Beruflich Dokumente
Kultur Dokumente
April Case Study Edited
Hochgeladen von
api-174496267Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
April Case Study Edited
Hochgeladen von
api-174496267Copyright:
Verfügbare Formate
1
Amanuel Negussie Clinical Practicum I April 22, 2013 Prostate bed Intensity Modulated Radiation Therapy (IMRT) History of Present Illness: DB is a 65-year-old male reported to have elevated prostate specific antigen (PSA) of 12.76 in February 2012. A needle biopsy showed acinar type prostatic adenocarcinoma with perineural invasion. The test presented no seminal vesicle extension, lymph node invasion, and vascular invasion. His Gleason score was 3+4=7. He was staged tumor (T) 3a lymph node (N) 0 metastasis (M) 0. As a result, DB underwent a radical retropubic prostactomy in July 2012. The surgery report indicates that the procedure was uncomplicated and that he tolerated the procedure well. The patient experienced postoperative ileus. However, he was able to tolerate a regular diet without nausea or emesis four days after surgery. His pain was well controlled with oral medications. His post operative (post op) PSA was detectable at 0.14. A few weeks later, he was diagnosed with bilateral inguinal and umbilical hernia. He was treated with bilateral mesh inguinal herniorrhaphies and primary suture repair of midline incisional hernias in October 2012. Past Medical History: DB has a past medical history of hypertension, depression, insomnia, anemia, and pseudophakia. He also had a surgery of the right eye for cataracts removal. The patient has no known allergies. Diagnostic Imaging Studies: DB had a bone scan of the whole body in May 2012 that showed some non-specific uptake in the bilateral acetabulum and ischium. He also had x-ray of the pelvis before and after his prostectomy procedure. Family History: DB has a 24 years old daughter and a 33 years old son. His father died of prostate cancer, and his mother died of breast cancer. Social History: DB is a veteran with a smoking history of 25 packs per year. He quit smoking in 1989. He is a social drinker and does not use drugs. Medication: DB takes Avastin, Citalopram, Hydrobromide, Docusate, Hydrochlorothiazide, Lisinopril, Multivitamin, Sildenafil Citrate, and Zolpide Tartrate. Recommendations: DB was recommended to receive external beam radiation therapy given his detectable PSA and adverse features on pathology. It was explained to him the difficulty of knowing if his disease is confined to the prostate bed, nodal, and distant metastasis. The acute
and long-term effects were briefly discussed. He was notified that during treatment patients typically experience fatigue and urinary symptoms including pain with urination, increased urination, and urgency with urination. There is a long-term risk of urethral stricture, as well as damage to bladder and possible bleeding. Patients may also experience erectile dysfunction, rectal bleeding, increases in bowel movement, and may develop diarrhea. In addition, there is a very small but possible chance of the treatment causing secondary cancer. The Plan (Prescription): After a discussion with the patient, reviewing the chart, and examining the diagnostic study, the radiation oncologist decided to proceed with intensity modulated radiation therapy (IMRT) treatment. The treatment was prescribed to 6660 centigray (cGy) at 180cGy per fraction to the 98% isodose line for 37 fractions. Patient setup/ Immobilization: DB was simulated in a supine position with a customized VacLok under his legs. His pants and belt were moved down away from the pelvic area. His hands were crossed on his chest. A pillow was placed under his head for comfort. A Philips large bore 16-slice computer tomography (CT) machine was used for the simulation. Pelvic images were taken at 0.3 centimeter (cm) slices. Tattoos were applied bilaterally and medially at the end of the simulation process. Anatomic Contouring: After the simulation was completed, the CT scan was imported in the Pinnacle3 9.0 radiation treatment planning system (TPS). The radiation oncologist contoured the prostate fossa and expanded it by 8 millimeter (mm) to make the planning target volume (PTV). He also contoured the penile bulb and the bladder. In addition, I contoured the femurs and rectum. The unspecified tissues were expanded from the external contour excluding the PTV. Beam Isocenter/Arrangement: Varian 21 IX 3501 linear accelerator (Linac) machine was