Beruflich Dokumente
Kultur Dokumente
Occupational Profile Weebly
Hochgeladen von
api-293253519Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Occupational Profile Weebly
Hochgeladen von
api-293253519Copyright:
Verfügbare Formate
Running head: OCCUPATIONAL PROFILE AND INTERVENTION PLAN
Occupational Profile and Intervention Plan
Evelyn Babaroudi
Touro University Nevada
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
Occupational Profile
Client Description
Ethan is a 45-year-old Caucasian male with a diagnosis of relapsing-remitting multiple
sclerosis (MS). The client is an active member of the National MS Society and serves the Las
Vegas area as a group leader for a support group for individuals with MS. The client lives with
his wife, daughter, and mother-in-law in a second-story home (2SH) in Henderson, Nevada. His
wife, Terra, functions as the primary caregiver. The client attends support groups twice a week on
Wednesdays and Saturdays. His wife and daughter are present at each support group meeting.
The clients support group takes place on the first Saturday of the month from 11:00 a.m. to
12:00 p.m. As a group leader, his primary duties consist of coordinating meetings, publicizing
events, attending meetings, facilitating discussions on MS, and sharing helpful information
regarding medication and therapy. The clients group focuses on providing support, fostering
friendships, and connecting with other individuals and families living with MS. The client was
recently hired as a Patient Ambassador for Snow Companies. Snow Companies is an agency that
specializes in pharmaceutical marketing and media. As Patient Ambassador, the client will travel
and connect with patients, healthcare professionals, and individuals in the pharmaceutical
industry to share his story.
Reason for Services
Upon review of medical history, signs detected during a neurologic exam, and symptoms
reported by the client, a clinical diagnosis of MS was determined. A definitive diagnosis of MS
was established in 2009 following brain magnetic resonance imaging (MRI) revealing lesions in
two distinct areas of the clients central nervous system (CNS). The clients past medical history
includes depression. The client schedules a visit to his neurologist in Long Beach, California
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
yearly for a physical examination and to discuss new limitations. In addition to this, the client
visits his primary care physician at the VA Southwest Primary Care Clinic in Las Vegas for acute
concerns regarding MS.
The client is not receiving occupational therapy (OT) services at the present time,
however is seeking referral to OT at an outpatient clinic to address effects of MS impeding his
daily function. He shared that he wishes to increase independence in daily function. The client
currently utilizes a single-point cane (SPC) for safety and support in functional ambulation. He
utilizes a motorized scooter for day-long events such as trip to the mall or amusement park with
his 7-year-old daughter named Hayley. The client is concerned about fatigue. He shared a
concern about his ability to maintain his group leader position and still have energy to be a father
and husband. The client also complained of recent sensory impairments affecting his fine motor
control. As a result, he is unable to button his clothing in the mornings and requires his wife to
complete the task.
Successful Occupations and Barriers
The client feels successful in his role as a group leader. He enjoys attending support
group meetings as it provides him with the opportunity to meet and interact with the MS
population in Las Vegas. The client is well alert and oriented. He is able to manage his
medication independently and has no reports of pain or discomfort. The clients memory,
attention, and safety awareness are within normal limits. The clients expressive and receptive
language is intact. He has strong interaction skills that allow him to work well with others, a skill
that is crucial to running a support group. The client has a cooperative attitude among the
individuals he interacts with. He has a friendly demeanor and a strong sense of humor. The
Community Development Manager at Nevadas National MS Society expresses how amicable he
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
is and admires his hard work and enthusiasm. The client shares that his success as a group leader,
and his desire to inspire other individuals with MS, serve as a source of motivation.
Prior to MS, the client was independent in all ADLs and IADLs. The client feels that his
activity tolerance has significantly decreased, and fears that this will impact his role as a group
leader. Although he is able to functionally ambulate with a SPC, he feels that he is beginning to
rely on his scooter, particularly in settings such as the support group. The client has an issue with
this as it prevents him from standing up and making appropriate eye-contact with the audience.
The client reported frustration with his balance and ability to remain standing during support
group meetings. As previously mentioned, sensory loss has contributed to weakness in fine
motor skills. This inhibits his ability to complete dressing independently. Further, the client
explained that he has trouble with meal preparation due to decreased in-hand manipulation and
coordination skills. The client also has poor activity tolerance, decreased endurance, and
increased levels of fatigue. He feels he has become a burden on his wife, as he is unable to
participate in activities with his daughter without her assistance. The client also complains of
poor dynamic standing balance and decreased activity tolerance. He feels that he is losing
endurance and would like to push harder to fight MS.
Contexts and Environments
As previously stated, the client lives in a 2SH home in Henderson with his wife,
daughter, and mother-in-law. The clients home is tidy and uncluttered. The master bedroom and
bathroom are located on the first floor where the client and his wife sleep. The clients daughter
and mother-in-law both have separate rooms upstairs. In the bathroom, the client has grab bars
and a tub-transfer bench (TTB) for bathing.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
The client lives in a gated community. He stated that his neighborhood is generally very
peaceful and safe. The family has a small dog that sleeps in the office. The client also has a large
garden in the backyard where he and his family spend time on weekends. There are no stairs in
the garden or backyard, therefore the client is able to navigate the area with ease. As previously
stated, the client functionally ambulates in the home using a SPC for safety and support. He uses
a motorized scooter in the community.
The client uses private transportation to travel to the support group, which take place at a
local church. The group meets in a seminar room that is located downstairs. The client was
previously utilizing a SPC, but has begun using his electric scooter at meetings, which allows
him to navigate around the room to interact with others. The client fears that he is becoming too
dependent on the scooter, and wishes to go back to using a SPC. The client enjoys attending
support group meetings and welcoming new members to the MS community.
Occupational History
The client is originally from Ann Arbor, Michigan. He completed his Bachelors of Arts
degree in Criminal Justice at the University of Michigan in 1997. Following his undergraduate
education, the client pursued a career in law enforcement. The client served as a Security
Policeman in the United States Air Force. Shortly after, the client worked for the police academy
in Michigan. During the end of his probationary period, the client experienced a flare-up.
