Beruflich Dokumente
Kultur Dokumente
Personal Social History
Hochgeladen von
ledfielcastilloOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Personal Social History
Hochgeladen von
ledfielcastilloCopyright:
Verfügbare Formate
PERSONAL SOCIAL HISTORY
Mr. M.H. is the youngest in their family. He has 2 brothers and 1 sister. At the age of 14, the patient started to become
a smoker and drinker. He used to drink liquor with his friends during his free time. He consumed 1-2 packs of cigarette and 1-2
bottle of gin four times a week. In terms on his exercise he plays basketball with his friends. When he reached the age of 16, he
started earning money by driving their own tricycle after attending on his classes to support his vices. At the age of 17, he
graduated from high school and did not pursue his study in college. He already consumed 2-3 packs of cigarette and 1-2 bottles
of gin six times a week. He had an intimate and committed relationship with his girlfriend at the age of 20. He has a lot of friends
and some of them influenced him to smoke (fortune cigarettes) and drink liquor (gin).
PAST HISTORY
He had a complete vaccination of BCG, OPV, DPT, Hepa-B, and Measles. He had no known allergy to food. Cough
and colds is one of his childhood illnesses and because they cannot afford to buy medication the illness became worst. In 1985, at
the age of 1, he was brought to Bataan Provincial Hospital with chief complaint of prolonged cough and colds and diagnosed to
have bronchopneumonia and was given some medication like bronchodam and clariget. Their environment has poor living
condition and during those times their source of water came from water pump. In 1987, at the age of 3, he was brought again to
Bataan Provincial Hospital with complaints of severe abdominal pain and frequent passage of watery stool. He was diagnosed to
have Amoebiasis and was given medication of metronidazole. Last 2005, he experience 3 days of high grade fever that lead to
convulsion and was rushed at St. Michael Hospital and he was confine for one week, and later diagnosed to have seizure and was
given medication like dilantin.
FAMILY HISTORY
Mr. M.H. mother side has a history of diabetes mellitus. Both sides of his parents have no history of cancer, mental
disorder, hypertension, tuberculosis and liver cirrhosis.
PRESENT HISTORY
Three days prior to admission, the patient had complaints of epigastric pain, fever, and body weakness. He was
admitted in Bataan General Hospital on November 1, 2009 at 11:50 pm under the care of Dr. Almario Malixi with initial
diagnosis of jaundice with icteric sclera. He was given an IVF of PNSS 1 liter and oxygen inhalation of 2-3 lpm via nasal
cannula. Before we handle the patient he is undergone laboratory test of Hematology on November 5, 2009, he has a decreased
Hemoglobin and Hematocrit, while on his Blood Chemistry he has decreased level of sodium and potassium. On November 6,
2009, after the readings of his result in hematology Dr. Malixi requests to have 4 units of PRBC with blood type A. When we
handle the patient on November 9, 2009 he was conscious and coherent, pale and weak in appearance, warm to touch. He has
difficulty of breathing with use of accessory muscle, sparse body hair and pruritus. His lips are dry and cracked, he has a bleeding
gums and with bruises on upper extremities. He has bloated stomach with abdominal girth of 34 cm. and bipedal edema of 2+.
An indwelling Foley catheter was inserted due to inability to void. Upon the interview the patient claim that he has a hemorrhoid
that’s why he had difficulty in defecating. His initial vital signs was temperature (38.5°C), respiratory rate (32 bpm), pulse rate
(73 bpm), and blood pressure (110/70 mmHg) and on November 10, 2009 Dr. Malixi ordered him to have abdominal ultrasound
but he cannot afford to undergo the abdominal ultrasound. On November 11, 2009 the patient manifested disorientation, delirium
and hallucination.
Because of unavailability of the blood and financial problem the patient was not able to undergo blood transfusion.
Only on November 16, 2009, at 3:35 pm, he was given 1 unit of PRBC type A.
