Beruflich Dokumente
Kultur Dokumente
Intergrative Review
Hochgeladen von
api-272448190Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Intergrative Review
Hochgeladen von
api-272448190Copyright:
Verfügbare Formate
Running head: AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
An Integrative Review: Prophylactic antibiotic use and surgical site infections
NUR4222 Nursing Research for RNs
Michael Phelps
May 3, 2015
I Pledge
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
Abstract
The evaluation of literature in regards to the administration of prophylactic antibiotics
with regards to the every patient or those at risk for developing a surgical site infection is the
goal of this integrative review. Surgical site infections are described as an infection that occurs
at or near a surgical incision within 30 days for a surgical procedure and within one year of an
implanted item. Prophylactic antibiotics have been used for more than 15 years for select
surgical procedures. And, with CDC and CMS development of the Surgical Care Improvement
Project, prophylactic antibiotic has prevalent presence for surgical procedures. Within this
integrative review, literature has been located with the aid of computer based search engines
like PubMed and EBSCO database. During my search 9 studies met the criteria for the topic but
only 5 were useful for this integrative review. Two limitations existed within this integrative
review: some articles were not available in full text or English, which decrease the number of
useful studies. And, statistical analysis test in the useful studies were not explained for readers.
The studies did not answer the question of usefulness of prophylactic antibiotics for minor
procedures; it did answer the PICOT question of administration to every patient or those with
surgical site infection risk factors. Further research should focus on the risk factors for surgical
site infections and use of prophylactic antibiotics.
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
An Integrative Review: Prophylactic antibiotic use and surgical site infections
This integrative review has one general purpose to search for and relate studies involving
prophylactic antibiotic use with minor surgical procedures. Surgical site infections are described
as an infection that occurs at or near a surgical incision within 30 days for a surgical procedure
and within one year of an implanted item (Heal, Buettner, & Drobetz, 2012). With surgical site
infections accounting for the third most common healthcare related infection resulting in
morbidity and deaths (Gharde, et al., 2014). Current prophylactic antibiotic guidelines
recommend prophylaxis for Cardiothoracic, Gastrointestinal, Orthopedic, Vascular, and GYN
procedures. Dermatological, General procedure not involving the gastrointestinal tract, and
urological procedures do not have a recommendation for prophylaxis. The PICOT question
proposed is as follows: Should prophylactic antibiotics be administered to every patient,
regardless, or just to those patients at risk for developing a surgical site infection?
Search Methods/ Designs
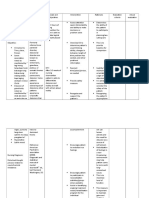
This integrative review is a complex collection of five studies involved in determining
the answer to one question without any assumptions for its research design. Research articles
were located with the use of two computer-based search engines PubMed and EBSCO. Related
terms included, antibiotics, prophylactic, prophylaxis, risk factors, and minor
procedures. The search resulted in 9 articles that met the criteria for the topic; however, only
five articles useful for the integrative review. While four of the articles were written within the
last six years, one article was written in 1998. This one article was deemed useful for its
research related to facial lacerations related to dog bites and contamination of the wound from
the dogs saliva. All related articles needed to be available in English. All related articles had to
relate to the PICOT question: should prophylactic antibiotics be administered to every patient,
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
regardless, or just to those patients at risk for developing a surgical site infection? Also, two out
of five of the articles had to have a qualitative in design and in relation to antibiotics, surgical site
infection risk factors, and the development of a surgical site infection. The other three articles are
quantitative in design and in relation to antibiotics, surgical site infection risk factors, and the
development of a surgical site infection. Articles not meeting the required criteria were exempt
from the integrative review.
Finding/Results
All five studies produced the same answer to the PICOT question regarding prophylactic
antibiotic administration for every patient or those with surgical site infection risk factors. All
five determined that prophylactic antibiotic usage has no significant role in reducing the
occurrence of surgical site infections. Also, the occurrence of a surgical site infection is
dependent on location, size of incision, comorbities of the patient, and the patients own microorganisms (Gharde, et al., 2014) (Heal, Buettner, & Drobetz, 2012) (Javaid, Feidberg, & Gipson,
1998) (Yuste, Romo, & Unamuno, 2015) (Zhou, Zhang, Wang, & Hu, 2009). The review has
been subdivided into three categories: Data collection, samples and subjects, and data analysis.
