Beruflich Dokumente
Kultur Dokumente
Case Study548
Hochgeladen von
api-282190669Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Case Study548
Hochgeladen von
api-282190669Copyright:
Verfügbare Formate
Running Head: CIMT/STROKE CAMP
Case Study- Saginaw Valley State University: Constraint Induced Movement Therapy
(CIMT)/Stroke Camp
Heather Pantea
Saginaw Valley State University
OT 548
CIMT/STROKE CAMP
Pantea 1
Personal Data and History
Personal Data
The person of interest in this case study is a middle-aged male client who received
10 days of post-stroke treatment at Constraint Induce Movement Therapy (CIMT)/stroke
camp on the campus of Saginaw Valley State University. The client currently lived at
home with his wife and children. While he was not employed at the time, the client
reported that he had a career of over 30 years in the culinary industry. Although he relied
on his wife to provide financially, the client stated he was independent with his daily
routine at home. The client reported that he owned a Saeboflex splint for his affected
arm; however, he stated that he never uses it. His current daily routine included activities
such as preparing meals, watching TV, completing household related chores such as
folding laundry, playing with his children, and doing yard work. The clients current
hobbies included watching TV, making homemade wine, and collecting coins.
Medical History
Because of the short intake interview form and no access to previous health
records, there was not extensive information on the clients medical history. Other preexisint/current conditions the client had included type-II diabetes (non-insulin
dependent). After experiencing his stroke, the client received multiple therapies for
treatment. The client spent 1 month in the hospital recovering from the stroke; once
released, he received physical, occupational, and speech therapy for a total of 6 months.
The stroke affected the right side of his body, which also is the side his dominant hand is
CIMT/STROKE CAMP
Pantea 2
on. He stated that he did not currently experience any hemiplegic shoulder pain on his
affected right side.
In the history intake interview, the client stated that his motivations for
participating in the CIMT/stroke camp included a desire to become more adaptive in his
daily life and to see how far he can go with his current status. When asked what he
would like to gain for the next 10 days in therapy, his goals were to gain all the
movement that he could in order to use his right hand and arm more functionally. Turning
door handles with his right hand, folding towels with both hands, and brushing his hair
and teeth with his right hand were some of the activities he stated he would like to
improve his performance in.
Diagnosis
The client was accepted into the stroke treatment program based on predetermined criteria that included experiencing a cerebral vascular accident (CVA), also
known as stroke, more than 6 months ago.
Because of the setting, there were no formal health records to review the
diagnosis. Based on client statements, he client experienced a CVA more than 2 years
ago. When asked about the type of stroke, the client stated he experienced first a clot then
a bleed.
A CVA is defined as when a persons blood supply to his or her brain is disrupted
in some way and consequently the brain is deprived of vital nutrients and oxygen. When
this occurs, areas of brain tissue cannot function properly and are significantly damaged
or dies off altogether. Depending on where tissue dies off or is damaged, a persons
functioning may be impacted in numerous areas. These may include disturbances in
CIMT/STROKE CAMP
Pantea 3
sensation, issues with motor functioning, impairments with cognition and perception,
problems with vision, changes in personality and intellect, and various speech and
language disorders (Gillen, 2013).
The client in this case has issues with motor functioning on the right side of his
body, particularly his right upper extremity. There are also problems present with gait on
the right side; however, this was not focused on in the program. During participation in
the CIMT/stroke camp, the client did not appear to have any problems with cognition or
perception, intellect, or vision. There may still have been slight speech deficits as the
client was difficult to understand and exhibited slight slurred speech at times. Because a
relationship was not established prior to the stroke and there are no documents/reports or
statements from the family or client on changes in his personality, it cannot be assumed
that any occurred due to the CVA.
There are 3 different types of stroke that can be experienced: ischemic,
hemorrhagic, and transient ischemic attacks. The client in this case, based on history
intake, experienced an ischemic then a hemorrhagic CVA.
An ischemic CVA occurs when the blood flow to the brain is insufficient for the
bodys needs. Ischemic strokes may result from various sources, which include
embolisms in the blood stream, atrial fibrillation, acute myocardial infarction, and others.
While there are some risk factors that cannot be altered to try to avoid an ischemic stroke
(age, gender, heredity), there are many that can be controlled. Lowering blood pressure,
proper management of diabetes, diet, and exercise are just a few of the aspects that can be
managed and maintained (Gillen, 2013).
CIMT/STROKE CAMP
Pantea 4
The second type of CVA that the client experienced would be categorized as a
hemorrhagic stroke. A hemorrhagic CVA occurs in the subarachnoid or intracerebral areas
of the brain and involves bleeding in those specific areas. This bleeding can be a result of
problems that include spontaneous hemorrhaging of the lobes in the brain, arteriovenous
malformations, and rupturing of aneurysms (Gillen, 2013).
While a hemorrhagic CVA may not be very preventable, in this clients case the
initial stroke that he experienced (ischemic) might have been in various aspects of his
life. The client is currently a type-II diabetic; this condition is one of the identified risk
factors to manage to try and reduce the chance of sustaining an ischemic CVA. It should
not be assumed that the client does not properly take care of his type-II diabetes,
however, this condition should be a red-flag and priority in this clients case for
preventing additional strokes from happening. Other areas that may be of concern and
important to address for recurrent CVA prevention in this clients case may include
amount of stress, level of physical activity, and proper diet (Gillen, 2013).
Psychosocial Frame of Reference
The frames of reference that were selected for this client were that of the
behavioral frame of reference and the model of human occupation (MOHO). Because of
the time allotted in CIMT/stroke camp to work with the client one-on-one, treatment can
very much be client-centered and individualized to fit the clients wants and needs. These
chosen frames of references were used concurrently to ensure interventions chosen
directly related this particular client's case.
The behavioral frame of reference incorporates the use of activity to influence a
client's current performance skills and behaviors. By engaging in activities, clients can
CIMT/STROKE CAMP
Pantea 5
alter current behaviors and skills and learn new skills, strategies, and behaviors to include
in their daily life. This helped the client in this case by overcoming current problems he
faced, giving him strategies for potential future issues, and working on skills he desired to
improve (Bruce & Borg, 2002).
The second frame of reference used in this case will be the MOHO. The MOHO
focuses directly engagement in occupational activity. Because the belief with this model
is that participation in occupation will help to make a person's life meaningful and
purposeful, it is imperative to examine each individual client's life in terms of
experiences, occupations engaged in, and his or her skills and barriers that facilitate or
prevent participation. By doing this, the therapist can create intervention plans that apply
directly to the client's issues, desires, and needs. The MOHO was used for this client to
help give meaning and purpose to treatment, as well as keep him motivated and interested
in the 10-day/6 hour sessions of CIMT/stroke camp (Bruce & Borg, 2002).
