Beruflich Dokumente
Kultur Dokumente
May Case Study Final
Hochgeladen von
api-174496267Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
May Case Study Final
Hochgeladen von
api-174496267Copyright:
Verfügbare Formate
1 Amanuel Negussie DOS 731 May case study June 2013 Intensity Modulated Radiation Therapy (IMRT) Treatment
t of a Tongue Lesion History of Present Illness: BR is a 63 year old gentleman with a left sided cancer of the tongue that extends to the base. He first presented to otolaryngology clinic with a three-week history of a sore tongue. A biopsy performed in clinic demonstrated poorly differentiated squamous cell carcinoma. Physical examination also confirmed a mass on the left lateral mobile tongue. Microscopic description presented a tumor size at least 3 centimeter (cm) with 2.4 cm thickness. Multiple linked margins were positive for invasive carcinoma, lymphovascular invasion, and perineural invasion. In addition, a computed tomography (CT) scan performed in April 2013 showed an infiltrative mass that extended across the midline and invaded the left genioglossus and geniohyoid muscle. It also extended to myohyoid muscle, left retromolar trigone region, left tonsil, midline of the left soft palate, and midline of the left hard palate. No definitive evidence of lymphadenopathy was recorded. The tumor was staged T2NoMo. As a result, BR underwent left heminglossectomy, left selective neck dissection, and direct laryngoscopy in April 2013. BRs postoperative course was reported to be unremarkable. He was discharged 4 days after his surgery. He reported good appetite, and he gained 4 pounds over a month. He was able to tolerate soft foods and liquids. He denied any significant oral or throat pain. However, he reported some decrease in taste and dryness in his mouth since his surgery. Past Medical History: BR has a past medical history of depression, hypertension, and anemia. Social History: BR was an auto technician for 30 years. He retired 3 years ago. He is divorced and has two children, ages 36 and 38. BR smoked less than a pack per day for 40 years. He quit smoking one month ago. He has a remote history of heavy alcohol consumption but now drinks 1 or 2 beers per week. BR has no family history of malignancy. Medications: BR is currently taking Bacitracin ointment, Calcium carbonate, Chlorhexidine mouthwash, Sodium docusate, Oxycodone, Hydrocodone, and Ibuprofen. He has no known allergies. Diagnostic Imaging: BR had a diagnostic CT scan of the head and neck with non-ionic iodinated contrast in April 2013.
2 Radiation Oncologist Recommendations: the radiation oncologist discussed with the patient the rationale for adjuvant radiation therapy to the oral cavity, oropharynx, and bilateral neck for optimizing local control. He recommended treating the primary site associated with positive margins to 6600 centigray (cGy) with IMRT. He also planned to treat high risk areas in the surgical bed to 6000 cGy, and high risk uninvolved areas in the undissected neck on the contralateral side and in level IV bilaterally to 5000 cGy and 5400 cGy using simultaneous integrated boost (SIB) technique with IMRT. The radiation oncologist discussed the side effects and risks of radiation therapy including skin reaction, mucositis, xerostomia, impairment or loss of taste, fatigue, localized hair loss, risks for hypothyroidism, development of dewlap, osteoradionecrosis of the mandible, long term risk for stroke, remote risk of secondary malignancy, and remote risk of serious injury to the spinal cord. It was also mentioned to him that when radiation therapy is given concurrently with chemotherapy, there is an association for improved local control at a price of increased treatment toxicity with more intense mucositis and chronic long term problems of swallowing. The patient was in understanding of this information and elected to proceed with the recommendation for concurrent chemoradiation treatment. Given