cerebral Tissue PerfusionDokument3 SeitenIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- NCP - Head InjuryDokument3 SeitenNCP - Head Injurykaheliyala94% (33)
- Nursing Care Plan (Septick Shock)Dokument6 SeitenNursing Care Plan (Septick Shock)REMILYN ROSE ASUNCION67% (9)
- Nursing Care Plan Patient EndotrachealDokument2 SeitenNursing Care Plan Patient EndotrachealCyrus De Asis67% (6)
- Nursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"Dokument9 SeitenNursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"jhonroks100% (7)
- Npte Exam TablesDokument586 SeitenNpte Exam TablesarbazNoch keine Bewertungen
- Nursing Care PlanDokument9 SeitenNursing Care PlanJam AbantaoNoch keine Bewertungen
- Nursing Care Plan Hemorrhagic StrokeDokument8 SeitenNursing Care Plan Hemorrhagic StrokeJeffrey Dela Cruz50% (4)
- 00.00 Reference Care Plan Tonsillectomy and Adnoidectomy Post OpDokument5 Seiten00.00 Reference Care Plan Tonsillectomy and Adnoidectomy Post OpMarya KemmieNoch keine Bewertungen
- NCP RHDDokument7 SeitenNCP RHDHenry Roque Tagalag80% (5)
- NCP Head InjuryDokument3 SeitenNCP Head InjuryEdelou Alegria Jumawan67% (3)
- Nursing Care Plan GlaucomaDokument3 SeitenNursing Care Plan Glaucomasephirus77750% (4)
- Nursing Care Plan Tracheoesophageal Fistula and Esophagus AtresiaDokument1 SeiteNursing Care Plan Tracheoesophageal Fistula and Esophagus Atresiagannadortch88% (17)
- Nursing Care Plan - Pericarditis PatientDokument2 SeitenNursing Care Plan - Pericarditis Patientsandie_best78% (9)
- NCP TbiDokument4 SeitenNCP TbiWyen CabatbatNoch keine Bewertungen
- Nursing Care Plan: West Visayas State University College of NursingDokument4 SeitenNursing Care Plan: West Visayas State University College of NursingLizaEllaga100% (1)
- Nursing Care PlanDokument4 SeitenNursing Care PlanJoy Callo100% (2)
- Myocarditis NCP 2Dokument8 SeitenMyocarditis NCP 2astro_aaron117375% (4)
- Assessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationDokument10 SeitenAssessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationApol Pen67% (3)
- SCIQuestions CaseStudyKeyDokument4 SeitenSCIQuestions CaseStudyKeyDeez NutsNoch keine Bewertungen
- MACI Case Study 3 TURPDokument13 SeitenMACI Case Study 3 TURPTepperoni0% (1)
- Nursing Care PlanDokument3 SeitenNursing Care PlanBhie DizonNoch keine Bewertungen
- Nursing Care Plan For Acute Head InjuryDokument4 SeitenNursing Care Plan For Acute Head InjuryAngie Mandeoya67% (3)
- Nursing Care Plan Clubfoot or Talipes EquinovarusDokument2 SeitenNursing Care Plan Clubfoot or Talipes Equinovarusderic100% (4)
- 14 Cerebrovascular Accident Nursing Care PlansDokument5 Seiten14 Cerebrovascular Accident Nursing Care PlansNickesha Mckenzie75% (4)
- Nursing Care Plan SeizureDokument2 SeitenNursing Care Plan Seizuretimie_reyes100% (1)
- Cva NCP AnxietyDokument1 SeiteCva NCP AnxietyQueenElsaDeVeraNoch keine Bewertungen
- Bronchopneumonia Care PlanDokument6 SeitenBronchopneumonia Care PlanAbhijit Soundade0% (1)
- Nursing Care Plan 1Dokument4 SeitenNursing Care Plan 1Johndelle Banlasan Hernan100% (1)
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDokument2 SeitenNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Nursing Care Plan For "Glaucoma"Dokument7 SeitenNursing Care Plan For "Glaucoma"jhonroks100% (7)
- NCP Knowledge DeficitDokument2 SeitenNCP Knowledge DeficitRose Ann100% (1)
- NCP - Tissue Perfusion (Cerebral)Dokument2 SeitenNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- Cardiovascular Assessment: Assessment Uses of CVS AssessmentDokument8 SeitenCardiovascular Assessment: Assessment Uses of CVS AssessmentKawaljit KaurNoch keine Bewertungen