Subsequently, the client resigned from his position at the police academy and moved on to
pursue his Master of Business Administration at the University of Michigan. Following the
completion of his MBA in 2009, the client was diagnosed with MS.
The client moved to Nevada five years ago with his wife, daughter, and mother-in-law.
His son, from a previous marriage, still lives in Michigan, however frequently visits and keeps in
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
touch through telephone and email. The client shared that his journey with MS has brought him
closer to his family, and has taught him to be a better and loving husband and father.
Values and Interests
Information regarding the clients values and interests were gathered through interview.
The client expressed that he enjoys mindfulness meditation as a means to coping with stress. The
client also enjoys yoga. He shared that yoga has positive effects on his psychosocial health. The
client shares a strong sense of connectedness to his community and frequently engages in
religious group activities. He and his family attend church every Sunday. The client values his
relationship with God and prays on a regular bases.
The client thoroughly enjoys sports and is a big fan of the University of Michigan
football team. Prior to his diagnosis, the client was a cross-country runner and basketball player.
Although he is no longer able to participate in physically demanding sports, he still enjoys
watching sports on television. The client and his wife also attend comedy shows. He expresses
that laughter helps him cope with MS, and in managing the complexity of his illness.
Daily Life Roles
The client is married and has two children. He is a husband, father, and friend. As
previously stated, his daughter is 7-years-old. The clients son, from a previous marriage, is 20years-old and still lives in Michigan with the mother. The clients mother-in-law is 72-years-old
and lives with the family in Las Vegas. The client is an active member of the National MS
Society, and is a group leader for a support group that meets the first Saturday of every month.
Patterns of Occupational Engagement
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
The client shared that he misses his home in Michigan. Prior to MS, his favorite leisure
activities consisted of barbecuing with neighbors, attending sporting events with friends, and
camping outdoors with family. Following his diagnosis, his patterns of occupational engagement
quickly shifted. He experienced a major depressive episode and began alienating himself from
family and friends. He and his wife had difficulty keeping up with medical expenses and decided
to move to Nevada. Since their move, the client no longer spends much time outdoors. Due to
impaired balance, decreased activity tolerance, and fatigue he no longer participates in physically
demanding sports such as, running and playing basketball. Instead, the client and his wife occupy
their time with church, support groups, and comedy shows. Following MS, the client spends
more time with the church community, which he minimally did in the past.
Clients Priorities and Desired Outcomes
The client realizes he is now requiring more assistance from his family and wishes to
increase his level of independence in all areas of ADL and IADL function. He wishes to increase
his activity tolerance and to maintain his position as a group leader. The client is also concerned
about his new job as Patient Ambassador, including his upcoming trip to Chicago, Illinois for
training. Furthermore, the client expressed concern regarding his balance and safety during
performance of activities in the home and community. He would like to improve his occupational
performance in dressing, and to manage buttoning of shirts independently without request for
assistance from a caregiver. Lastly, the client stated that he would like to lead his support groups
in a standing position, and tolerate moving around the environment with a SPC.
Occupational Analysis
Context and Setting
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
The client is a member of the National MS Society, a nonprofit organization that
advocates for individuals living with MS. As previously stated, the clients neurologist is at a
spinal cord injury (SCI) clinic in Long Beach, CA, whom he visits annually for physical exams
and to discuss new limitations. The clients primary physician is at the VA Southwest Primary
Care Clinic in Las Vegas. The client is seeking referral to OT to facilitate independence and
safety in ADL and IADL function.
The client will receive services at an outpatient rehabilitation clinic. The client will
receive treatment one hour per day, twice a week. The outpatient clinic will provide opportunities
to enhance and maintain physical, emotional, and psychological function. A skills lab, an open
and shared environment, will be available to implement functional and occupation-based
activities to promote independence in ADL and IADL function. The facility will also provide a
rehab gym for exercise groups, education and training with use of DME and A/E, and
rehabilitative technology and equipment to increase the clients performance in daily life roles.
Home-based services will also be provided as needed. The clinic will also provide individual
rooms with a quiet and private environment for intervention and assessment purposes.
Activity Performance
Analysis of occupational performance was used to gather information about the clients
participation within the social and physical environment, and to indicate any supports or barriers
related to function. Observation skills were used to assess the way in which the client functions
in the natural context. The client was observed at a local coffee shop. The interview was
scheduled before noon in order to respect the clients daily routine. The client takes a nap at 1:00
p.m. in order to help manage fatigue and to conserve energy for other activities throughout the
day. Upon my arrival, the client was seated at a table. His breakfast was served to him at the
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
table. He was able to eat his food independently. The client was able to socialize while eating his
breakfast. He was able to maintain appropriate eye-contact, and was able to carry on a
conversation while eating. When the client finished his breakfast, he transitioned to throw away
his trash. The client used a SPC for safety and support. When transitioning from a seated to
standing position, he used one hand to push off of the seat and the other hand on the cane for
support. Once the client accomplished a standing position, he took a moment to stretch before
walking. This indicated good safety awareness. His base of support was slightly narrow and he
walked at a slower than normal rate. The client demonstrated appropriate use of the cane on the
contralateral side.
Key Observations
Impaired balance and weakness in the lower-extremities were noted through observation
of the clients performance during functional activities. Dynamic standing balance was impaired.
The client required a SPC to functionally ambulate and appeared to have difficulty weightshifting and reaching to throw away his trash. He demonstrated a narrow base of support which
appeared to compromise his balance. Despite these challenges, the displayed good sitting
posture, including feet flat on floor, slight anterior pelvic tilt, erect spine, and head over shoulder
and shoulders over hips. The client was able to reach for items across the table without
compromising his balance. The client demonstrated good safety awareness by using both hands
to transition from sitting to standing position. In addition to this, he took a moment to adjust his
posture and stretch his legs before proceeding to walk with proper use of the SPC. Challenges
with fine motor skills and dexterity were noted through observation of the client attempting to
open his napkin. The client stated that this was due sensory impairments. The client was able to
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
10
remain engaged throughout the course of our conversation. As previously stated, he displayed
appropriate eye-contact and was able to remain on-topic during our conversation.
