Beruflich Dokumente
Kultur Dokumente
Root Cause Analysis Paper
Hochgeladen von
api-272959759Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Root Cause Analysis Paper
Hochgeladen von
api-272959759Copyright:
Verfügbare Formate
Running Head: MEDICATION NON-ADHERENCE: A ROOT CAUSE ANALYSIS
Medication Non-Adherence: A Root Cause Analysis
Brianna H. DeValk
Bon Secours Memorial College of Nursing
Authors Note
Brianna DeValk is currently a Registered Nurse enrolled in the
Bachelor of Science Degree program at Bon Secours Memorial College of Nursing. On my
honor, I have neither given nor received aid on this assignment or test, and I pledge that I am in
compliance with the BSMCON Honor System. Any correspondence to this paper can be
directed to the Bon Secours Memorial College of Nursing student website and addressed in the
Nursing 3206 class discussion board.
MEDICATION NON-ADHERENCE: A ROOT CAUSE ANALYSIS
Medication noncompliance, otherwise known as medication non-adherence, is one of the
leading causes of hospital re-admissions, poor disease outcomes, and rising health care costs in
chronically ill patients. Adherence, an expression used somewhat synonymously with the term
compliant, describes the ratio (timing, dosage, and frequency) of prescribed medication doses
actually taken by the patient over a designated time period. In contrast, compliance is used
within the medical profession to describe simply whether or not the patient is following
providers orders; a far more passive approach to analyzing patient date. The term Adherence,
implies an active role in collaboration with a prescriber, and non-adherence encompasses the
diverse reasons for patients not following a treatment recommendation (Kalogianni, 2011, pg.
157). As a healthcare provider, understanding the reasons for non-adherence is necessary to
improve therapeutic effectiveness and overall patient health.
Patients presenting with HIV, Human Immunodeficiency Virus, and an actively
replicating viral load are among the chronically ill who absolutely must remain adherent to
prescribed medication regimens. Medications such as Stribild and Atripla, potent antiretrovirals,
are designed to be taken at the same time every day. These medications prevent the replication of
the HIV virus essentially allowing the body to fight-off the remaining viral components. HIV
remains within the patients blood stream, however, it is no longer transmittable. The patient
needs to remain consistent with daily medication administration in order to control this
replicatory process; if an extended period of time has lapsed between doses, the patient risks
developing a drug resistance thus leading to a loss of viroligic control. Identifying those with
adherence-related challenges that require attention and implementing appropriate strategies to
enhance adherence are essential roles for all members of the treatment team (Guidelines, 2014).
Several factors may contribute to medication non-adherence in patients with HIV. Early
MEDICATION NON-ADHERENCE: A ROOT CAUSE ANALYSIS
diagnosis of those at risk for developing behaviors associated with non-adherence is crucial
when treating patients with chronic diseases processes, like HIV. Construction of a fishbone
diagram assisted with the identification of a number of predisposing factors associated with nonadherence. These factors consisted of variances of: knowledge deficits associated with
medications/ doses/ purposes/ symptom management, deficient communication on behalf of the
healthcare provider, and economic hardship.
Formulation of the fishbone diagram began with the problem statement Non-adherence
with HIV medication regimen. Categories designated to further analyze causative factors are as
follows: Economic, Healthcare Provider, Complexity of Therapy, Condition: Timeline, and
Patient. All causes identified fit appropriately into the diagram. Inclusions within each category
are as follows:
Category
Economic
Healthcare Provider
Complexity of Therapy
Condition: Timeline
Patient
Inclusions
Cost
Unpredictable living conditions
Inadequate access to health care
Lack of established relationship with patient leading to a lack of
necessary encouragement and support.
Lack of communication regarding benefits of therapy, medication
instructions, and side effects
Length of Therapy
Number of Medications and associated doses
Inconvenience with patients schedule
Side effects of medication: impotence, heart burn, etc.
Absence of symptoms leads many patients to feel that their
condition has been managed. There is a severe lack of knowledge
regarding effects if medication suddenly stopped.
Adherence to medication regimens for chronic disease processes is
known to decline over time. Patients get tired of taking the same
medication, adhering to the same schedule, etc.