used to treat the patient. During the simulation process, the radiation oncologist placed the isocenter in the tumor. An 8-field beam arrangement at gantry angles of 135o, 100o, 65o, 30o, 330o, 295o, 260o, and 225o was used. The collimator and couch angle were set at 0o for all fields. Treatment Planning: The maximum number of segments was set at 80 and a direct machine parameter optimization (DMPO) was selected. An objective of the PTV was set for a minimum dose volume histogram (min DVH) of 6660cGy and volume of 99%, maximum dose (max dose) of 6993cGy, and uniform dose of 6860cGy. The objective for right and left femurs was set at the maximum dose of 4800cGy. Two bladder max DVHs, three rectum max DVHs, and two penile
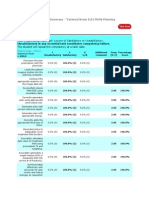
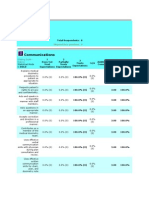
bulb max DVHs objectives were created. All the PTV objectives were weighed 5% and all the rest added objectives were weighed 1%. The plan was optimized. Due to the streaking effect of 50% isodose line around the skin surface, two rings were created. The first ring (ring 6660) was made by expanding the PTV by 2cm, and the second ring (ring 3330) was made by expanding the PTV by the 5cm (Figure 1). A 2mm space was left between the two rings and the PTV (Figure 1). In addition, a sphere shaped contour was loaded and adjusted around the posterior aspect of the rectum (Figure 2). The rings were assigned a max dose of 6660cGy for ring 6660, 3330cGy for ring 3330, and 3330cGy for the sphere. All rings were weighted 1%, and the plan was optimized. Multiple weighting arrangements were made on the PTV objectives to create higher dose coverage and minimize the maximum dose. The bladder, rectum, and penile bulb were slowly minimized by adjusting their max DVH. The posterior streaking effect of the 50% dose (3330cGy) was carefully analyzed, and the weighting on ring 3330 was adjusted to push the 50% dose away from the patients posterior external contour. The weight on ring 6660 was also adjusted to constrict the maximum dose within the PTV. The weight on the sphere was adjusted in order to push the 50% dose away from the posterior rectum wall. This is important as it helps minimize rectal toxicity.1 The plan was finalized with a total monitor unit (MU) of 625, maximum dose of 7086cGy, and hot spot of 6% located within the PTV. In addition, the 100% isodose line adequately covered the PTV and the dose to organs at risk (OR) met radiation therapy oncology group (RTOG) 534 protocol (Figure 3 and 4).2 The 50% isodose line did not include the posterior external contour and the posterior edge of the rectum (Figure 3). Each block was checked to ensure that a proper margin was used (Figure 5). After the final plan was carefully analyzed, the dose table created based on RTOG 534 protocol was filled out for the physician to review (Figure 6). Quality Assurance Checks: MU check was performed using the MuCheck 8.2.0. software. At our clinical site, a 5% deviation in MU is the tolerance for any IMRT plans. Anything outside this range needs to be recalculated and fixed by the dosimetrists or physicists prior to treatment. The plan was approved with an individual MU difference less than 5% except the beam angled at 3300(Figure 4 and 5). As a result, a different calculation point was picked for this angle. The MU
was rechecked and passed with less than 5% deviation. The total MU difference was 0.06% (Figure 7 and 8). A plan validation was also performed by ion chamber in solid water and ArcCheck diodes. The chamber plan percentage difference was 0.31% and the average percentage of ArcCheck diodes passed was 99.5%. The summery of the test was printed and double checked by the dosimetrist. The dosimetrist also wrote an IMRT note stating the prescription, the maximum dose, and the quality assurance tests. Conclusions: Through this case, I was able to work closely with my mentors. It was a challenging case that allowed me to learn more about IMRT. During the process, I learned the importance and utilization of rings in IMRT planning. It allowed me to analyze the effects they make on dose distribution and dose avoidance. In addition, I learned about the importance of minimizing dose to patients skin and how it can be achieved. I noted that allowing the 50% dose distribute towards the patient skin will likely enhance skin reaction. This is especially important in the posterior surface since backscatter from the table can increase the skin dose.