Domains of Occupational Therapy Practice Framework
The client presents deficits in various domains that intrinsically intertwine to affect his
overall functioning. First, changes in the clients ability to engage in leisure occupations or
pursue usual life roles have impacted his psychosocial health. Prior to MS, the client had a very
active lifestyle. He enjoyed running, playing basketball, and spending time outdoors with family
and friends. This shift or transition from an active to sedentary lifestyle has impacted his ability
to participate in previously preferred activities. In addition to this, the client is unable to perform
self-care and functional mobility as safely and independently as he did in the past, and fears that
the symptoms of his illness will increase.
Many client factors significantly impact the clients performance in occupations.
Increased levels of fatigue have lowered his energy and drive. Sensory functions, specifically the
presence of numbness in the fingertips have affected his fine motor skills, specifically manual
dexterity. Muscle power, tone, endurance, and involuntary movement reactions have impacted
postural responses to maintain balance, and deconditioning of unused muscles have exacerbated
weakness in the lower-extremities. Gait patterns have compromised balance and increased risk of
falls.
Specific performance skills have influenced the clients occupational performance,
including: aligns, stabilizes, reaches, manipulates, walks, endures, and paces (AOTA, 2014). As a
result of impairments and specific limitations, the clients personal routines and usual life roles
have changed. As previously mentioned, the client is no longer able to engage in physically
demanding activities or sports such as, running and playing basketball, which are two activities
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
11
that he finds meaningful. Given the complexity of MS and the presence of various symptoms
such as weakness and fatigue, the client is concerned about his energy, and fulfill his role as a
father. In addition to this, the presence of MS has significantly impacted the clients cultural
context, including activity choices. His physical and social environment has also changed since
his move to Nevada. He attempts to keep in contact with friends through social media, but misses
the face-to-face interaction.
Problem List
Problem statements help determine the intervention plan. The clients problem list was
prioritized to promote client-centeredness and feasibility of care. This process requires
consideration of the clients needs, as well as the context in which OT services are implemented.
The following list was determined by key problem areas identified during the initial evaluation in
conjunction with the clients goals.
1. Poor dynamic standing balance and decreased activity tolerance results in safety
concerns during functional ambulation. 2. Client requires moderate assistance for dressing due to
decreased fine motor skills. 3. Increased fatigue results in need for caregiver assistance in IADL
tasks such as child rearing. 4. Client is unable to engage in meal preparation due to decreased
fine motor skills. 5. Increased fatigue and weakness in LE limits the clients ability to participate
in leisure occupations.
The top priority is to keep the client safe. In order to ensure the client is safe, functional
ambulation will be addressed in treatment. This is important as occupational engagement
requires an individual to move from one location to another during performance of daily tasks. In
addition to this, the clients priority is to maintain independence in ADL and IADL function. As
identified in the initial evaluation, the client would like to complete his morning routine of
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
12
dressing or buttoning his clothing without assistance from a caregiver. In theory, in order to
promote the clients self-efficacy or beliefs in his capacity to execute fundamental tasks, selfdressing is an important area to address. Overall, dressing and functional mobility are two
significant components of ADL to target, given the clients desire to build autonomy in self-care.
Furthermore, it is important for the client to be able to dress himself and move around
safely and independently during performance of everyday activities before engaging in more
complex activities, such as meal preparation and participation in leisure occupations.
Intervention will still focus on building skills that will translate to IADL function.
The role of the occupational therapist at the outpatient rehabilitation clinic will be to help
the client maintain daily skills that are essential for independent living, both in the home and
community. The therapist working with the client can generate intervention strategies that will
target contributing factors impeding the clients occupational performance. Skilled therapy
services will be able to provide appropriately designed strengthening necessary for improvement
in balance and fine motor coordination for independence in ADL and IADL function. Further, the
use of assistive technology, as well as education and training in modifications will be
implemented to maintain maximal participation in preferred occupations.
Intervention Plan and Outcomes
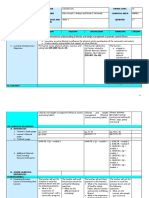
Long-term Goals (LTG)
1. Client will demonstrate functional mobility at support group with Mod using SPC
for support within 1 month.
2. Client will complete UE dressing with Mod using A/E for support within 1 month.
Short-term Goals (STG)
LTG 1: STG 1a: Client will demonstrate ability to stand and lecture for 20 min with SPV
using SPC for support within 2 weeks.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
13
LTG 1: STG 1b: Client will greet and usher at least 10 support group members to table
with SPV using SPC for support within 2 weeks.
LTG 2: STG 2a: Client will don button-up shirt with Min A using button-hook for support
within 2 weeks.
LGT 2: STG 2b: Client will doff button-up shirt with Min A using button-hook for
support within 2 weeks.
Intervention Ideas
STG 1a: Client will perform virtual practice of Nintendos Wii Sports. Clinical use of Wii
tennis from a standing position will help improve clinical measures of balance and increase
activity tolerance in client. Interactive video game will serve as a strengthening and endurance
program to increase the clients activity tolerance for functional activities. In addition to this, Wii
tennis simulation will be implemented to improve the clients dynamic standing balance.
Participation in Wii tennis requires similar skills or movements that translate to the clients
support group environment, such as having to maintain appropriate posture and balance during
performance of tasks such, standing up and lecturing to the group. More specifically, the activity
has various functional implications, such as increasing endurance through use of standing with
upper-extremity motion and increasing strength and flexibility through use of movements
required for successful scoring. More importantly, Wii tennis serves as a functional balance
activity to increase the clients confidence in ADL and IADL function.
