Beruflich Dokumente
Kultur Dokumente
Heart Failure
Hochgeladen von
gavtuckerOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Heart Failure
Hochgeladen von
gavtuckerCopyright:
Verfügbare Formate
Looking at heart failure, most common causes are HTN and IHD, most patients eventually have heart
failure, doesnt function as a pump and reduced cardiac output. Average age is 75, important thing is poor prognosis, heart failure has a worse one than most cancers, 50% dead in 10 years. Average length of stay is 8 days, accounts for a lot of healthcare expenditure. Heart failure, patient presents with breathlessness, initially on exertion but then at rest, orthopnoea, paroxysmal nocturnal dyspnoea. Signs, tachycardia, limbs are swollen, peripheral oedema, raised JVP, third heart sound, pleural effusion, dull percussion note on right lung base. To prove it definitely, perform an echo, reduction in LVEJ, should be 70%, can be 20-40%. In practice, make the diagnosis clinically, another test for diagnosis is blood test, BNP >1,000, indicative of heart failure, real value is in the negative predictive value, >99%. If you do have heart failure, radiological appearance bats wing, pulmonary oedema white-out, predominantly in mid and lower zones, purely gravitational. What do you do? Make sure patient is oxygenated. May be distressed, they might be having an MI! Appropriate to give morphine in this situation, 2.5-5mg IV, give cyclimorph due to anti-emetic effect. Patient starts to feel better after opiate, also have vasodilatory properties, reduce pressure on the heart, mainstay of treatment is giving IV diuretics, dont give oral diuretics or thiazides, GIVE IV FUROSEMIDE 20-40mg, need to get rid of fluid. Some patients may already have low BP, danger of kidney under perfusion. No role for digoxin in acute heart failure, unless atrial fibrillation. Important distinction between acute and chronic failure, chronic is separate and approached differently. Be careful of balance between fluid overload and hypovolemia. In some patients with huge resistance to loop diuretics, then combine with thiazide. Vasodilators excellent in heart failure, isosorbide mononitrate, reduces pressure on the heart, use it in CHF as well. What if pressure goes too low? Dobutamine would be the drug of choice, b1 agonist, increase cardiac output, then give other medications as well, can use dopamine as well but not as good. Write a brief note on the management of acute heart failure, know t he treatments and the issues around the treatment.
Chronic heart failure. This is when patient is stabilised. Now the issue is different, make sure they dont get it again, survival is increased and the symptoms resolve, huge change in this treatment in recent decades. Used to give digoxin and loop diuretic, used to call it dropsy. The slide with treatment algorithm will answer any question on CHF. ACE inhibitor is absolutely vital!!!!!! Should be on a beta blocker and a diuretic. Overactivation of RAAS and autonomic nervous system, principal goal in treatment, antagonising these two systems. Mouse and cheese model of activating RAAS using diuretic, heart failure is condition where you gradually get worse. Can go down one of two pathways, add an ARB in addition to vasodilator and digoxin, or aldosterone antagonist, vasodilator and glycoside. NEVER add ARB, ACEI and aldosterone antagonist (favourite MCQ question on this triad). Diuretics, over activate RAAS, angiotensin II is main culprit, give a loop diuretic (thiazides for HTN), combine with ACEI or ARB. No real role for thiazide diuretics in heart failure. ACEI are cornerstone of treatment, drugs of first choice. Consensus trial, 1987, used to be diuretics and digoxin. Pay attention to atrial fibrillation, no P waves, 1/3 of patients with HF will have AF, most will also have HTN or CHD. When you add in enalapril after 6 months, halved the mortality rate, in placebo group, 44% were dead in 6 months. First study to show conclusively that ACEI were game changers. ACEI as initial therapy, stabilise the patient then introduce the ACEI. Dont give immediately, way too much going on, wait for 2-3 days before introduction. Key point about treatment of HF, take it up to the highest dose you can possibly tolerate, may as well be taking two glasses of water if on lower dose, ramipril 10mg, even if symptoms are controlled on 5mg, probably the biggest error in therapeutics of HF. What are the things which cause poor toleration? Poor renal function, watch out creatinine levels. Timeframe for upping the dose, 1.25mg for 3 days, move on to 2.5mg, probably on 5mg after discharge (average 11 days), push the BNP down below 1,000, will be standard of care soon. REMEMBER RAMIPRIL, peanuts, 4 for 5mg per day.