Intellectual Limitation
Physical Impairment
Substance Abuse
MEDICATION NON-ADHERENCE: A ROOT CAUSE ANALYSIS
Further categorization of causative factors was deemed unnecessary.
The root cause of medication non-adherence in HIV patients is far more complicated than
the diagrams indicates. Each HIV patient presents with a unique history and risk potential. The
key to maintaining patient adherence is early recognition of causative factors. Adherence is
better conceptualized as a variable behavior, rather than a trait characteristic: (Elliot, 2008, pg.
601). Medication non-adherence is a series of behaviors that may be mistaken as noncompliance. Quality patient healthcare provider interaction should reveal the potential for risks.
Therapeutic communication and behavioral reviews may then be incorporated into plan of care
so as ensure patient adherence to ordered medication regimen.
MEDICATION NON-ADHERENCE: A ROOT CAUSE ANALYSIS
References:
Elliott, R., Shinogle, J., Peele, P., Bhosle, M., & Hughes, D. (2008). Understanding
Medication Compliance and Persistence from an Economics Perspective. Value in
Health,11(4), 600-610.
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and
Adolescents. (2014, May 1). Retrieved October 22, 2014.
Kalogianni, A. (2011). Factors affect in patient adherence to medication
regimen. Health Science Journal, 5(3), 157-158.
Das könnte Ihnen auch gefallen
- 8D ProblemDokument5 Seiten8D ProblempitherstaranNoch keine Bewertungen
- Root Cause Analysis Paper - e BlantonDokument9 SeitenRoot Cause Analysis Paper - e Blantonapi-314215771Noch keine Bewertungen
- WEEK 3. Quality and Safe Management in The ERDokument19 SeitenWEEK 3. Quality and Safe Management in The ERAira Espleguira100% (1)
- Zero Defect SamplingDokument7 SeitenZero Defect SamplingmasoodpashNoch keine Bewertungen
- PDSA Directions and Examples: IHI (Institute For Healthcare Improvement) Web SiteDokument8 SeitenPDSA Directions and Examples: IHI (Institute For Healthcare Improvement) Web Siteanass sbniNoch keine Bewertungen
- Root Cause AnalysisDokument7 SeitenRoot Cause Analysisapi-3163522290% (1)
- Chapter 1: Research & Evidence in NursingDokument3 SeitenChapter 1: Research & Evidence in NursingNurseNancy93100% (1)
- APPG Patient Empowerment ReportDokument36 SeitenAPPG Patient Empowerment ReportkiranNoch keine Bewertungen
- Ethical and Legal Issues in Nursing and HealthDokument33 SeitenEthical and Legal Issues in Nursing and HealthSofonias Selamu100% (1)
- Marketing 91Dokument6 SeitenMarketing 91Deepak Kalonia JangraNoch keine Bewertungen
- Pareto Chart Exercise1Dokument6 SeitenPareto Chart Exercise1Walt PrystajNoch keine Bewertungen
- Standards For Medicines ManagementDokument112 SeitenStandards For Medicines ManagementHélder AntunesNoch keine Bewertungen
- Factors, Measures, and Problems of Quality Costs Program Implementation in The Manufacturing EnvironmentDokument6 SeitenFactors, Measures, and Problems of Quality Costs Program Implementation in The Manufacturing EnvironmentFahad IzharNoch keine Bewertungen
- Morbidity and Mortality Conference ManualDokument22 SeitenMorbidity and Mortality Conference Manualkelly_ann23Noch keine Bewertungen
- TQMDokument5 SeitenTQMsocyantotNoch keine Bewertungen
- Final Assessment For PortfolioDokument20 SeitenFinal Assessment For PortfolioLatchmi UdhoNoch keine Bewertungen
