Beruflich Dokumente
Kultur Dokumente
Medication Safety Paper Amber
Hochgeladen von
api-283066063Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Medication Safety Paper Amber
Hochgeladen von
api-283066063Copyright:
Verfügbare Formate
1
Running head: Medication Safety
Medication Safety
Amber Morin
University of South Florida
Medication Safety
The prevalence of medication errors is astounding. On average, a hospital patient in the
US is exposed to one medication error per day; this ultimately leads to over 7,000 deaths per year
in this country alone (Flynn, Liang, Dickson, Xie, & Suh, 2012). The healthcare system as a
whole is continually trying to reduce this preventable problem. However, nurses are at the
forefront of this issue. In fact, research has shown that out of all healthcare employees nurses are
the most likely to identify and fix a medication error before these errors reach the patient (Flynn
et al., 2012). Since nurses play a part in both making errors and preventing them, it only makes
sense that nurses need to learn and understand the skills to prevent medication errors. While
there have been many strides to prevent medication errors, there still is work to be done. To still
have such a high prevalence of medication errors, even after all the work that has been put in
shows that there is still change that needs to ensue in order to minimize this devastating problem.
Leading Causes of Medication Errors
MEDICATION SAFETY
A medication error can occur at any stage of the process. There are so many people and
steps that a medication must go through in order to reach the patient, but we still have an
extremely high prevalence of medication errors. The top medication errors are:
prescription errors, such as wrong drug, dose, or form, interpretation errors, such as
misinterpretation of abbreviation, handwritten and spoken prescriptions, preparation
errors, such as calculation and dispensing errors, and administration errors, such as wrong
dose or wrong time to give or not give a medication. (Tzeng, Yin, & Schneider, 2013).
Another leading cause of medication errors is poor nursing environments. Nursing practice
environments are significantly associated with nurses error interception practices (Flynn et al.,
2012). Furthermore, cognitive errors may be involved in errors in human behavior, such as
medication errors (Tzeng et al., 2013). These cognitive errors happen due to deficient
knowledge. Therefore, changes in nursing education may need to be done to help prevent
medication errors.
The 6 Rights of Medication Safety
The six rights of medication safety is an invaluable tool for nurses to use in order to
prevent medication errors. If done correctly, the six rights should dramatically reduce medication
errors. To begin, the first right is right patient. Nurses need to make sure they are giving the
medication to the correct patient due to the harmful effects it could have for the patient you were
supposed to give the medication to and the patient you accidently gave the medication to. This
right can be implemented by matching up the patients name in the MAR, with the patients
wristband, and with the patient stating their name. The second right is right medication. Nurses
need to make sure they are giving the medication to the patient. Nurses also need to make sure
they are giving the right dose of the medication. Giving too small or too large of a dose could
cause a medication not to work, or worse could severely hurt the patient. Also, nurses need to
make sure there are giving the medication through the right route. Giving a medication IV push
MEDICATION SAFETY
when it was supposed to be IV piggyback would be disastrous. The fifth right is giving the
medication at the right time. Most medications are given at specific times of the day.
Furthermore, some medications have to be given at an exact same time due to dangerous side
effects if this is not followed. The final right is right documentation. If a nurse did not document
that they gave a medication, the next nurse will think that the patient never received the
medication. This could result in the patient receiving the medication for a second time, which
could clearly be very dangerous.
Supportive Nursing Environments
Good nursing environments are significantly associated with nurses more frequent
engagement in error interception practices (Flynn et al., 2012). Good nursing environments can
be made by encouraging collaborative teamwork, increasing opportunities for nurses to
participate in hospital and unit decisions, offering education opportunities, and retaining nurse
administrators that are accessible, listen to concerns, and expect high standards from the staff
(Flynn et al., 2012).
Building Clinical Cognition
Clinical cognition can be learned and taught by using a care-based approach with a
coached discussion to teach reasoning (Tzeng et al., 2012). Rather than waiting for the mistake
to happen in order to learn from it, clinical cognition can be learned through simulation-based
learning approaches with debriefing (Tzeng et al, 2012). This clinical cognition makes for more
experienced nurses; units with more experienced nurses had lower medication errors (Tzeng et
al., 2012).
Conclusion
Medication errors continue to be a major problem in the healthcare field. The most
common medication errors could be prevented by using the 6 rights of medication
administration. Moreover, supportive nursing environments and higher education of nurses were
associated with less medication errors. As a nursing student, I have been implementing the 6
MEDICATION SAFETY
rights every time I give a medication. I also look up the drugs in order to know what
assessments, side effects, and interactions that I need to look out for. These are both skills I need
to continue to implement throughout my nursing practice in order to prevent myself from making
a medication error. Also, I will soon have the opportunity to participate in simulation. This will
give me a patient scenario that will allow me to learn from any mistakes made without any true
repercussions such as hurting a patient. With these tools, I will be less likely to make a
medication error.
