Beruflich Dokumente
Kultur Dokumente
Heterogeneity Project
Hochgeladen von
api-174496267Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Heterogeneity Project
Hochgeladen von
api-174496267Copyright:
Verfügbare Formate
1
Amanuel Negussie DOS 423 Heterogeneity Project March 2013 Heterogeneity Correction in Non-Small Cell Lung Cancer Treatment Objective: The objective of this project is to conduct a lung treatment plan with and without heterogeneity correction and evaluate the difference. Purpose: Human anatomy is made of different tissues that have their own unique physical and radiological property. Interaction of tissues with radiation can result in complete absorption, partial absorption, scatter, and transmission. The attenuation of a photon beam in a tissue varies depending on the energy of the photon, the density of the tissue, and the effective atomic number of the tissue.1 In radiation therapy, it is essential to know and understand these factors as they affect the accuracy of the dose delivered to the target. Tissues including lung, oral cavities, teeth, nasal passages, soft tissues, and bones have different radiation absorption factor that can disrupt the amount of dose planned to reach the target. Traditionally, lung tumors were treated assuming the density of all tissues being equivalent to water. Previous radiation oncology task group (RTOG) protocols also supported this technique. This was established due to the limitation of treatment planning systems (TPS); the lack of evidences that supports the need for density correction; and to avoid calculation errors and underdosing of tumors when accounting heterogeneity corrections.2 However, due to the advancement of TPS, the application of heterogeneity correction in dose calculations became more practical. Currently, both RTOGs and American Association of Physics in Medicine (AAPMs) protocols recommend using heterogeneity correction for treatment planning and dose prescriptions.1,3 Since lung is surrounded by ribs, soft tissues, and air cavities, it can greatly be affected by heterogeneity correction. The effect of tissue inhomogeneity is mainly due to the change in absorption of primary or scattered photon beams and the change in secondary electron fluence.4 Consequently, it is difficult to assume accurate dose calculation of lung treatment plans without accounting tissue density variations. Undermining tissue inhomogeneity will create dose buildup at the distal interfaces and dose builddown at the proximal interface of the lung.5 Some studies have shown that heterogeneity corrections in lung treatment plans will increase the dose to
isocenter by 6-18% more than those calculated without correction.6 The dose reaching the target is also lower for high energy photon beams planned without heterogeneity correction.6 In addition, when corrections are applied, the dose to target will be less than prescribed. Therefore, it is necessary to increase the prescribed dose when using heterogeneity corrections in order to maintain the same dose within the planned target volume (PTV).2 Methods and Materials: RL is a 62-year-old man who presented with a stage III-A non-small cell lung cancer (NSCLC) was simulated in a supine position on a wingbord. A Philips large bore 16 slice computed tomography (CT) machine was used for the simulation, and a Pinnacle3 9.0 treatment planning system (TPS) was used to plan the treatment. The treatment was prescribed to 5040 centigray (cGy) at 180cGy per fraction to the 96% isodose line. Gross tumor volume (GTV), PTV, right lung, left lung, heart, and spinal cord were contoured. A two field anterior/posterior (AP) and posterior/anterior (PA) beam arrangement was used. The collimator and table angle were set at 0o for both fields. A 1.5 centimeter (cm) margin around the PTV was used to shape the treatment field with multileaf collimators (MLC). An enhanced dynamic wedge of 15o was used on the AP field to account for the curvature of the thorax and maintain dose uniformity across PTV. A mixed energy of 6 megavolt (MV) and 18 MV was used on both AP and PA fields for a better dose coverage with minimal maximum dose. Although the use of higher energy photon beams in lung treatment planning is controversial, RTOG 617 protocol recommends 6-18 MV energy for NSCLC. A beam weighting of 20% for the 6MV AP field, 12% for the 18 MV AP field, 53% for the 6MV PA field, and 15% for the 18 MV PA field was applied. The primary trial was planned without heterogeneity correction. It was completed with a total monitor unit (MU) of 280, a maximum dose of 5692cGy, and a hot spot of 12% located posteriorly. The dose to each organ at risk (OR) was below the RTOG recommended tolerance limit. The plan met all the guidelines and requirements of RTOG 617 protocol. A first trial was copied and recalculated using heterogeneity correction without any additional change to the plan. The second trial was completed with a total MU of 261, a maximum dose of 6300cGy, and a hot spot of 25% located posteriorly. Results: Figure 1 a, b, and c demonstrate the sagittal, axial, and coronal view of the AP/PA lung plan dose distribution, dose volume histogram (DVH), and MuCheck calculation sheet for the trial calculated without heterogeneity correction. Figure 2 a, b, and c demonstrate the sagittal, axial, and coronal view of the AP/PA lung plan dose distribution, DVH, and MuCheck
calculation sheet for the trial calculated with heterogeneity correction. Figure 3a demonstrates the DVH comparison of the two trials. Figure 1a: The sagittal, axial, and coronal view of dose distribution to the plan without heterogeneity correction
Figure 1b: DVH of the plan without heterogeneity correction
Figure 1c: MU dose calculation for the plan without heterogeneity
Figure 2a: The sagittal, axial, and coronal view of dose distribution to the plan with heterogeneity correction
Figure 2b: DVH of the plan with heterogeneity correction
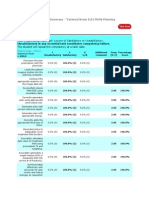
Figure 2c: MU dose calculation for the plan with heterogeneity correction
Figure 3a: DVH comparison of the plans with and without heterogeneity correction. The solid lines represent the plan with heterogeneity correction, and the dashed lines represent the plan without heterogeneity correction.