he does not have any significant facial swelling since his dental procedure, only 8 teeth were extracted. The Plan (Prescription): After a discussion with the patient, reviewing the chart, and examining the diagnostic study, the radiation oncologist decided to proceed with IMRT treatment. The treatment was prescribed to 6000 cGy at 200 cGy per fraction to the 97% isodose line for 30 fractions. This was followed by a boost of 600 cGy at 200 cGy per fraction to the 97% isodose line for 3 fractions. Patient Setup / Immobilization: BR was simulated in a supine position with his head towards the scanner (Figure 1). A wire was placed on his surgical scar. His head was fixed in a neutral position by using a headset (Figure 1). An aquaplast mask was made by warming a thermoplastic mesh in a warm bath and stretching it over the patients face, neck, and shoulders. The customized mask will be used to reproduce the same head position and restrict movement during treatment. BR had a sponge under his knees for comfort and his hands were crossed on his chest. No bite block was used to immobilize the tongue. In patients who are being treated for the base of the tongue with IMRT and where the contralateral neck is clinically negative, bite blocks should not be used in order to spare the contralateral parotid gland.1 Philips large bore 16 slice
3 CT machine was used for the simulation. Two head images were taken at 0.3 cm slices, with and without non-iodinated intravascular (IV) contrast. Anatomic Contouring: After the simulation was completed, the CT scan slices were imported in the Pinnacle3 9.0 treatment planning system (TPS). The CT slices without contrast were used as a primary image, and were fused with the CT slices with contrast and the preoperative CT diagnostic CT slices. The medical dosimetrist contoured the scar, spinal cord, brainstem, mandible, and posterior neck. He also created a skin contour by contracting the external contour by 3 millimeter (mm). Guided by the fused images, the radiation oncologist contoured the tumor bed, brachial plexus, right parotid, esophagus, larynx, oral cavity, clinical target volume (CTV) of the tumor bed, CTV of the surgical bed, CTV of the right neck, and CTV of the left neck. He also created the planning target volume (PTV) 66, PTV60, and PTV54 by expanding the CTVs by 5 mm. Before proceeding with planning, the dosimetrist created a spinal cord planning risk volume (PRV) and brainstem PRV by expanding the spinal cord and brainstem contour by 5 mm. He also created unspecified tissue (ust) contour by contracting the external contour and avoiding the PTV structures. In addition, he created a PTV54-60 with 1 mm margin around PTV 60 to help create adequate dose conformity for the two PTVs. Beam Isocenter / Arrangement: Varian 21 IX 3501 linear accelerator (Linac) machine was used to treat the patient. During the simulation process, the radiation oncologist placed the isocenter in the tumor. A 9-field beam arrangement at gantry angles of 160o, 120o, 80o, 40o, 0o, 320o, 280o, 240o, and 200o were arranged for the IMRT plan (Figure 2). In addition, a left and right lateral beam at 90o and 270o were set for the boost field (Figure 2). The collimator and couch angles were set at 0o for all fields. Treatment Planning: The maximum number of segments was set at 110 and a direct machine parameter optimization (DMPO) was selected. An objective of the Brainstem PRV was set for a maximum dose (max dose) of 1062 cGy, the spinal cord PRV was set for a max dose at 4500 cGy, the posterior neck was set for a max dose at 2800 cGy. In addition, PRV54-60 was set for a max dose of 5500 cGy, PTV 54 for a minimum dose volume histogram (min DVH) of 5400 cGy at 99% volume, PTV 60 max dose of 6500 cGy, PTV 60 for a min DVH of 6000 at 99% volume, and PTV 60 uniform dose of 6180 cGy. All the PTV objectives were weighted 5% and the rest objectives were weighted 1%. The plan was then optimized.