Additional Frames of Reference Used
The biomechanical and rehabilitative frames of reference were also used with this
client. The biomechanical frame of reference addressed physical factors that were
impacted by the clients CVA, such as range of motion and strength necessary to
participate functionally in day to day activity (Earley, 2014).
The rehabilitative frame of reference was used to assist with the clients current
status through adaptations to work towards improved performance in various
occupations. These adaptations were done through strategies used to compensate for lost
function or using equipment designed to enhance performance (Earley, 2014).
Observation of Evaluative Elements (based on The Occupational Therapy Practice
Framework: Domain and Process, 3rd Edition)
CIMT/STROKE CAMP
Pantea 6
Domain-Occupations, Client Factors, Performance Skills, Performance Patterns, and
Contexts and Environments
Occupations
In the setting of the CIMT/stroke camp, there were many different factors that
needed to be taken into account to maximize success for each individual client in
treatment. The domain, one of the main components of the 3 rd edition of the Occupational
Therapy Practice Framework: Domain and Process, contains 5 aspects that should be
addressed with each client. These aspects include: occupations, client factors,
performance skills, performance patterns, and contexts and environments.
Based on the intake interview and observation on the first day, the client certainly
had areas of occupation that were affected by his current status. Activities of daily living
(ADLs) the client stated he could not use his right hand in functionally at home included
bathing/showering (washing hair), toilet hygiene, and personal hygiene (combing hair,
brushing teeth). On the first day during lunchtime, it was observed that the client also
displayed issues during meals. Because the client was unable to open and close his right
hand properly to pick up food or eating utensils (e.g. silverware), the activity of feeding
was also noted as a concern.
When discussing instrumental activities of daily living (IADLs), the client stated
that when he is in charge of meal preparation at home, he does not use his right hand
much, if at all. He also said that in the activities of driving and home management tasks
(i.e. folding laundry), he does not use his right hand.
Although the client was not currently working and had no plans on becoming
employed in the near future, his affected right upper extremity could potentially hinder
his full capacity to engage in work-related tasks. For example, if the client returned to
CIMT/STROKE CAMP
Pantea 7
work in the culinary industry, he would be unable to use his right hand to properly
prepare and cook food.
As for the occupations of play and leisure, the client discussed how he felt he
could not fully participate in the activities that he wanted to do with his family. He
reported how he experienced troubles when trying to play with his youngest child. For
example, he stated he was not able to pick up and animate his childs action figures with
his right hand. The client also reported that his kids had been asking him to go swimming
with them but explained how he hadnt because he felt he didnt have enough motion in
his right upper extremity to properly swim.
The occupations of rest and sleep and social participation were reported by the
client as not being affected. As for education, this occupation did not apply to the clients
case.
Client Factors
The second aspect that is addressed in the domain is that of client factors. The
first component of client factors includes the category of values, beliefs, and spirituality.
Through the intake interview as well as discussion throughout the CIMT/stroke camp, it
became apparent that the client highly valued his family and being a good husband and
father. The client also seemed to value being able to keep up on properly maintaining the
home environment for himself and his family, which may imply that this task has now
replaced his previous job of working in the culinary industry. The client did not seem to
present with any profound beliefs or specific spirituality characteristics.
The second main component of client factors is the multi-faceted area of body
functions. This aspect includes various functional areas within the human body. Many of
CIMT/STROKE CAMP
Pantea 8
these body functions of the client were evaluated through the use of assessments, which
will be discussed in detail in an upcoming section of this study. Areas that were
specifically evaluated with this client included mental, sensory, neuromusculoskeletal and
movement related, and muscle and movement functions.
The mental function assessment that was used evaluated the patients cognitive
level in areas such as memory, attention, and judgment. Although the assessment did not
specifically address these factors, consciousness and orientation (global mental functions)
could also be considered as indirectly assessed.
In the sensory area, assessments looked at aspects that included level of pain,
discerning light touch, and proprioception. Functions such as taste and smell were not
assessed with this client.
Neuromusculoskeletal and movement related functions were examined by
assessing and evaluating joint mobility, specifically range of motion of certain joints.
Lastly, the clients muscle and movement functions were assessed and evaluated.
Factors such as muscle power, tone, endurance, and control of voluntary movement were
tested. Although not formally evaluated, it was observed that the client did display a stiff
gait pattern (specifically the right leg and foot) when walking.
The final component of client factors is body structures, which looks at the
various physical structures of the client. Other than apparent problems such as increased
muscle tone in the affected upper right extremity, there did not seem to be any significant
problems with any of the clients structures. This was determined through observation
and discussion with the client. If a significant issue was suspected, medical testing and
CIMT/STROKE CAMP
Pantea 9
consultation by other professions (e.g. physician) would be required to further investigate
the potential problem.
Performance Skills
Another area encompassed in the domain includes that of performance skills.
There are 3 overarching categories within this aspect, which are motor, process, and
social interaction skills. While motor skills can be directly evaluated through use of
assessments, these were also observed throughout the duration of the 10-day program.
The client worked on improving many skills in his right upper extremity, which included
but were not limited to manipulation, proper movement, endurance, grip, and
coordination.
Although process skills were not as highly emphasized with this client, there were
still important skills that were observed and worked on in the CIMT/stroke camp. These
included skills such as pacing, handling, and adjusting.
The last category of skills, social interaction, was not the main focus of treatment.
All in all, the client was polite and displayed proper communication with the facilitators,
therapists, and other clients of the 10 day program. Although the client expressed
emotional frustration to the therapist at times in treatment, he did so in ways that were
socially appropriate and/or extensive therapeutic intervention was not needed.
Performance Patterns
This area of the domain looks at performance patterns on an individual basis or
within a group or population. On an individual basis, the client did not demonstrate any
habits or rituals that he regularly participated in. What was significant about this area is
the roles the client holds, 2 overarching roles which include being a husband and a father.
CIMT/STROKE CAMP
Pantea 10
Other roles that may be of significance in this clients case are that of a homemaker/home
maintainer in place of his previous role as a working member of the culinary industry for
over 30 years. In a group, particularly the CIMT/stroke camp, the client did not seem to
hold any specific roles or initiate or participate in any ritualistic behavior. As for routines,
the client participated in typical and appropriate social behaviors such as greeting other
clients of the CIMT/stroke camp each morning.
Context and Environment
The last aspect of the domain is the contexts and environments of the client.