Grade Up: As the clients activity tolerance improves, activity can be performed from a
standing position without use of DME. Therapist will remain in close-proximity and use a gaitbelt for safety. Further, speed or duration of activity can be increased to build the clients
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
14
endurance. The therapist may also choose to have the client hold the control in the non-dominant
hand to increase the difficulty or complexity of the game.
Grade Down: Client will continue to perform activity with use of a SPC for support. In
addition to this, the speed or duration of the activity can be lowered to accommodate the clients
level of balance, endurance, and fatigue level.
Approach: Intervention will be implemented to help the client maintain or preserve
capabilities and prevent functional limitations. More specifically, clinical use of Wii tennis will
help target activity tolerance and balance to improve and maintain functional capacity. As
previously stated, specific intervention strategies will include having the client stand with upperextremity motion and balance in order to maintain function and overcome limitations needed to
participate in desired occupations.
Evidence: Impaired balance is prevalent amongst individuals diagnosed with MS. This
can be a limiting factor to occupational engagement and the ability to move from one location to
another during performance of activities. With the advancement of rehabilitation technology,
virtual reality environments have surfaced and are used in clinical practice to increase clientengagement, and to obtain objective results. In a random-controlled trial study examining the
effectiveness of virtual reality-video games for patients with MS, Gutirrez et al. (2013) reported
that telerehabilitation (TR) programs using virtual therapy demonstrate significant improvements
in balance and postural control (PC) for patients with MS. Moreover, they suggest that
improvements in balance and PC in the experimental group may be linked to motor control
principles such as distribution of practice, functional task repetition, and sensory feedback
(Gutirrez, 2013). The gaming protocol in the study incorporated tasks such as hitting objects
with hands and feet, hitting and receiving balls, dodging objects, imitating postures, and so forth.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
15
These results can, perhaps, be generalized to the clients intervention using Wii Tennis, and
demonstrate the potential to improve balance and activity tolerance needed to participate in
preferred occupations. Overall, implementation of Wii Tennis will provide a safe and clientcentered approach to rehabilitation therapy.
Outcome: The outcome of intervention is directed toward improvement. Intervention will
aim to improve functional ambulation during performance of IADL activities such as the clients
ability to lead his support group. Impaired balance and decreased activity are two limitations in
which the client currently faces. Thus, skilled intervention will aim to provide an appropriately
designed strengthening activity, which is necessary for improvement in balance and activity
tolerance.
STG 1b: Given the clients upcoming trip to Chicago, intervention will include an
organized treatment session to address travel preparation tasks that require functional
ambulation. The client will practice packing and unpacking a suitcase with supervision of the
therapist using a SPC for support. Prior to the activity, the occupational therapist will sit down
with the client and briefly discuss effective strategies for packing a suitcase such as, creating a
list and distributing weight evenly in the suitcase. Following this, the OT will supervise the client
as he packs a suitcase. The client will demonstrate safe clothing retrieval and transport from the
closet and place items into the suitcase. The client will use a SPC for support to functionally
ambulate during the activity. Further, the suitcase will be placed on a counter-top table to
promote dynamic standing balance. As previously stated, the client will functionally ambulate in
and around the room to retrieve items. The activity will require the client to maintain a good base
of support while standing and performing a functional activity. This real-life, meaningful activity
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
16
will aim to address dynamic standing balance and activity tolerance, which are important to
functional ambulation and participation in ADL and IADL activities.
Approach: The maintain approach was used to select and implement intervention. The
aim of intervention was to help the client continue to use his SPC for functional ambulation. If
the client were to rely on the scooter, functional ambulation would decrease thereby affecting his
ability to move within the support group environment. The overall goal of intervention is to
improve and maintain functional capacity.
Evidence: Functional ambulation is an important component of occupational engagement.
In order for individuals to pursue daily life roles and responsibilities, they must be able to move
about their environment in a safe and efficient manner. When implementing intervention to
promote the clients overall function, use of meaningful and important activities is needed to
facilitate change. Given the clients upcoming trip to Chicago, and the importance he places on
his this new job, the intervention discussed above is likely to be a meaningful activity that can
facilitate improvement in functional ambulation. According Kuo, By paying attention to the
ends-in-view, possible courses of action surrounding occupational choices are envisaged to
anticipate desirable experiences. Such an approach can be used to reinforce a positive and
meaningful occupational trajectory that promotes health and well-being. (p.131). The use of
occupations, both as a means and an end, is unique to the field of occupational therapy and in
implementing meaningful and purposeful activities in treatment (Gray, 1998). In order to
correspond with our profession and our scope of practice, occupations and functional outcomes
should be the target of our intervention.
Outcomes: The outcome of intervention is directed toward improvement and
participation. The aim of intervention is to achieve outcomes that support the clients
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
17
engagement in preferred occupations such as leading his current support group. Further,
intervention strategies were generated to improve the clients ability to functionally ambulate
with a SPC.
STG 2a: The client will receive education and training in upper-extremity dressing with
use of a button-hook for support. Information will be presented through use of verbal and visual
demonstration. The client will practice manipulating the button-hook from a seated position to
ensure safety. OT will thoroughly educate on A/E and how it can be implemented in the clients
daily routine to increase independence in dressing. The caregiver will also be educated on the use
of A/E, and the importance in continuing practice at home. The client and caregiver will be
encouraged to practice using A/E at home in order to reach progress.
Approach: This intervention utilizes the modify approach or compensation adaptation to
address the clients needs. Given the clients lack of hand dexterity due to sensory impairments,
A/E is introduced as a compensatory technique to accommodate the clients needs. The
intervention will aim to modify the current context or demands of dressing by implementing
compensatory techniques to help increase the clients performance of the activity.