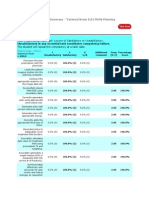
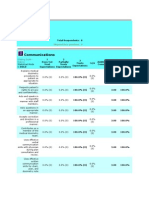
4 After reviewing the plan, more objectives were created to control dose to organs at risk (OR). These included 3 constraints for mandible, brachial plexus, esophagus, and larynx, 4 constraint for the right parotid, and 1 constraint for oral cavity. All the new objectives were weighted 1%. The weighting of the PTV objectives were changed to 10% and spinal cord PRV to 5%. The plan was reviewed multiple times, and the weightings of the IMRT objectives were adjusted based on the information retrieved from the DVH and the isodose lines. The plan was finalized with the 97% isodose line covering the PTV60 and PTV54 with a maximum dose of 6518 cGy located in PTV60 (Figure 3 and 4). All the ORs met the criteria except for the oral cavity, larynx, and mandible (Figure 4). This was due to the proximity of these structures to the tumor. In order to have an adequate PTV coverage, higher dose to these structures was needed. The dose to the mandible was 1.1% hotter, oral cavity 1% hotter, and larynx 1.8% hotter than the recommended tolerance. A right and left lateral field was used for the boost plan. A 1.3 cm margin around PTV60 was used to for the boost field (Figure 5). The spinal cord was blocked out of the treatment field by 7 mm. A new prescription point was used to calculate the plan since the isocenter from the primary IMRT did not fall within the boost field (Figure 6).2 A 15o wedge with the heel positioned anteriorly was used on both sides. However, the PTV coverage was cool superiorly and hot inferiorly. As a result, the orientation of the left wedge was adjusted to the heel facing inferiorly (Figure 6). A 48% weighting for the right lateral and 52% weighting for the left lateral provided the best PTV coverage. The plan was completed with the 97% isodose line covering PTV60 with a maximum dose of 681 cGy located within the PTV (Figure 6 and 7). Both plans were completed with a total monitor unit (MU) of 941, with 617 for the initial and 324 for the boost. The composite maximum dose was 7083 cGy located within PTV60. In addition, the composite dose meet the criteria, except the OR structures listed above (Figure 8). Quality Assurance / Physics Check: MU check was performed using the MuCheck 8.2.0 software. At our clinical site, a 5% deviation in MU is the tolerance for IMRT plans and 3% for 3 dimensional conformal radiation therapy (3DCRT) plans. Anything outside of this range needs to be recalculated and fixed by the dosimetrists or physicists prior to the first treatment. The initial IMRT plan was approved with an individual MU difference less than 5% (Figure 9a, 9b,
5 and 9c). In addition, the boost field was approved with both lateral MU difference below 3% (Figure 9d). A plan validation was also performed for the IMRT plan by ion chamber in solid water and ArcCheck diodes. The chamber plan percentage difference was 1.67%, and the average percentage of ArcCheck diodes passed by 98.4%. The summary of the test was printed and double checked by the dosimetrist. The dosimetrist also wrote an IMRT note stating the prescription, the maximum dose, and the quality assurance tests. In addition, medical dosimetrists and radiation therapists completed an IMRT pre-treatment checklist that included shifts, IMRT QA, and charting. Conclusion: One of the challenges that the dosimetrist faced when planning this case was meeting the constraints for all ORs while maintaining adequate PTV coverage. The extent of the tumor and the fact that the PTV covers a large portion of the neck area made it difficult to accomplish certain objectives. As a result, the physician decided covering the target is more important than delivering a few more doses to mandible, oral cavity, and larynx. In addition, according to RTOG 0920,3 the dose to spinal cord, brainstem, PTV56, PTV60, and PTV66 must be given a priority than all the rest structures. As a dosimetrist, it is always important to review these protocols for guidance in case of such challenges.
6 Figures
Figure 1. Patients setup position
Figure 2. Beam arrangement of the IMRT and boost fields
Figure 3. The sagittal, axial, and coronal view of the IMRT dose distribution
Brachial plexus Spinal cord PRV Spinal cord
PTV54 PTV60
PTV66
ust
Right parotid
Brainstem PRV Brainstem
Figure 4. DVH of the IMRT plan
Figure 5. The blocking pattern of the boost fields
Figure 6. The sagittal, axial, and coronal view of the boost dose distribution
10
Right parotid PTV60
PTV66
PTV54
Figure 7. DVH of the boost plan
11
PTV66 Brachial plexus PTV60 Spinal cord Spinal cord PRV PTV54
Right parotid ust Brainstem
PTV66
Brainstem PRV
Figure 8. DVH of the composite plan
12
Figure 9a. MuCheck of the IMRT treatment plan
13
Figure 9b. MuCheck of the IMRT treatment plan
14
Figure 9c. MuCheck of the IMRT treatment plan
15
Figure 9d. MuCheck of the boost treatment plan
16 References 1. Harrison LB, Sessions RB, Hong WK. Head and Neck Cancer: A Multidisciplinary Approach. 3rd ed. Philadelphia, PA. Lippincott Williams and Wilkins; 2009: 331-332. 2. IRCU Report 50. Prescribing, Recording, and Reporting, Photon Beam Therapy. Bethesda, MD. 1993: 29-30. 3. RTOG 0920. A phase III study of postoperative radiation therapy (IMRT) +/- Cetuximab for locally advanced resected head and neck cancer. http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0920. Accessed June 8, 2013.