- Cva NCPDokument2 SeitenCva NCPAkima Mulok0% (1)
- NCP For StrokeDokument4 SeitenNCP For StrokeJASON OGALESCONoch keine Bewertungen
- Nursing Care Plan For Peritonitis NCPDokument2 SeitenNursing Care Plan For Peritonitis NCPderic86% (7)
- Ineffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Hemorrhage As Evidenced by GCS of 7Dokument2 SeitenIneffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Hemorrhage As Evidenced by GCS of 7dana100% (4)
- Assessment Nursing Diagnosis Scientific Explanation Goal of Care Intervention Rationale EvaluationDokument4 SeitenAssessment Nursing Diagnosis Scientific Explanation Goal of Care Intervention Rationale EvaluationHowel CristobalNoch keine Bewertungen
- Disturbed Visual Sensory Perception Related: Nursing Care PlanDokument3 SeitenDisturbed Visual Sensory Perception Related: Nursing Care PlanMae Therese B. MAGNONoch keine Bewertungen
- Nursing Care PlanDokument13 SeitenNursing Care PlanCris Solis33% (3)
- Nursing Care Plan For GlaucomaDokument2 SeitenNursing Care Plan For GlaucomaEmiey Rara100% (1)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDokument3 SeitenAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimNoch keine Bewertungen
- NCP PancreatitisDokument2 SeitenNCP PancreatitisJeanelle Generoso100% (1)
- NCP - Ineffective Cerebral Tissue Perfusion R/T Space Occupying Lesion (Neuroblastoma On Frontal Lobe)Dokument4 SeitenNCP - Ineffective Cerebral Tissue Perfusion R/T Space Occupying Lesion (Neuroblastoma On Frontal Lobe)Carl Elexer Cuyugan Ano100% (4)
- Aneurysm NCPDokument4 SeitenAneurysm NCPAnneUXD100% (1)
- Philosophy, Mission, Vision of Hospital, College and CommunityDokument15 SeitenPhilosophy, Mission, Vision of Hospital, College and Communitykrishnasree100% (9)
- Nursingcrib Com NURSING CARE PLAN SeizureDokument2 SeitenNursingcrib Com NURSING CARE PLAN SeizureOscar Villados Jr.100% (2)
- Head InjuryDokument5 SeitenHead InjuryJames Jayson Liberto100% (3)
- NCPDokument17 SeitenNCPShayne Jessemae AlmarioNoch keine Bewertungen
- NCP Epidural HemDokument32 SeitenNCP Epidural HemKatrina PonceNoch keine Bewertungen
- NCPDokument11 SeitenNCPzharienabNoch keine Bewertungen
- PT Protocol - Part3-IcuDokument12 SeitenPT Protocol - Part3-IcuBlake BoggenpoelNoch keine Bewertungen
- NCP and DrugsDokument13 SeitenNCP and DrugsApRil ANn ChUa BingcangNoch keine Bewertungen
- Promoting Adequate Gas ExchangeDokument5 SeitenPromoting Adequate Gas Exchangeali sarjunipadangNoch keine Bewertungen
- GB SyndromDokument5 SeitenGB Syndromavinash dhameriyaNoch keine Bewertungen
- Wells' Criteria For DVT - MDCalcDokument4 SeitenWells' Criteria For DVT - MDCalcTepperoniNoch keine Bewertungen
- CoursesDokument2 SeitenCoursesTepperoniNoch keine Bewertungen
- SodiumDokument5 SeitenSodiumTepperoniNoch keine Bewertungen
- Metered Dose InhalersDokument2 SeitenMetered Dose InhalersTepperoniNoch keine Bewertungen
- Drug Study - Belladonna and OpiumDokument2 SeitenDrug Study - Belladonna and OpiumTepperoniNoch keine Bewertungen
- Interventions For Psych People DraftDokument8 SeitenInterventions For Psych People DraftTepperoniNoch keine Bewertungen
- Step by Step Tips On How To Become A Good SpeakerDokument27 SeitenStep by Step Tips On How To Become A Good SpeakerTepperoni67% (3)
- Connective Tissue CellsDokument8 SeitenConnective Tissue Cellsاسماء زياد عبدالجبارNoch keine Bewertungen