Evidence: Compensatory strategies, through use of A/E, in self-care tasks is commonly
implemented in treatment for individuals with MS. According to Finlayson (2013), incorporating
A/E to promote occupational engagement in self-care, and to accommodate for limitations, is
beneficial as it reduces demands in the presence of barriers to self-care for individuals with MS
(p. 343). A/E training can be viewed as a compensatory technique to promoting independence in
ADL function. Since the clients new job as Patient Ambassador will require frequent travel trips,
it is important for the client to demonstrate the ability to self-dress. Thus, it is important to
implement A/E so that he is able to perform the activity of dressing independently and safely.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
18
Outcome: Implementation of intervention is directed toward improving skills in
occupational performance. The use of a button-hook will enable the client to increase his ability
to complete upper-extremity dressing, despite decreased fine motor and manual dexterity skills.
Improving the clients ability to self-dress will reduce caregiver dependency and increase
independence in ADL function.
STG 2b: Intervention will take place in the outpatient rehabilitation setting. Activity will
involve an art project with the client and clients daughter to promote therapeutic use of craft
intervention. Client will grab tools and materials from table in preparation for crafty activity.
Client will twist open or close lids on a small bottle (e.g., bottle, container, jar) held within the
palm of the hand. Client will flip a coin from head to tail within the fingers of the hand to
determine if he or the daughter goes first in starting the activity. Client will work with his
daughter to cut with scissors and practice adjusting the grip on the construction paper or paper
plate being used. Client will manipulate different objects in hand such as buttons, coins, cotton
swabs, beads, and macaroni. Activity will require using bottles to squeeze glue, paint, glitter, and
fabric paint to place objects on material. The client will perform the activity with the daughter in
a seated position to ensure safety. Therapeutic purpose of activity is to improve fine motor skills
and hand dexterity needed to complete self-care skills, and is a functional activity that can
increase independence in ADL function.
Approach: This intervention will use the restore approach to help the client reestablish
hand dexterity to enable manipulation of button-hook for self-dressing. The client currently relies
on his primary caregiver to complete tasks that require manual dexterity. As a result, the purpose
of the intervention is to incorporate his hands in functional activities to address impaired hand
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
19
function. This will help the client utilize A/E, such as the button-hook more efficiently for upperextremity dressing.
Evidence: According to a sensory re-education training program on hand dexterity in
individuals with MS, Kalron, Greenberg-Abrahami, Gelav, and Achiron (2013) found that
sensory re-education did not affect sensory impairments, however did effectively improve select
measures of manual dexterity. The study was comprised of participants with relapsing-remitting
MS who had sensory deficits in one or both hands. Sensory re-education training a 7-week
control phase of OT twice a week with repeated exposure to stimuli varying in size, shape,
weight, hardness, and temperature through grasp of objects (2013). Hand function was measured
through use of a nine-hole peg test, two-point discrimination test, monofilaments test, and
functional dexterity test at baseline, following the control phase, and at the end of trial (2013).
Results indicated that intervention can have positive effects on manual dexterity. According to
Kalron et al. (2013), an overall improvement of 15% in manual dexterity measurements was
shown upon completion of the sensory re-education phase, as demonstrated by the nine-hole peg
and functional dexterity tests (p. 946). Results from the study may suggest important
implications for the clients intervention. Implementation of intervention was aimed to produce
improvements in manual dexterity needed to facilitate grasp or proper use of A/E for ADL
function.
Outcome: Intervention will aim to improve the clients performance in upper-extremity
dressing. Given the clients sensory impairments and decreased fine motor skills, this craft
activity will potentially produce improvement in manual dexterity needed to self-dress or
manipulate A/E for self-dressing.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
20
Precautions
Prior to treatment, appropriate steps should be taken to evaluate the clients safety. Given
the clients history of falls, it is imperative for the OT to place a gait belt on the client and to
remain in close-proximity throughout each intervention. In order to avoid fatigue, rest breaks
should be incorporated routinely.
Frequency & Duration
The client will receive skilled OT intervention 2 times a week with 60 minute sessions for
4 weeks to target both long-term goals indicated in the treatment plan. Focus will be on
increasing balance, building activity tolerance, and providing education and training on use of
A/E to increase the clients overall safety and independence in ADL and IADL function. Skilled
therapy is necessary to provide appropriately designed strengthening activities for improvement
in functional ambulation and fine motor skills for independence in functional activities. The
client will practice functional ambulation and dressing with use of A/E and DME to strengthen
and maintain his functional capacity. Education and training for the client and his primary
caregiver will continue to be provided to increase safety and independence in occupational
performance.
Primary Framework
Theory provides a framework within which the therapist can accurately assess the
strengths and needs of the client. It enables the therapist to view each client from a distinctive
lens, and in doing so, provides guidance in implementing an effective intervention plan. The
Canadian Model of Occupational Performance (CMOP) was used to evaluate the client, and to
select and implement an appropriate intervention plan. The CMOP aims to determine the
relationship between occupation, health, and well-being by evaluating the clients values, beliefs,
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
21
and their intrinsic need to engage in meaningful occupations (Clarke, 2003). This model
acknowledges the dynamic relationship between the person, environment, and occupation, and
how these three constructs interact with one another to yield occupational performance. The
CMOP embraces spirituality as the core of the model and emphasizes the importance of the
clients values, views, and beliefs in shaping occupational performance.
Occupations can be influenced by various factors, both intrinsic (from within, as when
we are passionate about something) and external (incentivized by rewards) motivation. The
CMOP was used as the theoretical approach to guiding the intervention because of its emphasis
on client-centered occupational performance, the dynamic interaction between person,
environment, and occupation, and the fundamental importance of spirituality embraced as the
core of the model. Prior to determining the intervention, the therapist analyzed the specific
activities in which the client expressed interest in and targeted important skills that are essential
to performing these occupations. The clients satisfaction and self-perception of occupational
performance was taken into consideration prior to implementing treatment.
Client/Caregiver Training and Education
The client will continue to receive education and training regarding use of DME & A/E
for ADL and IADL function. The client will practice utilizing the button-hook in therapy, and
will be encouraged to practice with the caregiver at home to improve self-care skills. The
therapist will assess the clients progress and take into consideration skill level when
implementing future interventions and activities. If further training is needed, the client will
continue to participate in functional activities with use of DME and A/E in a safe environment.