Figures
Figure 1: A sagittal, axial, and coronal view of ring6660 and ring 3330. Red represents ring 6660 and orange represents ring 3330
Figure 2: A sagittal, axial, and coral view of the sphere adjusted around the posterior edge of the rectum
Figure 3: Sagittal, axial, and coronal view of dose distribution
Figure 4: DVH of the treatment plan
Figure 5: A beams eye view (BEV) of the DRR
10
Figure 6: The dose table of the plan
11
Figure 7: MuCheck of the treatment plan
12
Figure 8: MuCheck of the treatment plan
13
Reference 1. Michalski JM, Gay H, Jackson A, et al. Radiation dose volume effects in radiation induced rectal injury. Int J Radiat Oncol Biol Phys. 76(3): 123-129. 2. Pollack A. RTOG 524. A Phase III Trial of Short Term Androgen Deprivation With Pelvic Lymph Node or Prostate Bed Only Radiotherapy (SPPORT) in Prostate Cancer Patients With a Rising PSA After Radical Prostatectomy. http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0534. Accessed April 22, 2013.
Das könnte Ihnen auch gefallen
- 021SAACK Burner Operating Instructions PDFDokument136 Seiten021SAACK Burner Operating Instructions PDFmekidmu tadesse100% (1)
- Required Reading For Piano Technicians PDFDokument28 SeitenRequired Reading For Piano Technicians PDFNinaNoch keine Bewertungen
- John PFTDokument231 SeitenJohn PFTAlexander Santiago ParelNoch keine Bewertungen
- May Case StudyDokument18 SeitenMay Case Studyapi-213055674Noch keine Bewertungen
- March Case StudyDokument7 SeitenMarch Case Studyapi-210258673Noch keine Bewertungen
- Research Proposal Group 10Dokument6 SeitenResearch Proposal Group 10api-483339757Noch keine Bewertungen
- Sethraheeljong Final PaperDokument13 SeitenSethraheeljong Final Paperapi-268623363Noch keine Bewertungen
- clinical oncology assignmentDokument9 Seitenclinical oncology assignmentapi-691277740Noch keine Bewertungen
- Final Case StudyDokument13 SeitenFinal Case Studyapi-334402872Noch keine Bewertungen
- Af Final Clincal ProjectDokument12 SeitenAf Final Clincal Projectapi-247864638Noch keine Bewertungen
- For E-PortfolioDokument14 SeitenFor E-Portfolioapi-174496267Noch keine Bewertungen
- En V79n2a07Dokument5 SeitenEn V79n2a07susanti bulanNoch keine Bewertungen
- Clinical Oncology AssignmentDokument8 SeitenClinical Oncology Assignmentapi-598481829Noch keine Bewertungen
- Capstone Paper Section V 2Dokument7 SeitenCapstone Paper Section V 2api-635186395Noch keine Bewertungen
- March Case StudyDokument13 SeitenMarch Case Studyapi-212894050Noch keine Bewertungen
- Adaptive Radiotherapy (ART) For A Prostate CaseDokument18 SeitenAdaptive Radiotherapy (ART) For A Prostate Caseapi-299189797Noch keine Bewertungen
- Clinical Assignment-Dos 531Dokument9 SeitenClinical Assignment-Dos 531api-633057533Noch keine Bewertungen
- Hybrid Planning Case Study Final DraftDokument20 SeitenHybrid Planning Case Study Final Draftapi-313040758Noch keine Bewertungen
- Final Draft 1Dokument14 SeitenFinal Draft 1api-502011468Noch keine Bewertungen
- June Case Study Final RevisedDokument18 SeitenJune Case Study Final Revisedapi-213108684Noch keine Bewertungen
- ClinoncDokument15 SeitenClinoncapi-631736561Noch keine Bewertungen
- Capstone Final Revisions 10-29-20-2Dokument14 SeitenCapstone Final Revisions 10-29-20-2api-483339757Noch keine Bewertungen
- Final Draft 2Dokument14 SeitenFinal Draft 2api-502011468Noch keine Bewertungen
- Clinical Oncology PaperDokument21 SeitenClinical Oncology Paperapi-632827798Noch keine Bewertungen
- Research Paper-Part 4Dokument15 SeitenResearch Paper-Part 4api-635954562Noch keine Bewertungen