In the cultural facet of context, the client did not demonstrate any remarkable cultural
customs or beliefs. His personal context included him being a middle-aged man who is
currently unemployed. While he did not indicate his socioeconomic status, he did not
allude to or state any concerns that this status had changed due to relying on his wifes
job for the main source of income. The clients educational status included a high school
diploma, as well as specialized training for a career in the culinary industry. The client
reported no memberships to any organizations, clubs, etc. His temporal context was
unclear in the aspect of how long he has been unemployed for, as he did not indicate this
at any time during CIMT/stroke camp. Due to the length of his culinary career and his
stroke occurring only a little over 2 years ago, the client may have not have experienced
very much time being unemployed. Based on his history intake and discussion, the client
has been in the roles of a father and husband for many years. The only indicator of a
virtual context for this client was his personal cell phone, which he used to show pictures
of his family to the therapist, as well as take pictures of treatment modalities used for him
in CIMT/stroke camp. The client stated that he also used his cell phone to call his family
CIMT/STROKE CAMP
Pantea 11
to update them on his progress during the 10-day program since he was not able to
commute from his home each day due to distance.
As for environments, there are two main areas examined. These include the
physical and social environments. In the clients physical treatment environment, the
Health and Human Services (HHS) building on the campus of Saginaw Valley State
University was the main area that encompassed the many spaces utilized for intervention.
These spaces included the rehabilitation lab classroom, the pediatric lab classroom, the
ADL suite, case study suites, the movement analysis lab (MAL), and the grassy area right
outside of the HHS building. Per the clients report, his home in rural Michigan was the
main physical environment he seemed to do the most activity in. The social environment
for this client during the program consisted of the camp facilitators, therapists, and other
clients of the CIMT/stroke camp. In terms of other social environments, the client seemed
to mainly interact with members of his family. Other possible social environments
outside of family for this client may include medical/health professionals he sees for
other treatment for his affected right upper and lower extremity.
Process-Evaluation, Intervention, and Targeted Outcomes
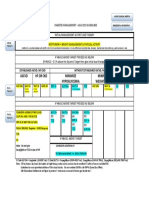
Evaluation: Occupational Profile and Analysis of Occupational Performance
Another main component of the framework is the process, which contains the
evaluation, intervention, and targeted outcomes. These should be addressed with each
client in every case. To complete the occupational profile portion of the process, an intake
interview was conducted with this client on the first day of the program to gather
background information, past medical history, and personal factors (e.g. interests, support
system, daily routines, etc.) Once this interview was completed, analysis of occupational
performance began. This analysis was done through four main assessments, which
CIMT/STROKE CAMP
Pantea 12
included: the Wolf Motor Function Test, the Motor Activity Log (for the upper
extremity), the Modified Fugl-Meyer Evaluation of Physical Performance, and the St.
Louis University Mental Status (SLUMS). These assessments were chosen by facilitators
of the CIMT/stroke camp as the best method to gather pertinent information on each
client. Results of each initial assessment for this particular client can be viewed in the
appropriate appendix with the exception of the SLUMS as facilitators of the camp kept
this assessment.
The Wolf Motor Function Test assessment (Appendix A) tested and measured
many motor abilities of the upper extremity in functional tasks. Motor aspects that were
assessed included abduction, extension, external rotation, flexion, grasp, grip, pinching,
lifting, and strength.
The Motor Activity Log (Appendix B) was used to determine what tasks and daily
activities the client participates in and identify problem areas. Common every-day tasks
and activities are focused on in this assessment, such as opening a refrigerator door,
buttoning a shirt, and getting out of a car.
The Modified Fugl-Meyer Evaluation of Physical Performance (Appendix C)
assessed many areas of the client. These areas included range of motion and manual
muscle testing of the upper extremities, testing of light touch and proprioception,
Brunnstrom stage level, the 9-Hole Peg Test for fine motor coordination, testing of the
three functional pinches (tripod, lateral, and pad to pad), testing of grip strength with the
Jamar dynamometer, and assessing levels of pain.
CIMT/STROKE CAMP
Pantea 13
Although results of this assessment are not available to view, the SLUMS was
used to evaluate different areas of the clients cognition, which included aspects such as
memory and problem solving skills.
Intervention: Plan, Implementation, and Review
Once initial evaluations have been completed, the next step of the process is to
move into the area of intervention. A plan must first be devised collaboratively by the
client and the therapist based on results of the initial evaluation assessments as well as the
goals of the client. All the previous information in the domain gathered from the client
must also be taken into account when planning interventions.
Because there was around 6 hours of treatment time per day at the CIMT/stroke
camp, the plan continuously changed each time the client and therapist met based on
observations from the previous session, client input and discussion, and group activities
that were being put on each day. However, there was one constant that remained in the
plan with this client. The therapist began each session of the program with at least an
hour of warm-up preparation activity for the client, which will be discussed more in
detail later on in this study.
Similar to the plan, interventions that were implemented depended on each
specific day of the CIMT/stroke camp. Types of intervention used varied greatly and
those that were used included occupation-based activities, activities gauged towards the
clients current performance skills and patterns and improving those that are affected by
his condition, group activities, education, training, and preparatory methods and tasks. To
build a healthy client-therapist relationship and establish and maintain rapport,
therapeutic use of self was also used by the therapist. These intervention selections will
be discussed in greater detail later on in this study.
CIMT/STROKE CAMP
Pantea 14
The final step of the intervention portion of the process is that of reviewing.
Before each daily session ended in the CIMT/stroke camp, the therapist and client would
set aside time to discuss treatment strategies chosen for that day and how those strategies
were being used to work towards the clients goals and targeted outcomes. The client was
asked what activities he would like to engage in or work on in the next session, as well as
to give feedback on interventions that had already been implemented. At times, reviewing
took place while engaging in an intervention to communicate the importance of the
chosen treatment or if the client did not understand the significance of the intervention.
Reviewing of interventions was continuous throughout the program and modifications
were made in the plan and implementation stages as necessary.
Targeted Outcomes
The final factor in the process component of the framework is targeted outcomes.
Before particular interventions are planned and implemented, the therapist and client
identify areas or issues to work on in therapy as well as choose evaluative methods or
assessments that will effectively measure outcomes of treatment. The client and therapist
should also work together to create goals for the client to try to attain through
engagement in therapy. These goals should also be measurable, clear, and concise in
order to track the clients progress towards these goals during intervention and determine
when they have been accomplished. Goals determined for this client will be discussed in
detail later on in this study. Measures that were chosen to obtain outcome results mostly
reflected the previously chosen assessments for initial evaluation, which were the Wolf
Motor Function Test, the Motor Activity Log, and the Modified Fugl-Meyer Evaluation
of Physical Performance. Additionally, all clients of the CIMT/stroke camp participated
in a focus group discussion on the last day of the program. Clients were also given take-
CIMT/STROKE CAMP
Pantea 15
home questions on the program the second to last day of the program by the facilitators.
These take-home questions were used exculsively by the faciliators to gather information
on the success of the CIMT/stroke camp.