Das könnte Ihnen auch gefallen
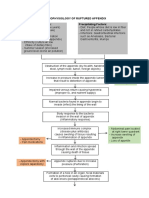
- Pathophysiology of Ruptured AppendixDokument2 SeitenPathophysiology of Ruptured AppendixAya PaquitNoch keine Bewertungen
- Appendix 1 Occupational Therapy Bathing-Showering ToolDokument3 SeitenAppendix 1 Occupational Therapy Bathing-Showering ToolNizam lotfiNoch keine Bewertungen
- Multiple Physical Injuries Secondary To Vehicular AccidentDokument31 SeitenMultiple Physical Injuries Secondary To Vehicular AccidentAnton Laurenciana50% (2)
- Case - Neck MassDokument78 SeitenCase - Neck MassMico TanNoch keine Bewertungen
- Post Anaesthesia Shivering - N PadayacheeDokument19 SeitenPost Anaesthesia Shivering - N Padayacheexxxvrgnt100% (2)
- Pathophysiology of Gastric Cancer Precipitating Factors: - Predisposing FactorsDokument3 SeitenPathophysiology of Gastric Cancer Precipitating Factors: - Predisposing FactorsJu Lie AnnNoch keine Bewertungen
- 2018 Doh Ambulance License RequirementsDokument31 Seiten2018 Doh Ambulance License RequirementsChris-Goldie Lorezo87% (31)
- NCP LeptospirosisDokument2 SeitenNCP LeptospirosisLouise Anne Asuncion OclimaNoch keine Bewertungen
- Pulmonary Tuberculosis: A Case Study ofDokument33 SeitenPulmonary Tuberculosis: A Case Study ofRJ MarquezNoch keine Bewertungen
- Chron's Disease 2Dokument3 SeitenChron's Disease 2TarantadoNoch keine Bewertungen
- Handout IV: DSM-5 ASD Checklist: Making An Autism Spectrum Disorder DiagnosisDokument2 SeitenHandout IV: DSM-5 ASD Checklist: Making An Autism Spectrum Disorder DiagnosisValentina IerotheouNoch keine Bewertungen
- Operating Room Write-Up: PathophysiologyDokument4 SeitenOperating Room Write-Up: PathophysiologyArian May MarcosNoch keine Bewertungen
- Pathophysiology of AGE With DHNDokument1 SeitePathophysiology of AGE With DHNFarr Krizha Tangkusan50% (2)
- 3 Developmental Tasks of Later MaturityDokument3 Seiten3 Developmental Tasks of Later MaturitySarah BenjaminNoch keine Bewertungen
- Jurisprudence RevDokument48 SeitenJurisprudence RevJoel JoseNoch keine Bewertungen
- NeuroMuscular Blocking AgentsDokument3 SeitenNeuroMuscular Blocking AgentsdrugdrugNoch keine Bewertungen
- Ondansetron (Zofran)Dokument1 SeiteOndansetron (Zofran)Cassie100% (1)
- Autonomic Nervous System PharmacologyDokument7 SeitenAutonomic Nervous System Pharmacologydonordarah93Noch keine Bewertungen
- Cellular AberrationDokument14 SeitenCellular AberrationjinahyangNoch keine Bewertungen
- Dental Case Sheet Corrcted / Orthodontic Courses by Indian Dental AcademyDokument8 SeitenDental Case Sheet Corrcted / Orthodontic Courses by Indian Dental Academyindian dental academyNoch keine Bewertungen
- Pathophysiology of Rheumatic FeverDokument3 SeitenPathophysiology of Rheumatic FeverGehlatin Tumanan100% (2)
- NAPREXDokument2 SeitenNAPREXKarl EdemNoch keine Bewertungen
- B. Diagram: Predisposing Factors: Precipitating Factors EtiologyDokument3 SeitenB. Diagram: Predisposing Factors: Precipitating Factors EtiologyKenneth Torres100% (1)
- Pediatric Community Acquired Pneumonia (PCAP) : Case StudyDokument38 SeitenPediatric Community Acquired Pneumonia (PCAP) : Case StudyAndrew Perez0% (1)
- Naprex Drug StudyDokument3 SeitenNaprex Drug StudyAngelica shane NavarroNoch keine Bewertungen
- Afinidad, Jiezl A: Davao Doctors College Nursing ProgramDokument4 SeitenAfinidad, Jiezl A: Davao Doctors College Nursing ProgramJiezl Abellano AfinidadNoch keine Bewertungen
- OR Write Up - Repeat LSCSDokument2 SeitenOR Write Up - Repeat LSCSWyen CabatbatNoch keine Bewertungen
- Patient 3 NSDDokument20 SeitenPatient 3 NSDBea Bianca CruzNoch keine Bewertungen