- Let's Talk Game CardsDokument4 SeitenLet's Talk Game CardssycagurlNoch keine Bewertungen
- Table of Specification Mapeh 10Dokument4 SeitenTable of Specification Mapeh 10Melody Anne Dinoso EvangelistaNoch keine Bewertungen
- Binomial Distribution ExercisesDokument3 SeitenBinomial Distribution ExercisesAlp Eren AKYUZNoch keine Bewertungen
- Cuscuta AssignmentDokument12 SeitenCuscuta AssignmentAshfaq Hussain KharalNoch keine Bewertungen
- Halosil Hospitals Sell Sheet 060817Dokument2 SeitenHalosil Hospitals Sell Sheet 060817duna tarimaNoch keine Bewertungen
- Immune Dysregulation Among Students Exposed To Exam Stress and Its Mitigation by Mindfulness Training - Findings From An Exploratory Randomised TrialDokument11 SeitenImmune Dysregulation Among Students Exposed To Exam Stress and Its Mitigation by Mindfulness Training - Findings From An Exploratory Randomised TrialPatricia Elena ManaliliNoch keine Bewertungen
- Analice Mendel: Clinical Doctorate in Occupational Therapy GPA: 4.0Dokument1 SeiteAnalice Mendel: Clinical Doctorate in Occupational Therapy GPA: 4.0api-518311936Noch keine Bewertungen
- Jadwal Pir MalangDokument4 SeitenJadwal Pir MalangAbraham BayuNoch keine Bewertungen
- FRE - L3 Core Terminology - 2018Dokument28 SeitenFRE - L3 Core Terminology - 2018RahulNoch keine Bewertungen
- Assessments For The Newborn BabiesDokument11 SeitenAssessments For The Newborn BabiesBeatrice ChenNoch keine Bewertungen
- (EPEC) : Enteropathogenic E. ColiDokument1 Seite(EPEC) : Enteropathogenic E. ColiBig BearNoch keine Bewertungen
- Symbolism in The Masque of The Red DeathDokument8 SeitenSymbolism in The Masque of The Red DeathmihacryssNoch keine Bewertungen
- Revision 1 English Open LetterDokument9 SeitenRevision 1 English Open Letterapi-441660843Noch keine Bewertungen
- Lesson Plan NutritionDokument7 SeitenLesson Plan NutritionPraveenNoch keine Bewertungen
- Surgical Catalogue PDFDokument690 SeitenSurgical Catalogue PDFSazzadNoch keine Bewertungen
- NAVLE Study Strategies Zuku ReviewDokument60 SeitenNAVLE Study Strategies Zuku ReviewMohamed Omar90% (10)
- Cases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseDokument3 SeitenCases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseIrma Suriani DarwisNoch keine Bewertungen
- DEV2011 2018 Practical Week 8 DRAFT REPORT PDFDokument1 SeiteDEV2011 2018 Practical Week 8 DRAFT REPORT PDFAreesha FatimaNoch keine Bewertungen
- HRCA GK Quiz Syllabus Class 7-8Dokument19 SeitenHRCA GK Quiz Syllabus Class 7-8Sualiha MalikNoch keine Bewertungen
- Pathophysiology: United StatesDokument11 SeitenPathophysiology: United StatesNurullia RahmawatiNoch keine Bewertungen
- Neuro-Ophthalmology: DR Jusuf Wijaya, SPM FK - Uki CawangDokument65 SeitenNeuro-Ophthalmology: DR Jusuf Wijaya, SPM FK - Uki CawanggeorgyNoch keine Bewertungen
- ToradolDokument2 SeitenToradolAdrianne Bazo100% (1)
- Urinary Retention PostpartumDokument5 SeitenUrinary Retention PostpartumpaswordnyalupaNoch keine Bewertungen
- Diadynamic CurrentDokument30 SeitenDiadynamic Currentpartizan_bl100% (2)
- Protein C Corgenix UKDokument32 SeitenProtein C Corgenix UKvijayaNoch keine Bewertungen
- Situation Analysis of Children in Timor-LesteDokument194 SeitenSituation Analysis of Children in Timor-LesteBunga P.Noch keine Bewertungen
- A To Z Orthodontics - Vol 9 - Preventive and Interceptive OrthodonticsDokument37 SeitenA To Z Orthodontics - Vol 9 - Preventive and Interceptive OrthodonticsĐạt HuỳnhNoch keine Bewertungen
- Refractory MigraineDokument495 SeitenRefractory MigraineSuresh Srinivas100% (1)