The priority of treatment is to maximize the clients safety and independence in the performance
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
22
of functional ambulation and dressing. Thus, training and education will be provided throughout
intervention.
Clients Response to the Intervention
The clients response to intervention is an important component of therapy. Assessment
and reassessment will be used to monitor the clients progress towards goals and identified
outcomes. The clients response to treatment will be recorded daily through use of a therapy log
with information regarding attendance and participation in therapy. Review of the intervention
process, as well as the patients gains and progress toward targeted outcomes will be monitored
to ensure that the demands of the activity and the skills of the client coincide. Reinforcement and
grading of activities will also be implemented to provide the right level of challenge and learning
needed to improve performance.
References
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
23
American Occupational Therapy Association.(2014).Occupational therapy practice framework:
Domain and process (3rd ed.).American Journal of Occupational Therapy, 68(Suppl.1),
S1S48.http://dx.doi.org/10.5014/ajot.2014.682006
Ann Kuo (2011) A Transactional View: Occupation as a Means to Create Experiences that
Matter, Journal of Occupational Science, 18:2, 131-138, DOI:
10.1080/14427591.2011.575759
Clarke, C. (2003). Clinical application of the Canadian Model of Occupational Performance in a
forensic rehabilitation hostel. The British Journal of Occupational Therapy, 66(4), 171174.
Finlayson, M. (Ed.). (2012). Multiple Sclerosis Rehabilitation: From Impairment to
Participation. CRC
Press.
Gutirrez, R. O., Galn del Ro, F., Cano de la Cuerda, R., Alguacil Diego, I. M., Gonzlez, R.
A., & Page, J. M. (2013). A telerehabilitation program by virtual reality-video games
improves balance and postural control in multiple sclerosis patients. Neurorehabilitation,
33(4), 545-554. doi:10.3233/NRE-130995
Kalron, A., Greenberg-Abrahami, M., Gelav, S., & Achiron, A. (2013). Effects of a new sensory
re-education training tool on hand sensibility and manual dexterity in people with
multiple sclerosis. Neurorehabilitation, 32(4), 943-948. doi:10.3233/NRE-130917
Law, M. (2002). Participation in the occupations of everyday life. American Journal of
Occupational Therapy, 56(6), 640-649. doi:10.5014/ajot.56.6.640
McLaughlin Gray, J. (1998). Putting occupation into practice: Occupation as ends, occupation as
means. American Journal of Occupational Therapy, 52(5), 354-364.
doi:10.5014/ajot.52.5.354
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
24
Intervention: Patient will perform gardening from a standing position using a FWW for support.
The intervention will help address standing balance and bilateral UE strength through use of a
planting activity, which is meaningful to the patient. The patient will pot plants on a counter with
the therapists standing beside the patient on the involved side, guiding the affected extremity in
normal patterns of movement. The plants can be positioned at different levels of reach on the
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
25
counter to increases the patients weight shift and UE function. A wheelchair will be positioned
behind the patient for rest breaks. This planting activity will help increase activity tolerance,
balance, and hand function required for performing safe transfers. Gardening is an activity that
is familiar and meaningful to the patient, and provides repetition of movement needed to increase
motor function, which can improve the patients overall function.
Approach: This intervention approach will help restore the patients balance, trunk
stability, and UE function in order to perform safe and functional transfers. It is important for the
patient to remediate these skills in order to increase safety and independence in ADL function.
Evidence: In suggesting treatment strategies for patients with motor impairment after
stroke, Davis (2009) states, Select activities requiring repetition of movement. Repetition is
beneficial for motor learning and, at the same time, gives you more opportunity to refine, correct,
and guide your patients patterns of movement during the activity. Gardening is an activity that
requires repetition of movement and can help build the patients UE function. The therapist can
use HOH assistance to guide the patients affected extremity in normal patterns of movement.
Repetition and continuity enable patients who have experienced a stroke build skills required for
performance of everyday activities. Selecting meaningful activities allow patients to problemsolve and generalize skills to real-life scenarios. In regards to the patient performing the activity
on a counter-top, Davis (2006) explains, Contact with a solid surface encourages better trunk
and limb control with fearful patients (p. 9). The counter provides support and stability for the
patient while performing the activity from a standing position.
Outcome: The potential outcome is participation in safe and functional transfers. Through
the intervention process, the patient will recover the skill and ability to perform self-care and
functional mobility with increased safety and independence. Continuous practice and
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
26
participation with use of DME will enable the patient to build functional independence in
movement during performance of everyday activities.
Short-Term Goal 2B: Pt. will transfer safely 3:1 commode for toileting Min A
utilizing FWW for safety within 5x sessions.
Intervention: The patient will receive education and training regarding safe and functional
transfers with use of DME. The therapist will provide clear, concise information on utilizing
FWW and 3:1 commode, and education regarding the proper technique and form to use to
perform the transfer safely. The patient will practice the activity in a safe environment and
problem-solve the steps of the task in sequence utilizing verbal and physical cues as needed. Rest
breaks will be incorporated to help manage symptoms of fatigue.
Approach: This intervention uses a modified approach to increase the patients level of
independence in safe and functional transfers through use of DME. Education and training will
be provided to help the patient complete a toileting routine. The activity will be modified
through implementation of a FWW and 3:1 commode to support ADL function.
Evidence: According to Wolf and Birkenmeier (2011), Prescribing and training clients in
the use of assistive devices and adapted equipment is one way occupational therapists try to
improve and maintain occupational performance (p. 289). Implementation of DME and A/E is
common in patients with motor impairments after stroke as it provides a tool that increases
performance in ADL function. Thus, it allows them to complete self-care activities more
independently and safely despite loss of function.
Outcome: The targeted outcome is improvement in occupational performance.
Intervention implementation will enable the patient to perform toileting independently and
safely. Given the patients left hemiparesis, as well as decreased balance and activity tolerance,
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
27
this intervention will potentially improve the patients occupational performance and capacity to
complete safe and functional transfers.