- Case PresDokument5 SeitenCase PresBeverlyNoch keine Bewertungen
- Drug StudyDokument12 SeitenDrug StudyAnne Marie Angelica BilonoNoch keine Bewertungen
- Final Case Study PCAPDokument72 SeitenFinal Case Study PCAPKelly Tayag100% (1)
- 4.0 Doctors Order Grand CaseDokument23 Seiten4.0 Doctors Order Grand CasekeithNoch keine Bewertungen
- Acute Lymphoblastic Leukemia Pathophysiology: Predisposing Factors: Etiology: Precipitating FactorsDokument3 SeitenAcute Lymphoblastic Leukemia Pathophysiology: Predisposing Factors: Etiology: Precipitating FactorsKyla ValenciaNoch keine Bewertungen
- Pcap PathophysiologyDokument3 SeitenPcap PathophysiologyZandra Lyn AlundayNoch keine Bewertungen
- Nursing Care Plan For Dengue Hemmorrhagic FeverDokument6 SeitenNursing Care Plan For Dengue Hemmorrhagic FeverMean Elepaño100% (1)
- KASP Package RateDokument502 SeitenKASP Package RateAnoop VijayakumarNoch keine Bewertungen
- DengueDokument4 SeitenDengueKathleen DimacaliNoch keine Bewertungen
- NCP of MGH PatientDokument2 SeitenNCP of MGH PatientMaverick LimNoch keine Bewertungen
- Narrative PathophysiologyDokument1 SeiteNarrative PathophysiologyJemsMei Comparativo MensuradoNoch keine Bewertungen
- PATHOPHYSIOLOGY TCHI Client BasedDokument1 SeitePATHOPHYSIOLOGY TCHI Client BasedGem MarasiganNoch keine Bewertungen
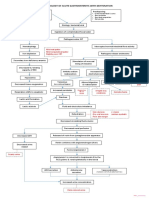
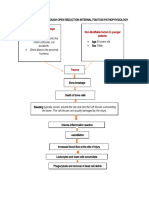
- Post Open Reduction Internal Fixation PathophysiologyDokument3 SeitenPost Open Reduction Internal Fixation PathophysiologyRizalyn QuindipanNoch keine Bewertungen
- Nursing Health HistoryDokument2 SeitenNursing Health HistorySheryhan Tahir BayleNoch keine Bewertungen
- Pcap Pathophysiology PDFDokument3 SeitenPcap Pathophysiology PDFMikaela RamosNoch keine Bewertungen
- PDF Albumin Drug StudyDokument1 SeitePDF Albumin Drug StudyJamie John EsplanadaNoch keine Bewertungen
- Ineffective Health MaintenanceDokument6 SeitenIneffective Health MaintenanceRYAN SAPLADNoch keine Bewertungen
- You Are Caring For A Patient With An NG Feeding TubeDokument2 SeitenYou Are Caring For A Patient With An NG Feeding TubeWen Silver100% (1)
- NCP & Drugstudy FormatDokument7 SeitenNCP & Drugstudy Formatanonymous89ify100% (1)
- Charting CraniotomyDokument1 SeiteCharting CraniotomyJrBong SemaneroNoch keine Bewertungen
- University of Northern PhilippinesDokument2 SeitenUniversity of Northern PhilippinesCezanne Cruz0% (1)
- Cristobal, Rocelyn P. MS Lec Post Task Triage FinalDokument10 SeitenCristobal, Rocelyn P. MS Lec Post Task Triage FinalRocelyn CristobalNoch keine Bewertungen
- Measles PathophysiologyDokument1 SeiteMeasles PathophysiologyAl TheóNoch keine Bewertungen
- DRUG+STUDY NaprexDokument2 SeitenDRUG+STUDY NaprexJoevence Gazo CuaresmaNoch keine Bewertungen
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDokument6 SeitenAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasNoch keine Bewertungen
- Patho Pott's DseDokument2 SeitenPatho Pott's Dsexai_teovisioNoch keine Bewertungen
- OB Group 1 PA ToolDokument23 SeitenOB Group 1 PA ToolAubrey Dynise C. TorralbaNoch keine Bewertungen
- Balance Skeletal TractionDokument5 SeitenBalance Skeletal TractionRachel Ann JimenezNoch keine Bewertungen
- Pathophysiology - AppendicitisDokument5 SeitenPathophysiology - AppendicitisAzielle Joyce RosquetaNoch keine Bewertungen
- DOCTORS ORDER CRMCDokument2 SeitenDOCTORS ORDER CRMCMarielle ChuaNoch keine Bewertungen
- Pathophysiology AGEDokument2 SeitenPathophysiology AGEMareeze Hatta100% (1)
- Gordon's HisDokument4 SeitenGordon's HisJee ShangNoch keine Bewertungen
