Beruflich Dokumente
Kultur Dokumente
Cardiac Catheterization
Hochgeladen von
jacallisOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cardiac Catheterization
Hochgeladen von
jacallisCopyright:
Verfügbare Formate
CARDIAC CATHETERIZATION
More information in Pagana and Pagana
Clarification for catheterization and chronic stable angina patient:
Main reasons a cardiac catheterization is recommended for a patient with chronic stable
angina (according to American College of Cardiology Foundation and American Heart
Association):
Patients with disabling chronic stable angina despite medical therapy
High-risk criteria on clinical assessment or noninvasive testing regardless
of anginal severity
Patient who have survived sudden cardiac death or serious ventricular
arrhythmia
Patients with angina and symptoms and signs of congestive heart failure
PRE:
1. Assess for allergies to radiopaque dye, iodine, or shellfish. Patient may be
pretreated for the allergies.
2. Written, informed consent by physician
3. NPO for 6-8 hours prior to procedure
4. Adequate hydration
a. IV insertion with fluids as ordered
b. Clear liquids up to 4 hours before procedure may be allowed
5. Use of N-acetylcysteine (Mycomyst) prior to and post cardiac catheterization in
patients who are at risk for contrast nephropathy (for example, may treat if
creatinine > 1.5, but depends on the hospital policy)
6. Assessment of baseline vital signs, oxygen saturation, and peripheral pulses.
Abnormal labs that may affect the catheterization should be communicated to the
cath lab (information on front of chart, called to cath lab).
7. Explain the procedure to the patient. Explain that they will be awake and may
experience a flushing sensation as the dye is injected or feel fluttering as the
catheter passes through the heart.
8. Medications: Hold metformin (Glucophage). Generally, hold low molecular
weight heparin (for example, Lovenox) on the day of the catheterization. Check
adjusted insulin order for day of catheterization.
POST:
1. View post procedure orders and agency policy
2. Maintain strict bedrest per physician’s orders (up to 4-6 hours) with head of
bed elevated < 15-30 degrees
3. Continuous EKG monitoring
4. Monitor VS, oxygen saturation per agency protocol.
5. Assess peripheral pulses, color, sensation, temperature of extremity, signs of
bleeding or hematoma at insertion site with vital signs
6. Maintain dressing at insertion site
7. Maintain IV, encourage oral fluids, and monitor intake and output
8. Report significant problems to physician: chest pain, dysrhythmias, bleeding,
hematoma, significant changes in vital signs or peripheral pulses
Das könnte Ihnen auch gefallen
- 2017 05 GC Pocket CardDokument2 Seiten2017 05 GC Pocket Cardapi-312241089Noch keine Bewertungen
- CC Concept MapDokument11 SeitenCC Concept Mapapi-546355187Noch keine Bewertungen
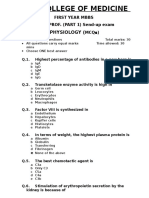
- 1st Year Sendup MCQsDokument8 Seiten1st Year Sendup MCQsTARIQNoch keine Bewertungen
- Lightning Flowers by Katherine E. StandeferDokument260 SeitenLightning Flowers by Katherine E. StandeferPranab Pattanaik100% (2)
- CCU Clinical GuidelinesDokument63 SeitenCCU Clinical GuidelinesHAMMYER ALROKHAMINoch keine Bewertungen
- CardioDokument7 SeitenCardioGerald AndrinNoch keine Bewertungen