10
Discussion: The two trials have evident differences in their MU, PTV coverage, and maximum dose. When calculated with heterogeneity correction, the second trials maximum dose increased by 648cGy. Although the location remained the same, the hotspot increased by 13%. On the other hand, the MU of the AP field with the homogeneity plan increased by 15% for the 6MV and 10% for the 18 MV photon beam. The MU calculation demonstrated a -5.5% difference for the 6MV and 6.32% difference for the 18 MV AP fields (Figure 1c and 2c). This is over my clinical sites tolerance limit, which is +/- 3% difference. In addition, the PTV coverage by the 100% isodose line appeared more adequate in the plan calculated without heterogeneity correction (Figure 1a and 1c). Whereas, dose uniformity in the lung appeared worse when the distributions were corrected for inhomogeneity (Figure 2a and 2c). The dose to OR were also lower in the plan with heterogeneity correction than without (Figure 3a).This is due to the differences in absorption and scatter of the photon beam as it passes through different tissues. Since the target is located at the posterior edge of the lung, the AP beam has to penetrate more tissues than the PA beam. When heterogeneity correction is applied, the MU increased for the AP fields so that the same desired dose can be delivered to the target. Heterogeneity correction increases with lower energy beams.1 This was demonstrated in the two trials as the MU increased by 20% for the 6MV and 13% for the 18 MV AP field (Figure 1c and 2c). Lower energy beams cannot travel far into tissues compared to high-energy beams. Accordingly, the AP 6MV beam will lose more energy than the 18MV beam as it passes through tissues to reach the target. As a result, when calculated with heterogeneity correction, the change in MU for the 6MV will be higher than the 18 MV. Conclusion: Dose determination using heterogeneity correction is an essential component of dose optimization which allows us develop a reliable treatment plan. The two plans calculated with and without heterogeneity correction demonstrated that different density tissues that lie in the path of a photon beam affect dose distribution to target volumes. Heterogeneity correction simply accounts the density differences between air spaces, lung tissues, bone minerals, and soft tissues. Generally, tissue heterogeneity in a lung depends on the lung density, the lung length traversed, beam energy, and beam field size. When a correction is applied, the dose distribution will be distorted due to tissue inhomogeneity. This will not just affect the dose to the PTV but also to OR.
11
References 1. AAPM Report No. 85. Tissue Inhomogeneity Corrections for Megavoltage Photon Beams. College Park, MD. 2004. 2. Frank SJ, Forster KM, Stevens CW, et al. Treatment planning for lung cancer: traditional heterogeneous point-dose prescription compared with heterogeneity-corrected dosevolume prescription. Int J Radiation Oncology Biol Phys.2003; 56(5): 1308-1318. 3. RTOG 0617. A Randomized Phase III Comparison of Standard dose (60Gy) Versus Highdose (74 Gy) Conformal Radiotherapy with Concurrent and Consolidation Carboplatin/Paclitaxel +/- Cetuximab (IND #103444) in Patients with Stage IIIA/IIIB Non-Small Cell Lung Cancer. 2012. 4. Khan F. The Physics of Radiation Therapy. 4th ed. Baltimore, MD: Lippincott, Williams, and Wilkins; 2010: 220-229. 5. Bentel GC. Radiation Therapy Planning. 2nd ed. New York, NY: McGraw-Hill; 1996:100-101. 6. Orton CG, Chungbin S, Klein E, et al. Study of lung density corrections in a clinical trial (RTOG 88-08). Int J Radiation Oncology Biol Phys.1998; 41(4): 787-794.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- VC AndrewsDokument3 SeitenVC AndrewsLesa O'Leary100% (1)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- T688 Series Instructions ManualDokument14 SeitenT688 Series Instructions ManualKittiwat WongsuwanNoch keine Bewertungen
- BA 4722 Marketing Strategy SyllabusDokument6 SeitenBA 4722 Marketing Strategy SyllabusSri GunawanNoch keine Bewertungen
- Roland Fantom s88Dokument51 SeitenRoland Fantom s88harryoliff2672100% (1)
