Beruflich Dokumente
Kultur Dokumente
Pericardial Disease Questions
Hochgeladen von
api-277508327Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pericardial Disease Questions
Hochgeladen von
api-277508327Copyright:
Verfügbare Formate
Pericardial Disease Questions
Name: _Jennifer Pittman___________________
Date: __1/13/2014_______________
1. Name and describe the 2 main layers of the pericardium?
- Visceral (Continuous with epicardium)
- Parietal (thicker fibrous sac surrounding heart)
2. What is the normal amount of pericardial fluid?
- 5-10 mL
3. Describe the constraint of the pericardium and how alterations in the volume of
one chamber effects other chambers?
- The pericardium restrains the four chambers within a confined volume
and space, the total volume of the four chambers is limited and
alterations in the volume of one chamber must be reflected in an
opposite change in volume of another chamber.
4. How is a hemodynamic compromise related to pericardial fluid and why is this
relation important to understand as a sonographer?
- Accumulation of significant pericardial fluid reduces the total volume
that the 4 chambers can contain and may result in hemodynamic
deterioration related to under filling of the ventricles. Hemodynamic
compromise is related to elevated intrapericardial pressure, which is
related to the volume of pericardial fluid and the compliance or
distensibility of the pericardium.
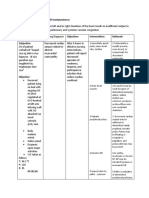
5. List the 7 etiologies of pericardial disease given in your text book. Table 10.1 page
241
- Idiopathic, infectious, inflammatory, post-myocardial infarction,
systemic dz, malignancy, miscellaneous
6. What is demonstrated in Figure 10.2 image A and image B?
- PAX view demonstrating a minimal pericardial effusion
7. According to your book, what 2 echo techniques are used to help detect pericardial
effusion?
- 2D and M-mode
8. Describe how a pericardial effusion would appear on M-mode.
- An echo-free space both anterior and posterior to the heart
9. According to your book, how is pericardial effusions characterized and quantified?
Pericardial Disease Questions
Minimal, small, moderate, large. Characterized as free circumferential
or loculated as well as the presence or absence of hemodynamic
compromise.
10.
Where should you be able to measure a pericardial effusion to document its
maximal size?
- Posterior atrioventricular groove
11.
Which views should you document a pericardial effusion in to demonstrate
its extent?
- PLAX, PSAX, Apical, subcoastal
12.
What is the cause of electric alterans seen on the EKG in the presence of a
large effusion? Use Figure 10.7 and reading from page 242
- There is no constraint of an inflammatory component, allowing the
heart to move freely.
13.
-
How are small, moderate, and large effusions described?
Small: 1 cm of posterior echo-free space, with or without fluid
accumulation elsewhere.
Moderate: 1 2 cm of posterior echo-free space
Large: more than 2 cm of maximal separation and the heart may swing
within the pericardial space
14.
True / False: In disease-free states, the normal pericardium is rarely
visualized with TEE or TTE modalities? Page 246
- True
15.
When is it possible for a TTE to determine the thickness of the pericardium?
Page 246
- When both pericardial and pleural effusions are present
16.
What are the echo findings in Figure 10-14 and what is the significance of the
measurement?
- Pericardial effusion and pleural effusion, the pericardium is visualized
and the thickness can be measured.
17.
What does the detection of stranding imply in the case of pericardial
effusion? View Figure 10.16 and 10.17
Pericardial Disease Questions
Inflammatory or possible hemorrhage or malignant etiology of the
pericardial effusion
18.
How is a pleural effusion differentiated from pericardial effusion in the
Parasternal views? Page 248
- Pleural effusion is an echo-free space posterior to the heart in the
supine or LLD position, located exclusively behind the left atrium and
-
posterior to the thoracic aorta.
Pericardial fluid surround the pulmonary veins, located anterior to the
aorta
19.
What effect does the pericardium have on the combined volume of the 4
cardiac chambers and why do you need to understand this as a sonographer? Page
248
- Respiratory variations in intrapericardial pressure results in linked
variation in filling of the right and left ventricle. Important to know so
you can detect an abnormality.
20.
Describe the normal response to intrathroacic and intrapericardial pressures
to INSPIRATION
- The pressures decrease. The result is to augment flow into the right
heart and reduce flow out of the pulmonary veins.
21.
Describe the normal response to intrathroacic and intrapericardial pressures
to EXPIRATION
- Pressure increases. The result is a mild decrease in right ventricular
diastolic filling and a subsequent increase in left ventricular filling.
22.
What does any process that results in increasing pressure variation with the
respiratory cycle leads to? Page249
- Cardiac Tamponade
23.