References
Flynn, L., Liang, Y., Dickson, G.L., Xie, M., & Suh, D. (2012). Nurses Practice Environments,
Error Interception Practices, and Inpatient Medication Errors. Journal of Nursing
Scholarship, 44(2), 180-186. doi: 10.1111/j.1547-5069.2012.01443.x
Tzeng, H., Yin, C., & Schneider, T.E. (2013). Medication Error-Related Issues in Nursing
Practice. Medsurg Nursing, 22(1), 13-16.
Das könnte Ihnen auch gefallen
- Chi Medication Errors PaperDokument6 SeitenChi Medication Errors Paperapi-698305049Noch keine Bewertungen
- Medication Errors 1Dokument7 SeitenMedication Errors 1api-661765354Noch keine Bewertungen
- Medication Errors FinalDokument7 SeitenMedication Errors Finalapi-469407326Noch keine Bewertungen
- MederrorpaperDokument6 SeitenMederrorpaperapi-642984838Noch keine Bewertungen
- Medications Error PaperDokument7 SeitenMedications Error Paperapi-676526945Noch keine Bewertungen
- Medication Error PaperDokument6 SeitenMedication Error Paperapi-272761526Noch keine Bewertungen
- Medication ErrorsDokument5 SeitenMedication Errorsapi-456052042Noch keine Bewertungen
- Med Error PaperDokument4 SeitenMed Error Paperapi-314062228100% (1)
- medication errors 3Dokument6 Seitenmedication errors 3api-692972467Noch keine Bewertungen
- Med ErrorsDokument6 SeitenMed Errorsapi-641561231Noch keine Bewertungen
- Nurses Compliance With The Five Rights of Medication AdministrationDokument8 SeitenNurses Compliance With The Five Rights of Medication AdministrationLuckyhansel CerezoNoch keine Bewertungen
- Running Head: Medical Errors: Wrong Dosage 1Dokument5 SeitenRunning Head: Medical Errors: Wrong Dosage 1api-315192697Noch keine Bewertungen
- Medication ErrorsDokument7 SeitenMedication Errorsapi-679663498Noch keine Bewertungen
- Med Error Paper 11Dokument9 SeitenMed Error Paper 11api-576936136Noch keine Bewertungen
- medication errors paper 1Dokument6 Seitenmedication errors paper 1api-739232245Noch keine Bewertungen
- Medication Errors PaperDokument6 SeitenMedication Errors Paperapi-487459879Noch keine Bewertungen
- Medication Errors in Nursing 1Dokument6 SeitenMedication Errors in Nursing 1Komal TanveerNoch keine Bewertungen
- Medication Errors in PediatricsDokument5 SeitenMedication Errors in Pediatricsapi-609304902Noch keine Bewertungen
- Clinical Paper FinalDokument6 SeitenClinical Paper Finalapi-679675055Noch keine Bewertungen
- Final Draft Medication Administration ErrorsDokument13 SeitenFinal Draft Medication Administration Errorsapi-466369078100% (1)
- Medication Safe Practice PaperDokument5 SeitenMedication Safe Practice Paperapi-301424065Noch keine Bewertungen
- Medication Errors Paper 2019Dokument6 SeitenMedication Errors Paper 2019api-485472556100% (1)
- Medication Errors Paper OmarDokument7 SeitenMedication Errors Paper Omarapi-679742031Noch keine Bewertungen
- Med Errors PaperDokument5 SeitenMed Errors Paperapi-433705780Noch keine Bewertungen
- Thesis Medication ErrorsDokument7 SeitenThesis Medication ErrorsMichele Thomas100% (2)
- Medication Error PaperDokument5 SeitenMedication Error Paperapi-457485362Noch keine Bewertungen
- NURS4020 Ashley Assessment1 Attemp1Dokument6 SeitenNURS4020 Ashley Assessment1 Attemp1ashleyNoch keine Bewertungen
- Med Error Paper 1Dokument4 SeitenMed Error Paper 1api-456592801100% (1)
- Med Error PaperDokument5 SeitenMed Error Paperapi-433370150Noch keine Bewertungen
- Medication Errors in The United States and How To Improve Simple Mistakes 1Dokument7 SeitenMedication Errors in The United States and How To Improve Simple Mistakes 1api-681331537Noch keine Bewertungen
- Medication Error ThesisDokument6 SeitenMedication Error Thesisoaehviiig100% (2)
- Ms 1 Clinical DocumentDokument5 SeitenMs 1 Clinical Documentapi-322601311Noch keine Bewertungen
- Medication ErrorsDokument7 SeitenMedication ErrorsNelly CheptooNoch keine Bewertungen