It is also important to not only determine outcomes and evaluative methods to
measure end results, but also to effectively and efficiently track progress throughout
intervention towards these targeted outcomes. This was done by individual discussion
with the client each session to gain feedback, as well as a review of the clients journal
log at the beginning of each day. This journals purpose was to track the clients activity
after leaving CIMT/stroke camp for the day, mini-milestones reached out of the therapy
environment, and any other important thoughts or feelings experienced by the client. The
journal was also used as a tool to help the therapist include and plan for certain activities
within treatment. Observation by the therapist was used to track progress, as well as
advice and suggestions made by other therapists and the facilitators in the CIMT/stroke
camp. Additionally, volumeter measurements were taken of the right hand to measure
edema and track the effectiveness/progress of the use of a treatment modality to reduce
this edema.
Types of Occupational Therapy Interventions
In this clients case, a number of different occupational therapy interventions were
used to work towards improved results within the CIMT/stroke camp. Although the client
did not meet criteria to wear a constraint-mitt for CIMT, a collaborative decision was
made by facilitators and the therapist to have the client try and wear the constraint
throughout the duration of the program. The purpose of the constraint was to hinder and
restrict use of the unaffected left upper extremity and promote/force use of the affected
right upper extremity (Earley, 2005). The client was instructed to wear the constraint as
CIMT/STROKE CAMP
Pantea 16
much as possible in and out of therapy, only being allowed to take the mitt off during
activities that included toileting and bathing hygiene, driving, and sleeping or only if it
interfered with full participation in an activity/casued a safety issue. Because the
constraint did not pose a safety threat during mobility in this individual case, the client
was encouraged to wear the mitt when walking.
To start each treatment session, the therapist would implement preparatory
methods (warm-up activities) to help prepare the client for the day. These methods
included functional movements of the scapula, passive range of motion (PROM), and
stretching of the affected right upper extremity, which were all done by the therapist.
Facilitative techniques (e.g. vibration), moist heat, neuromuscular electrical stimulation,
and kinesiotaping (to reduce edema) of the affected upper extremity were included as
well among the different modalities and techniques used in preparatory methods. Icing,
PROM, and stretching were among methods used at the end of each session as a cooldown for the client. Additionally, a specially configured splint was made for the client by
some of the facilitators in the program to increase participation in the group activity game
of corn hole. Although the client possessed an expensive splint for his affected arm made
by the company Saeboflex and modeled it for the therapists, facilitators, and other
members of the CIMT/stroke camp, he did not want to use it to participate in any of the
activities in treatment.
Preparatory tasks were also used in intervention with this client. Tasks that were
included were use of pegboards, practicing self-Affolter (hand-over-hand) technique with
various objects, weight bearing exercises, place and hold exercises of the right upper
extremity, pinching and rolling theraputty for fine motor purposes, bilateral rowing, self-
CIMT/STROKE CAMP
Pantea 17
range of motion (SROM) and active range of motion (AROM), exercises, and use of the
BTE simulator to simulate various activities, such as arm movements in swimming. Tasks
were not limited to previous tasks listed, as there were other additional preparatory tasks
that were used for this client throughout the duration of the CIMT/stroke camp.
Activities (both occupation based not occupation based) that related directly to the
clients case were included in this clients case to help keep treatment client-centered.
Occupations that were focused on included handwriting, kitchen and cooking tasks,
laundry tasks with and without an occupation-based kit, coin collecting and sorting tasks
with the use of an occupation-based kit. Non-occupation based activities included the use
of various games and tasks, such as scavenger hunts, giant checkers, the board game
Guess Who? and many others. These activities worked on different skills such as
pinching and grasping, hand and finger manipulation, and functional movement.
Group activities were also a large portion of intervention within the CIMT/stroke
camp. Group activity not only allowed the clients to get to know one another and have
fun, but also helped to build a sense of supportive community with each other, the
therapists, and facilitators. These activities worked on many of the same skills and issues
(e.g. functional motor movements) that were focused in other types of interventions.
Group activities included corn hole tournaments, preparing lunch together, card games, a
washer-tossing game, and croquet.
The last type of intervention used with this client were that of education and
training. The client received a home program/packet at the end of the 10 day program,
which included treatment interventions and activities used in CIMT/stroke camp, a
picture and step-by-step handout of the kinesiotaping pattern used for edema in his
CIMT/STROKE CAMP
Pantea 18
affected right upper extremity, a word-key for unfamiliar terms and acronyms, a handout
on therapeutic heating and icing, copies of handwriting exercises the client completed,
and a handout that tracked timed trials of folding various laundry items. The client also
received information and training from the therapist and a facilitator on how to safely use
neuromuscular electrical stimulation units and where to purchase one for use at home.
Throughout the duration of the CIMT/stroke camp, the therapist utilized
therapeutic use of self by being personable (being positive and encouraging to the client),
showing empathy (allowing client to express and discuss his frustrations), and offering
advice and insights in the course of treatment.
Activity and Occupational Demands
When deciding upon what interventions to use with a client, it is important to
consider the activity and occupational demands of each intervention. It is up to the
therapist to ensure that these demands allow for the client to have a therapeutic
experience
when
participating
in
treatment.
Demands
are
centered
around
relevance/importance to the individual client, objects used for the activity, physical area
needed to participate, social elements included in the activity, sequencing and timing,
required actions and performance skills to participate, and lastly required body functions
and structures for participation. Depending upon the activity, these demands would
change.
Because of the large number of activities that were used with this client in
intervention, only one activity will be discussed in detail for activity and occupational
demands. The activity to be discussed focuses on the task of folding various laundry
items in one treatment session.
CIMT/STROKE CAMP
Pantea 19
While folding laundry may not seem very important to many people, in this
client's case it was one of the main household tasks he was in charge of. The client was
very adamant on improving his skills with his right hand in this activity, specifically
being able to grab and pinch laundry items to help himself fold. This task was also the
focus of one of the two occupation-based kits made for this client. All in all, working on
folding different laundry items reflected importance and relativity to this client's case.
Objects that were used with this activity included a flat surface (in this case, a
table top surface was used) and laundry items which included a pillow case, bath towel,
hand towel, pants, and a long-sleeved shirt. The client was given the option to use a chair
to sit and fold these items but he declined and preferred to stand while engaging in this
activity. A timer, paper, and writing utensil were used by the therapist. These particular
objects were used with this task to time the client on how long he took to fold each item
properly and neatly, which were both based on his standards of proper and neat.
To fully engage in this activity, not much space was required. The activity took
place in the pediatric lab classroom with adequate temperature and lighting. There was a
moderate level of noise due to other CIMT/stroke camp clients, therapists, and
facilitators; however, it did not interfere with the activity.
Because the client stated he often folds laundry on his own at home, there were no
required social demands for this activity. The therapist interacted with the client during
this activity to start and stop time, offer encouragement during engagement, and to
discuss the activity with the client upon completion.