Describe the mechanism of a pathologic pulsus paradoxus as seen in cardiac
tamponade. Page 249
- During expiration when the right ventricular filling is impeded to a
greater degree, and there is a marked exaggeration in the respiratorydependent phasic changes in right and left ventricular stroke volume.
There is also a greater decrease in systolic arterial blood pressure with
inspiration.
Pericardial Disease Questions
24.
-
True or False: Cardiac tamponade is a clinical diagnosis.
True
25.
-
What is one of the earlier signs of tamponade?
A swinging heart detected on M-Mode.
26.
What is the mechanism of electrical alternans seen in large pericardial
effusions?
- The varying cardiac positions within the pericardium from beat to
beat, related to the EKG leads.
27.
-
List the more specific sonographic features (2) of tamponade.
Diastolic right ventricular outflow collapse
Exaggerated right atrial collapse during atrial systole.
28.
-
Which views is the right ventricle collapse best appreciated?
PLAX, PSAX, and occasionally in the apical 4 chamber
29.
-
Which view is the RA collapse best appreciated?
Subcostal or apical 4 chamber
30.
-
What does the images in Figure 10.23 A and B demonstrate?
Diastolic right ventricular collapse in M-mode with a posterior motion
of the anterior right ventricular wall in diastole. This patient has
evidence of a hemodynamic compromise.
31.
How can Pulsed Doppler of TV and MV inflow be used to help evaluate for
tamponade? Page 251 and Figures10.28
- It can used to show the inspiratory and expiratory phases. In the TV
inflow, there is augmented flow during inspiration and diminished flow
during expiration. The MV inflow has the opposite effect.
32.
33.
What is the classic form of pericardial constriction? Page 254
Calcification constriction secondary to tuberculous pericarditis
What is the more common reason for constrictive pericarditis in todays
practice?
- The result of infectious or inflammatory processes such as connective
tissue disease or radiation therapy or develops several years after
cardiac surgery.
Pericardial Disease Questions
34.
-
Anatomically, when does constriction occur?
When there is stiffening of the pericardium.
35.
-
What are two Echo features seen with constrictive pericarditis?
The pericardium forms a rigid shell in which the cardiac chambers are
encased.
Persistence of pericardium thickening during gradual dampening on Mmode through the posterior ventricular wall
Das könnte Ihnen auch gefallen
- Time TotalsDokument31 SeitenTime Totalsapi-277508327Noch keine Bewertungen
- Sdms CmecertificateDokument1 SeiteSdms Cmecertificateapi-277508327Noch keine Bewertungen
- Clinical Internship RecordsDokument3 SeitenClinical Internship Recordsapi-277508327Noch keine Bewertungen
- Sdms CmecertificateDokument1 SeiteSdms Cmecertificateapi-277508327Noch keine Bewertungen
- Pittman, Thyroid Written AssignmentDokument5 SeitenPittman, Thyroid Written Assignmentapi-277508327Noch keine Bewertungen
- Clinical Internship Record - CompsDokument3 SeitenClinical Internship Record - Compsapi-277508327Noch keine Bewertungen
- Final, Jennifer Pittman, LeaDokument9 SeitenFinal, Jennifer Pittman, Leaapi-277508327Noch keine Bewertungen
- Sdmsmembershipcert JenniferpittmanDokument1 SeiteSdmsmembershipcert Jenniferpittmanapi-277508327Noch keine Bewertungen
- Fall2014, Bilat Hydro Uvj, PittmanDokument10 SeitenFall2014, Bilat Hydro Uvj, Pittmanapi-277508327Noch keine Bewertungen
- Spine and Extremity PittmanDokument19 SeitenSpine and Extremity Pittmanapi-277508327Noch keine Bewertungen
- Fall 2014, Bilar Hydro, PittmanDokument20 SeitenFall 2014, Bilar Hydro, Pittmanapi-277508327Noch keine Bewertungen
- Jennifer Pittman ResumeDokument3 SeitenJennifer Pittman Resumeapi-277508327Noch keine Bewertungen
- 2nd Trimester Protocol r14Dokument9 Seiten2nd Trimester Protocol r14api-276847924Noch keine Bewertungen
- Adult Echocardiography Protocol 13Dokument10 SeitenAdult Echocardiography Protocol 13api-276847924Noch keine Bewertungen