- Problem-based Approach to Gastroenterology and HepatologyVon EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNoch keine Bewertungen
- Selected Nursing Diagnoses and Interventions For Patients With DysrhythmiasDokument19 SeitenSelected Nursing Diagnoses and Interventions For Patients With Dysrhythmiaslanie_jecielNoch keine Bewertungen
- Acute Biologic Crisis 1Dokument45 SeitenAcute Biologic Crisis 1Nina OaipNoch keine Bewertungen
- StrokeDokument6 SeitenStrokebrendavenegasNoch keine Bewertungen
- Shock Types 141009102815 Conversion Gate01Dokument41 SeitenShock Types 141009102815 Conversion Gate01Samjaisheel SamsonNoch keine Bewertungen
- Rosenberg Circulatory Assist DevicesDokument61 SeitenRosenberg Circulatory Assist DevicesMilisha Albro100% (1)
- Care of Patient With TPM Slide PresentationDokument16 SeitenCare of Patient With TPM Slide PresentationirzehronNoch keine Bewertungen
- Cardiac II Study GuideDokument6 SeitenCardiac II Study GuiderunnermnNoch keine Bewertungen
- Swan Ganz CathetersDokument27 SeitenSwan Ganz CatheterschadchimaNoch keine Bewertungen
- Cardiac Catheterization - Post ProcedureDokument2 SeitenCardiac Catheterization - Post ProcedureHendi Refiaguna100% (1)
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDokument34 SeitenArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Noch keine Bewertungen
- Acuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiesDokument16 SeitenAcuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiessamuelNoch keine Bewertungen
- 18 NCP Ileal ConduitDokument11 Seiten18 NCP Ileal ConduitICa MarlinaNoch keine Bewertungen
- Cardiovascular System: By: Marc Anthony Liao RNDokument59 SeitenCardiovascular System: By: Marc Anthony Liao RNloveseeker06Noch keine Bewertungen
- MVR CabgDokument57 SeitenMVR CabgRoshani sharmaNoch keine Bewertungen
- Necrotizing Otitis 2022Dokument20 SeitenNecrotizing Otitis 2022asmashNoch keine Bewertungen
- Fluid and Electrolyte Balance in ICUDokument46 SeitenFluid and Electrolyte Balance in ICUtapas_kbNoch keine Bewertungen
- Nervous System AlterationsDokument45 SeitenNervous System AlterationsMajesty ParkerNoch keine Bewertungen
- Chest Pain: Jean J. Chatham, MDDokument40 SeitenChest Pain: Jean J. Chatham, MDYermia RashaquatNoch keine Bewertungen
- Temporary Pacemakers-SICU's 101 PrimerDokument51 SeitenTemporary Pacemakers-SICU's 101 Primerwaqas_xsNoch keine Bewertungen
- Medical Surgical Nursing Critical Thinking in Patient Care Single Volume 4th Edition Lemone Test BankDokument4 SeitenMedical Surgical Nursing Critical Thinking in Patient Care Single Volume 4th Edition Lemone Test BankRebeccaGilliamNoch keine Bewertungen
- Ventricular Assist DeviceDokument4 SeitenVentricular Assist DevicemariakristinaNoch keine Bewertungen
- Arterial LinesDokument9 SeitenArterial LinesRei IrincoNoch keine Bewertungen
- Basic Ecg: A Report By: Clinical Clerk Mary Hazel TeDokument74 SeitenBasic Ecg: A Report By: Clinical Clerk Mary Hazel TeHazel Arcosa100% (1)
- Arrhythmia: Diagnosis and ManagementDokument79 SeitenArrhythmia: Diagnosis and ManagementBill DiazNoch keine Bewertungen
- HW InotropesDokument3 SeitenHW InotropesNatalie YeohNoch keine Bewertungen
- Hepatic Encephalopathy and ComaDokument19 SeitenHepatic Encephalopathy and ComaJas Castro JoveroNoch keine Bewertungen