- Capstone Paper Section IVDokument7 SeitenCapstone Paper Section IVapi-633434674Noch keine Bewertungen
- Group 1-Vijay Brittany Pat Seth Veronica Stephanie Sadie Ashley Draft 1Dokument15 SeitenGroup 1-Vijay Brittany Pat Seth Veronica Stephanie Sadie Ashley Draft 1api-334644774Noch keine Bewertungen
- Final DraftDokument15 SeitenFinal Draftapi-334402872Noch keine Bewertungen
- March Case Study Final RevisionDokument13 SeitenMarch Case Study Final Revisionapi-213108684Noch keine Bewertungen
- March Final CsDokument10 SeitenMarch Final Csapi-243468464Noch keine Bewertungen
- Clinical Oncology AssignmentDokument10 SeitenClinical Oncology Assignmentapi-635186395Noch keine Bewertungen
- Draft 1Dokument15 SeitenDraft 1api-334402872Noch keine Bewertungen
- Clinical Oncology PaperDokument14 SeitenClinical Oncology Paperapi-633087057Noch keine Bewertungen
- Dysphagia: Impact On Quality of Life After Radio (Chemo) Therapy of Head and Neck CancerDokument7 SeitenDysphagia: Impact On Quality of Life After Radio (Chemo) Therapy of Head and Neck CancerNurul Afika LubisNoch keine Bewertungen
- The Role of The Radiotherapy Technician During Prostate Radiation TreatmentDokument10 SeitenThe Role of The Radiotherapy Technician During Prostate Radiation TreatmentFlorian QordjaNoch keine Bewertungen
- Villegas2012 PDFDokument5 SeitenVillegas2012 PDFDiego Antonio Rodriguez CoronadoNoch keine Bewertungen
- Clinical Oncology AssignmentDokument10 SeitenClinical Oncology Assignmentapi-633434674Noch keine Bewertungen
- Intensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningDokument8 SeitenIntensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningAlberto GonzalesNoch keine Bewertungen
- Effectiveness of A Patient-Specific ImmobilizationDokument12 SeitenEffectiveness of A Patient-Specific ImmobilizationHollis LukNoch keine Bewertungen
- Clinical Oncology Assignment 1Dokument15 SeitenClinical Oncology Assignment 1api-576043594Noch keine Bewertungen
- Clinonc Assignment FinalDokument28 SeitenClinonc Assignment Finalapi-633652323Noch keine Bewertungen
- Estenosis AnalDokument5 SeitenEstenosis AnalluissparkNoch keine Bewertungen
- Research Paper-Part 2 1 1 - 1 1Dokument10 SeitenResearch Paper-Part 2 1 1 - 1 1api-635954562Noch keine Bewertungen
- Brachytherapy - Discussion 4Dokument3 SeitenBrachytherapy - Discussion 4api-633434674Noch keine Bewertungen
- Manuscript PDFDokument8 SeitenManuscript PDFapi-635186395Noch keine Bewertungen
- Clinical Oncology Assignment RaverDokument7 SeitenClinical Oncology Assignment Raverapi-635923017Noch keine Bewertungen
- Treatment Planning ProjectDokument12 SeitenTreatment Planning Projectapi-302696314Noch keine Bewertungen
- Research Paper FinalDokument15 SeitenResearch Paper Finalapi-635954562Noch keine Bewertungen
- Clinical Oncology PaperDokument16 SeitenClinical Oncology Paperapi-642376263Noch keine Bewertungen
- Dosimetric Comparison of AcurosBV With AAPMDokument19 SeitenDosimetric Comparison of AcurosBV With AAPMBruno MendesNoch keine Bewertungen
- Dose Evaluation For Skin and Organ in HepatocellulDokument11 SeitenDose Evaluation For Skin and Organ in HepatocellulAnne MbrkNoch keine Bewertungen
- Kevin FinalDokument20 SeitenKevin Finalapi-213055674Noch keine Bewertungen
- Clinical Oncology AssignmentDokument7 SeitenClinical Oncology Assignmentapi-632928455Noch keine Bewertungen
- Destiny J Rtog 0839 LunglabDokument5 SeitenDestiny J Rtog 0839 Lunglabapi-314709759Noch keine Bewertungen
- Pi Is 0360301611018256Dokument1 SeitePi Is 0360301611018256Olyndo IwanNoch keine Bewertungen