- Med Errors FinalDokument7 SeitenMed Errors Finalapi-485620816Noch keine Bewertungen
- Medication Errors PaperDokument6 SeitenMedication Errors Paperapi-542442476Noch keine Bewertungen
- Med Errors PaperDokument7 SeitenMed Errors Paperapi-733165948Noch keine Bewertungen
- The Importance of Correct Medication Administration 1Dokument5 SeitenThe Importance of Correct Medication Administration 1api-608069746Noch keine Bewertungen
- Medication Error - Michael SandinDokument5 SeitenMedication Error - Michael Sandinapi-379546477Noch keine Bewertungen
- medication errors paperDokument6 Seitenmedication errors paperapi-740209346Noch keine Bewertungen
- Medication Safe PracticeDokument5 SeitenMedication Safe Practiceapi-288858560Noch keine Bewertungen
- ch1 Clinical PaperDokument6 Seitench1 Clinical Paperapi-641501601Noch keine Bewertungen
- Med Error FinalDokument5 SeitenMed Error Finalapi-302151448Noch keine Bewertungen
- The Nurse's Role in Medication SafetyDokument6 SeitenThe Nurse's Role in Medication Safetyloker ihc100% (1)
- Attributable To The Use of Medications (: Near MissesDokument4 SeitenAttributable To The Use of Medications (: Near MissesdudijohNoch keine Bewertungen
- medicationerrorpaperDokument7 Seitenmedicationerrorpaperapi-739619370Noch keine Bewertungen
- Medication Errors in NursingDokument7 SeitenMedication Errors in Nursingapi-307925878Noch keine Bewertungen
- ms1 Medication Errors PaperDokument5 Seitenms1 Medication Errors Paperapi-417446716Noch keine Bewertungen
- Medication Errors Heidi BosmansDokument7 SeitenMedication Errors Heidi Bosmansapi-283672381Noch keine Bewertungen
- Qsen Paper-SubmittedDokument7 SeitenQsen Paper-Submittedapi-396919069Noch keine Bewertungen
- Answer 1Dokument6 SeitenAnswer 1Hezekiah AtindaNoch keine Bewertungen
- Reducing Medication Errors in HospitalsDokument9 SeitenReducing Medication Errors in Hospitalsakko aliNoch keine Bewertungen
- Research Paper Medication ErrorsDokument6 SeitenResearch Paper Medication Errorsegxtc6y3100% (1)
- Medication Errors FinalDokument5 SeitenMedication Errors Finalapi-379817190Noch keine Bewertungen
- Medication Errors Their Causative and Preventive Factors2.Doc 1Dokument11 SeitenMedication Errors Their Causative and Preventive Factors2.Doc 1Mary MannNoch keine Bewertungen
- Medication Error PaperDokument7 SeitenMedication Error Paperapi-315569993Noch keine Bewertungen
- What Are The 5 Rights of Dispensing Medicine - InvisitRxDokument4 SeitenWhat Are The 5 Rights of Dispensing Medicine - InvisitRxShanza WaheedNoch keine Bewertungen
- Medication Errors - EditedDokument7 SeitenMedication Errors - EditedHezron RonoNoch keine Bewertungen
- Research PaperDokument14 SeitenResearch Paperapi-455600000Noch keine Bewertungen
- Research PaperDokument14 SeitenResearch Paperapi-455767165Noch keine Bewertungen
- Drug Administration in Nursing: A Comprehensive Guide to Drug Administration and Calculation in NursingVon EverandDrug Administration in Nursing: A Comprehensive Guide to Drug Administration and Calculation in NursingNoch keine Bewertungen
- Certificate of Induction To Sigma Theta TauDokument1 SeiteCertificate of Induction To Sigma Theta Tauapi-283066063Noch keine Bewertungen
- Cover Letter Am 2016Dokument1 SeiteCover Letter Am 2016api-283066063Noch keine Bewertungen
- New Resume 4-4-16 AmDokument1 SeiteNew Resume 4-4-16 Amapi-283066063Noch keine Bewertungen
- Community Cancer Capstone PaperDokument11 SeitenCommunity Cancer Capstone Paperapi-283066063Noch keine Bewertungen
- Evidence Based Practice Synthesis PaperDokument16 SeitenEvidence Based Practice Synthesis Paperapi-283066063Noch keine Bewertungen
- Nursing Process WorksheetsDokument5 SeitenNursing Process Worksheetsapi-283066063Noch keine Bewertungen
- Nurse RecommendationsDokument7 SeitenNurse Recommendationsapi-283066063Noch keine Bewertungen
