Beruflich Dokumente
Kultur Dokumente
Group D Ebp Presentation 2
Hochgeladen von
api-301506104Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Group D Ebp Presentation 2
Hochgeladen von
api-301506104Copyright:
Verfügbare Formate
1
Improving Pa-ent-Nurse Communica-on in the ICU
Se9ng: A Best Prac-ce Recommenda-on
PICOT Ques-on
Introduc-on
Issue:
Current prac-ce for communica-on with mechanically
ven-lated, conscious pa-ents is impaired due to the lack of
educa-on and resources available to ICU nurses.
Signicance:
Lack of nurse-pa-ent communica-on can lead to lengthy
hospital stays and adverse pa-ent outcomes ul-mately
resul-ng in decreased pa-ent sa-sfac-on.
Devyn Weber Rayna McParlane
Kaitlyn Parks Pa-ence Bekoe
Marlee Feinholz Lauren Grin
Mary Sepulveda Madison Bardsley
(Otuzoglu & Karahan, 2014)
In the popula-on of non-speaking,
intubated, ICU pa-ents with a GCS score
of 13 or higher, how does the use of the
illustra-ve and
assis-ve communica-on
devices, when compared
to current prac-ce,
inuence the overall
pa-ent-nurse
communica-on aYer a
single 12-hour shiY?
(Tingsvik, Bexell, Andersson, & Henricson, 2013)
Summary of Current Prac-ce
Within various ICU se9ngs, there are
no well-established levels of
communica-on between nurses and
their pa-ents.
Examples of current methods include:
Lip reading, gestures, wri^en
messages, head nodding, subjec-ve
provider interpreta-on, and the use of
alphabet boards
(Otuzoglu & Karahan, 2014)
(Happ et al., 2014)
Nega-ve Outcomes Associated with
Current Prac-ce
Current Prac-ce Regula-ons
Na#onal Prac#ce
American Associa-on of Cri-cal Care Nursing denes access to appropriate tools
for eec-ve nurse-pa-ent communica-on to be a cri-cal element, though a
formal policy is not implemented.
1) Increased Risk for Aspira-on
Lip reading, head-nodding, and excessive upper-body
movements may increase the risk for ven-lated pa-ents to
aspirate oropharyngeal contents, enhancing their likelihood for
injury or respiratory infec-on
State of Arizona
Suggests the prac-ce of u-lizing eec-ve communica-on strategies throughout
ICU admi^ance, though no formal policy is implemented.
Banner UMC
Evalua-on of pain and physiological needs will be assessed via the Cri-cal-Care
Pa-ent Observa-on Tool (CPOT), a behavioral scale relying on providers personal
interpreta-on of pain and physiological needs.
2) Increased Oxygen Demand
Excessive movement increases a pa-ents oxygen demand
which commonly leads to nega-ve hemodynamic altera-ons
(Banner Health, 2011)
(American Assoication of Critical Care Nursing, 2005)
(Otuzoglu & Karahan, 2014)
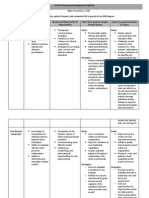
Synopsis of Current Literature
Synopsis of Current Literature
Synopsis of Current Literature
What is the issue with current prac-ce?
Best Prac-ce: Why is it important?
Solu-ons to current prac-ce issue:
In order to evoke change, evidence based interventa-ve
strategies include:
The use of visual diagrams allowing
pa-ents and nurses to point out
specic pa-ent needs
Clinical educa-on to teach nurses about
the use of low-tech communica-on
devices including spiral notebooks,
whiteboards, and whiteboard markers.
Basic pa-ent needs including toile-ng, pain management,
reposi-oning, and emo-onal and social support are
ineec-vely being met with current prac-ce.
Improving the communica-on between nurses and pa-ents in
the ICU will increase
sa-sfac-on and create less
trauma-c experiences for the
pa-ents.
37.7% of ven-lated ICU pa-ents
report unsuccessful a^empts at
eec-vely communica-ng their
pain with their nurse.
(Happ, et al., 2011)
(Otuzoglu & Karahan, 2014)
(Karlsson, Forsberg & Bergbom, 2011)
10
Synopsis of Current Literature
(Happ et al., 2014)
11
12
Synopsis of Current Literature
Summary of Strengths and Limita-ons...
Why change is necessary:
Why change is necessary:
Pa-ents view the ICU environment as unfamiliar and feel that
they have no impact on how it is organized, which leads to
dependency, especially on the nursing sta.
ICU pa-ents commonly report feelings of frustra-on, lack
of control/self-determina-on, and physical discomfort
during their stay in the ICU.