Data Collection
Even though all five studies produced a uniform outcome to prophylactic antibiotic
administration, they all had different methods to collecting data. Informed consent is only
mentioned in one of the five studies. The study conducted by Gharde and associates utilized data
collected from two groups (open cholecystectomies and laparoscopic cholecystectomies). The
study employed a comparative approach with regards to the two groups. All participants
received prophylactic antibiotics before surgery. Out of the two groups, the researchers
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
interviewed the participants on day seven post-surgery or whenever the participant exhibited
signs of infection (discharge, pain, and/or fever) (Gharde, et al., 2014).
The study conducted by Heal, Buettner, and Drobetz used a comparative approach after
interviewing patients from sixteen general practitioners in North Queensland, Australia. With
information like demographics, clinical data, and a body site map, the researchers formulate the
possible risk factors for infection related to patients. Even though the study does not mention an
informed consent, the researchers asked any patient presenting with a minor skin excision to
participate within the trail (Heal, Buettner, & Drobetz, 2012).
The study from Javaid, Feidberg, and Gipson is the only study that uses case notes from
April 1994 to April 1997. With the use of the case notes, the patients outcome and
complications related to the repair or reconstruction of the face (Javaid, Feidberg, & Gipson,
1998). Out of the all the studies, this study appeared to have the simplest data collection.
Even though the study conducted by Yuste, Romo, and Unamun does not contain a
specific plan for data collection. The researchers use already proven approaches to determining
the best effective route and antibiotic to use for postsurgical site infection prevention (Yuste,
Romo, & Unamuno, 2015). The data collected is provided from antibiotic literature that has
been already published from antibiotic manufactures. Since the data collection does not utilize
or quantify with a specific number, this study utilizes a ground theory for its qualitative view.
The same qualitative view applies towards the study conducted by Zhou, Zhang, and
Wang. The researchers utilize previous studies and recorded data pertaining to the previous
studies (Zhou, Zhang, Wang, & Hu, 2009). As a result, the use of the previous studies for data
collection supplies the researchers with a collaborative approach to defining the results for this
study.
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
Samples and Subjects
The Gharde, Heal, and Javaid studies are the only quantitative studies that utilize subjects
and a sampling method for the analysis of information. However, the Javaid study is the only
study that simplifies the answer with tables and grafts. The Heal study does not separate subjects
into different sexes, unlike the other two quantitative studies. Samples within these three studies
were convenient; subjects were either eligible or not eligible. The information on subjects for
the Javaid study were convenient and probable, subjects having already gone through surgery,
and case notes were the only information used for the study (Javaid, Feidberg, & Gipson, 1998).
The Gharde and Heal studies utilized information after a subject was located and a procedure had
been completed (Gharde, et al., 2014) (Heal, Buettner, & Drobetz, 2012). The Gharde study was
the only study to have 2 groups with a random number for males and females; however, each
group corresponded to two different types of cholecystectomy surgeries (Gharde, et al., 2014).
Two of the quantitative studies, Gharde and Heal, had a non-probability sampling method. The
researcher did not know what the possible outcome would be with this random number of
subjects.
In addition, the Yuste and Zhou studies employed a convenient sampling method with a
probability of the subjects outcome. The Yuste study utilized the already known outcomes and
information available for antibiotic administration effectiveness (Yuste, Romo, & Unamuno,
2015). On the other hand, the Zhou study used 20 previous studies and any recorded data
pertaining to antibiotic prophylaxis for elective laparoscopic cholecystectomies and created a
large scale analysis of those previous studies findings (Zhou, Zhang, Wang, & Hu, 2009). Even
though both studies, Yuste and Zhou, are qualitative in method and are using already published
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
information to a produce the same answer, these studies still provide a manage to devise the
answer from different sources.
Data analysis
Data analysis of the studies is more than likely the most difficult portion of the studies to
analysis. Therefore data analysis within this integrative review is a limitation for understanding
of the researchers needs to quantify the numerical answers within the Gharde, and Heal studies.