Beta blockers
Give them in heart failure, antagonising sympathetic nervous system, sodium and water retention, RAAS stimulation. Number of pivotal trials in mid 90s. Carvedilol is drug of choice, also bisoprolol. Average age of people in trials was 66, decade below patients we see, thats why we cant get to top doses of beta blockers, elderly patients cant tolerate well, still try and get as high as possible. On top of ACEI (Reduce mortality by 30%), reduces mortality by an EXTRA 34%. Contraindications, heart block, diabetes, Raynauds, asthma, COPD. Try to introduce beta blocker while patient is in hospital, start low and go slow. Watch the pulse rate. 3.125mg twice daily carvedilol, increase as much as you can, target is 25mg bd but we never reach that because patients are usually elderly. Tell patients to check their weight! Weight gain may be first sign of changes. Potassium-sparing diuretic is spironolactone, adding on spironolactone to BB, ACEI and diuretic is very good as shown by RAIL study, further 35% increase in survival. Other route is to add in ARB, will get a reduction in mortality, 25% reduction in mortality, remember candesartan, ARB of choice, losartan is crap, valsartan is BD, candesartan is cheapest, OD and has good outcome data. Principle, start with 4mg and work up to 32mg. Vasodilator therapy, if you have to add in spironolactone or ARB, immediately add in a nitrate, cant stress the importance of this enough. Allows you to unload so much better but no pressure on the kidneys. Isosorbide mononitrate, if ACEI and ARB intolerant, add in hydralazine with nitrate, only other combination that will reduce mortality in HF, 5-10 patients per year. Digoxin, product of the foxglove. Particularly used due to positive inotropic effect for atrial fibrillation, or in CHF, wont help survival or mortality, very good improvement in symptoms and hospitalisation. Add in digoxin even if no AF, to help patients symptoms.
Das könnte Ihnen auch gefallen
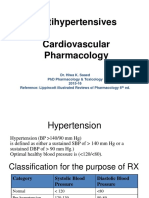
- Cardiovascular PharmacotherapyDokument32 SeitenCardiovascular PharmacotherapyFarahEzzlynnNoch keine Bewertungen
- 8D - HypertensionDokument58 Seiten8D - Hypertensionmashe1Noch keine Bewertungen
- HypertensionDokument10 SeitenHypertensionaa zzNoch keine Bewertungen
- Genxraver Girl Interrupted Usmle Step 2 Notes PDFDokument259 SeitenGenxraver Girl Interrupted Usmle Step 2 Notes PDFughbuzzoffNoch keine Bewertungen
- FARMAKOGNOSI - Obat AntihipertensiDokument7 SeitenFARMAKOGNOSI - Obat AntihipertensiTrianisa FebyNoch keine Bewertungen
- Cardiovascular Pharmacotherapy: Sutomo Tanzil Dept - of Pharmacology, Faculty of Medicine, Sriwijaya UniversityDokument44 SeitenCardiovascular Pharmacotherapy: Sutomo Tanzil Dept - of Pharmacology, Faculty of Medicine, Sriwijaya UniversitydeviamufidazaharaNoch keine Bewertungen
- Test Your Knowledge CHFDokument6 SeitenTest Your Knowledge CHFlorapeteNoch keine Bewertungen
- Drugs For Congestive Heart FailureDokument46 SeitenDrugs For Congestive Heart Failuresultan khabeeb100% (1)
- Treating Heart Failure: Current Guidelines for Pharmacological ManagementDokument11 SeitenTreating Heart Failure: Current Guidelines for Pharmacological ManagementKareem SaeedNoch keine Bewertungen
- Pharmacologic Treatment For Cardiac Failure: ACE InhibitorsDokument36 SeitenPharmacologic Treatment For Cardiac Failure: ACE InhibitorsGleden UmayamNoch keine Bewertungen