Being voiceless creates a loss of pa-ent freedom and
personhood
(Otuzoglu & Karahan, 2014)
(Karlsson, Forsberg & Bergbom, 2011)
Pa-ents feel that they
are unable to build
trust and condence in
their nurse, resul-ng in
self-reliance for their
survival.
Review of literature iden-es the need for:
Educa-on for ICU nurses on best prac-ce
Assis-ve communica-on devices and strategies
(Karlsson, Forsberg & Bergbom, 2011)
13
Training classes leY the
nurses feeling less
frustrated when
communica-ng with nonspeaking pa-ents.
14 out of 15 nurses felt that
the class was benecial.
15
Assis-ve Communica-on Devices and
Strategies
Educa-ng ICU Nurses on Best Prac-ce
Strengths
14
Limita#ons
Elevated cost for training
Small sample size was
tested (n=15)
Training was -me
consuming for both the
sta and hospital
(Radtke, Tate, & Happ, 2012)
16
Strengths
Limita#ons
Tes-ng to narrow sample size
to exclude pa-ents with vision
loss, demen-a, orienta-on or
confusion disorders or
linguis-cs problems to prevent
skewed data
Nurses approve simplicity of
comprehension and
applica-on of devices and
strategies
Studies included narrow
pa-ent popula-ons
Change in pa-ent condi-on
altered the par-cipa-on in the
study
Pa-ents had diculty
remembering the
communica-on material due
to eects of seda-on
Evidence Based Nursing
Recommenda-ons
1. ICU nurses should complete educa-on seminar
addressing best prac-ce communica-on techniques
This seminar should include teaching the use of illustrated
communica-on materials and low-tech devices
2. Hospitals should implement the use of illustrated
pa-ent materials and low-tech devices in every pa-ent
room in various ICU se9ngs.
(Otuzoglu & Karahan, 2014)
(Happ et al., 2014)
17
Overall Applica-on/Implementa-on to
Nursing Prac-ce
18
Overall Applica-on/Implementa-on to
Nursing Prac-ce
Implementa-on for Recommenda-on 2:
Implementa-on for Recommenda-on 1:
Schedule a paid-for, one-hour seminar for currently employed ICU
nurses.
Newly-hired ICU nurses will be required to complete the paid-for,
one-hour seminar as part of their New Hire Orienta-on
The seminar will include demonstra-on of how to use the
illustra-ve assis-ve devices as well as teaching the pa-ents on how
to use them.
The Clinical Nurse Manager on each ICU unit will purchase supplies
with hospital funding including a diagram, white board, and
markers for each pa-ent room.
Implement a procol sugges-ng that upon admission of a nonspeaking pa-ent to the ICU, the nurse will instruct the pa-ent
about the use of the diagram and white board.
(Radtke, Tate, & Happ, 2012)
19
20
21
Detailed Cost Analysis
Recommenda-on 1: Educa-on
Average hourly pay rate for ICU nurses at BUMC: $24 - $30
Number of nurses staed in ICUs at BUMC:
90
Cost to pay nurses to a^end the 1-hour seminar:
$2,160 - $2,700
Room reserva-on (College of Medicine room 5403):
$0.00
Cost of educator:
$174.55
Cost to run PowerPoint and a Projector:
$0.00
Refreshments for each nurse in a^endance:
$37.29
Total: $2,371.84 - $2,911.84
(Otuzoglu & Karahan, 2014)
22
23
Risk vs. Benet to Hospital
Detailed Cost Analysis
Risk
Recommenda-on 2: Materials and Supplies
Whiteboard (2 cases of 48 boards, totalling 96 boards): $153.90
Markers (6 packs of 12 markers, totalling 72 markers):
$24.30
Paper for prin-ng (80 diagrams, 500 surveys):
$7.39
Color toner to print (prints up to 1,300 pages): $80.99
Lamina-on for 80 diagrams:
$160.00
Loss of money due to lack of
implementa-on of educa-on
Loss of money due to not using
supplied materials
Benet
Hospital gains be^er pa-ent
sa-sfac-on
Less cost to the hospital with
eec-ve implementa-on due to
shorter hospital stay
Total: $426.58
(Bulk Office Supply, 2015)
(Costco, 2015)
(Otuzoglu & Karahan, 2014)
(Otuzoglu & Karahan, 2014)
24
Risk vs. Benet to Pa-ent
Risk
Benet
Diagram could become inaccessible
due to misplacement
Level of pa-ent educa-on may
limit understanding of material
Dependent upon nurses
willingness to teach and implement
Decrease the chance of adverse
pa-ent events including:
Risk of aspira-on, changing
oxygen levels, and an increased
risk for injury.
Increased pa-ent-nurse
communica-on and sa-sfac-on
Reduc-on of pa-ent powerlessness
Improves nurses -me
management resul-ng in
priori-za-on of pa-ent needs
(Otuzoglu & Karahan, 2014)
25
Evalua-on
Summary
At the end of a single 12-hour shiY, the pa-ents will be
asked by the nurse to report their sa-sfac-on at a 5 with
the implemented communica-on techniques according to a
1-5 facial expressions scale.
28
References
American Associa-on of Cri-cal Care Nursing [AACN]. (2005). AACN standards for establishing and sustaining healthy
work environments. Retrieved from h^p://www.aacn.org/wd/hwe/docs/hwestandards.pdf
Banner Health. (2011). Policy and procedure. Retrieved from h^p://www.bannerhealth.com/NR/rdonlyres/
559C0B25-C5E1-4875-9372-77BFFF85F140/62013/MedicalRecordAbbrevia-onsandSymbols37885.pdf
Bulk Oce Supply. (2015). Wholesale pricing made easy. Retrieved from h^p://www.bulkocesupply.com/
guidedsearch.aspx?keyword=whiteboard+markers&mxp=50
Costco. (2015). Beverages: SoA drinks. Retrieved from http://www2.costco.com/Browse/Product.aspx?
prodid=11223431&whse=BD_827&topnav=b
Happ, M.B., Garre^, K.L., Tate, J.A., DiVirgilio, D., Houze, M.P., Demirci, J.R., & Sereika, S.M. (2014). Eect of a
mul--level interven-on on nurse-pa-ent communica-on in the intensive care unit: Results of the SPEACS trial.
Heart & Lung: The Journal of Acute and CriGcal Care, 43(2), 89-98. doi: 10.1016/j.hrtlng.2013.11.010
Happ, M.B., Garre^, K., Thomas, D.D., Tate, J., George, E., Houze, M., Radtke, J., & Sereika, S. (2011). Nurse-pa-ent
communica-on interac-ons in the intensive care unit. American Journal of CriGcal Care: An Ocial PublicaGon,
American AssociaGon of CriGcal-Care Nurses, 20(2) e28-e40. doi: 10.4037/ajcc2011433
Karlsson, V., Forsberg, A., & Bergbom, I. (2012). Communica-on when pa-ents are conscious during respirator
treatment A hermeneu-c observa-on study. Intensive and CriGcal Care Nursing, 28(4), 197-207. doi: 10.1016/
j.iccn.2011.12.007
Otuzoglu, M. & Karahan, A. (2014). Determining the eec-veness of illustrated communica-on material for
communica-on with intubated pa-ents at an intensive care unit. InternaGonal Journal of Nursing PracGce, 20(5),
490-498. doi: 10.1111/ijn.12190
Radtke, J.V., Tate, J.A., & Happ, M.B. (2011). Nurses percep-ons of communica-on training in the ICU. Intensive and
CriGcal Care Nursing, 28, 16-25. doi: 10.1016/j.iccn.2011.11.005
Tingsvik, C., Bexell, E., Andersson, A., & Henricson, M. (2012). Mee-ng the challenge: ICU nurses' experience of
lightly sedated pa-ents. Australian CriGcal Care, 26, 124-129. doi: 10.1016/j.aucc.2012.12.005
26
Problem:
Current prac-ce allows for inadequate nurse-pa-ent
communica-on among ven-lated ICU pa-ents
Poor communica-on increases pa-ents risk for adverse
events and increased dura-on of ICU admission
What can we do?
Improving the communica-on between nurses and pa-ents
in the ICU will increase sa-sfac-on and create less trauma-c
experiences for the pa-ents.
Assis-ve and illustra-ve communica-on techniques are
evidence based solu-ons to improving ven-lated pa-ent
communica-on
27
Why is it necessary?
Pa-ents view the ICU environment as unfamiliar and feel
that they have no impact on how it is organized, which leads
to dependency, especially on the nursing sta.
Lets get implemen-ng!