Within these two studies, the researchers used the Chi square test; however, none of the studies
explain what the Chi square test is and the significance behind the test (Gharde, et al., 2014)
(Heal, Buettner, & Drobetz, 2012). However, the Heal study did provide the purpose for MannWhitney-Wilcoxon test, generalized linear modeling, Poisson distribution, and logarithmic link
function were used for (Heal, Buettner, & Drobetz, 2012). The Zhou study utilized a Jadad
composite scale, quality assessment, odds ratio, and random effect model for its data analysis
(Zhou, Zhang, Wang, & Hu, 2009).
However, two studies, Javaid and Yuste, placed tables and grafts within the study that
corresponded to information gathered from the case notes and supplied information. These two
studies are the only two that simplify and provide easy to understand information regarding their
studies. Even though the Javaid and Yuste studies do not utilize some statistical analysis test,
they do use categories to produce and measure the data received and produced for the studies.
Discussion/ Implications
The PICOT question proposed whether or not prophylactic antibiotics be administered to
every patient, regardless, or just to those patients at risk for developing a surgical site infection?
Through this integrative review and research provided, five articles have provided a definitive
answer and also raised a possible future research topic. All five studies used a different method
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
or additional method in relation to each other in order to produce the same answer to the PICOT
question. Through data collection, different sampling sizes, varying subjects, even a study from
1998, varying statistical analyses, different research designs, and different types of produced
data, the researchers for each study produced the same findings. The Yuste study a qualitative
grounded theory to say that antibiotic prophylaxis is not necessary for uncontaminated clean skin
and that use is dependent on environmental and patient related factors (Yuste, Romo, &
Unamuno, 2015). Another study, Zhou, which analyzed 20 different studies, determined that
antibiotic prophylaxis has no role in reducing the incidences of surgical site infections in elective
laparoscopic cholecystectomies (Zhou, Zhang, Wang, & Hu, 2009). Within the total consensus,
the researchers have determined that antibiotic prophylaxis does not provide any type of
prevention or control in regards to surgical site infection occurrence, and that other factors
(wound location, wound type, comorbidities, and contamination) play a part in surgical site
infection occurrence (Gharde, et al., 2014) (Heal, Buettner, & Drobetz, 2012) (Javaid, Feidberg,
& Gipson, 1998) (Yuste, Romo, & Unamuno, 2015) (Zhou, Zhang, Wang, & Hu, 2009).
Implications of this information would be helpful with several issues. If healthcare
programs could predict or place patient within a surgical site infection probably, and only
administer antibiotics to those at risk for a surgical site infection, antibiotic usage could be
decreased. In essence, the occurrence of superbugs or drug resistant microbes could be curbed or
decreased within hospital setting. One study, Heal, suggests that their study will encourage the
judicial use of prophylactic antibiotics by defining high risk individuals for infection in regards
to skin lesion excisions (Heal, Buettner, & Drobetz, 2012). Another study, Yuste, suggests
prophylaxis for infection of orthopedic devices and other implants does not seem necessary, and
that corresponding specialist should be consulted in cases involving high-risk patients (Yuste,
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
Romo, & Unamuno, 2015). Another study, Zhou, suggests that antibiotic prophylaxis is
unnecessary and should not be routinely used in low-risk elective laparoscopic
cholecystectomies. In essence from all five studies, there is a future study or implication leading
to the decreased use of prophylactic antibiotics and/or the role of prophylactic antibiotics for
high-risk surgical site infection patients.
Limitations
Two limitations were observed during this integrative review. There are a limited number
for studies that were available within the database that were in full text. Some studies available
in full text were not available in English. Some full text studies were on sites that required
payment or membership. In addition, some full text studies in context were more like articles
and not research studies. The second limitation involved the statistical analyses of the
information within some of the studies used within this integrative review. The Gharde, and
Heal studies used the Chi square test; however, none of the studies explain what the Chi square
test is and the significance behind the test (Gharde, et al., 2014) (Heal, Buettner, & Drobetz,
2012). However, the Heal study did provide the purpose for Mann-Whitney-Wilcoxon test,
generalized linear modeling, Poisson distribution, and logarithmic link function were used for
(Heal, Buettner, & Drobetz, 2012). The Zhou study utilized a Jadad composite scale, quality
assessment, odds ratio, and random effect model for its data analysis (Zhou, Zhang, Wang, & Hu,
2009). However, process by which the researchers came up with their findings was not
understood and passed off as a generalized number.