- Pat 1 Med Surge 2 PortfolioDokument21 SeitenPat 1 Med Surge 2 Portfolioapi-283066063Noch keine Bewertungen
- Body Mechanics PaperDokument5 SeitenBody Mechanics Paperapi-259018499Noch keine Bewertungen
- Nursing For Wellness in Older Adults Miller 6th Edition Test BankDokument36 SeitenNursing For Wellness in Older Adults Miller 6th Edition Test Bankdripplenecrosisdufk9s100% (40)
- CV Nusrat Farha 1Dokument1 SeiteCV Nusrat Farha 1Tuners republicNoch keine Bewertungen
- Ebook A Guide To Improving Your Patient Safety Event Reporting Culture Plus A Leadership Action ListDokument8 SeitenEbook A Guide To Improving Your Patient Safety Event Reporting Culture Plus A Leadership Action ListJery JsNoch keine Bewertungen
- Principles of Test Taking MTCDokument28 SeitenPrinciples of Test Taking MTCMyk MacalintalNoch keine Bewertungen
- General WardDokument2 SeitenGeneral WardDilshad TasnimNoch keine Bewertungen
- Interior Health Medication Management AuditDokument46 SeitenInterior Health Medication Management AuditJoe Fries100% (1)
- Module 11 - Instructional SettingsDokument2 SeitenModule 11 - Instructional SettingsrishellemaepilonesNoch keine Bewertungen
- Radiologic Observation PowerPointDokument14 SeitenRadiologic Observation PowerPointMariela RonquilloNoch keine Bewertungen
- Patient Safety Incident Report Form SummaryDokument9 SeitenPatient Safety Incident Report Form SummaryJhun SantiagoNoch keine Bewertungen
- Writing Patient Notes and Tour Guiding Tips(39Dokument4 SeitenWriting Patient Notes and Tour Guiding Tips(39Remedios Abiera Bianes100% (5)
- Finalized Report 17nov2018 REVISEDDokument30 SeitenFinalized Report 17nov2018 REVISEDMario WallaceNoch keine Bewertungen
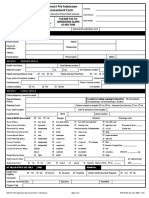
- Patient Admission Assessment FormDokument1 SeitePatient Admission Assessment Formprasanna_326avanthiNoch keine Bewertungen
- Mental Health Nursing PrinciplesDokument26 SeitenMental Health Nursing PrinciplesShamala Anjanappa100% (3)
- Clinical Nursing Judgement 2Dokument6 SeitenClinical Nursing Judgement 2api-545172676Noch keine Bewertungen
- Session 7Dokument2 SeitenSession 7Sistine Rose LabajoNoch keine Bewertungen
- Health Education 2 2Dokument13 SeitenHealth Education 2 2simbulanrhaiza2Noch keine Bewertungen
- Registered Nurse Resume SampleDokument2 SeitenRegistered Nurse Resume Sampleresume7.com100% (8)
- PDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateDokument5 SeitenPDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateNilanjana ChakrabortyNoch keine Bewertungen
- IHH Annual Report 2022Dokument144 SeitenIHH Annual Report 2022&Noch keine Bewertungen
- HIS 1st Semester LIMS ReviewDokument4 SeitenHIS 1st Semester LIMS ReviewLYKA ANTONETTE ABREGANANoch keine Bewertungen
- Resume For PortfolioDokument5 SeitenResume For Portfolioapi-282992446Noch keine Bewertungen
- NCM 122 Ratio FinalsDokument2 SeitenNCM 122 Ratio FinalsLorenz Jude CańeteNoch keine Bewertungen
- Withholding & Withdrawing Life-Sustaining TreatmentDokument11 SeitenWithholding & Withdrawing Life-Sustaining TreatmentDr. Liza Manalo100% (1)
- History and Mental Status Exam GuideDokument17 SeitenHistory and Mental Status Exam Guideyeney armenterosNoch keine Bewertungen
- Case 1 Carilion ClinicDokument14 SeitenCase 1 Carilion ClinicVikram KumarNoch keine Bewertungen
- Expand Shouldice Hospital's CapacityDokument2 SeitenExpand Shouldice Hospital's CapacityRishabh SinghNoch keine Bewertungen
- Title of Project:-Military Hospital Report Management SystemDokument4 SeitenTitle of Project:-Military Hospital Report Management SystemAkbar AliNoch keine Bewertungen
- Synopsis DR Mahfishan Amended FinalDokument26 SeitenSynopsis DR Mahfishan Amended FinalMominah MayamNoch keine Bewertungen
- Phil HealthDokument129 SeitenPhil HealthAnthony Joshua OrdenNoch keine Bewertungen