- (2022) - Effect of Manipulation Technique Using UltrasoundDokument8 Seiten(2022) - Effect of Manipulation Technique Using UltrasoundCristobal LopezNoch keine Bewertungen
- Bisa 1Dokument8 SeitenBisa 1justforuroNoch keine Bewertungen
- Research ProjectDokument16 SeitenResearch Projectapi-373572658Noch keine Bewertungen
- Modified Technique of Radical Inguinal Lymphadenectomy For Penile Carcinoma: Morbidity and OutcomeDokument7 SeitenModified Technique of Radical Inguinal Lymphadenectomy For Penile Carcinoma: Morbidity and OutcomeAlwin PrasetyaNoch keine Bewertungen
- Entrance Surface and Ovarian Doses in HysterosalpingographyDokument4 SeitenEntrance Surface and Ovarian Doses in HysterosalpingographyTryana HuangNoch keine Bewertungen
- Capstone Paper Section IIIDokument6 SeitenCapstone Paper Section IIIapi-633434674Noch keine Bewertungen
- A Case Study of DIBH To Spare Abdominal Organs at Risk For Renal Cell Carcinoma MR-Guided RadiotherapyDokument14 SeitenA Case Study of DIBH To Spare Abdominal Organs at Risk For Renal Cell Carcinoma MR-Guided Radiotherapyapi-525837437Noch keine Bewertungen
- Clinical Applications of Nuclear Medicine Targeted TherapyVon EverandClinical Applications of Nuclear Medicine Targeted TherapyEmilio BombardieriNoch keine Bewertungen
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDokument1 SeiteV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267Noch keine Bewertungen
- For E-PortfolioDokument14 SeitenFor E-Portfolioapi-174496267Noch keine Bewertungen
- Ec 102 Eclipseinverseplanningimrtandrapidarcv 13 CamanuelnegussieDokument1 SeiteEc 102 Eclipseinverseplanningimrtandrapidarcv 13 Camanuelnegussieapi-174496267Noch keine Bewertungen
- Amanuel Negussie: Certificate of AttendanceDokument1 SeiteAmanuel Negussie: Certificate of Attendanceapi-174496267Noch keine Bewertungen
- Monthly EvalDokument2 SeitenMonthly Evalapi-174496267Noch keine Bewertungen
- BrachytherapyDokument3 SeitenBrachytherapyapi-174496267Noch keine Bewertungen
- Joe RTDokument1 SeiteJoe RTapi-174496267Noch keine Bewertungen
- ResumeDokument2 SeitenResumeapi-174496267Noch keine Bewertungen
- Amanuel Final 5 1 14Dokument19 SeitenAmanuel Final 5 1 14api-174496267Noch keine Bewertungen
- Fall EvalsDokument6 SeitenFall Evalsapi-212894050Noch keine Bewertungen
- PhotonDokument3 SeitenPhotonapi-174496267Noch keine Bewertungen
- Case Log FallDokument2 SeitenCase Log Fallapi-174496267Noch keine Bewertungen
- ImrtDokument3 SeitenImrtapi-174496267Noch keine Bewertungen
- ElectronDokument2 SeitenElectronapi-174496267Noch keine Bewertungen
- Fall EvalsDokument6 SeitenFall Evalsapi-212894050Noch keine Bewertungen
- Fall EvalsDokument6 SeitenFall Evalsapi-212894050Noch keine Bewertungen
- Comprehensive Case Study - AnDokument31 SeitenComprehensive Case Study - Anapi-174496267Noch keine Bewertungen
- ConferenceDokument7 SeitenConferenceapi-174496267Noch keine Bewertungen
- October Case StudyDokument15 SeitenOctober Case Studyapi-174496267Noch keine Bewertungen
- Comprehensive Case Study Final - AdjustedDokument17 SeitenComprehensive Case Study Final - Adjustedapi-174496267Noch keine Bewertungen
- ComptotalsDokument3 SeitenComptotalsapi-174496267Noch keine Bewertungen
- Tally 1Dokument2 SeitenTally 1api-174496267Noch keine Bewertungen
- ConferencesDokument4 SeitenConferencesapi-174496267Noch keine Bewertungen
- September Case StudyDokument20 SeitenSeptember Case Studyapi-174496267Noch keine Bewertungen
- August Citation AssignmentDokument2 SeitenAugust Citation Assignmentapi-174496267Noch keine Bewertungen