Conclusion
This integrative reviews finding have provided an answer to the use of prophylactic
antibiotic use for those patients in regards to risk of surgical site infection. Findings indicate that
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
10
antibiotic prophylaxis has not significant role in prevention or control of the occurrence of a
surgical site infection. The review continues to signify that there are several risk factors in the
occurrence of a surgical site infection: wound type, wound location, comorbidities of the patient,
and contamination of the site. This integrative review has not only answered a question, it has
also provided a support structure for the sensible use of prophylactic antibiotics. It has also,
provided a basis for the establishment of risk factors associated with surgical site infections and
the effect of antibiotic prophylaxis for high risk surgical site infection patients. However, until
the mandatory use of prophylactic antibiotics is deemed harmful to every surgical patient, the use
of it will be continuing.
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
11
References
Gharde, P., Swarnkar, M., Waghmare, L., Bhagat, V., Gode, D., Wagh, D., . . . Sharma, A. (2014,
January). Role of antibiotics on surgical site infection in cases of open and laparoscopic
cholecystectomy : a comparative observational study. Journal of Surgical Technique &
Case Report. doi:10.4103/2006-8808.135132
Heal, C., Buettner, P., & Drobetz, H. (2012). Risk factors for surgical site infection after
dermatological surgery. International Journal of Dermatology, 796-803.
Javaid, M., Feidberg, L., & Gipson, M. (1998). Primary repair of dog bites to the face: 40 cases.
Journal of the Royal Society of Medicine, 414-416.
Yuste, M., Romo, A., & Unamuno, P. (2015). Antibiotic prophylaxis in dermatologic surgery.
Retrieved from Apps.elsevier.es: http://apps.elsevier.es/watermark/ctl_servlet?
_f=10&pident_articulo=90183736&pident_usuario=0&pcontactid=&pident_revista=403
&ty=46&accion=L&origen=actasdermo&web=www.actasdermo.org&lan=en&fichero=4
03v99n09a90183736pdf001.pdf
Zhou, H., Zhang, J., Wang, Q., & Hu, Z. (2009). Meta-analysis: Antibiotic prophylaxis in
elective laparoscopic cholecystectomy. doi:doi:10.1111/j.1365-2036.2009.03977.x
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
Authors
(Year)
Title of
Article
(Gharde,
et al.,
2014)
Role of
antibiotics
on surgical
site
infection in
cases of
open and
laparoscopi
c
cholecystec
tomy: a
comparativ
e
observation
al study.
Risk
PubMed
Factors for EBSCO
Surgical
Site
Infection
after
dermatologi
cal Surgery.
(Heal,
Buettner,
&
Drobetz,
2012)
Databas Keywords
e
used in
search
PubMed Antibiotics,
EBSCO Prophylactic,
Prophylaxis
Risk Factors
Minor
Procedures
Antibiotics,
Prophylactic,
Prophylaxis
Risk Factors
Minor
Procedures
12
Research
Design
Data Collection
Subjects
Sampling
Methods
Quantitative
Experimental
2 Groups
Interviews on 7th
day or whenever
signs of infection
appeared
Group A
(16-M
26-F)
Group B
(11-M
31-F)
Abdominal
symptoms
with
cholelithiasi
s
convenien
e
Nonprobabilit
Quantitative
Comparative
nonexperimental
Interviews with
general
practitioners and
patients
Demographics,
clinical data, and
body site map
972 patients
nonprobabilit
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
13
(Javaid,
Feidberg,
&
Gipson,
1998)
Primary
Repair of
Dog Bites
to the Face:
40 cases.
PubMed
EBSCO
Antibiotics,
Prophylactic,
Prophylaxis
Risk Factors
Minor
Procedures
Quantitative
Quasiexpermental
Case notes from
April 1994 to
April 1997
17-M
23-F
Within 3
hour of
injury.