- Pacemaker NotesDokument7 SeitenPacemaker Notesrohit860Noch keine Bewertungen
- Intra Aortic Balloon PumpDokument5 SeitenIntra Aortic Balloon PumpZainal 'babeh' Arifin100% (1)
- Valvular Heart Disease 2Dokument46 SeitenValvular Heart Disease 2Topea BogdanNoch keine Bewertungen
- Icu Sop: TOPIC: Length of Stay in ICUDokument5 SeitenIcu Sop: TOPIC: Length of Stay in ICURohit RajeevanNoch keine Bewertungen
- Cad ....Dokument94 SeitenCad ....AnanthibalaNoch keine Bewertungen
- Sinus ArrhythmiaDokument6 SeitenSinus ArrhythmiaVincent Maralit MaterialNoch keine Bewertungen
- Cs-Cardiac-023-Essential Cardiac LabsDokument2 SeitenCs-Cardiac-023-Essential Cardiac LabsColeen YraolaNoch keine Bewertungen
- Aortic RegurgitationDokument7 SeitenAortic RegurgitationazaliavirsaNoch keine Bewertungen
- Renal Failure PresentationDokument65 SeitenRenal Failure PresentationBhawna JoshiNoch keine Bewertungen
- Pulsus ParadoxusDokument2 SeitenPulsus ParadoxusHassan.shehriNoch keine Bewertungen
- Peak Flow MeterDokument3 SeitenPeak Flow MeterNicole PramonoNoch keine Bewertungen
- ACLS Class Packet PDFDokument9 SeitenACLS Class Packet PDFImam GultomNoch keine Bewertungen
- Abg Made EasyDokument24 SeitenAbg Made EasynbvillarazoNoch keine Bewertungen
- PedsnotesDokument18 SeitenPedsnoteskp13oyNoch keine Bewertungen
- S1M3 Update Fluid Resuscitation Management in Emergency CasesDokument70 SeitenS1M3 Update Fluid Resuscitation Management in Emergency Casesgriya medicaNoch keine Bewertungen
- Emergency Drugs KathDokument29 SeitenEmergency Drugs Kathmajin655Noch keine Bewertungen
- Supraventricular TachycardiaDokument9 SeitenSupraventricular TachycardiaclubsanatateNoch keine Bewertungen
- ElectrocardiogramDokument52 SeitenElectrocardiogramTuong HoangManhNoch keine Bewertungen
- Pacing Week PresentationsDokument54 SeitenPacing Week PresentationsjoejenningsNoch keine Bewertungen
- ECMO and Right Ventricular FailureDokument9 SeitenECMO and Right Ventricular FailureLuis Fernando Morales JuradoNoch keine Bewertungen
- Concept MapDokument22 SeitenConcept Mapapi-3017275530% (1)
- Inotropes, Excellent Article, With DosingDokument47 SeitenInotropes, Excellent Article, With DosingNavojit ChowdhuryNoch keine Bewertungen
- Arrhythmia ReviewDokument33 SeitenArrhythmia ReviewMark Hammerschmidt100% (3)
- Acls Course HandoutsDokument8 SeitenAcls Course HandoutsRoxas CedrickNoch keine Bewertungen
- HUTTDokument25 SeitenHUTTdrdj14100% (1)
- ICU Scoring Systems A Complete Guide - 2020 EditionVon EverandICU Scoring Systems A Complete Guide - 2020 EditionNoch keine Bewertungen
- NURSING CARE OF ADULTS II: Passbooks Study GuideVon EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNoch keine Bewertungen
- NCERT - Exemplar - Life ProcessesDokument26 SeitenNCERT - Exemplar - Life ProcessesRagini BaghelNoch keine Bewertungen
- Shock: Principles of Management: Nathan W. Mick, MD Massachusetts General Hospital Brigham and Women's HospitalDokument21 SeitenShock: Principles of Management: Nathan W. Mick, MD Massachusetts General Hospital Brigham and Women's Hospitalifan zulfantriNoch keine Bewertungen
- 9501-001-50 REV H1 Physicians GuideDokument54 Seiten9501-001-50 REV H1 Physicians GuidejimurgaNoch keine Bewertungen