- Critical IncidentDokument11 SeitenCritical Incidentrumba2009Noch keine Bewertungen
- AssingmentnfdnDokument2 SeitenAssingmentnfdnapi-302133133Noch keine Bewertungen
- Revalidation Forms CombinedDokument12 SeitenRevalidation Forms CombinedG RobinsonNoch keine Bewertungen
- 3806NRS Nursing Assignment HelpDokument5 Seiten3806NRS Nursing Assignment HelpMarry WillsonNoch keine Bewertungen
- Seminar PresentationDokument31 SeitenSeminar Presentationapi-520940649Noch keine Bewertungen
- Quality Management and Performance A ReviewDokument19 SeitenQuality Management and Performance A ReviewIAEME PublicationNoch keine Bewertungen
- 17 Quality ManagementDokument45 Seiten17 Quality ManagementAbhishek MishraNoch keine Bewertungen
- NMC GuidelinesDokument28 SeitenNMC GuidelinesRazvannusNoch keine Bewertungen
- Information Package-Nursing Practicum I STUDENTDokument36 SeitenInformation Package-Nursing Practicum I STUDENTPui Pui LamNoch keine Bewertungen
- Introduction Quality ManuscriptDokument8 SeitenIntroduction Quality ManuscriptKristine Mae SampuangNoch keine Bewertungen
- Systematic Review PDSADokument11 SeitenSystematic Review PDSAMulyono Aba Athiya100% (1)
- 4.3: Quality Measures and Quality Gates: - Quality Gates Can Be Used To Improve TheDokument9 Seiten4.3: Quality Measures and Quality Gates: - Quality Gates Can Be Used To Improve TheVenkatesh PerumalNoch keine Bewertungen
- Decision Making LectureDokument24 SeitenDecision Making Lectureakram1978Noch keine Bewertungen
- Root Cause Analysis ToolsDokument15 SeitenRoot Cause Analysis ToolscmlimNoch keine Bewertungen
- Quality and Patient SafetyDokument19 SeitenQuality and Patient SafetyRekhaNoch keine Bewertungen
- L & M in Nursing - ConflictDokument26 SeitenL & M in Nursing - ConflictMichael SamaniegoNoch keine Bewertungen
- Six Sigma - A Case Study - Express Healthcare PDFDokument5 SeitenSix Sigma - A Case Study - Express Healthcare PDFmsulgadleNoch keine Bewertungen
- Chapter 1 Review of Basic Concepts of StatisticsDokument31 SeitenChapter 1 Review of Basic Concepts of StatisticsMarianie AvilaNoch keine Bewertungen
- Week 2 Reflection Journal - Chelsea PoligratisDokument2 SeitenWeek 2 Reflection Journal - Chelsea Poligratisapi-339668544Noch keine Bewertungen
- Hemodialysis Thesis - Analytical EssayDokument4 SeitenHemodialysis Thesis - Analytical EssayDianne LopezNoch keine Bewertungen
- Change InitiativeDokument7 SeitenChange InitiativeWajiha ShaikhNoch keine Bewertungen
- Implementation of (Plan-Do-Check-Act) Process of Quality and Measuring Its Effect On Nurses' Practice of Patient Safety GoalsDokument16 SeitenImplementation of (Plan-Do-Check-Act) Process of Quality and Measuring Its Effect On Nurses' Practice of Patient Safety GoalsVicennia SerlyNoch keine Bewertungen
- Mod2 - Ch3 - Health IndicatorsDokument13 SeitenMod2 - Ch3 - Health IndicatorsSara Sunabara100% (1)
- Data CollectionDokument30 SeitenData CollectionHarihara PuthiranNoch keine Bewertungen
- Artificial IntelligenceDokument8 SeitenArtificial IntelligenceKalluru Rajasekhar ReddyNoch keine Bewertungen
- An Introduction To Evidence-Based NursinDokument8 SeitenAn Introduction To Evidence-Based NursinAli MaqsudiNoch keine Bewertungen
- Differences Between Descriptive and Inferential StatisticsDokument1 SeiteDifferences Between Descriptive and Inferential StatisticsHaslindaNoch keine Bewertungen