Within 1
hour of
injury.
More than 3
hours after
injury.
Convenien
and
probabilit
(Yuste,
Romo, &
Unamun
o, 2015)
Antibiotic
Prophylaxis
in
Dermatolog
ic Surgery.
PubMed
EBSCO
Antibiotics,
Prophylactic,
Prophylaxis
Risk Factors
Minor
Procedures
Qualitative
Grounded
theory
Antibiotic
administration
routes
3 groups
(Oral,
Topical, and
Intravenous)
Convenien
and
probabilit
(Zhou,
Zhang,
Wang, &
Hu, 2009)
Metaanalysis:
Antibiotic
prophylaxis
in elective
laparoscopi
c
cholecystec
tomy.
PubMed
EBSCO
Antibiotics,
Prophylactic,
Prophylaxis
Risk Factors
Minor
Procedures
Qualitative
Generic
research
Previous studies.
Recorded data
20 Relevant
studies
Convenien
and
probabilit
AN INTEGRATIVE REVIEW: PROPHYLACTIC ANTIBIOTIC USE
14
Das könnte Ihnen auch gefallen
- ContentServer - Asp 2Dokument13 SeitenContentServer - Asp 2Nanda Nurdara TaharaNoch keine Bewertungen
- Jurnal Interna UTIDokument8 SeitenJurnal Interna UTIErdika Satria WahyuonoNoch keine Bewertungen
- Integrative Review of Literature: Michael A. GrayDokument17 SeitenIntegrative Review of Literature: Michael A. Grayapi-547657525Noch keine Bewertungen
- Longitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionDokument11 SeitenLongitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionMITA RESTINIA UINJKTNoch keine Bewertungen
- Muzii Et Al., 2020Dokument9 SeitenMuzii Et Al., 2020Jonathan LucisNoch keine Bewertungen
- 3avijeet EtalDokument9 Seiten3avijeet EtaleditorijmrhsNoch keine Bewertungen
- 10.1186@s13756 019 0659 3Dokument12 Seiten10.1186@s13756 019 0659 3RaffaharianggaraNoch keine Bewertungen
- Ijerph 16 03859 v2 PDFDokument13 SeitenIjerph 16 03859 v2 PDFIrwin FitriansyahNoch keine Bewertungen
- Journal BEDAHDokument40 SeitenJournal BEDAHmeitikaNoch keine Bewertungen
- Integrative Review Paper 1Dokument19 SeitenIntegrative Review Paper 1api-273018832Noch keine Bewertungen
- Rab 8Dokument21 SeitenRab 8Belia DestamaNoch keine Bewertungen
- Synthesis Paper Final DraftDokument11 SeitenSynthesis Paper Final Draftapi-332323350Noch keine Bewertungen
- Clinical Research - Vol 1 - Issue 1 - Article - 3Dokument8 SeitenClinical Research - Vol 1 - Issue 1 - Article - 3marnNoch keine Bewertungen
- Link To Publication in University of Groningen/UMCG Research DatabaseDokument13 SeitenLink To Publication in University of Groningen/UMCG Research DatabaseAhmedNoch keine Bewertungen
- JurdingDokument9 SeitenJurdingChristo LimbongNoch keine Bewertungen
- Jurnal FixDokument2 SeitenJurnal Fixuflah_Noch keine Bewertungen
- A Study of Prescription Pattern of Antibiotics in Pediatric In-Patients of Mc-Gann Teaching Hospital Shivamogga Institute of Medical Sciences (SIMS), Shivamogga, Karnataka.Dokument5 SeitenA Study of Prescription Pattern of Antibiotics in Pediatric In-Patients of Mc-Gann Teaching Hospital Shivamogga Institute of Medical Sciences (SIMS), Shivamogga, Karnataka.International Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Knowledge and Attitude of Rational Use of Antibiotics Among General Practitioners, Khartoum Locality, SudanDokument8 SeitenKnowledge and Attitude of Rational Use of Antibiotics Among General Practitioners, Khartoum Locality, SudanInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Ghadah Asaad Assiri, Nada Atef Shebl, Mansour Adam Mahmoud, Nouf Aloudah, Elizabeth Grant, Hisham Aljadhey, Aziz SheikhDokument30 SeitenGhadah Asaad Assiri, Nada Atef Shebl, Mansour Adam Mahmoud, Nouf Aloudah, Elizabeth Grant, Hisham Aljadhey, Aziz SheikhberlianNoch keine Bewertungen