Das könnte Ihnen auch gefallen
- Ec 102 Eclipseinverseplanningimrtandrapidarcv 13 CamanuelnegussieDokument1 SeiteEc 102 Eclipseinverseplanningimrtandrapidarcv 13 Camanuelnegussieapi-174496267Noch keine Bewertungen
- Amanuel Negussie: Certificate of AttendanceDokument1 SeiteAmanuel Negussie: Certificate of Attendanceapi-174496267Noch keine Bewertungen
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDokument1 SeiteV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267Noch keine Bewertungen
- BrachytherapyDokument3 SeitenBrachytherapyapi-174496267Noch keine Bewertungen
- Fall EvalsDokument6 SeitenFall Evalsapi-212894050Noch keine Bewertungen
- ResumeDokument2 SeitenResumeapi-174496267Noch keine Bewertungen
- Amanuel Final 5 1 14Dokument19 SeitenAmanuel Final 5 1 14api-174496267Noch keine Bewertungen
- ElectronDokument2 SeitenElectronapi-174496267Noch keine Bewertungen
- Joe RTDokument1 SeiteJoe RTapi-174496267Noch keine Bewertungen
- ImrtDokument3 SeitenImrtapi-174496267Noch keine Bewertungen
- PhotonDokument3 SeitenPhotonapi-174496267Noch keine Bewertungen
- Fall EvalsDokument6 SeitenFall Evalsapi-212894050Noch keine Bewertungen
- ComptotalsDokument3 SeitenComptotalsapi-174496267Noch keine Bewertungen
- For E-PortfolioDokument14 SeitenFor E-Portfolioapi-174496267Noch keine Bewertungen
- Fall EvalsDokument6 SeitenFall Evalsapi-212894050Noch keine Bewertungen
- August Citation AssignmentDokument2 SeitenAugust Citation Assignmentapi-174496267Noch keine Bewertungen
- ConferenceDokument7 SeitenConferenceapi-174496267Noch keine Bewertungen
- Monthly EvalDokument2 SeitenMonthly Evalapi-174496267Noch keine Bewertungen
- September Case StudyDokument20 SeitenSeptember Case Studyapi-174496267Noch keine Bewertungen
- Tally 1Dokument2 SeitenTally 1api-174496267Noch keine Bewertungen
- ConferencesDokument4 SeitenConferencesapi-174496267Noch keine Bewertungen
- Case Log FallDokument2 SeitenCase Log Fallapi-174496267Noch keine Bewertungen
- Comprehensive Case Study - AnDokument31 SeitenComprehensive Case Study - Anapi-174496267Noch keine Bewertungen
- Conference LogsDokument1 SeiteConference Logsapi-174496267Noch keine Bewertungen
- Comprehensive Case Study Final - AdjustedDokument17 SeitenComprehensive Case Study Final - Adjustedapi-174496267Noch keine Bewertungen
- May EvalDokument6 SeitenMay Evalapi-174496267Noch keine Bewertungen
- October Case StudyDokument15 SeitenOctober Case Studyapi-174496267Noch keine Bewertungen
- 2nd Rotation PallDokument3 Seiten2nd Rotation Pallapi-174496267Noch keine Bewertungen
- PT Case LogsDokument2 SeitenPT Case Logsapi-174496267Noch keine Bewertungen
- July Case StudyDokument18 SeitenJuly Case Studyapi-174496267Noch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Prevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDDokument7 SeitenPrevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDMusainah FeisalNoch keine Bewertungen
- Legalizing abortion in the Philippines for women's health and rightsDokument2 SeitenLegalizing abortion in the Philippines for women's health and rightsRosario Antoniete R. Cabilin100% (1)
- Weeblylp MedicinaDokument18 SeitenWeeblylp Medicinaapi-538325537Noch keine Bewertungen
- Part A Reading Task Playground Injuries Playground Surface MaterialDokument8 SeitenPart A Reading Task Playground Injuries Playground Surface MaterialMitra NabizadehNoch keine Bewertungen