- Azithromycin Drug StudyDokument2 SeitenAzithromycin Drug StudySHEILA MAE SACLOTNoch keine Bewertungen
- 13-Areas-of-Assessment-2017 2Dokument3 Seiten13-Areas-of-Assessment-2017 2Alyssa Moutrie Dulay ArabeNoch keine Bewertungen
- Case Study - LeptospirosisDokument3 SeitenCase Study - LeptospirosisMarie Jennifer ParilNoch keine Bewertungen
- Geographical Area - Tropical Islands in Thepacific (Philippines) and AsiaDokument1 SeiteGeographical Area - Tropical Islands in Thepacific (Philippines) and AsiaGenevang SeaweedsNoch keine Bewertungen
- PCAP CPDokument14 SeitenPCAP CPMikael R. SmileNoch keine Bewertungen
- Pathophysiology VolvulusDokument2 SeitenPathophysiology VolvulusHyacinth Bueser Bondad0% (2)
- Interview Guide For Nursing Health HistoryDokument3 SeitenInterview Guide For Nursing Health HistoryDersly LaneNoch keine Bewertungen
- CasepresDokument3 SeitenCasepresJoyce Ramos CadondonNoch keine Bewertungen
- Irene's Care StudyDokument68 SeitenIrene's Care StudyLawrence AckahNoch keine Bewertungen
- April LeDokument21 SeitenApril LeAprille Anne SagmitNoch keine Bewertungen
- Chapter 6 Confidence Interval Estimates SolutionDokument18 SeitenChapter 6 Confidence Interval Estimates SolutionShrey Mangal92% (12)
- Aritmia AHA 2017Dokument120 SeitenAritmia AHA 2017Corticosteroids MobileLegendNoch keine Bewertungen
- Drug Study (Cervical Polyp)Dokument4 SeitenDrug Study (Cervical Polyp)aerondominicbasilioNoch keine Bewertungen
- Chrisanthopoulos Marika 300453 Cleft Lip and PalateDokument14 SeitenChrisanthopoulos Marika 300453 Cleft Lip and PalateCharles IppolitoNoch keine Bewertungen
- Formulary - Good ReadDokument121 SeitenFormulary - Good ReadJananiRajamanickamNoch keine Bewertungen
- RhinosporidiosisDokument9 SeitenRhinosporidiosisDrAnwar MKNoch keine Bewertungen
- Standardizing Standard Operating Procedures SOP MDokument3 SeitenStandardizing Standard Operating Procedures SOP MTejasNoch keine Bewertungen
- PSYCHIATRY Classification of Psychiatric Disorder (Dr. Rosal)Dokument11 SeitenPSYCHIATRY Classification of Psychiatric Disorder (Dr. Rosal)Valcrist BalderNoch keine Bewertungen
- 2007 Tweed ProfileDokument60 Seiten2007 Tweed ProfileYeny Valdivia AlbornozNoch keine Bewertungen
- Short WaveDokument31 SeitenShort WaveDharmesh MaheshwariNoch keine Bewertungen
- WelchAllyn Propaq Encore Vital Signs Monitor - Reference GuideDokument178 SeitenWelchAllyn Propaq Encore Vital Signs Monitor - Reference GuideSergio PérezNoch keine Bewertungen
- Carefusion CannulasDokument8 SeitenCarefusion Cannulasrubenr25Noch keine Bewertungen
- DR Ahmed Abar CVDokument7 SeitenDR Ahmed Abar CVAnonymous H1EZvy1yQNoch keine Bewertungen
- Adrenergic Antagonists EditedDokument60 SeitenAdrenergic Antagonists EditedJohn Benedict VocalesNoch keine Bewertungen
- Canine Elbow Dysplasia: Heidi Reuss-Lamky, LVT, VTS (Anesthesia)Dokument6 SeitenCanine Elbow Dysplasia: Heidi Reuss-Lamky, LVT, VTS (Anesthesia)Katarina SimicicNoch keine Bewertungen
- Therapeutic Drug MonitoringDokument6 SeitenTherapeutic Drug MonitoringEdi Uchiha SutarmantoNoch keine Bewertungen
- Leading Dentist in Oshawa - Scarborough - Grandview Dental ClinicDokument7 SeitenLeading Dentist in Oshawa - Scarborough - Grandview Dental Clinicnaveen bansalNoch keine Bewertungen
- Pharmaceutical Sales & Marketing Legal and Ethical ConsiderationsDokument41 SeitenPharmaceutical Sales & Marketing Legal and Ethical ConsiderationsqmnwebNoch keine Bewertungen
- Nursing EducationDokument136 SeitenNursing EducationNishi Vaibhav KumarNoch keine Bewertungen
- By Dr. Myra C. BritillerDokument72 SeitenBy Dr. Myra C. BritillerCharleneBunquin100% (1)