- Risk Assessment For Pressure InjuryDokument34 SeitenRisk Assessment For Pressure InjuryNandarNoch keine Bewertungen
- Hsag Qapi CompanionDokument21 SeitenHsag Qapi CompanionAngel Inestroza100% (1)
- Clinical Reasoning QuestionsDokument8 SeitenClinical Reasoning Questionsvrasiah100% (1)
- Quality Management ME414Dokument67 SeitenQuality Management ME414نورالدين اعقاب عبدالسلام صالح0% (1)
- CHAPTER 1 - OUTLINE For QUALITY AND PERFORMANCE EXCELLENCEDokument7 SeitenCHAPTER 1 - OUTLINE For QUALITY AND PERFORMANCE EXCELLENCEKenedy FloresNoch keine Bewertungen
- Ai PosterDokument1 SeiteAi PosterLovekush KumarNoch keine Bewertungen
- Procurement of Supplies and Reagents.Dokument3 SeitenProcurement of Supplies and Reagents.Gretchel PontilarNoch keine Bewertungen
- Quantitative Research DesignDokument19 SeitenQuantitative Research DesignAli Ahmed GhouriNoch keine Bewertungen
- Public Health Mini-Guides - Alcohol Misuse - 1st Edition (2015)Dokument143 SeitenPublic Health Mini-Guides - Alcohol Misuse - 1st Edition (2015)Andrei Cristea100% (1)
- Conflict Management 2Dokument1 SeiteConflict Management 2Adeel AhmedNoch keine Bewertungen
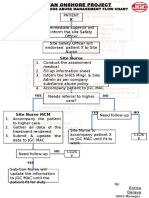
- Alcohol and Drug Abuse Flow ChartDokument1 SeiteAlcohol and Drug Abuse Flow Chartboen jaymeNoch keine Bewertungen
- Applied Nutrition Unit 01-1Dokument36 SeitenApplied Nutrition Unit 01-1Hira KhanNoch keine Bewertungen
- Juran's Quality TrilogyDokument2 SeitenJuran's Quality TrilogySuhail KhanNoch keine Bewertungen
- Microsoft Powerpoint - PB T.slide Phar Inv Adv-V0.4Dokument132 SeitenMicrosoft Powerpoint - PB T.slide Phar Inv Adv-V0.4raj_pegasusNoch keine Bewertungen
- NMBA Case Studies Code of Conduct For Nurses and Code of Conduct For MidwivesDokument7 SeitenNMBA Case Studies Code of Conduct For Nurses and Code of Conduct For Midwivestom doyleNoch keine Bewertungen
- The Investigation and Analysis of Critical Incidents and Adverse Events in HealthcareDokument162 SeitenThe Investigation and Analysis of Critical Incidents and Adverse Events in HealthcareBryan NguyenNoch keine Bewertungen
- Adherence TheoriesDokument6 SeitenAdherence TheoriesmakmgmNoch keine Bewertungen
- CPG Management of Type 2 Diabetes Mellitus (5th Edition) Special AFES Congress EditionDokument141 SeitenCPG Management of Type 2 Diabetes Mellitus (5th Edition) Special AFES Congress Editionkhangsiean89100% (1)
- Foundation Programme: Pharmaceutical Care Plan ChecklistDokument7 SeitenFoundation Programme: Pharmaceutical Care Plan ChecklistP D SpencerNoch keine Bewertungen
- WPC AssignmentDokument7 SeitenWPC AssignmentNarend GunnerNoch keine Bewertungen
- Smart Pill Reminder BoxDokument7 SeitenSmart Pill Reminder BoxIJARSCT JournalNoch keine Bewertungen
- Expanded HIV Pre-Exposure Prophylaxis PrEP ImplemeDokument11 SeitenExpanded HIV Pre-Exposure Prophylaxis PrEP ImplemeLuana MarinsNoch keine Bewertungen
- FNCP SampleDokument36 SeitenFNCP SampleLyka Milo AvilaNoch keine Bewertungen
- Therapeutics HandbookDokument49 SeitenTherapeutics Handbookaasdf100% (1)
- Effect of Whatsapp Reminder On Antenatal Care RevisitDokument11 SeitenEffect of Whatsapp Reminder On Antenatal Care RevisitElita NapiaNoch keine Bewertungen
- Psychological Aspects of Diabetes ManagementDokument2 SeitenPsychological Aspects of Diabetes ManagementsobanNoch keine Bewertungen