- Risk For: Decreased Cardiac OutputDokument5 SeitenRisk For: Decreased Cardiac OutputJamal HudaNoch keine Bewertungen
- 2017 Guideline for High Blood Pressure ManagementDokument3 Seiten2017 Guideline for High Blood Pressure ManagementSydrex SarmientoNoch keine Bewertungen
- Case Study Number 1Dokument5 SeitenCase Study Number 1Kevin Kyle RizarriNoch keine Bewertungen
- Jurnal Reading 2Dokument14 SeitenJurnal Reading 2Riko KuswaraNoch keine Bewertungen
- CardiologyDokument20 SeitenCardiologycnnc21Noch keine Bewertungen
- Antihypertensive AgentsDokument52 SeitenAntihypertensive Agentssameena ramzanNoch keine Bewertungen
- HYPERTENSION For Internal WrkshopDokument27 SeitenHYPERTENSION For Internal Wrkshopwalter agyemanNoch keine Bewertungen
- ACE Inhibitors & Angiotensin II Antagonists: October 1997Dokument4 SeitenACE Inhibitors & Angiotensin II Antagonists: October 1997indee533Noch keine Bewertungen
- Chapter - 024 Heart Failure DrugsDokument7 SeitenChapter - 024 Heart Failure DrugsthubtendrolmaNoch keine Bewertungen
- HypertensionDokument44 SeitenHypertensionMushabeNoch keine Bewertungen
- GROUP3 Multiple-ChoiceDokument4 SeitenGROUP3 Multiple-Choicelea mae andoloyNoch keine Bewertungen
- What Are The Toxicities of Amiodarone?: CardiologyDokument33 SeitenWhat Are The Toxicities of Amiodarone?: Cardiologylakshminivas PingaliNoch keine Bewertungen
- A Must-Read Review of HTN MedsDokument15 SeitenA Must-Read Review of HTN MedsCLAUDIANoch keine Bewertungen
- Anticoagulants: Commonly Prescribed IncludeDokument8 SeitenAnticoagulants: Commonly Prescribed IncludeRusmir GadzoNoch keine Bewertungen
- USMLE World Step 3 High Yield Notes 90 PagesDokument90 SeitenUSMLE World Step 3 High Yield Notes 90 PagesVS95% (55)
- Buletin Farmasi 06/2013Dokument12 SeitenBuletin Farmasi 06/2013afiq83Noch keine Bewertungen
- Heart Failure and Antidysrhythmic DrugsDokument38 SeitenHeart Failure and Antidysrhythmic DrugsYza Belle RamoNoch keine Bewertungen
- Essential Facts For Med-Surg Nurses: Emergency Cardiac DrugsDokument7 SeitenEssential Facts For Med-Surg Nurses: Emergency Cardiac DrugssanthyakunjumonNoch keine Bewertungen
- 7,8 - Antihypertensive DrugsDokument10 Seiten7,8 - Antihypertensive DrugsHusniya MehamedNoch keine Bewertungen
- Cardiac MedsDokument10 SeitenCardiac MedsSareeta MarieNoch keine Bewertungen
- Pharmacology 3Dokument7 SeitenPharmacology 3Maria Nichole JavarNoch keine Bewertungen
- Client With AnginaDokument3 SeitenClient With AnginavitaceeNoch keine Bewertungen
- CardiologyDokument8 SeitenCardiologykhalidzubairiNoch keine Bewertungen
- Cardiovascular Agents: Florianne E. Adlawan, R.NDokument31 SeitenCardiovascular Agents: Florianne E. Adlawan, R.NadlawanflorianneNoch keine Bewertungen
- Pharmacology Chapter 42 p-3Dokument19 SeitenPharmacology Chapter 42 p-3sho bartNoch keine Bewertungen
- Y7PH0566, Yedla Pradeep Kumar, 4 B.Pharmacy, Cips, Lam, GunturDokument33 SeitenY7PH0566, Yedla Pradeep Kumar, 4 B.Pharmacy, Cips, Lam, Gunturప్రదీప్ కుమార్100% (4)
- Antihypertensive Drugs GuideDokument52 SeitenAntihypertensive Drugs GuideAlan LealNoch keine Bewertungen
- Nadolol (RX) : Category: Beta-BlockersDokument6 SeitenNadolol (RX) : Category: Beta-BlockersSerious BlackNoch keine Bewertungen
- Lecture 1 antihypertensionSDSDokument7 SeitenLecture 1 antihypertensionSDSSara AbbasNoch keine Bewertungen
- Heart Failure With Reduced Ejection FractionDokument11 SeitenHeart Failure With Reduced Ejection Fractionpricilia ardianiNoch keine Bewertungen