- Abdomen Protocol 14Dokument8 SeitenAbdomen Protocol 14api-276847924Noch keine Bewertungen
- Lower Extremity Venous Protocol 14Dokument3 SeitenLower Extremity Venous Protocol 14api-276847924Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Monitoring of Critically Ill PatientDokument11 SeitenMonitoring of Critically Ill PatientAnusikta PandaNoch keine Bewertungen
- Managerial Business Analytics Mgt782 (Finished)Dokument22 SeitenManagerial Business Analytics Mgt782 (Finished)Eryn LisaNoch keine Bewertungen
- Q1 Periodic Test in Science 9Dokument4 SeitenQ1 Periodic Test in Science 9Jezha Mae NelmidaNoch keine Bewertungen
- Aj L3 CHD Qs & Ms Q1.: Diagram 1 Shows A Section Through The Heart. Diagram 1Dokument9 SeitenAj L3 CHD Qs & Ms Q1.: Diagram 1 Shows A Section Through The Heart. Diagram 1IntelaNoch keine Bewertungen
- Clinical Biochemistry: MSD Manual Veterinary ManualDokument5 SeitenClinical Biochemistry: MSD Manual Veterinary ManualDursa MiressaNoch keine Bewertungen
- Acute Coronary SyndromeDokument9 SeitenAcute Coronary Syndromekimchi girlNoch keine Bewertungen
- Code Sisrute 5Dokument41 SeitenCode Sisrute 5Bayu BimarthaNoch keine Bewertungen
- IJGMP - RV Function Assessment Pre and Post PTMC in Patients With Severe - AutosavedDokument8 SeitenIJGMP - RV Function Assessment Pre and Post PTMC in Patients With Severe - AutosavedImpact JournalsNoch keine Bewertungen
- Short Learning Topics On Biomedical Equipments by Heer Thoshani 22998Dokument55 SeitenShort Learning Topics On Biomedical Equipments by Heer Thoshani 22998Salim AloneNoch keine Bewertungen
- Course, Unit, Lesson Plan B.sc.n.ii SemDokument25 SeitenCourse, Unit, Lesson Plan B.sc.n.ii Semprachi jainNoch keine Bewertungen
- GRADE HandbookDokument75 SeitenGRADE HandbookEzequiel ZacañinoNoch keine Bewertungen
- CVD Statistics 2021 Chapter 1 Mortality FinalDokument80 SeitenCVD Statistics 2021 Chapter 1 Mortality FinalStoian SpasovNoch keine Bewertungen
- Chelliah2019 Article CardiovascularCTInCyanoticCong 210913 062234Dokument14 SeitenChelliah2019 Article CardiovascularCTInCyanoticCong 210913 062234Rika PutriNoch keine Bewertungen
- 7 - Spinal Column and Spinal Cord Injuries TestDokument3 Seiten7 - Spinal Column and Spinal Cord Injuries Testkamilkasim262Noch keine Bewertungen
- STEMIDokument34 SeitenSTEMIefendiNoch keine Bewertungen
- Hypertensive States at Pregnancy: Modern Methods of Classification, Diagnostics and TreatmentDokument73 SeitenHypertensive States at Pregnancy: Modern Methods of Classification, Diagnostics and TreatmentMuhammed ElnakibNoch keine Bewertungen
- Diver First Aid CPRDokument108 SeitenDiver First Aid CPREthanBrandtNoch keine Bewertungen
- Medical Terminologies and AbbreviationsDokument6 SeitenMedical Terminologies and AbbreviationsDapnie Ubalubao OcampoNoch keine Bewertungen
- CHF NCPDokument8 SeitenCHF NCPZy Hallasgo100% (1)
- Rheumatology - LupusDokument2 SeitenRheumatology - LupusFernando LoulaNoch keine Bewertungen
- Guideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementDokument26 SeitenGuideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementYo Me100% (1)
- Sirkulasi Pulmonal CharacteristicDokument21 SeitenSirkulasi Pulmonal CharacteristiclindaNoch keine Bewertungen
- Concept MapDokument4 SeitenConcept Mapdejosep_informaticsNoch keine Bewertungen
- A Cardiomyopathy PPT NEWDokument62 SeitenA Cardiomyopathy PPT NEWShetal Sharma100% (1)
- Cardiovascular NursingDokument30 SeitenCardiovascular NursingAnusha Verghese100% (3)
- Muscle Tissue DefinitionDokument3 SeitenMuscle Tissue DefinitionEleanor RamosNoch keine Bewertungen
- Biventricular Pacing For Atrioventricular Block and Systolic DysfunctionDokument9 SeitenBiventricular Pacing For Atrioventricular Block and Systolic DysfunctionRaul OrtegaNoch keine Bewertungen
- Post Op CareDokument21 SeitenPost Op Careahmadkhanmansoor09Noch keine Bewertungen
- Urine AnalysisDokument32 SeitenUrine AnalysisbnmjgcNoch keine Bewertungen
- Blood AnalysisDokument5 SeitenBlood AnalysisRiccardo PremoliNoch keine Bewertungen