- Conference LogsDokument1 SeiteConference Logsapi-174496267Noch keine Bewertungen
- PT Case LogsDokument2 SeitenPT Case Logsapi-174496267Noch keine Bewertungen
- 2nd Rotation PallDokument3 Seiten2nd Rotation Pallapi-174496267Noch keine Bewertungen
- May EvalDokument6 SeitenMay Evalapi-174496267Noch keine Bewertungen
- July Case StudyDokument18 SeitenJuly Case Studyapi-174496267Noch keine Bewertungen
- SIO 12 Syllabus 17Dokument3 SeitenSIO 12 Syllabus 17Paul RobaiaNoch keine Bewertungen
- Badminton Lesson 1 4 - 5 Grade: TH THDokument31 SeitenBadminton Lesson 1 4 - 5 Grade: TH THLoxcey LopezNoch keine Bewertungen
- Principal Component Analysis of Protein DynamicsDokument5 SeitenPrincipal Component Analysis of Protein DynamicsmnstnNoch keine Bewertungen
- Plants Life Cycles and PartsDokument5 SeitenPlants Life Cycles and PartsseemaNoch keine Bewertungen
- MP & MC Module-4Dokument72 SeitenMP & MC Module-4jeezNoch keine Bewertungen
- Marketing of Agriculture InputsDokument18 SeitenMarketing of Agriculture InputsChanakyaNoch keine Bewertungen
- KS4 Higher Book 1 ContentsDokument2 SeitenKS4 Higher Book 1 ContentsSonam KhuranaNoch keine Bewertungen
- Gujarat Technological University: Aeronautical EngineeringDokument16 SeitenGujarat Technological University: Aeronautical EngineeringumodiNoch keine Bewertungen
- Lec 5Dokument22 SeitenLec 5Abcdefgh EfghabcdNoch keine Bewertungen
- 6a. ICMR STSDokument15 Seiten6a. ICMR STSVishnu Praba ANoch keine Bewertungen
- List of StateDokument5 SeitenList of StatedrpauliNoch keine Bewertungen
- Impression Techniques in Complete Denture Patients: A ReviewDokument6 SeitenImpression Techniques in Complete Denture Patients: A ReviewRoja AllampallyNoch keine Bewertungen
- IS 2848 - Specition For PRT SensorDokument25 SeitenIS 2848 - Specition For PRT SensorDiptee PatingeNoch keine Bewertungen
- AP World History: Islamic Empires and Scientific AdvancementDokument55 SeitenAP World History: Islamic Empires and Scientific AdvancementJa'TasiaNoch keine Bewertungen
- Relation of Jurisprudence With Other Social Sciences - LLB NotesDokument4 SeitenRelation of Jurisprudence With Other Social Sciences - LLB NotesPranjaliBawaneNoch keine Bewertungen
- ROM Magazine V1i6Dokument64 SeitenROM Magazine V1i6Mao AriasNoch keine Bewertungen
- Design Your Loyalty Program in 2 WeeksDokument53 SeitenDesign Your Loyalty Program in 2 WeeksLorena TacuryNoch keine Bewertungen
- LDokument32 SeitenLDenNoch keine Bewertungen
- 2 Case StudyDokument8 Seiten2 Case Studysehrish khawerNoch keine Bewertungen
- KCL Thesis PrintingDokument4 SeitenKCL Thesis PrintingMelinda Watson100% (2)
- Optimum Work Methods in The Nursery Potting ProcessDokument107 SeitenOptimum Work Methods in The Nursery Potting ProcessFöldi Béla100% (1)
- 2019 ASME Section V ChangesDokument61 Seiten2019 ASME Section V Changesmanisami7036100% (4)
- Amma dedicates 'Green Year' to environmental protection effortsDokument22 SeitenAmma dedicates 'Green Year' to environmental protection effortsOlivia WilliamsNoch keine Bewertungen
- Lks Bahasa Inggris Kelas Vii Semester 1 Dan 2Dokument6 SeitenLks Bahasa Inggris Kelas Vii Semester 1 Dan 2ꓰꓡꓡꓰꓠ.ꓓꓰꓖꓰꓠꓰꓣꓰꓢꓢ.Noch keine Bewertungen
- Publications FireSafetyDesign SDokument369 SeitenPublications FireSafetyDesign SJayachandra Reddy AnnavaramNoch keine Bewertungen
- List of DEA SoftwareDokument12 SeitenList of DEA SoftwareRohit MishraNoch keine Bewertungen
- Biotechnology Eligibility Test (BET) For DBT-JRF Award (2010-11)Dokument20 SeitenBiotechnology Eligibility Test (BET) For DBT-JRF Award (2010-11)Nandakumar HaorongbamNoch keine Bewertungen