Since items that needed to be folded differed from one another and the client had
his own way of folding, there was no particular order or steps that needed to be followed
CIMT/STROKE CAMP
Pantea 20
in order for this activity to take place. The element of time came into play by timing the
client for each individual item that needed to be folded. Individual times for each item
varied depending on ease or difficulty the client experienced during folding. Altogether,
the duration of folding these items lasted approximately 20 minutes total.
Actions and performance skills that were required to participate in this particular
activity required motor skills included but are not limited to stabilizing laundry items to
be folded on the table, coordinating movements of the upper extremities to fold, and
properly manipulating the textile material/laundry items. Process skills that were
necessary included handling the material, proper pacing, and making adjustments with
items as needed. Because the client stated he did this task on his own, social interaction
skills were not focused on.
Body functions that were necessary to engage in this activity included being
awake and conscious, attentiveness, perception, adequate visual and tactile senses, upper
extremity mobility, voluntary movement, and adequate muscle power and tone. Although
the client had spastic tone and diminished strength in his right upper extremity, he was
still able to participate in this activity and work on improving his skills with his affected
arm. The client possessed the necessary body structures (e.g. fingers, hands, arms, etc.) to
engage in the task of folding laundry.
Intervention Approaches
There are a number of approaches a therapist can employ when it comes to
intervention. Many of these approaches were used in this particular client's case in order
to work towards targeted outcomes and goals, give meaning and purpose to treatment,
and to include the client's interests, desires, and needs.
CIMT/STROKE CAMP
Pantea 21
Approaches that were used with this client included establishing/restoring of skills
(e.g. worked on restoring movement, coordination, and strength to the affected upper
extremity), modification (e.g. creation of a splint to be able to better perform and engage
in the game of corn hole), creating/promoting (e.g. giving the client a home-program to
continue progress), and prevention (e.g. therapeutic icing to reduce additional edema or
swelling caused by participation in activity at the CIMT/stroke camp).
Types of Outcomes
The final section of the framework to be discussed within this study involves the
types of outcomes that come as a result of treatment. For this particular client, outcomes
were measured by the previously mentioned assessments used for initial evaluation.
Results of these assessments can be seen in each proper appendix.
Wolf Motor Function Test-Post Treatment (Appendix D)
Motor Activity Log-Post Treatment (Appendix E)
Modified Fugl-Meyer Evaluation of Physical Performance- Post
Treatment (Appendix F)
The types of outcomes that were seen in this client's case included improvement
and enhancement in occupational performance, improvements in his quality of life,
increased participation, more confidence in his daily roles, and an overall improved
feeling with his well-being.
Improvement and enhancement in occupational performance was tracked by
keeping records of the client's performance over time. For example, handwriting
improvements were captured by keeping a log of the client's shapes and words he
practiced writing. This log was organized by date and included the actual handwriting
worksheets of the client with notes on what writing utensils were used, trial numbers, and
the amount of time the client took per trial. The client also discussed areas in which he
CIMT/STROKE CAMP
Pantea 22
felt improvements in both with the therapist and in the large focus group at the end of the
CIMT/stroke camp.
While the client's quality of life was not directly measurable, the client openly
discussed (both in private with the therapist and in focus group discussion) how he felt
this 10-day program had improved various areas of his life. In the focus group, he stated
how just only a short time ago he struggled picking up his child's action figures and
playing with his son using his affected upper extremity. He went on to say how he was
now able to pick up an action figure and while that seemed like a small feat, he was
happy he felt he had improved his status enough to better engage with his family. He also
discussed how he felt more confident in participating in activities with his affected arm
that included brushing his teeth, folding laundry, and writing.
All throughout the CIMT/stroke camp, the client was cooperative and open to
participating in many activities with his affected right upper extremity. However, the
client would not automatically use his right arm for certain activities and needed
encouragement from the therapist to try to use it. One of these activities was eating lunch.
The first day of CIMT/stroke, the therapist prompted the client to try to use his right hand
to feed himself. While the client did try, it was challenging, difficult, and messy for him.
This caused him to become frustrated and he asked to revert back to using his unaffected
arm to finish his meal. With practice and further positive reinforcement throughout the
treatment program, the client began to have better control over his affected upper
extremity when feeding himself. Towards the end of the program, the client would use his
right arm almost entirely to feed himself during lunch. Consequently, he was able to
CIMT/STROKE CAMP
Pantea 23
improve his participation in the activity of feeding by being able to use his right upper
extremity effectively.
The outcome of increased role competence was identified through statements
made directly by the client in individual and group discussion. As previously stated, the
client felt he improved his skills for engaging in laundry tasks. Because of this, he felt he
was able to contribute to his family by being able to engage and complete this home
maintenance activity successfully. He also felt because there were improvements made in
his physical status is terms of functional movement, he would be more able to fully
participate in activities with his family in his role as a father and a husband.
The last outcome noted for this client included an improved feeling with wellbeing. In discussion (both group and with the therapist), the client said he was excited
about the improvements that he has made and that these improvements motivated him to
further his progress. He stated that he felt more confident with using his affected upper
extremity and because of his positive experience in the CIMT/stroke camp, he was
willing to participate in more stroke-related treatment groups at Saginaw Valley State
University if the opportunity ever arose.
Pharmacological Assessment and Impact on Therapeutic Intervention
In the intake interview, the client reported that he currently takes 3 medications on
a regular basis. These medications included Metformin, Atorvastatin, and over-thecounter aspirin.
Metformin
This medication is taken orally on a regular daily basis and is used to treat those
affected by type-II diabetes to help control levels of blood sugar. Metformin may be taken
CIMT/STROKE CAMP
Pantea 24
on its own or in combination with other medications to treat type-II diabetes. This
medication should not be used by those who are allergic to Metformin or who are in a
state of what is known as diabetic ketoacidosis (insufficient insulin production to convert
sugar into usable energy in the body). Conditions such as liver disease or having a history
of heart disease should be discussed with a physician before taking Metformin. There are
uncomfortable side effects that may develop such as headache, diarrhea, nausea, etc., but
these may disappear as the clients body adjusts to the medication. What is important to
remember that with Metformin there is a heightened risk of developing condition called
lactic acidosis, which may be life-threatening if left untreated. This build-up of lactic acid
in the body can first cause symptoms that may include muscle pain/weakness, flu-like
symptoms, swelling or rapid weight gain, as well as others. More severe symptoms can
develop as time progresses and if left untreated. Medical help should be sought if any of
symptoms of lactic acidosis are experienced (Metformin drugs.com, 2014).
