Beruflich Dokumente
Kultur Dokumente
Health System Improvement Slides
Hochgeladen von
api-300842084Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Health System Improvement Slides
Hochgeladen von
api-300842084Copyright:
Verfügbare Formate
12/2/15
Care
Delivery Model: Team Nursing and Multidisciplinary
o STICU at BUMC
o Type of care: Emergent and Critical Care
o Conditions: TBI, GSW, Burns, and MVA
o Services: RT, PT, OT, Case Management, Social Work
o 20 beds
o Nurse to patient ratio
Madison Bardsley, Kevin Cornett, Mariya Isarevich, Rayna McParlane,
Michelle Splaver
12/2/2015
1:1 or 1:2
Nursing
leadership includes Clinical Nurse Leader and
Nurse Manager
Leadership positively influences care
o
o
o
o
o
o
o
Why
Currently there is a basic patient
organization form, but not
evidence-based or standardized
This leads to inconsistencies
when transferring patients
Banner supports this unit
through:
o Providing resources to
succeed, CEUs, recognition of
nurses, promoting team
environment
Ensures the staff has equipment needed
Teamwork encouraged through nurse rounds
Mandates and encourages ongoing education
Equal opportunity/work environment
Empowers nurses
Holds nurses accountable
Strives for constant improvement of unit
is strong leadership important?
o Studies show that positive leadership, such as relational
leadership, results in improved patient outcomes (Wong,
Cummings & Ducharme, 2013).
Patient
Interdisciplinary
teamwork
supporting patient-centered
care
Focus
o Implementation of individualized care
o Leadership rounds and check patient/family satisfaction
o Committed to exceptional patient care
Staff
o
o
o
o
o
o Clear and receptive
communication
Focus
Continuing education
Collaborative patient assignment process
Staff support with complex patients
Importance of staff wellbeing/debriefing (Keene, et al., 2010).
Voices are heard
o Universal respect and trust
o Interdisciplinary collaboration
o Valuing specific roles of each
individual
o Overall improves patient care
outcomes and patient
satisfaction (Wen & Schulman,
2014)
6
12/2/15
Integration
Quality
improvement activities
o Concurrent Audits occur daily
o Data directly impacts the quality of Pt care
Both the nurse manager and clinical leader are in
charge of these audits
Examples- Catheter Associated Urinary Tract Infection
(CAUTI) and central line audits
of information with patients
o Patient education, family education, language translation
resources, My Chart
Integration
of information with providers and staff
o EPIC, cellphones/pagers, physician/resident available on
unit, pre-shift meeting
Integration
of information with technology
o EPIC, Pyxis, patient barcode scanning, online policies,
electronic EKG
7
Concurrent
and process
audits to assess compliance
after improvements
Organization
support issue
o Patient handoff during report on Trauma ICU
Patient
handoff to Trauma ICU can be unclear
leads to decreased patient outcomes,
quality of care, and safety
Specific problems seen on Trauma ICU
o Re-Audits
o Accountability checks
for CNLs performing
audits
Miscommunication
Data
reported back to
nursing staff
o Individual meetings
o Results publicly posted
9
10
In
order to implement our intervention of providing a
standardized shift report we as the unit leader would:
Pilot
of evidencebased, standardized
report tool in Trauma
ICU
o
o
o
o
o
o See Handouts!
Goal:
Decrease
miscommunication and
consequential errors
11
Month 1- plan intervention and design seminar
Month 2- hold 3 seminars for Trauma ICU staff
Month 3- initiate standardized shift report on the unit
Month 4- Progress report with staff
Month 6- Evaluate intervention
12
12/2/15
Cresswell,
K. M., Bates, D. W., & Sheikh, A. (2013). Ten key
considerations for the successful implementation and adoption
of large-scale health information technology. Journal of the
American Medical Informatics Association, 20(e1), 9-13.
doi:http://dx.doi.org/10.1136/amiajnl-2013-001684
Jukkala, A.M., James, D., Autrey, P., Azuero, A., & Miltner, R.
(2012). Developing a standardized tool to improve nurse
communication during shift report. Journal of Nursing Care
Quality, 27(3), 240-246. doi: 10.1097/NCQ.
0b013e31824ebbd7
Keene, E. A., Hutton, N., Hall, B., & Rushton, C (2010).
Bereavement debriefing sessions: An intervention to support
health care professionals in managing their grief after the
death of a patient. Pediatric Nursing, 36(4), 185-189.