- Psychoeducational and Family Therapy in Relapse PreventionDokument4 SeitenPsychoeducational and Family Therapy in Relapse PreventionEdson HilárioNoch keine Bewertungen
- Ppa 11 221Dokument8 SeitenPpa 11 221Riska Resty WasitaNoch keine Bewertungen
- 10 Chaney Et Al 2004 A New Asthma Spacer Device To Improve ComplianceDokument8 Seiten10 Chaney Et Al 2004 A New Asthma Spacer Device To Improve ComplianceFrancis Gladstone-QuintupletNoch keine Bewertungen
- MCQS CPHQ 3Dokument329 SeitenMCQS CPHQ 3Ahmed Aborahma75% (4)
- Soto Et Al. 2015. An Ecological Perspective On Diabetes Self-Care Support, Self-Management Behaviors, and Hemoglobin A1C Among LatinosDokument10 SeitenSoto Et Al. 2015. An Ecological Perspective On Diabetes Self-Care Support, Self-Management Behaviors, and Hemoglobin A1C Among LatinosNatalia MocNoch keine Bewertungen
- PDF Hospital Training Report CompressDokument19 SeitenPDF Hospital Training Report CompressAdnan RAHATNoch keine Bewertungen
- CUHKMCDokument19 SeitenCUHKMCLam Chun YuNoch keine Bewertungen
- Appointment Letters Independent DirectorsDokument62 SeitenAppointment Letters Independent DirectorsArudra KumarNoch keine Bewertungen
- PharmacotherapyDokument15 SeitenPharmacotherapyPrincess RonsableNoch keine Bewertungen
- Doctor-Patient Relationship: Dr. Truong Trong Hoang, M.DDokument44 SeitenDoctor-Patient Relationship: Dr. Truong Trong Hoang, M.DQuỳnh NguyễnNoch keine Bewertungen
- DTC Training Course Session 10Dokument20 SeitenDTC Training Course Session 10drgroomNoch keine Bewertungen
- 2014 June - Makomba Games For Diabetic Children - Presentation at ILAMI Tel Aviv - Ofer Atzmon PDFDokument25 Seiten2014 June - Makomba Games For Diabetic Children - Presentation at ILAMI Tel Aviv - Ofer Atzmon PDFOfer AtzmonNoch keine Bewertungen
- Nurs FPX 4050 Assessment 3 Care Coordination Presentation To ColleaguesDokument6 SeitenNurs FPX 4050 Assessment 3 Care Coordination Presentation To Colleaguesfarwaamjad771Noch keine Bewertungen
- 89-Article Text-248-3-10-20191208Dokument16 Seiten89-Article Text-248-3-10-20191208Rizal MantovaniNoch keine Bewertungen
- To Study Drug Utilization and QoL in Patients With Bronchial AsthDokument89 SeitenTo Study Drug Utilization and QoL in Patients With Bronchial Asthomprakashcn9865Noch keine Bewertungen
- Cte STD Career PracticumDokument8 SeitenCte STD Career Practicumapi-307849917Noch keine Bewertungen
- Trans Accio NalDokument260 SeitenTrans Accio NalErick Maldonado HerreraNoch keine Bewertungen
- 08 - Oral and Sip FeedingDokument11 Seiten08 - Oral and Sip Feedingbocah_britpopNoch keine Bewertungen
- Ppa 299294 Adherence To Iron With Folic Acid Supplementation Among PregDokument9 SeitenPpa 299294 Adherence To Iron With Folic Acid Supplementation Among PregHailu DemekeNoch keine Bewertungen
- Metoprolol Teaching PlanDokument18 SeitenMetoprolol Teaching Planapi-419091662Noch keine Bewertungen
- FAMILY FUNCTION AND MEDICATION ADHERENCE IN PROLANIS PATIENTS IN PEKANBARU Rev 1Dokument16 SeitenFAMILY FUNCTION AND MEDICATION ADHERENCE IN PROLANIS PATIENTS IN PEKANBARU Rev 1fakhirahfitri217Noch keine Bewertungen
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (46)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4.5 von 5 Sternen4.5/5 (6)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingVon EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingBewertung: 1 von 5 Sternen1/5 (1)