- Pharmacy Education Article Page 107Dokument42 SeitenPharmacy Education Article Page 107Cristine ChubiboNoch keine Bewertungen
- 1741 7015 8 30Dokument8 Seiten1741 7015 8 30Andres HernándezNoch keine Bewertungen
- What Is The Epidemiology of MedicationDokument31 SeitenWhat Is The Epidemiology of MedicationNadial uzmahNoch keine Bewertungen
- Review: The Ef Ficacy and Safety of Probiotics in People With Cancer: A Systematic ReviewDokument11 SeitenReview: The Ef Ficacy and Safety of Probiotics in People With Cancer: A Systematic ReviewNatália LopesNoch keine Bewertungen
- Search BMJ GroupDokument23 SeitenSearch BMJ GroupCharles BrooksNoch keine Bewertungen
- Morimoto 2020Dokument6 SeitenMorimoto 2020Remberto RamosNoch keine Bewertungen
- Antibiotic 02Dokument4 SeitenAntibiotic 02Arslan ShahNoch keine Bewertungen
- Final Research Paper 2015Dokument11 SeitenFinal Research Paper 2015api-312565044Noch keine Bewertungen
- Analisis Minimalisasi Biaya (CMA)Dokument7 SeitenAnalisis Minimalisasi Biaya (CMA)diahsaharaNoch keine Bewertungen
- Ab StewardshipDokument10 SeitenAb StewardshipAdkhiatul MuslihatinNoch keine Bewertungen
- 655 1767 1 PBDokument9 Seiten655 1767 1 PBFARMASI PRIMA HUSADA SUKOREJONoch keine Bewertungen
- Tugas Review JurnalDokument16 SeitenTugas Review JurnalKrisna dan Theresia BestieNoch keine Bewertungen
- Drug Utilisation Study of UTIDokument4 SeitenDrug Utilisation Study of UTIviva.anu24Noch keine Bewertungen
- Jur DingDokument9 SeitenJur DingChristo LimbongNoch keine Bewertungen
- Thu 2012Dokument5 SeitenThu 2012Nadila Hermawan PutriNoch keine Bewertungen
- Double Checking Injectable Medication Administration: Does The Protocol Fit Clinical Practice?Dokument15 SeitenDouble Checking Injectable Medication Administration: Does The Protocol Fit Clinical Practice?Saiful BahriNoch keine Bewertungen
- Combined Use of Antibiotics As A Risk Factor For HDokument15 SeitenCombined Use of Antibiotics As A Risk Factor For HGemala AdillawatyNoch keine Bewertungen
- Alganabi2021 Article SurgicalSiteInfectionAfterOpenDokument9 SeitenAlganabi2021 Article SurgicalSiteInfectionAfterOpenWahyudhy SajaNoch keine Bewertungen
- 2667 PDFDokument6 Seiten2667 PDFMahmudi Sudarsono MNoch keine Bewertungen
- Impact of ASP in IcuDokument8 SeitenImpact of ASP in Icuguilherme_ribeirNoch keine Bewertungen
- Quasi-Experimentos Infect DeseaseDokument8 SeitenQuasi-Experimentos Infect DeseaseAlan MoraesNoch keine Bewertungen
- Clinical Microbiology and InfectionDokument6 SeitenClinical Microbiology and InfectionAccel XtremeNoch keine Bewertungen
- Treatment Outcomes of Multidrug-Resistant Tuberculosis: A Systematic Review and Meta-AnalysisDokument9 SeitenTreatment Outcomes of Multidrug-Resistant Tuberculosis: A Systematic Review and Meta-AnalysisKamalina YustikariniNoch keine Bewertungen
- Pain Management Postop in EthopiaDokument9 SeitenPain Management Postop in EthopiabahrinanikNoch keine Bewertungen