- Nature of Science-Worksheet - The Amoeba Sisters HWDokument2 SeitenNature of Science-Worksheet - The Amoeba Sisters HWTiara Daniel25% (4)
- Chapter 24 - The Solar SystemDokument36 SeitenChapter 24 - The Solar SystemHeather Blackwell100% (1)
- Amanuel Negussie: Certificate of AttendanceDokument1 SeiteAmanuel Negussie: Certificate of Attendanceapi-174496267Noch keine Bewertungen
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDokument1 SeiteV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267Noch keine Bewertungen
- ImrtDokument3 SeitenImrtapi-174496267Noch keine Bewertungen
- For E-PortfolioDokument14 SeitenFor E-Portfolioapi-174496267Noch keine Bewertungen
- ElectronDokument2 SeitenElectronapi-174496267Noch keine Bewertungen
- Conference LogsDokument1 SeiteConference Logsapi-174496267Noch keine Bewertungen
- WK VII WikiDokument6 SeitenWK VII Wikiapi-174496267Noch keine Bewertungen
- WK II WikiDokument4 SeitenWK II Wikiapi-174496267Noch keine Bewertungen
- WK VI WikiDokument4 SeitenWK VI Wikiapi-174496267Noch keine Bewertungen
- Esophagus and ProstateDokument3 SeitenEsophagus and Prostateapi-174496267Noch keine Bewertungen
- Garments Costing Sheet of LADIES Skinny DenimsDokument1 SeiteGarments Costing Sheet of LADIES Skinny DenimsDebopriya SahaNoch keine Bewertungen
- Controlador DanfossDokument2 SeitenControlador Danfossfrank.marcondes2416Noch keine Bewertungen
- Nikasil e AlusilDokument5 SeitenNikasil e AlusilIo AncoraioNoch keine Bewertungen
- Model Answer Winter 2015Dokument38 SeitenModel Answer Winter 2015Vivek MalwadeNoch keine Bewertungen
- Chunking Chunking Chunking: Stator Service IssuesDokument1 SeiteChunking Chunking Chunking: Stator Service IssuesGina Vanessa Quintero CruzNoch keine Bewertungen
- MSC ACFN2 RD4 ClassDokument25 SeitenMSC ACFN2 RD4 Classmengistu jiloNoch keine Bewertungen
- 2001 Ford F150 ManualDokument296 Seiten2001 Ford F150 Manualerjenkins1100% (2)
- What Is Denim? Why It's Called Denim?: Properties of Denim FabricDokument21 SeitenWhat Is Denim? Why It's Called Denim?: Properties of Denim Fabricrahmanshanto623100% (1)
- Modified Airdrop System Poster - CompressedDokument1 SeiteModified Airdrop System Poster - CompressedThiam HokNoch keine Bewertungen
- Individual Daily Log and Accomplishment Report: Date and Actual Time Logs Actual AccomplishmentsDokument3 SeitenIndividual Daily Log and Accomplishment Report: Date and Actual Time Logs Actual AccomplishmentsMarian SalazarNoch keine Bewertungen
- Watch One Piece English SubDub Online Free On Zoro - ToDokument1 SeiteWatch One Piece English SubDub Online Free On Zoro - ToSadeusuNoch keine Bewertungen
- Example of Flight PMDG MD 11 PDFDokument2 SeitenExample of Flight PMDG MD 11 PDFVivekNoch keine Bewertungen
- LSL Education Center Final Exam 30 Minutes Full Name - Phone NumberDokument2 SeitenLSL Education Center Final Exam 30 Minutes Full Name - Phone NumberDilzoda Boytumanova.Noch keine Bewertungen
- Operational Readiness and Airport TransferDokument2 SeitenOperational Readiness and Airport TransferochweriNoch keine Bewertungen
- Afzal ResumeDokument4 SeitenAfzal ResumeASHIQ HUSSAINNoch keine Bewertungen
- How To Be A Better StudentDokument2 SeitenHow To Be A Better Studentct fatima100% (1)
- EDB Postgres Failover Manager Guide v2.1Dokument86 SeitenEDB Postgres Failover Manager Guide v2.1Anggia MauritianaNoch keine Bewertungen
- Durability of Prestressed Concrete StructuresDokument12 SeitenDurability of Prestressed Concrete StructuresMadura JobsNoch keine Bewertungen
- ASHRAE Elearning Course List - Order FormDokument4 SeitenASHRAE Elearning Course List - Order Formsaquib715Noch keine Bewertungen
- Compact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightDokument2 SeitenCompact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightStanley Ochieng' OumaNoch keine Bewertungen
- DevOps Reference CardDokument2 SeitenDevOps Reference CardIntizarchauhanNoch keine Bewertungen
- Coco Mavdi Esl5Dokument6 SeitenCoco Mavdi Esl5gaurav222980Noch keine Bewertungen
- MQXUSBDEVAPIDokument32 SeitenMQXUSBDEVAPIwonderxNoch keine Bewertungen
- Micro - Systemic Bacteriology Questions PDFDokument79 SeitenMicro - Systemic Bacteriology Questions PDFShashipriya AgressNoch keine Bewertungen