Retrieved from http://www.medscape.com/viewarticle/729872
13
Lacroix, D. Management, leadership, power and politics [PDF
document]. Retrieved from Lecture Notes Online Website
https://d2l.arizona.edu/d2l/le/content/434224/viewContent/3634
200/View
Marquis, B.L. & Huston, C.J. (2015). Leadership roles and
management functions in nursing. Philadelphia, PA: Wolters
Kluwer Health
UC Irvine Health (2015). Traumatic and critical care surgery
services: Conditions and treatments. Retrieved from
http://www.ucirvinehealth.org/medical-services/trauma-criticalcare-surgery/conditions-treatments/
14
Wong,
C. A., Cummings, G. G., & Ducharme, L.
(2013). The relationship between nursing
leadership and patient outcomes: A systematic
review update. Journal of Nursing Management,
21, 709-724. doi:10.1111/jonm.12116
Wen, J., & Schulman, K. A. (2014). Can team based
care improve patient satisfaction? A systematic
review of randomized control trials. PLoS
ONE, 9(7). doi:10.1371/journal.pone.0100603
15
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- C305 - QTO Workshop PDFDokument90 SeitenC305 - QTO Workshop PDFJason SecretNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Massey Ferguson MF7600 Technician Workshop ManualDokument798 SeitenMassey Ferguson MF7600 Technician Workshop Manualgavcin100% (5)
- CA-idms Ads Alive User Guide 15.0Dokument142 SeitenCA-idms Ads Alive User Guide 15.0svdonthaNoch keine Bewertungen
- Reviewer For Bookkeeping NCIIIDokument18 SeitenReviewer For Bookkeeping NCIIIAngelica Faye95% (20)
- Handbook - European Choral AssociationDokument24 SeitenHandbook - European Choral AssociationMonica SaenzNoch keine Bewertungen
- (Essential Skills For Nurses Series) Philippa Sully - Joan Dallas-Essential Communication Skills For Nursing and Midwifery-Mosby - Elsevier (2010) PDFDokument250 Seiten(Essential Skills For Nurses Series) Philippa Sully - Joan Dallas-Essential Communication Skills For Nursing and Midwifery-Mosby - Elsevier (2010) PDFRetno SumaraNoch keine Bewertungen
- Sample Engagement LetterDokument5 SeitenSample Engagement Letterprincess_camarilloNoch keine Bewertungen
- CS1 Entity Level Controls SolutionsDokument16 SeitenCS1 Entity Level Controls SolutionsPakistan Breaking News100% (6)
- Professional Development SlidesDokument2 SeitenProfessional Development Slidesapi-300842084Noch keine Bewertungen
- Ebp PresentationDokument4 SeitenEbp Presentationapi-300842084Noch keine Bewertungen
- Basic Ekg CertDokument1 SeiteBasic Ekg Certapi-300842084Noch keine Bewertungen
- 478 Development GridDokument3 Seiten478 Development Gridapi-300842084Noch keine Bewertungen
- NW Clinical OrientationDokument1 SeiteNW Clinical Orientationapi-300842084Noch keine Bewertungen
- Code CompDokument1 SeiteCode Compapi-300842084Noch keine Bewertungen
- Glucose CompDokument1 SeiteGlucose Compapi-300842084Noch keine Bewertungen
- Stanford Unofficial TranscriptDokument1 SeiteStanford Unofficial Transcriptapi-300842084Noch keine Bewertungen
- Pandemic Disaster Preparedness 2014 CertificationDokument2 SeitenPandemic Disaster Preparedness 2014 Certificationapi-300842084Noch keine Bewertungen
- Ip Senior Mentor ProgramDokument1 SeiteIp Senior Mentor Programapi-300842084Noch keine Bewertungen
- Ucla Cover Letter UpdatedDokument1 SeiteUcla Cover Letter Updatedapi-300842084Noch keine Bewertungen
- N479 Professional Activity Evaluation Form Describe The Community Service/professional Activity/s You Attended or Participated WithDokument2 SeitenN479 Professional Activity Evaluation Form Describe The Community Service/professional Activity/s You Attended or Participated Withapi-300842084Noch keine Bewertungen
- 478 Job DescriptionDokument1 Seite478 Job Descriptionapi-300842084Noch keine Bewertungen
- Ua College of Nursing Skills ListDokument22 SeitenUa College of Nursing Skills Listapi-300842084Noch keine Bewertungen
- Peter Letter of RecDokument1 SeitePeter Letter of Recapi-300842084Noch keine Bewertungen
- Ihi Certificate - Ihi Open School Certificate of CDokument1 SeiteIhi Certificate - Ihi Open School Certificate of Capi-301431860Noch keine Bewertungen
- Laura Letter of RecDokument1 SeiteLaura Letter of Recapi-300842084Noch keine Bewertungen
- 478 Goals CertificationDokument1 Seite478 Goals Certificationapi-300842084Noch keine Bewertungen
- Jessica Letter of RecDokument1 SeiteJessica Letter of Recapi-300842084Noch keine Bewertungen
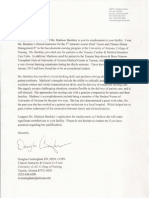
- Reference Letter - DougDokument1 SeiteReference Letter - Dougapi-300842084Noch keine Bewertungen
- Certificate - Workplace Violence PreventionDokument1 SeiteCertificate - Workplace Violence Preventionapi-300842084Noch keine Bewertungen
- Job Resume PDFDokument2 SeitenJob Resume PDFapi-300842084Noch keine Bewertungen
- L15 PDFDokument15 SeitenL15 PDFlesNoch keine Bewertungen
- Why Do Kashmiris Need Self-Determination?: UncategorizedDokument16 SeitenWhy Do Kashmiris Need Self-Determination?: UncategorizedFarooq SiddiqiNoch keine Bewertungen
- Et200sp Im 155 6 PN ST Manual en-US en-USDokument47 SeitenEt200sp Im 155 6 PN ST Manual en-US en-USayaz officeNoch keine Bewertungen
- APS PresentationDokument32 SeitenAPS PresentationRozack Ya ZhackNoch keine Bewertungen
- Celestino vs. CIRDokument6 SeitenCelestino vs. CIRchristopher d. balubayanNoch keine Bewertungen
- UNIT 4 Digital Integrated CircuitsDokument161 SeitenUNIT 4 Digital Integrated CircuitssimhadriNoch keine Bewertungen
- 88 Year Old Man Missing in SC - Please ShareDokument1 Seite88 Year Old Man Missing in SC - Please ShareAmy WoodNoch keine Bewertungen
- Pe8 Mod5Dokument16 SeitenPe8 Mod5Cryzel MuniNoch keine Bewertungen
- Al Multaqaa Presentation v2Dokument22 SeitenAl Multaqaa Presentation v2Hasaan WaheedNoch keine Bewertungen
- CR-805 Retransfer PrinterDokument2 SeitenCR-805 Retransfer PrinterBolivio FelizNoch keine Bewertungen
- A Review On Different Yogas Used in The Management of Mandali Damsa Vrana W.S.R. To KriyakaumudiDokument11 SeitenA Review On Different Yogas Used in The Management of Mandali Damsa Vrana W.S.R. To KriyakaumudiTiya TiwariNoch keine Bewertungen
- No Experience ResumeDokument2 SeitenNo Experience ResumeNatalia PantojaNoch keine Bewertungen
- Spike Magazine Cup PackDokument5 SeitenSpike Magazine Cup PackBungle MarleyNoch keine Bewertungen
- Victaulic-FP-FireLock Fire-Pac Series 745 PreactionDokument9 SeitenVictaulic-FP-FireLock Fire-Pac Series 745 PreactionTấn ĐạtNoch keine Bewertungen
- CfoDokument13 SeitenCfocarmen pirvanNoch keine Bewertungen
- Risk Assessment For ExcavationDokument6 SeitenRisk Assessment For ExcavationAhmed GamalNoch keine Bewertungen
- Digital ThermometerDokument12 SeitenDigital Thermometershahpatel19Noch keine Bewertungen
- 3rd Quarter SUMMATIVE TEST in MAPEHDokument3 Seiten3rd Quarter SUMMATIVE TEST in MAPEHzaile felineNoch keine Bewertungen
- Taxonomy: Family StaphylococcaceaeDokument40 SeitenTaxonomy: Family StaphylococcaceaeMarissa Terrado SorianoNoch keine Bewertungen
- January 11, 2019 Grade 1Dokument3 SeitenJanuary 11, 2019 Grade 1Eda Concepcion PalenNoch keine Bewertungen
- Cambridge IGCSE Physics 0625 Complete Notes PDokument5 SeitenCambridge IGCSE Physics 0625 Complete Notes PYamikani ManthandoNoch keine Bewertungen
- Luyện nghe Tiếng Anh có đáp án: I/ Listen and complete the textDokument3 SeitenLuyện nghe Tiếng Anh có đáp án: I/ Listen and complete the textVN LenaNoch keine Bewertungen