Long-Term Goal 1: Pt. will demonstrate dressing SPV using A/E within 2 wks.
Short-Term Goal 1A: Pt. will don & doff pants Min A using reacher & dressing stick
within 5x sessions.
Intervention: Patient will perform virtual practice of Nintendos Wii Sports. Clinical use
of Wii bowling from a seated position will help improve clinical measures of balance & motor
function in patient. Interactive video game intervention will help support trunk stability in
patient who demonstrates fall risks & difficulty with bending & reaching for LE dressing. Wii
bowling simulation provides an effective approach to balance training. Activity requires similar
movements needed for LE dressing from a seated position. Activity provides repetition of
movement and encourages weight shift. More importantly, it serves as a functional balance
activity to increase confidence with ADL activities.
Grading Up: Patient will perform activity from a standing position utilizing FWW for
stability & support.
Grading Down: Patient will continue to perform activity from a seated position. Patient
will utilize front wheel walker (FWW) with right hand for stability & support, while
manipulating controller in left UE.
Evidence: According to Nilsen et al. (2015), nonimmersive video game systems,
such as the Wii, can improve UE function and activity and participation in patients with motor
impairments after stroke. These virtual reality (VR) environments provide training and exercise
of the affected UE using goal-directed activities requiring repetition of task-specific movements
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
28
that is beneficial for motor learning and allows patients to refine or correct patterns of
movement. Moreover, in a research study discussing the effectiveness of Wii gaming in stroke
rehabilitation, Saposnik et al. (2010) assert that VR games offer a safe and feasible alternative to
implement rehabilitation therapy and to promote motor recovery in patients following a stroke.
Outcome: The potential outcome is for the patient to improve his occupational
performance of dressing. Implementation of the intervention will help address trunk stability and
balance, two important skills that are needed to bend and reach for LE dressing. Improving these
skills will allow the patient to complete self-care more safely and independently with use of A/E.
Short-Term Goal 1B: Pt. will don & doff button-up shirt Min A using button-hook
within 5x sessions.
Intervention:
Approach: This intervention utilizes aspects of restore and modify to address the patients
desired outcomes. Given the patients left hemiparesis, A/E is introduced as a compensatory
technique to dressing while use of the affected extremity is encouraged throughout the activity to
address impairments and goals that have been identified. The intervention will aim to modify the
current context or demands of the activity by using compensatory techniques to help the patient
perform the activity of dressing. The affected extremity will still be incorporated in the activity
for rehabilitation purposes and for restoring muscle control and strength that has been impaired.
Evidence: According to Wolf and Berkenmeier (2011), Compensation through the use of
the unaffected side to perform ADLs is common as part of routine stroke care. Therapists should
encourage use of the affected extremity when possible; when unable, they should use
compensatory strategies with the unaffected side (p. 288). A/E training can be viewed as a
compensatory technique to promoting ADL function. Since the patient does not have a caregiver
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
29
and is likely to be unsupervised after discharge from the IRF, it is important to teach and
implement A/E so that he is able to perform the activity of dressing both independently and
safely. It is crucial for the patient to participate in several education and training sessions prior to
discharge in order to ensure that compensatory strategies are properly learned. Throughout the
intervention process, the patient should still be encouraged to incorporate the affected extremity
into different components of the activity.
Outcome: Through the intervention process, the patient will improve his ability to selfdress. This will help support self-care autonomy and ADL function, which is required to return
home and perform day-to-day activities with better safety and independence.
Frequency & Duration
The patient will receive Tx. for 90 min daily 5x/wk for 2 wks for skilled instruction in
dressing and functional mobility DME & A/E to & safety D/C. Focus will be on
activity tolerance, standing balance, strengthening L UE, & utilizing DME & A/E with safety.
Pt. will practice dressing A/E & performing transfers DME to achieve optimum level of in
ADL & IADL function. In addition to OT, the patient will also receive physical therapy, speech
therapy, and 24 hr rehabilitation nursing supervision. This treatment could not be provided at a
lower level of care.
Primary Framework
Theory significant influences the process of treatment by providing a framework within
which the therapist can evaluate and assess the needs of the patient. It enables the therapist to
view each patient from a distinctive lens, and in doing so, it provides guidance in implementing
an effective intervention plan. The Occupational Therapy Task-Oriented Approach (OT-TOA)
was the most applicable model to increase the patients occupational performance, and to
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
30
increase efficiency of compensatory strategies used to perform functional activities. Due to the
patients left hemiparesis and weakness in the left UE, as well as decreased balance, activity
tolerance, and trunk stability, the OT-TOA poses potential benefits in enabling the patient to
achieve functional independence.
The OT-TOA is rooted in the model of motor control and theories of motor learning
(Cohn & Coster, 2014). The theory aims to help individuals with motor impairment increase
efficiency in task performance and restore the skills needed to engage in meaningful occupations.
The OT-TOA is unique in that it highlights the role of the patient and uses real life activities to
promote success. The theory follows the principle that movement is influenced by personal and
environmental factors, and that in order to fulfill desired roles, one must be able to meet the
demands of the tasks associated with the role (Cohn & Coster, 2014). For example, since
gardening is a meaningful activity to the patient, the activity of potting plants is likely to increase
motivation and therefore promote progress. As indicated above, an essential aspect of the OTTOA is individualizing the treatment plan by tailoring the intervention to what is purposeful to
the patient.
The OT-TOA also emphasizes the importance of intervention occurring in a natural
environment. Despite the clinical setting in which the patient is in (IRF), therapists can replicate
a functional activity in a natural environment (e.g., gardening in the skills lab). According to
Cohn and Coster (2014), a natural context promotes more flexible patterns of movement. The
OT-TOA helped guide intervention efforts for the patient by implementing functional activities in
a natural setting to maximize the patients motor performance. Therapeutic activities such as
gardening and Wii bowling were incorporated into the intervention to encourage repetition of
movement, which is needed for motor learnings. Implementing meaningful activities in a natural
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
31
context provides the patient with opportunities to improve his overall performance in ADL and
IADL function.