While there were no issues that occurred in treatment, experiencing
uncomfortable symptoms of this medication may have affected the clients cooperation in
participation in intervention activities. Also, if the client was experiencing symptoms of
lactic acidosis and proper medical authorities had not been contacted (i.e. client was
unaware of condition, therapists in treatment were not alerted, etc.), this could have
jeopardized the clients current health status and caused further setbacks. Based on the
information given for this medication, there were no apparent contraindications to any
modalities or activities used in treatment.
Atorvastatin
CIMT/STROKE CAMP
Pantea 25
This medication is also taken orally on a daily basis. Atorvastatin is used to treat
high cholesterol (reducing bad levels of cholesterol while raising good levels), as well
as lower the risk of stroke, heart attack, and other heart complications in those with
conditions such as type-II diabetes and coronary heart disease. Those who are currently
pregnant, have liver disease, or experience an allergic reaction to this medication should
not use Atorvastatin. There may be mild side effects experienced such as mild muscle
pain, diarrhea, or nausea and these symptoms may disappear as the client adjusts to the
medication. It is important to remember that with this medication (in very rare cases) a
condition may result in which skeletal muscle tissue is broken down in the body and
leads to kidney failure. A physician should be consulted to evaluate individual risk and
discuss any other medications being taken currently that may increase the risk for this
condition to develop. Another interesting and important factor to remember when taking
this medication is that grapefruit (both the fruit and juice) in the clients diet should be
considered to be reduced or eliminated, as it is believed to cause dangerous interactions
with Atorvastatin. Lastly, the physician should be alerted to any other medications being
taken to avoid undesirable or dangerous drug interactions (Atorvastatin, 2014).
Again, while there were no problems that occurred within treatment,
uncomfortable side effects of the medication might have affected the clients cooperation
and motivation to participate in intervention activities. The serious condition of skeletal
muscle tissue breakdown did not seem to be present at any time during the 10 days of the
CIMT/stroke camp. However, if the client had experienced symptoms of this condition
and did not seek or receive the proper care, this could have caused a negative change in
his health status and created further setbacks in treatment. Again, based on the given
CIMT/STROKE CAMP
Pantea 26
information for this medication, no treatment modalities or activities for intervention
were contraindicated.
Over-the-counter aspirin
Aspirin is a commonly used over-the-counter drug for reducing symptoms of
pain, fever, and/or inflammation. While it is used for ailments such as fever or headaches,
it can also be used for preventative purposes for conditions such as heart attack and
stroke. While this medication is generally safe to use, there are some important aspects
that need to be considered. Those who have had an allergic reaction to aspirin should not
use it, as well as those who recently experienced stomach or intestinal bleeding, those
who have bleeding disorders, or are allergic to non-steroidal anti-inflammatory drugs
(NSAIDs). A physician should be consulted to evaluate individual risk with certain
conditions (i.e. gout, asthma, etc.) while using this medication. Aspirin should not be
used by those who are breastfeeding. Those who plan on becoming pregnant or who are
pregnant and use this medication should consult a physician to reduce dangerous effects
on the unborn baby. Mild side effects may occur such as an upset stomach or drowsiness
but these should alleviate as the body becomes adjusted to the medication (if aspirin is
used as a daily regimen). A physician should also be alerted to other medications being
taken, as certain medications can interact with aspirin and cause bruising and bleeding
more easily and other safety issues. Taking ibuprofen concurrently with this medication
may also reduce the effectiveness of aspirin; this should be avoided if possible (Aspirin,
2014).
In this clients case, the aspirin being taken did not cause any concern for
interference with treatment. Potentially, if mild side effects were experienced, this may
CIMT/STROKE CAMP
Pantea 27
have affected the clients willingness to participate if he was experiencing discomfort.
Once again, based on the information given for the medication, there are no treatment
activities or modalities that were contraindicated for use.
Summary of Pharmacological Assessment
It is important to remember that while the 3 previously discussed medications are
used to maintain and manage certain conditions, they are not meant to be as the end-all
solution for the client. The client should ensure that in addition to adhering to proper
medication management, he should also incorporate exercise, proper diet, and healthy
habits into his lifestyle that will work to help prevent another CVA.
Treatment Plan
Assets/Strengths
Motivated and cooperative
Open to ideas for treatment
Independent in daily routine
No sensory or proprioceptive deficits
Personal splint (Saeboflex) that assists with functional movement
No pain in affected area/pain does not affect activity
Concerns/Weaknesses
Decreased range of motion in the right upper extremity in scapular elevation,
shoulder flexion, abduction, and external and internal rotation, elbow flexion and
extension, wrist flexion and extension, finger extension and flexion (both of the
PIP and MP joints), and forearm pronation and supination
Decreased strength in the right upper extremity in shoulder flexion, extension,
abduction, and adduction, elbow flexion and extension, wrist flexion and
extension, and digital grasp
Decreased fine motor coordination in the right upper extremity
Decreased functional pinch strength in the right upper extremity
CIMT/STROKE CAMP
Pantea 28
Decreased grip strength in the right upper extremity
Decreased participation in activity (e.g. opening door handles, personal hygiene,
etc.) with the right upper extremity; right arm only is used to help participate at
times
Short Term Goal (goal identified by client)
The client will improve range of motion in elbow flexion and extension each by
10 degrees so that he may be better able to fold laundry items with his right upper
extremity within 10 sessions.
Long Term Goal
The client will complete the task of brushing his hair independently in the time
frame of 5 minutes using his right upper extremity with a standard comb or brush within
3 months.
Current Treatment Methods/Interventions
In the case of this client, he received many different treatment methods within the
10 sessions at CIMT/stroke camp. Because of the large amount of methods used with this
client, not all treatments chosen will be named in this study. Interventions included
education on reflex-inhibiting patterns (RIPs) with pillow positioning, use of constraint
on unaffected hand, weight bearing with and without an air splint, scapular mobilization,
use of the BTE work simulator, place and hold exercises, stretching, range of motion
exercises (active, self, and passive), therapeutic heating and icing, neuromuscualar
electrical stimulation, use of associated reactions, facilitative techniques (e.g. vibration
and tapping), group activities such as playing corn hole or with cards, occupational
activities such as folding laundry or cooking lunch, and many others. Although the client
did not originally meet the criteria for CIMT, a constraint was still used to promote use of
CIMT/STROKE CAMP
Pantea 29
his affected upper extremity. Along with the constraint and the other various treatment
methods, activities and occupations that reflected meaning and purpose to the client were
also used to identify and work on skills that had been consequently affected by his
affected right upper extremity.
Methods for treatment in the CIMT/stroke camp were chosen by therapists in the
CIMT/stroke camp. However, one particular facilitator (an occupational therapist and
doctor of occupational therapy at the university) influenced and guided treatment choices
as he had substantial experience with a CIMT/stroke camp program before. In an article
written by this facilitator and his colleagues, many of the treatment methods that were
used in this CIMT/stroke camp (e.g. occupation-based activities, preparatory methods,
etc.) were also used in a similar program which produced results that included improved
function in the affected arm of the client (Earley, Herlache, and Skelton, 2010). Based on
this expertise, CIMT-protocols, and interventions available at the program site, these
treatment methods were included in treatment for this client.