- Pemilihan Anastesi Penyakit JantungDokument10 SeitenPemilihan Anastesi Penyakit JantungAndri HikmawanNoch keine Bewertungen
- Critical Care of Children With Heart Disease 2010Dokument735 SeitenCritical Care of Children With Heart Disease 2010Haikel Mhamed100% (1)
- DLL Week 3 Eng Q3Dokument15 SeitenDLL Week 3 Eng Q3Clarine Jane NunezNoch keine Bewertungen
- HemodialysisDokument120 SeitenHemodialysissigmundmaharajanNoch keine Bewertungen
- Grade 6 Q2 Science LASDokument52 SeitenGrade 6 Q2 Science LASEMILY MAG-ALASIN100% (7)
- BPT First Year Syllabus Rabindranath Tagore UniversityDokument33 SeitenBPT First Year Syllabus Rabindranath Tagore Universitysubhu7678Noch keine Bewertungen
- Guide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Dokument8 SeitenGuide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Ernie G. Bautista II, RN, MD100% (6)
- Drug Study AMIODARONE & PROPOFOLDokument3 SeitenDrug Study AMIODARONE & PROPOFOLNIKKI CARYL ZAFRANoch keine Bewertungen
- Doppler UltrasoundDokument2 SeitenDoppler UltrasoundReiruki SawadaNoch keine Bewertungen
- Cath Lab - Interventional Radiology Nursing Skills ChecklistDokument7 SeitenCath Lab - Interventional Radiology Nursing Skills Checklistdk15janNoch keine Bewertungen
- PracticeExam 4 QsDokument17 SeitenPracticeExam 4 QsBehrouz YariNoch keine Bewertungen
- Manajemen Disritmia Kardiak IntraoperatifDokument53 SeitenManajemen Disritmia Kardiak IntraoperatifAbi FaizNoch keine Bewertungen
- Learn The Anatomy of The HeartDokument2 SeitenLearn The Anatomy of The Heartapi-534129744Noch keine Bewertungen
- Date: 26 July 2019 Ms Zohra Shiraz Contractor Saidunnisa House, 2Nd FLR, Flat No 12,48/A, Naushir Bharucha Marg, Opp Grant Road Rly STN West Mumbai Mumbai 400007 MaharashtraDokument7 SeitenDate: 26 July 2019 Ms Zohra Shiraz Contractor Saidunnisa House, 2Nd FLR, Flat No 12,48/A, Naushir Bharucha Marg, Opp Grant Road Rly STN West Mumbai Mumbai 400007 MaharashtraZohra ContractorNoch keine Bewertungen
- Anatomy and PhysiologyDokument22 SeitenAnatomy and PhysiologyFreeNursingNotes100% (6)
- Venous System Arterial System: A. Artery A.A. Arteries L. Left R. Right v. Vein V.V. VeinsDokument2 SeitenVenous System Arterial System: A. Artery A.A. Arteries L. Left R. Right v. Vein V.V. VeinsJann ericka Jao100% (2)
- Chapter 13 Cardiovascular ResponsesDokument32 SeitenChapter 13 Cardiovascular ResponsesMARIA FERNANDA RONDONNoch keine Bewertungen
- A01628 CH19Dokument36 SeitenA01628 CH19Yannis ZoldenbergNoch keine Bewertungen
- PBL FisiologiDokument12 SeitenPBL FisiologiZakiah Tuan MahmoodNoch keine Bewertungen
- 1 Practise Questions Keith Moore 5th Edition Should ReadDokument113 Seiten1 Practise Questions Keith Moore 5th Edition Should ReadNasan Shehada100% (1)
- Structure of Human Heart-External FeaturesDokument5 SeitenStructure of Human Heart-External FeaturesAde Sintia DeviNoch keine Bewertungen
- Blue Boxes SummaryDokument16 SeitenBlue Boxes Summaryridin007Noch keine Bewertungen
- Nano Technology in MedicineDokument9 SeitenNano Technology in MedicineNandhini Nataraj NNoch keine Bewertungen
- Post Op Cabg CareDokument31 SeitenPost Op Cabg CareYeria Rayanti100% (1)
- All Four Heart Valves Lie Along The Same PlaneDokument2 SeitenAll Four Heart Valves Lie Along The Same PlaneSulochana ChanNoch keine Bewertungen