Beruflich Dokumente
Kultur Dokumente
Think Safe
Hochgeladen von
api-279731052Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Think Safe
Hochgeladen von
api-279731052Copyright:
Verfügbare Formate
Think
SAFE
Four crucial elements for diabetes education
By Lucille Hughes, MSN/ED, RN, CDE
WHEN PATIENTS ARE discharged,
its often difficult to find the time to
provide proper education before they
leave your facility. Patients who are
newly diagnosed with diabetes need to
learn many new skills, including how
to monitor their blood glucose levels
and give themselves insulin injections
if needed. Yet theyre discharged in
less time than ever, and patients often
dont feel up to learning when theyre
feeling stressed, anxious, and wanting
to go home. So how can you make
sure your patients get proper diabetes
education before discharge?
Focusing on four crucial elements
of diabetes education will help you
give patients the information they
need to manage their diabetes when
theyre at home. This article describes
how to use the SAFE acronym to
improve your patients learning
experience.
The SAFE way
Using the acronym SAFE is an easy
way to remember the four crucial elements of diabetes education patients
need before discharge from an acute
care facility. (See Play it SAFE.)
Before you begin your patient
teaching, perform a learning needs
assessment and an assessment of the
patients readiness to learn. Results of
58 l Nursing2012 l January
www.Nursing2012.com
Copyright 2012 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
the learning needs assessment will tell
you two things: what your patient
already knows and what he or she
needs to know. Assessing the patients
readiness to learn helps you gauge
your patients ability and desire to
learn at this moment.1 Lets take a
look at each one.
Learning needs assessment: Assess
what your patient already knows.
Even newly diagnosed patients may
have some knowledge about their
disease. Make sure this knowledge is
current and applicable to their type of
diabetes. Ask open-ended questions
to assess your patients learning needs,
such as How does having diabetes
affect your life? or Tell me what
medications are you taking for
your diabetes, and how they work.
Observation is another important
assessment tool.1 If a patient requires
insulin but hasnt self-administered an
insulin injection or performed fingerstick blood glucose (FSBG) monitoring,
youve just identified two important
learning needs for your patient that
fall under the A and F of the
acronym SAFE.
Patients readiness to learn: At
times, you may be ready to teach
patients all the elements of SAFE
but theyre not ready to learn them.
In this situation, you may have to
prioritize which elements of the
SAFE acronym youll teach. For
example, you may only teach the
A and E. Ask questions to help
you assess your patients readiness
to learn, such as Would you like to
Play it SAFE
S Signs and symptoms of hypoglycemia and hyperglycemia as well as
management
A Administration of oral hypoglycemic
agents and/or insulin
F Finger-stick blood glucose monitoring
E Emergency numbers to call and
outpatient diabetes education
www.Nursing2012.com
Recognizing
hypoglycemia
Recognizing
hyperglycemia
Signs and symptoms of hypoglycemia
include:
dizziness
fast heartbeat
confusion
shaking
sweating
weakness
headache
passing out
getting very sleepy
seizures.4
Signs and symptoms of hyperglycemia
include:
high blood glucose
high levels of sugar in the urine
frequent urination
increased thirst.
Signs and symptoms of ketoacidosis
(very high blood glucose level thats
life threatening and requires immediate treatment) include:
shortness of breath
breath that smells fruity
nausea and vomiting
very dry mouth.2
learn some facts about your diabetes
self-management that can keep you
safe at home? or Are you interested in learning about the diabetes
medicine youll be taking at home?1
If your patient truly isnt ready to
learn, include additional diabetes
education material in the discharge
papers to be read at home.
Providing patients with a brightly
colored folder just for their diabetes
education material can be helpful. A
colorful folder will make it easy for
your patients to identify the diabetes
information from the sea of papers
they get at discharge. It may be quite
some time before your patient is
ready to read them, so make them
stand out from the rest.
Another helpful hint for situations when patients just arent ready
to learn would be to teach a family
member, spouse, child, parent, partner, or other caregiver. Ask patients if
theyre willing to give you permission
to teach someone close to them about
their diabetes treatment and ask the
patient who they would like that person to be. Be mindful of confidentiality issues and make sure patients give
you permission to discuss their care
with someone other than themselves.