The treatment methods chosen worked towards the clients short term goal by
engaging the affected extremity in movement and working on skills that affected the
clients performance in daily activity, such as being able to use his right arm to fold
laundry items. Through use of these various interventions, the client worked on multiple
issues from his problem list such as range of motion, strength, and coordination, which
then in turn affected/improved his performance abilities in activity.
Recommended Treatment Methods/Interventions
Although the client received a home program that included all of the interventions
used in the CIMT/stroke camp and was educated on how he could do these at home, it
CIMT/STROKE CAMP
Pantea 30
may be recommended for the client to continue receiving occupational therapy services to
further progress with his affected upper extremity. In an article written by Trombly and
Ma (2002), those who experienced a stroke and received occupational therapy services
had improved in areas of participation and engagement of activity afterwards. Even
though the clients stroke is not recent, he still suffers from deficits and issues caused by
his post-stroke status. Continuation of occupational therapy services may help to further
ameliorate these deficits and improve skills for functional performance in activity, such
as reaching his long term goal of being able to comb his hair independently. However,
this may not be possible if the client cannot afford treatment (e.g. paying out of pocket)
or if his health insurance will not pay for it. In this case, it would be imperative for the
client to use his home program (written by occupational therapists and based on
occupational therapy interventions) on a regular basis to continue progressing with his
affected upper extremity.
It would also be recommended for the client to use adaptive equipment in some
areas to assist him in performing the activity or task properly. Although the client has
demonstrated that he does not prefer the use of adaptive equipment, his Saeboflex splint
as well as other equipment (e.g. built-up handles to assist with grasp) would be beneficial
in his case by helping him to engage in activity more easily. As stated by Kraskowsky
and Finlayson (2011), using adaptive equipment can assist by prevent any further deficits
in a clients health status and helps to promote engagement in occupation. Additional
education on how adaptive equipment may be helpful in the clients daily routine and
improve his quality of life may be necessary for the client to consider using any
equipment in a regular basis.
CIMT/STROKE CAMP
Pantea 31
Other Services Involved and Referrals Recommended
In the case of this client, no major or potential problems were presented with the
client's home environment or his mental/psychological status. Therefore, services would
most likely not be needed in these areas at this time. However, because the client has to
deal with his pre-existing condition of diabetes and with current deficits due to his stroke,
he may be at risk for developing depression. The client and his family should monitor for
symptoms and seek counseling or psychological intervention he does start to exhibit signs
of depression.
Although the client was currently unemployed and relied on his wife to provide
financially, this did not seem to be a concern for him. More information would need to be
gathered from the family, specifically the wife, in order to determine if proper financial
services are needed.
A referral that may be beneficial for this client would be for physical therapy
services. Because the client seemed to have issues with his gait and his right lower
extremity, physical therapy would be recommended in this case to help improve these
areas.
To help the client broaden his social circle and manage his current health
conditions, support programs for his diabetes and post-stroke status might be
recommended for this client. By participating in a diabetes support group, the client could
participate in social interaction outside his home as well as maintain and possibly learn
new strategies to healthily manage his condition (e.g. learning about healthy recipes to
cook). A support group centered around stroke survivors may also benefit the client by
motivating him to continue improving and being able to cope with his current status.
CIMT/STROKE CAMP
Pantea 32
Another benefit may perhaps include creating new friendships and having a sense of
community by providing and receiving support from other members of the stroke group.
Psychological and Social Factors and Impact on Therapeutic Intervention
The client did not exhibit any remarkable psychological factors during the 10-day
program. However, he did display moments of frustration, exhibited by swearing under
his breath or making statements such as, 'how is this helping me?' Also, the client seemed
to have some unrealistic expectations at first about improvements that would be made
through the CIMT/stroke camp, such as seeing leaps and bounds in terms of range of
motion and functional movement. While this did not hinder further treatment,
encouragement, discussion, and motivation were given by the therapist in order to
address and work through what the client was experiencing.
Because the client did not live close to Saginaw Valley State University, he had to
make accommodations for himself to stay the 10 days of the CIMT/stroke camp. Based
on conversations with the client, his family seemed to be very important to him. During
the camp, there were other clients who were able to have family members be there
throughout the each day with them. The client may have experienced additional
emotional hardship due to the fact that he did not have his family physically there to
support him while other clients did.
The client did experience significant fatigue during participation in the program.
Because of the length of each session and constantly participating in physical
intervention, this was draining to some of the clients involved in the program. The client
stated a few times throughout the CIMT/stroke camp that after each session ended for the
day, he would go and take a nap. His exhaustion that he experienced may have somewhat
CIMT/STROKE CAMP
Pantea 33
impacted him from being able to engage and fully participate in all therapeutic activities
every single session.
Lastly, the client rejected many times to use any adaptive equipment. Although he
had gone to great lengths to obtain his Saeboflex splint, he stated he did not feel like
using it to help his affected arm at all. When offered various types of equipment, the
client would almost always not use it (with the exception of the corn hole splint.) While it
was not discussed in detail with the client, he seemed to feel that in his case adaptive
equipment was not necessary for him to engage in various activities.
Discharge/Transition Plan
The client was successfully discharged from the CIMT/stroke camp with a home
program to use to continue his progress. Upon discharge, the client stated he would return
home to his family and daily routine. It is imperative that once the client returns home, he
should maintain his health status (through home program, medication management,
proper lifestyle choices, etc.) to help prevent a recurrent stroke and other health issues,
such as problems with his diabetes. If the client does not properly take care of his health
or the client experiences a significant health issue due to his pre-existing conditions, this
could cause setbacks or create new problems for him. Support from the clients family
will be necessary to help the client continue progress and maintain his health. Although
the clients family was not able to be there physically for the CIMT/stroke, the client
stated that his family is very supportive and would help him continue with progressing
his status.
Conclusion
CIMT/STROKE CAMP
Pantea 34
After the client was discharged, no additional contact took place between the
therapist and client. The client gave contact information to facilitators if any additional
post-stroke programs would be planned to take place at Saginaw Valley State University.
References
American Occupational Therapy Association. (2014). Occupational therapy practice
framework: Domain and process (3rd edition). American Journal of
Occupational Therapy, 68 (Suppl. 1), S1-S48.
<http://dx.doi.org/105014/ajot.2014.682006>
Aspirin. Drugs.com (2000-2014).
<http://www.drugs.com/aspirin.html>
CIMT/STROKE CAMP
Pantea 35
Atorvastatin. Drugs.com. (2000-2014).