- Major criteria and diagnosis of rheumatic feverDokument5 SeitenMajor criteria and diagnosis of rheumatic feverMarcoNoch keine Bewertungen
- Anti Hypertensive 20191211Dokument35 SeitenAnti Hypertensive 20191211helloitsmenadNoch keine Bewertungen
- Chapter 2 - A - III Hypertension TreatmentDokument37 SeitenChapter 2 - A - III Hypertension TreatmentEmmaNoch keine Bewertungen
- AntihypertensiveDokument17 SeitenAntihypertensiveDheeraj AryaNoch keine Bewertungen
- This Is ItDokument6 SeitenThis Is Itjagipeb439Noch keine Bewertungen
- The Beta-Blockers: Treating High Blood Pressure and Heart DiseaseDokument18 SeitenThe Beta-Blockers: Treating High Blood Pressure and Heart DiseaseAchmad Hidayat100% (1)
- AntihypertensiveDokument17 SeitenAntihypertensivelolNoch keine Bewertungen
- Management of HypertensionDokument19 SeitenManagement of HypertensionChandana RajuNoch keine Bewertungen
- CVS PharmacologyDokument60 SeitenCVS PharmacologyGølà Sèèñàà–baale irraaNoch keine Bewertungen
- Manage Hypertension with Activity Restrictions and MedicationsDokument19 SeitenManage Hypertension with Activity Restrictions and MedicationsLyre Byron CarpioNoch keine Bewertungen
- CVS (HF, HTN) PharmacologyDokument99 SeitenCVS (HF, HTN) PharmacologyCherenet TomaNoch keine Bewertungen
- Drugs For Chronic Heart FailureDokument6 SeitenDrugs For Chronic Heart FailureAndrés LópezNoch keine Bewertungen
- End-Stage Heart Disease Management and Palliative Care GuidelinesDokument44 SeitenEnd-Stage Heart Disease Management and Palliative Care GuidelinesCyrille AgnesNoch keine Bewertungen
- Heart Failure Managing HF Related Peripheral Oedema in Primary CareDokument1 SeiteHeart Failure Managing HF Related Peripheral Oedema in Primary CareParth VinaypatilNoch keine Bewertungen
- (PCOL) Cardio and Renal Drugs - Test BankDokument20 Seiten(PCOL) Cardio and Renal Drugs - Test BankGriselle GomezNoch keine Bewertungen
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesVon EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesBewertung: 4 von 5 Sternen4/5 (1)
- A Simple Guide to Hypertension and Heart DiseasesVon EverandA Simple Guide to Hypertension and Heart DiseasesBewertung: 5 von 5 Sternen5/5 (1)
- The High Blood Pressure Diet Natural Foods that will Lower your Blood Pressure within Weeks!Von EverandThe High Blood Pressure Diet Natural Foods that will Lower your Blood Pressure within Weeks!Noch keine Bewertungen
- The Amazing Way to Reverse Heart Disease Naturally: Beyond the Hypertension Hype: Why Drugs Are Not the AnswerVon EverandThe Amazing Way to Reverse Heart Disease Naturally: Beyond the Hypertension Hype: Why Drugs Are Not the AnswerBewertung: 5 von 5 Sternen5/5 (2)
- Cholesterol: 50 Ways to Reduce It NaturallyVon EverandCholesterol: 50 Ways to Reduce It NaturallyBewertung: 3 von 5 Sternen3/5 (1)
- Swan Essay Gavin Tucker 11365886Dokument4 SeitenSwan Essay Gavin Tucker 11365886gavtuckerNoch keine Bewertungen
- Gavin Tucker CVDokument1 SeiteGavin Tucker CVgavtuckerNoch keine Bewertungen
- Irish Mace Debating ScheduleDokument12 SeitenIrish Mace Debating SchedulegavtuckerNoch keine Bewertungen
- Heart FailureDokument2 SeitenHeart FailuregavtuckerNoch keine Bewertungen
- Inventaris IGD 2022 TerbaruDokument5 SeitenInventaris IGD 2022 TerbaruEryNoch keine Bewertungen
- 490.082 Microsite PublicDokument16 Seiten490.082 Microsite PublicA.J. YounesNoch keine Bewertungen
- Left Ventricular VentingDokument3 SeitenLeft Ventricular VentingVAD CoordinatorNoch keine Bewertungen
- NRes1 AssignmentDokument2 SeitenNRes1 AssignmentAinee MeuvinNoch keine Bewertungen
- WB CC Critical Care Front MatterDokument18 SeitenWB CC Critical Care Front MatterkushishaNoch keine Bewertungen
- Streptococcus Pneumoniae (Pneumococcus) - OverviewDokument4 SeitenStreptococcus Pneumoniae (Pneumococcus) - OverviewstarykNoch keine Bewertungen
- Surveillance of Healthcare-Associated Infections in Indonesian HospitalsDokument12 SeitenSurveillance of Healthcare-Associated Infections in Indonesian HospitalsRidha MardiyaniNoch keine Bewertungen
- Factors Affecting Inter Individual Variations in Drug ResponseDokument10 SeitenFactors Affecting Inter Individual Variations in Drug Responsehumera50% (4)
- Gabix Caps Leaflet PakistanDokument2 SeitenGabix Caps Leaflet Pakistandalalala7662Noch keine Bewertungen
- Artificial PancreasDokument5 SeitenArtificial PancreasShreeja SPNoch keine Bewertungen
- Endoscopic DacryocystorhinostomyDokument17 SeitenEndoscopic Dacryocystorhinostomyapi-19500641Noch keine Bewertungen
- 4749 BPV Catalogue EU 2017 Final PDFDokument107 Seiten4749 BPV Catalogue EU 2017 Final PDFkim bouNoch keine Bewertungen
- Healthcare Waste Management EssentialsDokument10 SeitenHealthcare Waste Management EssentialsMohamedErrmaliNoch keine Bewertungen
- Gamil Sayed Gamil ZeedanDokument48 SeitenGamil Sayed Gamil ZeedangamNoch keine Bewertungen
- Herpangina FinalDokument7 SeitenHerpangina FinalDeity CelleNoch keine Bewertungen
- Chapter 31 Dyslipidemia UpdatedDokument37 SeitenChapter 31 Dyslipidemia UpdatedMai TarekNoch keine Bewertungen
- Common Side Effects of OtezlaDokument57 SeitenCommon Side Effects of OtezlaMica JeremijevicNoch keine Bewertungen
- Dissociation Affect Dysregulation Somatization BVDKDokument22 SeitenDissociation Affect Dysregulation Somatization BVDKkanuNoch keine Bewertungen
- OperativenotesinsurgeryDokument9 SeitenOperativenotesinsurgerySakib EhsanNoch keine Bewertungen
- Shilajit Benefits, Nutrition Facts, Uses and Side Effects - Dr. AxeDokument13 SeitenShilajit Benefits, Nutrition Facts, Uses and Side Effects - Dr. Axefoundryx2561Noch keine Bewertungen
- Joshua Greenlee Mba HT/HTL (Ascp), Scott Webster PHD, Howard Gray Bs MT (Ascp), Patricia Reeves HT (Ascp), Erico Von Bueren PHD MorDokument1 SeiteJoshua Greenlee Mba HT/HTL (Ascp), Scott Webster PHD, Howard Gray Bs MT (Ascp), Patricia Reeves HT (Ascp), Erico Von Bueren PHD MorRashid AliNoch keine Bewertungen
- DKD and Sglt2iDokument61 SeitenDKD and Sglt2iماكريلا المصريNoch keine Bewertungen
- Caries Risk AssessmentDokument33 SeitenCaries Risk AssessmentSomya Jain100% (1)
- Distribution of Narcotic and Other Controlled SubstancesDokument11 SeitenDistribution of Narcotic and Other Controlled SubstancesJyothsna SathpadiNoch keine Bewertungen
- Cebu Normal University: Drug StudyDokument2 SeitenCebu Normal University: Drug StudyGwen Marie Taboada100% (1)
- Review - Presby Residency ManualDokument400 SeitenReview - Presby Residency ManualSneha SutharNoch keine Bewertungen
- Hemolytic UremicsyndromeDokument60 SeitenHemolytic UremicsyndromeMuhammad AleemNoch keine Bewertungen
- Organophosphorus Insecticide Induced Hemorrhagic Pancreatitis - A Case ReportDokument3 SeitenOrganophosphorus Insecticide Induced Hemorrhagic Pancreatitis - A Case ReportIOSRjournalNoch keine Bewertungen
- Pharmacy Formulary - Booklet - 2016Dokument178 SeitenPharmacy Formulary - Booklet - 2016pcartercNoch keine Bewertungen
- Intermittent ExotropiaDokument15 SeitenIntermittent ExotropiakarenafiafiNoch keine Bewertungen