- Antibiotic Prophylaxis in Orthognathic Surgery - An Overview of Systematic ReviewsDokument12 SeitenAntibiotic Prophylaxis in Orthognathic Surgery - An Overview of Systematic ReviewsBruno GuardieiroNoch keine Bewertungen
- SISTEMATIC REVIEW - I Nyoman Triaditya Kresna Putra - 71225050 - 10b.id - enDokument19 SeitenSISTEMATIC REVIEW - I Nyoman Triaditya Kresna Putra - 71225050 - 10b.id - enTriaditya KresnaNoch keine Bewertungen
- Cohort and Case 2020Dokument39 SeitenCohort and Case 2020Providence MuswizuNoch keine Bewertungen
- Endokrin JurnalDokument5 SeitenEndokrin JurnalNiatazya Mumtaz SagitaNoch keine Bewertungen
- PHAR Article 73597 en 1Dokument7 SeitenPHAR Article 73597 en 1AhmadNoch keine Bewertungen
- Different Analgesics Prior To Intrauterine Device Insertion: Is There Any Evidence of Efficacy?Dokument6 SeitenDifferent Analgesics Prior To Intrauterine Device Insertion: Is There Any Evidence of Efficacy?Leonardo Daniel MendesNoch keine Bewertungen
- Knowledge, Attitude and Practices of Antibiotic Usage Among Students From Mumbai UniversityDokument5 SeitenKnowledge, Attitude and Practices of Antibiotic Usage Among Students From Mumbai UniversityFiji IndahNoch keine Bewertungen
- NouwenDokument2 SeitenNouwenmarkinceNoch keine Bewertungen
- Amiks-Ebn ProjectDokument9 SeitenAmiks-Ebn Projectapi-530909386Noch keine Bewertungen
- Journal Homepage: - : IntroductionDokument10 SeitenJournal Homepage: - : IntroductionIJAR JOURNALNoch keine Bewertungen
- Postoperative Nausea and Vomiting at A Tertiary Care Hospital in North-Western TanzaniaDokument9 SeitenPostoperative Nausea and Vomiting at A Tertiary Care Hospital in North-Western TanzaniaAsfaw NurhussenNoch keine Bewertungen
- Probioticos e Pancreatite Aguda SeveraDokument10 SeitenProbioticos e Pancreatite Aguda SeveraYoussef Al ZeinNoch keine Bewertungen
- Knowledge, Attitude and Practice of Antibiotics: A Questionnaire Study Among 2500 Chinese StudentsDokument9 SeitenKnowledge, Attitude and Practice of Antibiotics: A Questionnaire Study Among 2500 Chinese StudentsAnonim musNoch keine Bewertungen
- Quality, safety and EBP glossary 2012Dokument6 SeitenQuality, safety and EBP glossary 2012Hani TuasikalNoch keine Bewertungen
- 2046-4053-2-52Dokument12 Seiten2046-4053-2-52Nitya KrishnaNoch keine Bewertungen
- s12905-015-0196-z Yang TerpilihDokument12 Seitens12905-015-0196-z Yang TerpilihMc'onethree BrownNoch keine Bewertungen
- Phase I Oncology Drug DevelopmentVon EverandPhase I Oncology Drug DevelopmentTimothy A. YapNoch keine Bewertungen
- Nursing PhilosophyDokument5 SeitenNursing Philosophyapi-272448190Noch keine Bewertungen
- Wound DehiscenceDokument8 SeitenWound Dehiscenceapi-272448190Noch keine Bewertungen
- Root Cause Analysis PaperDokument6 SeitenRoot Cause Analysis Paperapi-272448190100% (1)
- Bsmcon20skills20checklist20-Rn bsn1 - Michael PhelpsDokument5 SeitenBsmcon20skills20checklist20-Rn bsn1 - Michael Phelpsapi-272448190Noch keine Bewertungen
- E-Poster Michael PhelpsDokument1 SeiteE-Poster Michael Phelpsapi-272448190Noch keine Bewertungen
- Maintaining Mobility Through ROM ExercisesDokument16 SeitenMaintaining Mobility Through ROM ExercisesAttila Tamas100% (1)
- Pressure Pointer ManualDokument17 SeitenPressure Pointer ManualsorinmoroNoch keine Bewertungen