<http://www.drugs.com/atorvastatin.html>
Bruce, M. & Borg, B. (2002). Psychosocial frames of reference: Core for occupational
based practice (3rd ed.). Thorofare, NJ: Slack Inc.
Earley, Donald. (2005). Course Wookbook: Constraint-Induced Movement Therapy
for Rehabilitation of Stroke Patients. Cross Country Education, Inc.
Earley, Donald. (February 4th, 2014). Frames of Reference. OT 520 Class Winter 2014.
Lecture conducted from Saginaw Valley State University at University Center,
MI.
Earley, D., Herlache, E., & Skelton, D. R. (2010). Case ReportUse of occupations and
activities in a modified constraint induced movement therapy program: A
musicians triumphs over chronic hemiparesis from stroke. American Journal of
Occupational Therapy, 64, 735744.
Gillen, Glen (2013). Cerebrovascular Accident/Stroke. In Pendleton and Schultz- Krohn
(Ed.). Pedrettis Occupational Therapy: Practice Skills for Physical
Dysfunction, 7th Edition (pg. 844-880). St. Louis, MO: Elsevier Mosby.
Kraskowsky, L.H., & Finlayson, M. (2001). Factors affecting older adults use of
adaptive equipment: Review of the literature. American Journal of Occupational
Therapy, 55, 303-310.
Metformin. Drugs.com. (2000-2014).
<http://www.drugs.com/metformin.html>
Trombly, C. A., & Ma, H. (2002). A synthesis of the effects of occupational therapy for
persons with stroke, part I: Restoration of roles, tasks, and activities. American
Journal of Occupational Therapy, 56, 250259.
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Numeracy Trainee HandoutDokument11 SeitenNumeracy Trainee HandoutoladapoNoch keine Bewertungen
- Mono Dual Triple Therapy DiabetesDokument1 SeiteMono Dual Triple Therapy DiabetesbharatNoch keine Bewertungen
- Januvia-Janumet June 24 2010.Ppt FinalDokument32 SeitenJanuvia-Janumet June 24 2010.Ppt Finaldrnasim200881710% (1)
- Ting Ming Yew p18090781Dokument9 SeitenTing Ming Yew p18090781Ming Yew TingNoch keine Bewertungen
- Galvus: Name of The MedicineDokument19 SeitenGalvus: Name of The MedicinevrtzioNoch keine Bewertungen
- Promethazine Hydrochloride Tablets 25mg Usp - Taj Pharma, Leaflet Patient Medication InformationDokument3 SeitenPromethazine Hydrochloride Tablets 25mg Usp - Taj Pharma, Leaflet Patient Medication InformationTAJ PHARMA — A Health Care ProviderNoch keine Bewertungen
- MTP2022Dokument333 SeitenMTP2022ABDULJWAD HADDAD100% (1)
- Laporan PBLDokument12 SeitenLaporan PBLLuna MiraNoch keine Bewertungen
- Diabetes Acog 2017Dokument15 SeitenDiabetes Acog 2017Holger Vicente Guerrero Guerrero100% (1)
- Makalah FarmakoepidemiologiDokument24 SeitenMakalah FarmakoepidemiologiAkbar NugrahaNoch keine Bewertungen
- Amaryl M PI - May 2018marylDokument11 SeitenAmaryl M PI - May 2018marylvicky upretiNoch keine Bewertungen
- Interaction of Metformin and Nifedipine in Type II Diabetic Patients With HypertensionDokument5 SeitenInteraction of Metformin and Nifedipine in Type II Diabetic Patients With HypertensionAndi PermanaNoch keine Bewertungen
- Ada 2015 Summary PDFDokument41 SeitenAda 2015 Summary PDFcuambyahooNoch keine Bewertungen
- Glucocorticoid-Induced Diabetes Mellitus: An Important But Overlooked ProblemDokument10 SeitenGlucocorticoid-Induced Diabetes Mellitus: An Important But Overlooked ProblemRengganis PutriNoch keine Bewertungen
- Patent Application Publication (10) Pub. No.: US 2010/0323011 A1Dokument15 SeitenPatent Application Publication (10) Pub. No.: US 2010/0323011 A1salman afzalNoch keine Bewertungen
- GLYBURIDEDokument3 SeitenGLYBURIDEJohn Carlo SamsonNoch keine Bewertungen
- Anc 1Dokument128 SeitenAnc 1Naila OmerNoch keine Bewertungen
- PCOS Guidelines 1Dokument14 SeitenPCOS Guidelines 1Angelie Therese ChuaNoch keine Bewertungen
- Sample Questions For HAAD, Prometric and DHA For NursesDokument23 SeitenSample Questions For HAAD, Prometric and DHA For Nurseskichoo185% (97)
- Passmedicine MRCP Mcqs-Clinical Pharmacology and ToxicologyDokument135 SeitenPassmedicine MRCP Mcqs-Clinical Pharmacology and ToxicologyHashim Ahmad100% (1)
- Formulation and Evaluation of Transdermal Patch of Metformin HydrochlorideDokument4 SeitenFormulation and Evaluation of Transdermal Patch of Metformin HydrochlorideAnonymous izrFWiQNoch keine Bewertungen
- OLD-Effect of Hibiscus Rosa Sinensis On Blood SugarDokument30 SeitenOLD-Effect of Hibiscus Rosa Sinensis On Blood SugarKryscel Czarinah100% (1)
- Pancreatic AdenocarcinomaDokument19 SeitenPancreatic AdenocarcinomaKarla Alejandra Torres Rangel100% (1)
- AAFP Diabetes MedicationsDokument7 SeitenAAFP Diabetes MedicationsThaysa LimaNoch keine Bewertungen
- Drug CardsDokument187 SeitenDrug Cardsintaaf82% (33)
- Diabetes Mellitus CPGDokument157 SeitenDiabetes Mellitus CPGejikieru03100% (3)
- Tableau Antidiabetiques 2018 enDokument1 SeiteTableau Antidiabetiques 2018 enpraefatioNoch keine Bewertungen
- Metformin Tablet 500mg (Metformin Hydrochloride) Dynapharm (M) 1apr2014 EngDokument3 SeitenMetformin Tablet 500mg (Metformin Hydrochloride) Dynapharm (M) 1apr2014 EngWei Hang100% (1)
- Vildagliptin: The Evidence For Its Place in The Treatment of Type 2 Diabetes MellitusDokument18 SeitenVildagliptin: The Evidence For Its Place in The Treatment of Type 2 Diabetes Mellitusp k agarwalNoch keine Bewertungen
- Ebook The Ai Revolution in Medicine GPT 4 and Beyond PDF Full Chapter PDFDokument67 SeitenEbook The Ai Revolution in Medicine GPT 4 and Beyond PDF Full Chapter PDFdorothy.cook305100% (23)