S: Signs and symptoms
S stands for the signs and symptoms of
hypoglycemia and hyperglycemia as well
as their proper management. If your
patient is taking a sulfonylurea (such
as glipizide), a meglitinide (such as
repaglinide), or any kind of insulin,
provide education about the signs
and symptoms of hypoglycemia along
with the recommended treatment
options for a hypoglycemic episode
(see Recognizing hypoglycemia).2
Encourage patients to carry both a
blood glucose meter and appropriate
treatment options at all times. Let
them know about options that are
safe and reliable (see Oral treatment
options for hypoglycemia). Make sure
they understand that during a hypoglycemic episode, treatment must be
fast and appropriate.2-5
Teach patients that if they experience the signs and symptoms of
hypoglycemia, they need to check
their blood glucose levels to confirm.
(Youll show them how to use a
blood glucose monitor under F).
If the blood glucose level is less than
70 mg/dL, advise them to follow the
American Diabetes Associations
Rule of 15 (see Follow the rules).3,4
Tell patients that if they find themselves without a blood glucose
meter but are experiencing the signs
and symptoms of hypoglycemia, they
should follow the Rule of 15 just to
be safe.
January l Nursing2012 l 59
Copyright 2012 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Reinforce the importance of carrying a blood glucose monitor and
treatment options at all times. Remind
patients to stick to the guidelines
and eat 15 or 30 g of carbohydrate
depending on the blood glucose
reading.
Hyperglycemia, although not
considered an acute complication,
is a major cause of complications
associated with diabetes. Signs and
symptoms include a high blood glucose level, frequent urination, and
increased thirst (see Recognizing
hyperglycemia). Remind patients to
report these signs and symptoms to
their healthcare provider.6
Exercise is often used to lower
blood glucose levels. Advise patients
to check their urine for ketones if the
blood glucose level is above 240 mg/
dL. If ketones are present, exercise
should be avoided because ketones
may make blood glucose levels go
even higher. Advise patients to work
with their healthcare providers to find
the safest ways to lower blood glucose
levels.6
A: Administration
A stands for administration of oral
medications and/or insulin. Review
your patients prescribed medications.
Oral treatment options
for hypoglycemia
The following options contain 15 g of
carbohydrates:
4 oz (1/2 cup) of fruit juice
4 oz (1/2 cup) of regular (not diet)
soda
8 oz (1 cup) of milk
5 or 6 pieces of hard candy
2 tablespoons of raisins
4 teaspoons of sugar
1 tablespoon of honey or corn syrup
3 or 4 glucose tablets
1 serving of glucose gel.4,7
Provide printed materials to enhance
the learning process and provide
a reference when theyre at home.
Teach them the indication and
action of each medication. Let your
patients know which are best taken
with meals and review possible
adverse reactions, especially those
that have the potential to cause
hypoglycemia. Warn them not to
stop taking them on their own if
they experience adverse reactions. If
adverse reactions are troublesome,
they should contact their healthcare
provider for instructions.
Insulin analogues can cause hypoglycemia if not taken with enough
carbohydrate or if the patient skips a
Follow the rules
Teach your patients to follow the American Diabetes Associations Rule of 15
when their blood glucose level is low:
Eat or drink something with 15 g of carbohydrates.
Wait 15 minutes and recheck your blood glucose level.
If its still too low, eat another 15 g of carbohydrates and recheck your blood
glucose level after 15 minutes. Once your blood glucose level begins to move
into your target range, you should start to feel better.
Some patients overtreat themselves when their blood glucose level is low because
they treat the symptoms, not the blood glucose level. Even if you dont feel better
instantly after eating 15 g of carbohydrates, stick with the Rule of 15. If you keep
eating until you feel better, your blood glucose level may get too high too fast. Be
patient and wait the full 15 minutes.3
Let patients taking acarbose or miglitol know that only pure glucose (dextrose),
which is available in tablet or gel form, will raise their blood glucose level during a
low blood glucose episode. Food and drinks wont raise the blood glucose level fast
enough because these drugs slow the digestion of other carbohydrates.4
60 l Nursing2012 l January
meal. Let patients know this before
heading home and returning to their
usual meal plan and lifestyle.2
Before instructing patients about
insulin administration, ask the healthcare provider which delivery method
will be prescribed for use at home.
Have patients observe the insulin
administration process from start to
finish, following the specific manufacturers guidelines if an insulin pen is
prescribed.
After providing patients a few
opportunities to observe, have them
self-administer as you observe. This
same process holds true if theyre
going to use insulin vials and syringes
at home.
F: FSBG
F stands for FSBG monitoring. Performing an accurate finger-stick test
may be all you get to show your
patients before discharge. Learning
their personal target blood glucose
levels, when to check them, and
how to interpret the numbers can
be too much information for some
patients at discharge, but its important for them to know. Encourage
patients to learn at least the basics
of doing a finger stick and the general principles involved in using a
blood glucose monitor, especially
because the monitors they use at
home may not be the same ones
used in the hospital.
Before patients are discharged, let
them know what their target blood
glucose levels are and at what levels
they should call their healthcare provider.
E: Emergency numbers and
education
E stands for emergency numbers to
call and outpatient diabetes education.
Make sure your patients have the
phone number of their healthcare
provider in case blood glucose levels
get too high or too low. Encourage
www.Nursing2012.com
Copyright 2012 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
them to continue their education
about FSBG monitoring at a local
outpatient Diabetes Education Center. If youre not sure of one thats
close to where a patient lives, contact
the American Diabetes Association
(www.diabetes.org) or the American
Association of Diabetes Educators
(www.diabeteseducator.org). Instruct
them on when to call 911.
In the SAFE zone
Encouraging your patients to continue their diabetes education is a
lesson that will serve them long after
discharge. Even if you dont have the
time youd like to spend for proper
education, providing the crucial
elements of SAFE helps ensure that
your patients get the information
they need to manage their diabetes
at home.
REFERENCES
1. Moghissi ES, Korytkowski MT, DeNardo
M, et al. American Association of Clinical
Endocrinologists and American Diabetes
Association consensus statement on inpatient
glycemic control. Endocr Pract. 2009;15(4):
353-369.
2. Cryer PE. Hypoglycemia in Diabetes: Pathology,
Prevalence, and Prevention. Alexandria, VA:
American Diabetes Association; 2011.
3. American Diabetes Association. Hypoglycemia.
http://www.diabetes.org/living-with-diabetes/
parents-and-kids/planet-d/new-to-diabetes/
hypoglycemia.html.
4. American Diabetes Association. Living with
diabetes: hypoglycemia. http://www.diabetes.org/
living-with-diabetes/treatment-and-care/bloodglucose-control/hypoglycemia-low-blood.html.
5. National Diabetes Information Clearinghouse.
Hypoglycemia. http://diabetes.niddk.nih.gov/dm/
pubs/hypoglycemia/#treatment.
6. American Diabetes Association. Living with
diabetes: hyperglycemia. http://www.diabetes.org/
living-with-diabetes/treatment-and-care/bloodglucose-control/hyperglycemia.html.
7. Burkhart JA. Training nurses to be teachers. J
Contin Educ Nurs. 2008;39(11), 503-510.
Lucille Hughes is director of diabetes services at St.
Joseph Hospital in Bethpage, N.Y.
The author has disclosed that she has no financial
relationships related to this article.
DOI-10.1097/01.NURSE.0000406197.96182.bf
Your Primary Source for
Evidence-Based Healthcare Information
Personalize your
experience with
tools to export
and email
content, save
your searches,
view image
galleries and
most popular
articles, receive
RSS alerts, and
more
Full access to
archived issues
eAlert
Services
email
notifications
of eTocs,
citations,
collections,
and more
Online-Only
Journal
PACEsetterS covers all facets
of healthcare. This online-only
publications practical focus on
evidence utilization and its
unique, accessible style makes
it an ideal publication for both
managers and clinicians at
the point of care.