- ClonazepamDokument2 SeitenClonazepamjhezelle05100% (2)
- Dog Therapy PowerPointDokument99 SeitenDog Therapy PowerPointKörözsi BarbaraNoch keine Bewertungen
- Brochure Ism Eye DiseasesDokument2 SeitenBrochure Ism Eye Diseasesapi-426395895Noch keine Bewertungen
- CancersNaturalEnemy05 2008Dokument144 SeitenCancersNaturalEnemy05 2008devoe.mark6844Noch keine Bewertungen
- Terapii ExperiențialeDokument14 SeitenTerapii ExperiențialeCretu IleanaNoch keine Bewertungen
- Yoga Client Intake Form PDFDokument2 SeitenYoga Client Intake Form PDFΑντώνιος Σακελλάρης0% (1)
- TAT Counselling techniquesDokument5 SeitenTAT Counselling techniquesdhyandevNoch keine Bewertungen
- Freedom at Your FingertipsDokument30 SeitenFreedom at Your FingertipsLucian Grec100% (2)
- MumpsDokument1 SeiteMumpsFikri PutroNoch keine Bewertungen
- Nursing 215 Care Plan 2 FinalDokument7 SeitenNursing 215 Care Plan 2 Finalapi-283303129Noch keine Bewertungen
- Adherence To Antipsychotics in Schizophrenia PDFDokument168 SeitenAdherence To Antipsychotics in Schizophrenia PDFCosmin Ungureanu100% (1)
- Treatment of Angina Pectoris with VasodilatorsDokument39 SeitenTreatment of Angina Pectoris with VasodilatorsRose AnnNoch keine Bewertungen
- Final Coaching CardioDokument70 SeitenFinal Coaching CardiomarykristiroseNoch keine Bewertungen
- Disturbed Thought Process NCP Gallano May 22 2018Dokument3 SeitenDisturbed Thought Process NCP Gallano May 22 2018Charles Mallari ValdezNoch keine Bewertungen
- Dose and IntervalDokument37 SeitenDose and IntervalRosel Ann BontiaNoch keine Bewertungen
- IVF ComputationDokument21 SeitenIVF ComputationCutay Cristene Mae OrmidoNoch keine Bewertungen
- Higgins 2005Dokument14 SeitenHiggins 2005Maria Nuñez NevarezNoch keine Bewertungen
- Understanding AuriculotherapyDokument4 SeitenUnderstanding AuriculotherapyFelipe de Jesus HernandezNoch keine Bewertungen
- Phys Dys Soap Note WeeblyDokument1 SeitePhys Dys Soap Note Weeblyapi-351572858Noch keine Bewertungen
- Massage & Massage & Massage: Reyes Spa Reyes Spa Reyes SpaDokument2 SeitenMassage & Massage & Massage: Reyes Spa Reyes Spa Reyes SpaEloisa ReyesNoch keine Bewertungen
- Bobath Concept Effectiveness in Stroke RehabDokument15 SeitenBobath Concept Effectiveness in Stroke RehabAfrizal BintangNoch keine Bewertungen
- Panic Self HelpDokument4 SeitenPanic Self HelpWanda FschraNoch keine Bewertungen
- Quality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisDokument15 SeitenQuality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisNarendraNoch keine Bewertungen
- The Georgia Psychotropic Medication Monitoring Project, Jan 2012Dokument62 SeitenThe Georgia Psychotropic Medication Monitoring Project, Jan 2012Rick ThomaNoch keine Bewertungen
- Gestalt TherapyDokument6 SeitenGestalt TherapyLily lyka PranillaNoch keine Bewertungen
- Project Echo Didactic On Somatic Symptom Disorder 04022015Dokument25 SeitenProject Echo Didactic On Somatic Symptom Disorder 04022015Iswaran AmpalakanNoch keine Bewertungen
- NCP Nutrition Assesment MatrixDokument22 SeitenNCP Nutrition Assesment MatrixPoschita100% (1)
- Bioscalar Energy: The Healing PowerDokument4 SeitenBioscalar Energy: The Healing PowerSagarsinh RathodNoch keine Bewertungen