- Sdera Demo Lesson DVD Worksheet 2021Dokument2 SeitenSdera Demo Lesson DVD Worksheet 2021api-396577001Noch keine Bewertungen
- Detailed Advertisement of Various GR B & C 2023 - 0 PDFDokument47 SeitenDetailed Advertisement of Various GR B & C 2023 - 0 PDFMukul KostaNoch keine Bewertungen
- PEMEDokument1 SeitePEMERajesh MohananNoch keine Bewertungen
- 100 Days of Jessica Smith Rotation Using DVDsDokument4 Seiten100 Days of Jessica Smith Rotation Using DVDsAusra CrowderNoch keine Bewertungen
- Mind Body PDFDokument357 SeitenMind Body PDFAzhari RahmatNoch keine Bewertungen
- The Real Paul Thibault: Nothing But The Truth..Dokument20 SeitenThe Real Paul Thibault: Nothing But The Truth..LancasterFirstNoch keine Bewertungen
- Interactive CME Teaching MethodsDokument5 SeitenInteractive CME Teaching MethodsROMSOPNoch keine Bewertungen
- EV3110 SIA Group ReportDokument38 SeitenEV3110 SIA Group ReportWill MyatNoch keine Bewertungen
- Pharmacology Mock Exam MCQDokument8 SeitenPharmacology Mock Exam MCQanaeshklNoch keine Bewertungen
- Resolve Family Drainage CatetherDokument16 SeitenResolve Family Drainage CatetherradeonunNoch keine Bewertungen
- Gene Ieee PDFDokument8 SeitenGene Ieee PDFJayaprabha ManiNoch keine Bewertungen
- Fitness WalkingDokument60 SeitenFitness WalkingJC LeriaNoch keine Bewertungen
- Massage Client Waiver Form 1 2Dokument1 SeiteMassage Client Waiver Form 1 2api-516845106Noch keine Bewertungen
- 798 3072 1 PBDokument12 Seiten798 3072 1 PBMariana RitaNoch keine Bewertungen
- Heavy Water Board RecruitmentDokument7 SeitenHeavy Water Board RecruitmentramavarshnyNoch keine Bewertungen
- Lucas MattoonDokument1 SeiteLucas Mattoonapi-248178524Noch keine Bewertungen
- Life Threatening Rhythm: Presenter: Muhammad Najmuddin Bin Hussain 2. Wan Muhammad Nasirudin Bin Wan YusoffDokument17 SeitenLife Threatening Rhythm: Presenter: Muhammad Najmuddin Bin Hussain 2. Wan Muhammad Nasirudin Bin Wan YusoffWan NasirudinNoch keine Bewertungen
- OrthodonticsDokument9 SeitenOrthodonticsReda IsmaeelNoch keine Bewertungen
- Kaplan Grade OverviewDokument5 SeitenKaplan Grade Overviewapi-310875630Noch keine Bewertungen
- Report On Legal Medicine PowerpointDokument31 SeitenReport On Legal Medicine PowerpointEdwin VillaNoch keine Bewertungen
- Roberts Race Gender DystopiaDokument23 SeitenRoberts Race Gender DystopiaBlythe TomNoch keine Bewertungen
- Hazards of Dietary Supplement Use: Anthony E. Johnson, MD Chad A. Haley, MD John A. Ward, PHDDokument10 SeitenHazards of Dietary Supplement Use: Anthony E. Johnson, MD Chad A. Haley, MD John A. Ward, PHDJean CotteNoch keine Bewertungen
- GIGITAN ULAR BERBISA: GEJALA, PENANGANAN DAN JENIS ULAR PALING BERBISADokument19 SeitenGIGITAN ULAR BERBISA: GEJALA, PENANGANAN DAN JENIS ULAR PALING BERBISAYudhistira ArifNoch keine Bewertungen
- Fertilizer Use by Crop in The Islamic Republic of IranDokument78 SeitenFertilizer Use by Crop in The Islamic Republic of Iransiamak77Noch keine Bewertungen
- Food Production (409) : Sample Question Paper Class X (2018-19) (NSQF)Dokument2 SeitenFood Production (409) : Sample Question Paper Class X (2018-19) (NSQF)Janavi M SNoch keine Bewertungen
- Chapter 9 - Managing Crises and National EmergenciesDokument26 SeitenChapter 9 - Managing Crises and National EmergenciesJayson TasarraNoch keine Bewertungen