Client/Caregiver Training & Education
Education and training will be implemented throughout the intervention process to
The patient will continue to receive training and education regarding use of DME & A/E for
ADL and IADL function. The therapist will impart knowledge and information regarding transfer
techniques and equipment use. The patient will practice utilizing FWW, 3:1 commode, reacher,
dressing stick, and button-hook to improve mastery of self-care skills. The therapist will assess
the patients progress and take into consideration skill level when implementing future
interventions and activities. If further training is needed, the patient will continue to participate in
functional activities with use of DME and A/E in a safe environment. The priority of treatment
is to maximize the patients safety and independence in functional mobility and dressing in order
to achieve self-care autonomy, therefore as much training and education that is needed will be
provided.
Clients Response to the Intervention
The patients response to treatment is an important component of therapy. Assessment
and reassessment will be used to monitor the patients progress towards goals and identified
outcomes. The patients response to treatment will be recorded daily through use of a therapy
log with information regarding attendance and participation in therapy. Review of the
intervention process, as well as the patients gains and progress toward targeted outcomes, will
be monitored to ensure that the demands of the activity and the skills of the patient coincide.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
32
Reinforcement and grading of activities will also be implemented to provide the right level of
challenge and learning that is needed to achieve functional independence.
Problem List
Problem Statement #1:
Patient is unable to dress self 2 P trunk stability & muscle strength in L UE.
Problem Statement #2:
Patient is unable to complete functional mobility safely 2 P standing balance &
activity tolerance.
Problem Statement #3:
Patient is unable to perform bathing 2 to P core strength & ROM in L UE.
Problem Statement #4:
Patient is unable to groom self 2 fatigue & endurance.
Problem Statement #5:
Patient is unable to perform gardening 2 hand function & muscle strength in L UE.
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
33
References
Davis, J. Z. (2006). Task selection and enriched environments: A functional upper extremity
training program for stroke survivors. Topics in Stroke Rehabilitation, 13(3), 1-11.
doi:10.1310/D91V-2NEY-6FL5-26Y2
Nilsen, D. M., Gillen, G., Geller, D., Hreha, K., Osei, E., & Saleem, G. T. (2015). Effectiveness
of interventions to improve occupational performance of people with motor impairments
after stroke: An evidence-based review. American Journal of Occupational Therapy, 69,
6901180030. http://dx.doi.org/10.5014/ajot.2015.011965
Poole, J. L. (2011). Enabling performance and participation for persons with movement
disorders. In C. H. Christiansen & K. M. Matuska (Eds.), Ways of living: Intervention
strategies to enable participation (4th ed., p. 288-289). Bethesda, MD: American
Occupational Therapy Association
Saposnik, G., Teasell, R., Mamdani, M., Hall, J., McIlroy, W., Cheung, D., . . . Bayley, M.
(2010). Effectiveness of Virtual Reality Using Wii Gaming Technology in Stroke
OCCUPATIONAL PROFILE AND INTERVENTION PLAN
34
Rehabilitation: A Pilot Randomized Clinical Trial and Proof of Principle. Stroke.
doi:10.1161/STROKEAHA.110.584979
Das könnte Ihnen auch gefallen
- Occupation Analysis in PracticeVon EverandOccupation Analysis in PracticeLynette MackenzieNoch keine Bewertungen
- Occt651 - Occupational Profile Paper - FinalDokument20 SeitenOcct651 - Occupational Profile Paper - Finalapi-293182319Noch keine Bewertungen
- Rheumatology Practice in Occupational Therapy: Promoting Lifestyle ManagementVon EverandRheumatology Practice in Occupational Therapy: Promoting Lifestyle ManagementLynne GoodacreNoch keine Bewertungen
- Occupational Profile and Intervention PlanDokument13 SeitenOccupational Profile and Intervention Planapi-251993533Noch keine Bewertungen
- 630 Submitted Occupational Profile and AnalysisDokument21 Seiten630 Submitted Occupational Profile and Analysisapi-310815315Noch keine Bewertungen
- Occupational Profile & Intervention PlanDokument19 SeitenOccupational Profile & Intervention Planapi-262531856100% (1)
- 630 Occupational Profile and Intervention PlanDokument22 Seiten630 Occupational Profile and Intervention Planapi-282538590100% (1)
- 630 Occupational Profile AssignmentDokument13 Seiten630 Occupational Profile Assignmentapi-201999002Noch keine Bewertungen
- Occupational Profile and Intervention Plan FinalDokument21 SeitenOccupational Profile and Intervention Plan Finalapi-263352281Noch keine Bewertungen
- Occupational Profile PaperDokument20 SeitenOccupational Profile Paperapi-292814113Noch keine Bewertungen
- Occupational ProfileDokument21 SeitenOccupational Profileapi-293223028100% (1)
- Model of Human OccupationDokument5 SeitenModel of Human OccupationPatrick IlaoNoch keine Bewertungen
- Running Head: Occupational Profile and Intervention Plan 1Dokument19 SeitenRunning Head: Occupational Profile and Intervention Plan 1api-292735638Noch keine Bewertungen
- Ot Goals NuevoDokument157 SeitenOt Goals NuevoElbania PerezNoch keine Bewertungen
- Pediatric SpaDokument11 SeitenPediatric Spaapi-420919156100% (2)
- Occupational Therapy Survival GuideDokument12 SeitenOccupational Therapy Survival Guideapi-256686248Noch keine Bewertungen
- Dickson Occupational ProfileDokument18 SeitenDickson Occupational Profileapi-255001706Noch keine Bewertungen
- CO OP AOTA - July - 2020Dokument10 SeitenCO OP AOTA - July - 2020Ana Claudia GomesNoch keine Bewertungen
- Eval Soap NoteDokument10 SeitenEval Soap Noteapi-436577744Noch keine Bewertungen
- Ethics Occupational TherapyDokument7 SeitenEthics Occupational TherapyGeyanne GeyrosagaNoch keine Bewertungen
- