Beruflich Dokumente
Kultur Dokumente
Addressing Cognition Poster 36x42
Hochgeladen von
api-262531856Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Addressing Cognition Poster 36x42
Hochgeladen von
api-262531856Copyright:
Verfügbare Formate
Addressing Meta-Cognition and Executive Function in Patients with
Traumatic and Acquired Brain Injury:
An Overview of Assessment and Treatment Approaches
Dani Goddard, OTS, CCLS
School of Occupational Therapy, Touro University Nevada, Henderson, Nevada, 89014
Abstract
Treatment Approaches
Evidence indicates that there are many
negative functional implications which can
result from acquired and traumatic brain
injury, especially when meta-cognition and
executive function are impacted. Decreased
deficit awareness and problems with
executive functioning may make a patient
unsafe to live or work independently even if
he or she appears functionally competent
while completing basic activities of daily
living.
Retrieved from http://www.nursingcenter.com/pdf.asp?AID=828299
While an in-depth chart review may provide
the therapist with a broad overview of what to
expect from the patient based on the injury
location and severity, further evaluation and
assessment is needed in order to identify
specific functional and cognitive deficits. It is
important for occupational therapists to
address basic cognition, insight and selfawareness, ADL and IADL functionality, and
community re-entry across the continuum of
care. All of these areas and their related
occupations can be greatly affected by metacognitive and executive functioning deficits in
patients with acquired and traumatic brain
injuries.
Treatment Progression
Screening Tools & Assessments
Basic Cognition:
Mini Mental State Examination (MMSE)
Montreal Cognitive Assessment (MoCA)
Trail-Making Test (oral version), COWAT
(letters F/A/S), & CLOX 1 & 2
FIM-Based Communication/Cognition
Screening
Insight & Self-Awareness:
Self-Awareness of Deficits Interview
(SADI)
Mayo-Portland Adaptability Inventory-4
(MPAI-4)
ADL- & IADL-Based Cognition:
Cognitive Screen for Grooming (CSG)
Executive Function Performance Test
(EFPT)
Community Re-Entry:
Multiple Errands Test (MET)
Site-specific and community-based
scavenger hunts
References (A Partial List)
In addition to these levels of treatment,
insight and self-awareness should be
assessed continuously to evaluate metacognition as the patient progresses.
Doig, E., Kuipers, P., Prescott, S., Cornwell, P., & Fleming, J. (2014).
Development of self-awareness after severe traumatic brain injury
through participation in occupation-based rehabilitation: Mixedmethods analysis of a case series. American Journal of Occupational
Therapy, 68(5), 578-588. doi: 10.5014/ajot.2014.010785
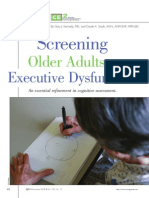
Kennedy, G. J., & Smyth, C. A. (2008). Screening older adults for
executive dysfunction. The American Journal of Nursing, 108(12), 6271. doi: 10.1097/01.naj.0000341886.15318.20
Task-Specific Training:
Occupationally/functionally based and meaningful, repetitive practice, spaced
retrieval of information (graded as memory improves), dual task training as
appropriate (increases divided attention and working memory)
Metacognitive Strategies:
Cognitive Orientation to Daily Occupational Performance (CO-OP Approach)
Goal, plan, do, check: planning should be facilitated by therapist; can use
COPM-based format to set goals
Predict and evaluate
Error-free Learning:
Break down the targeted task into small, discreet steps
Provide demonstration until patient is able to return demo properly
Encourage patient to avoid guessing and ask for assistance if needed
Correct errors immediately
Carefully fade prompts (verbal, tactile, and physical)
Chaining (forward, backward)
Sample Interventions
Create a memory book or daily log to help patients keep up with therapy sessions
(schedule, goals, interventions, and plans), visits from loved ones, or other events
Practice shopping online, paying bills; provide budgets and needed tools like a
balance register or calculator (or encourage patient to use tools on his/her phone)
Acquire a bus schedule/route map and plan a trip using public transit
Help the patient use social media, email, or text messages appropriately to
communicate with family and friends (or find online peer support groups)
Write a note or post card, address it, and send it in the mail
Print out a menu online, give the patient a budget, and have the patient choose a
meal (including beverage, appetizer, and dessert); have patient total amount and
calculate tip (ideally, take the patient out to a restaurant to practice first-hand)
Plan a meal, use the internet to search for a recipe, create a shopping list, then
cook the meal (have the patient do all steps except grocery shop, unless applicable)
Review home safety scenarios and emergency protocols
Play memory or categorization games such as Simon, Scattergories, or The Game
of Things (free online word category games are also available)
Use a map to plan a day trip or sequence outings
Learn how to use a navigation app on a cell phone or online for printed directions
Teach a novel sequence of exercises/steps to a task (patient return demonstrates)
Use newspaper or online resources to check weather, sports, or current events
Complete small fix-it tasks (i.e. install batteries and set a portable alarm clock)
Unload dishwasher and sort utensils/put away dishes in the proper place
Help patient set up medication sorter before discharge
Walk to a store to make a small purchase (book, magazine, snack, gift for a loved
one); set a budget beforehand and see if the patient can recall and follow limit
Utilize digital apps such as Lumosity, Flow Free, and Brew the Word to address
specific cognitive deficits; may also use apps to address memory, schedules, etc.
Das könnte Ihnen auch gefallen
- Rabideau Kitchen Eval AjotDokument8 SeitenRabideau Kitchen Eval Ajotapi-291380671Noch keine Bewertungen
- Reflection On Evidence-Based PracticeDokument2 SeitenReflection On Evidence-Based Practiceapi-262531856Noch keine Bewertungen
- Leadership Development PlanDokument5 SeitenLeadership Development Planapi-262531856Noch keine Bewertungen
- Cognitive Rehabilitation For Older AdultsDokument4 SeitenCognitive Rehabilitation For Older AdultsJosé Carlos Sánchez-RamirezNoch keine Bewertungen
- Cognitive Impairment Evaluation and ManagementDokument19 SeitenCognitive Impairment Evaluation and ManagementSAMUEL MARIN FUQUENENoch keine Bewertungen
- Fundies II Exam 1 Blue PrintDokument24 SeitenFundies II Exam 1 Blue PrintStephanieNoch keine Bewertungen
- Neuropsychological Assessment: Principles, Pearls and PerilsDokument8 SeitenNeuropsychological Assessment: Principles, Pearls and Perilsnellianeth orozco garciaNoch keine Bewertungen
- Plan de RehabilitaciónDokument5 SeitenPlan de RehabilitaciónJaime NevarezNoch keine Bewertungen
- Outcome MeasureDokument94 SeitenOutcome MeasureSylvia LoongNoch keine Bewertungen
- Occupational Therapy's Role in Adult Cognitive DisordersDokument2 SeitenOccupational Therapy's Role in Adult Cognitive DisordersThe American Occupational Therapy AssociationNoch keine Bewertungen
- NursingDokument61 SeitenNursingMrs Rehan50% (2)
- L3 Activity AnalysisDokument19 SeitenL3 Activity Analysispriyaa Ms balanNoch keine Bewertungen
- Key Words: Neuropsychological Evaluation, Standardized AssessmentDokument20 SeitenKey Words: Neuropsychological Evaluation, Standardized AssessmentRALUCA COSMINA BUDIANNoch keine Bewertungen
- Cat Evidence Table - FinalDokument31 SeitenCat Evidence Table - Finalapi-293258738Noch keine Bewertungen
- Hoppe and Matthews Cat Poster1Dokument1 SeiteHoppe and Matthews Cat Poster1api-238169773Noch keine Bewertungen
- Lehal Luis Evidence-Based Rationale 535Dokument11 SeitenLehal Luis Evidence-Based Rationale 535api-703558964Noch keine Bewertungen
- Nursing Care Plan - PPT HandoutDokument43 SeitenNursing Care Plan - PPT HandoutCharlie Abagon100% (2)
- CU02A WEEK02-NursingProcessinPMHNPractice28VAL2928129MODULEDokument8 SeitenCU02A WEEK02-NursingProcessinPMHNPractice28VAL2928129MODULEduca.danrainer02Noch keine Bewertungen
- Comunidad Salud MentlDokument4 SeitenComunidad Salud MentlRafael MezaNoch keine Bewertungen
- Care Plan - Arsenault 1031575Dokument10 SeitenCare Plan - Arsenault 1031575api-282962289100% (1)
- Chapter 06Dokument7 SeitenChapter 06loveteddybear0% (2)
- Steps of The Needs AssessmentDokument9 SeitenSteps of The Needs AssessmentPeter HuppiNoch keine Bewertungen
- 1 The Nursing ProcessDokument3 Seiten1 The Nursing ProcessStefany JoyNoch keine Bewertungen
- CognitiveDokument19 SeitenCognitiveLaila MajenumNoch keine Bewertungen
- NCM 114 Topic 4 Comprehensive Geriatric AssessmentDokument16 SeitenNCM 114 Topic 4 Comprehensive Geriatric AssessmentCaitlynNoch keine Bewertungen
- SR20518111615Dokument26 SeitenSR20518111615DrPreeti Thakur ChouhanNoch keine Bewertungen
- Module 2 JMDokument11 SeitenModule 2 JMJordan Abosama MamalumpongNoch keine Bewertungen
- Geria AssessmentDokument32 SeitenGeria AssessmentSteffi MurielNoch keine Bewertungen
- Nur 862 Clinical Competencies PortfolioDokument11 SeitenNur 862 Clinical Competencies Portfolioapi-457407182Noch keine Bewertungen
- Occupational Therapy Thesis TitlesDokument4 SeitenOccupational Therapy Thesis Titlesbk3q07k5100% (1)
- Improving Attention and Managing Attentional Problems (Sohlberg & Mateer) (2001)Dokument17 SeitenImproving Attention and Managing Attentional Problems (Sohlberg & Mateer) (2001)KILAMAZUKENoch keine Bewertungen
- Thinking Skills ExplainedDokument7 SeitenThinking Skills Explainedmr_jamzNoch keine Bewertungen
- SAS 2 Health Assessment LecDokument6 SeitenSAS 2 Health Assessment LecMove4Change PayatasNoch keine Bewertungen
- Nursing Process SOAPIEDokument33 SeitenNursing Process SOAPIEChoi Gong Ju100% (4)
- Research Article: Machine Learning For The Preliminary Diagnosis of DementiaDokument10 SeitenResearch Article: Machine Learning For The Preliminary Diagnosis of DementiaAyon DattaNoch keine Bewertungen
- Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Solutions ManualDokument16 SeitenHealth Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Solutions ManualJohnTaylortbios100% (9)
- Explain What Is Nursing and Relate Its Practice With Nursing ProcessDokument7 SeitenExplain What Is Nursing and Relate Its Practice With Nursing ProcessWac GunarathnaNoch keine Bewertungen
- Dwnload Full Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Solutions Manual PDFDokument35 SeitenDwnload Full Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Solutions Manual PDFlatifahhanhga7100% (10)
- Full Download Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Solutions ManualDokument35 SeitenFull Download Health Assessment and Physical Examination Australian and New Zealand Edition 2nd Edition Estes Solutions Manualzoism.waygoose.3fuhqv100% (30)
- Foundations Study Guide FINAL EXAMDokument15 SeitenFoundations Study Guide FINAL EXAMigorot89100% (1)
- Fall, 2018 - WK 4 Day 1&2 - OLG - Nursing Process (Assessment - Diagnosis) Revised For 4th EditionDokument11 SeitenFall, 2018 - WK 4 Day 1&2 - OLG - Nursing Process (Assessment - Diagnosis) Revised For 4th EditionmarieNoch keine Bewertungen
- PTH 870 - Interdisciplinary - Occupational TherapyDokument14 SeitenPTH 870 - Interdisciplinary - Occupational Therapyapi-551757456Noch keine Bewertungen
- AbstractDokument4 SeitenAbstractkhizarNoch keine Bewertungen
- Concept MappingDokument39 SeitenConcept MappingTob JurNoch keine Bewertungen
- Midwifery Skills Clinical Laboratory: The Midwives ProcessDokument26 SeitenMidwifery Skills Clinical Laboratory: The Midwives ProcessNano KaNoch keine Bewertungen
- The Nursing Process in Psychiatric/Mental Health Nursing: PlanningDokument49 SeitenThe Nursing Process in Psychiatric/Mental Health Nursing: PlanningJonalynCollodChewacheo50% (2)
- The Nursing ProcessDokument3 SeitenThe Nursing ProcessBianca Marithè RejanoNoch keine Bewertungen
- Comprehensive: Geriatric AssessmentDokument38 SeitenComprehensive: Geriatric AssessmentDingsNoch keine Bewertungen
- Chapter 5Dokument42 SeitenChapter 5peachypeachyNoch keine Bewertungen
- Restorative324234423 Techniques in Cognitive Rehabilitation Program Design and Clinical BenefitsDokument5 SeitenRestorative324234423 Techniques in Cognitive Rehabilitation Program Design and Clinical BenefitsRiNiNoch keine Bewertungen
- 2020.relationship Between Moral Distress, WorkplaceDokument1 Seite2020.relationship Between Moral Distress, WorkplaceFernandoCedroNoch keine Bewertungen
- And Utilization of Nursing ResourcesDokument10 SeitenAnd Utilization of Nursing ResourcesSimran ChauhanNoch keine Bewertungen
- Health Assessment 2Dokument12 SeitenHealth Assessment 2shannon c. lewisNoch keine Bewertungen
- CopyofcareerworksheetDokument4 SeitenCopyofcareerworksheetapi-335230100Noch keine Bewertungen
- Stroke Rehab Fact SheetDokument2 SeitenStroke Rehab Fact SheetHendra PrayogaNoch keine Bewertungen
- NURSING PROCESS LectureDokument56 SeitenNURSING PROCESS LectureSamantha SunglaoNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument10 SeitenNIH Public Access: Author ManuscriptjimakosjpNoch keine Bewertungen
- Employability Model and Career Paper AssignmentDokument5 SeitenEmployability Model and Career Paper Assignmentapi-581717268Noch keine Bewertungen
- Mosc Template Reflective Portfolio SubmissionDokument5 SeitenMosc Template Reflective Portfolio Submissiondoctor hausseNoch keine Bewertungen
- Nursing Process in Psychiatric NursingDokument14 SeitenNursing Process in Psychiatric NursingJomark Palgan100% (1)
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodVon EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNoch keine Bewertungen
- Resume With No Contact Info PubDokument2 SeitenResume With No Contact Info Pubapi-262531856Noch keine Bewertungen
- Addressing Cognition and Executive Function in Patients With Tbi & AbiDokument40 SeitenAddressing Cognition and Executive Function in Patients With Tbi & Abiapi-262531856Noch keine Bewertungen
- Research Day-Nidcap - Goddard & Noss 2015Dokument16 SeitenResearch Day-Nidcap - Goddard & Noss 2015api-262531856Noch keine Bewertungen
- HSH EvalDokument5 SeitenHSH Evalapi-262531856Noch keine Bewertungen
- Ncep EvalDokument4 SeitenNcep Evalapi-262531856Noch keine Bewertungen
- Occupational Profile & Intervention PlanDokument20 SeitenOccupational Profile & Intervention Planapi-262531856Noch keine Bewertungen
- Nidcap Poster Final Edited For Research DayDokument1 SeiteNidcap Poster Final Edited For Research Dayapi-262531856Noch keine Bewertungen
- Evaluating Executive Function in Older Adults ArticleDokument10 SeitenEvaluating Executive Function in Older Adults Articleapi-262531856Noch keine Bewertungen
- Vertigo and Balance TX ArticleDokument7 SeitenVertigo and Balance TX Articleapi-262531856Noch keine Bewertungen
- Home Evaluation Self-ReflectionDokument6 SeitenHome Evaluation Self-Reflectionapi-262531856Noch keine Bewertungen
- Occupational Profile & Intervention PlanDokument19 SeitenOccupational Profile & Intervention Planapi-262531856100% (1)
- Montano NCP TbiDokument6 SeitenMontano NCP TbiKarl Angelo MontanoNoch keine Bewertungen
- Synopsis de Addiction CenterDokument2 SeitenSynopsis de Addiction CenterNishana100% (1)
- Bipolar Manic Depression Chinese Medicine and AyurvedaDokument42 SeitenBipolar Manic Depression Chinese Medicine and AyurvedaRueth Annafeye100% (1)
- Impaired Oral Mucous Membranes - NCPDokument2 SeitenImpaired Oral Mucous Membranes - NCPXtianna Jade Doquila100% (1)
- Personal Hygiene: Didik S AtmojoDokument25 SeitenPersonal Hygiene: Didik S AtmojoRetno BeniNoch keine Bewertungen
- 1.3 Patients Assessment PolicyDokument6 Seiten1.3 Patients Assessment PolicySwati BajpaiNoch keine Bewertungen
- Oxytocin and Arginine Vasopressin - A Bridge Between Acupuncture and Autism Spectrum DisorderDokument6 SeitenOxytocin and Arginine Vasopressin - A Bridge Between Acupuncture and Autism Spectrum DisordersovalaxNoch keine Bewertungen
- Meralgia Paresthetica: A Review of The LiteratureDokument11 SeitenMeralgia Paresthetica: A Review of The LiteratureEileen Torres CerdaNoch keine Bewertungen
- Hypothesis ProblemsDokument7 SeitenHypothesis Problemsrj0% (1)
- DNR VDokument1 SeiteDNR Vquinn1696Noch keine Bewertungen
- CS URTIs BSN3AG3Dokument21 SeitenCS URTIs BSN3AG3GLORY MI SHANLEY CARUMBANoch keine Bewertungen
- MastoiditisDokument37 SeitenMastoiditisAkanksha EkkaNoch keine Bewertungen
- Acne RosaceaDokument28 SeitenAcne Rosaceanathy_soares100% (1)
- Documentation Techniques PDFDokument24 SeitenDocumentation Techniques PDFPooja varmaNoch keine Bewertungen
- Antihypertensive DrugsDokument64 SeitenAntihypertensive DrugsPSC100% (1)
- AT & Complicated GriefDokument4 SeitenAT & Complicated GriefCarolina BertaNoch keine Bewertungen
- Chaibasa Master Plan - 2040 Draft Report EnglishDokument241 SeitenChaibasa Master Plan - 2040 Draft Report EnglishArvind S.100% (3)
- SustanonDokument8 SeitenSustanonRamesh SubramanianNoch keine Bewertungen
- Common Cancers in WomenDokument27 SeitenCommon Cancers in Womensuha damagNoch keine Bewertungen
- Bar Screen: Aeration Tank Activated Sludge ProcessDokument15 SeitenBar Screen: Aeration Tank Activated Sludge ProcessBEn Kwan SimNoch keine Bewertungen
- WarfarinDokument10 SeitenWarfarinMar Ordanza100% (1)
- PSYCHOLOGYDokument5 SeitenPSYCHOLOGYHarvinder Sodhi SaraswatNoch keine Bewertungen
- Finalpaper SchnakeDokument6 SeitenFinalpaper Schnakeapi-315989347Noch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care PlanJoyce AnglubenNoch keine Bewertungen
- Monoclonal AntibodiesDokument35 SeitenMonoclonal Antibodiespreetylyall100% (5)
- 50 Bedded Private Hospital: Site Study, Structural Grid, Design Idea & ZoningDokument12 Seiten50 Bedded Private Hospital: Site Study, Structural Grid, Design Idea & ZoningHtoo Myat AungNoch keine Bewertungen
- Medicinal Chemistry: The Molecular Basis of Drug Discovery: Khan AcademyDokument17 SeitenMedicinal Chemistry: The Molecular Basis of Drug Discovery: Khan AcademyRinta MoonNoch keine Bewertungen
- 2005 - Stavridakis - Immediate Dentin Sealing of Onlay Preparations - Thickness of Pre-Cured Dentin Bonding Agent and Effect of Surface CleaningDokument11 Seiten2005 - Stavridakis - Immediate Dentin Sealing of Onlay Preparations - Thickness of Pre-Cured Dentin Bonding Agent and Effect of Surface CleaningAndreea BorislavschiNoch keine Bewertungen
- 04Dokument48 Seiten04Keith AmorNoch keine Bewertungen
- Facial Fillers Relevant Anatomy Injection TechniquDokument9 SeitenFacial Fillers Relevant Anatomy Injection TechniquMasoud Rahimi100% (1)