Official Journal of
The Joanna Briggs Institute
Download ePUB
articles to read on
most ereader devices
Subscribers can also access fulltext through the
Journals@LWW app available through the App Store
Mobile viewread full text
on the go on most internet
enabled mobile devices
To subscribe, call TOLL FREE
1-800-638-3030
or go to
www.JBIpacesetters.com
ABK147ZZ
www.Nursing2012.com
January l Nursing2012 l 61
Copyright 2012 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Specific Instuctions To BiddersDokument37 SeitenSpecific Instuctions To BiddersShahed Hussain100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- GMDSSDokument1 SeiteGMDSSRahul rajeshNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Synopsis SsDokument14 SeitenSynopsis SsJYOTI KATIYAR SVUNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Manual ML 1675 PDFDokument70 SeitenManual ML 1675 PDFSergio de BedoutNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Probset 3 KeyDokument7 SeitenProbset 3 KeyhoneyschuNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Splash25 Winner InstructionsDokument8 SeitenSplash25 Winner InstructionsRamkrishna PaulNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- P4 Science Topical Questions Term 1Dokument36 SeitenP4 Science Topical Questions Term 1Sean Liam0% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Subtotal Gastrectomy For Gastric CancerDokument15 SeitenSubtotal Gastrectomy For Gastric CancerRUBEN DARIO AGRESOTTNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Abhishek Parmar: Personal DetailsDokument2 SeitenAbhishek Parmar: Personal DetailsabhishekparmarNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The 100 Best Books For 1 Year Olds: Board Book HardcoverDokument17 SeitenThe 100 Best Books For 1 Year Olds: Board Book Hardcovernellie_74023951Noch keine Bewertungen
- Method Statement For Construction of Concrete Batching Plant (Combined)Dokument72 SeitenMethod Statement For Construction of Concrete Batching Plant (Combined)NP Dien100% (1)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- PresentationDokument6 SeitenPresentationVruchali ThakareNoch keine Bewertungen
- Richard IIIDokument36 SeitenRichard IIIXuan Mai Nguyen ThiNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- You'Re My Everything - Glenn FredlyDokument2 SeitenYou'Re My Everything - Glenn FredlyTommy Juliansyah MarsenoNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Datasheet Brahma (2023)Dokument8 SeitenDatasheet Brahma (2023)Edi ForexNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Ahu 1997 22 1 95Dokument15 SeitenAhu 1997 22 1 95Pasajera En TranceNoch keine Bewertungen
- The Frozen Path To EasthavenDokument48 SeitenThe Frozen Path To EasthavenDarwin Diaz HidalgoNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- NRNP PRAC 6665 and 6675 Focused SOAP Note ExemplarDokument6 SeitenNRNP PRAC 6665 and 6675 Focused SOAP Note ExemplarLogan ZaraNoch keine Bewertungen
- E WiLES 2021 - BroucherDokument1 SeiteE WiLES 2021 - BroucherAshish HingnekarNoch keine Bewertungen
- Elad Shapira - Shall We Play A Game - Lessons Learned While Playing CoreWars8086Dokument61 SeitenElad Shapira - Shall We Play A Game - Lessons Learned While Playing CoreWars8086james wrightNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Major Chnage at Tata TeaDokument36 SeitenMajor Chnage at Tata Teasheetaltandon100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Aloe Vera An Ancient Herb For Modern Dentistry-A LDokument7 SeitenAloe Vera An Ancient Herb For Modern Dentistry-A LRuth Ransel Yadao ValentinNoch keine Bewertungen
- LUNG ARTIFACTSreviewDokument13 SeitenLUNG ARTIFACTSreviewMayra ValderramaNoch keine Bewertungen
- GDCR - Second RevisedDokument290 SeitenGDCR - Second RevisedbhaveshbhoiNoch keine Bewertungen
- Cooperative LinuxDokument39 SeitenCooperative Linuxrajesh_124Noch keine Bewertungen
- Hypoglycemia After Gastric Bypass Surgery. Current Concepts and Controversies 2018Dokument12 SeitenHypoglycemia After Gastric Bypass Surgery. Current Concepts and Controversies 2018Rio RomaNoch keine Bewertungen
- JurnalDokument12 SeitenJurnalSandy Ronny PurbaNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Abbott 2021 ApJL 915 L5Dokument24 SeitenAbbott 2021 ApJL 915 L5Manju SanthakumariNoch keine Bewertungen
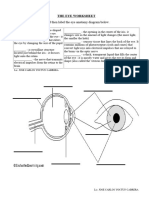
- The Eye WorksheetDokument3 SeitenThe Eye WorksheetCally ChewNoch keine Bewertungen
- Functions of The Gastrointestinal Organs: Muhammad ImranDokument21 SeitenFunctions of The Gastrointestinal Organs: Muhammad ImranSalman KhanNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)