Oering educa-onal classes
and implemen-ng bedside
assis-ve communica-on
diagrams are feasible
interven-ons to improve
nurse-pa-ent
communica-on in the
ICU.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- ProfdevgridDokument7 SeitenProfdevgridapi-301506104Noch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- ConskillsDokument2 SeitenConskillsapi-301506104Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Nurs478 Healthcaredelivery Group 5Dokument3 SeitenNurs478 Healthcaredelivery Group 5api-301522421Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- ParkskDokument41 SeitenParkskapi-301506104Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- ParksprofessionalactivitypaperDokument2 SeitenParksprofessionalactivitypaperapi-301506104Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- 478 CoverletterDokument1 Seite478 Coverletterapi-301506104Noch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Parkskaitlynresume 11 2015Dokument1 SeiteParkskaitlynresume 11 2015api-301506104Noch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- VUJ ObstructionDokument2 SeitenVUJ ObstructionSheikh Mizanur RahmanNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Update On Stemi Management: Dr. Adi Purnawarman, SP - JP (K) - Fiha.,FasccDokument39 SeitenUpdate On Stemi Management: Dr. Adi Purnawarman, SP - JP (K) - Fiha.,FasccArfiska Ridha Fausa 'ucha'Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- BIOPSY Oral SurgeryDokument34 SeitenBIOPSY Oral SurgeryNisha ChoudharyNoch keine Bewertungen
- Introduction To Critical Care NursingDokument10 SeitenIntroduction To Critical Care NursingRENEROSE TORRES0% (1)
- Septum Drill Kit: User Manual Ver.01Dokument12 SeitenSeptum Drill Kit: User Manual Ver.01Ashok ChaurasiaNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Diabetic Ketoacidosis Protocol PICU Oct 2010 2Dokument9 SeitenDiabetic Ketoacidosis Protocol PICU Oct 2010 2Vidini Kusuma AjiNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- ReferatDokument35 SeitenReferatYuni AurraNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Bruxism (Tooth Grinding) in Adults: SymptomsDokument3 SeitenBruxism (Tooth Grinding) in Adults: SymptomsalgaipNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Chapter 9: Communication and The Therapeutic RelationshipDokument3 SeitenChapter 9: Communication and The Therapeutic RelationshipKINDATNoch keine Bewertungen
- PROSTHODONTICS SEMINAR II Topics 1Dokument1 SeitePROSTHODONTICS SEMINAR II Topics 1Jalil Enock0% (1)
- Neonatal Resuscitation DrugsDokument4 SeitenNeonatal Resuscitation Drugsblast2111Noch keine Bewertungen
- Assessment Explanation Objectives Interventions Rationale Evaluation (AEORIEDokument3 SeitenAssessment Explanation Objectives Interventions Rationale Evaluation (AEORIEMjhay Montemayor100% (1)
- Leaked Sha Covid-19 PlanDokument20 SeitenLeaked Sha Covid-19 PlanKatelyn Guignard100% (1)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Certificate and Duties and ResponsibilitiesDokument2 SeitenCertificate and Duties and ResponsibilitiesShiredan Rose BagarinaoNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- PESTLE Analysis of Square PharmaDokument3 SeitenPESTLE Analysis of Square PharmaMuddasir NishadNoch keine Bewertungen
- Oral Antidiabetic DrugsDokument2 SeitenOral Antidiabetic DrugshiteshnpednekarNoch keine Bewertungen
- Tonsillitis, Tonsillectomy and Hodgkin's LymphomaDokument5 SeitenTonsillitis, Tonsillectomy and Hodgkin's LymphomaD.E.P.HNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- CASE REPORT-Devyana Enggar TaslimDokument24 SeitenCASE REPORT-Devyana Enggar TaslimvivitaslimNoch keine Bewertungen
- Nursing Swallow ScreenDokument2 SeitenNursing Swallow ScreenAldo Hip NaranjoNoch keine Bewertungen
- Gilbert's SyndromeDokument2 SeitenGilbert's SyndromeClarissa Putri DiarsaNoch keine Bewertungen
- DKADokument64 SeitenDKAAravindhan Gunasekaran PaediatricianNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Cupping & Hijama BookDokument25 SeitenCupping & Hijama BookMatthew GilsonNoch keine Bewertungen
- Hospital Case Study FlexsimDokument2 SeitenHospital Case Study FlexsimMano KanthanathanNoch keine Bewertungen
- Icd 10 Chapter XviiiDokument2 SeitenIcd 10 Chapter Xviiifebi novrizalNoch keine Bewertungen
- Schizophrenia and HomeopathyDokument5 SeitenSchizophrenia and HomeopathyAlokojjal Banerjee100% (1)
- Veterinary Neurologic Rehabilitation The Rationale For ADokument9 SeitenVeterinary Neurologic Rehabilitation The Rationale For ACarolina Vargas VélezNoch keine Bewertungen
- Buku Objektif Praktek Klinis Keperawatan Iv (PKK Iv) : Nama MahasiswaDokument53 SeitenBuku Objektif Praktek Klinis Keperawatan Iv (PKK Iv) : Nama MahasiswaGamaliel Kevin WinarnoNoch keine Bewertungen
- An Epidemic of DepressionDokument2 SeitenAn Epidemic of DepressionMel Schwartz100% (3)
- Homoeopathic Perspective of Thyroid DisordersDokument20 SeitenHomoeopathic Perspective of Thyroid DisordersSaurav AroraNoch keine Bewertungen
- Drinking Your Own Urine Can Make You StrongDokument16 SeitenDrinking Your Own Urine Can Make You StrongGlenn OrtizNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)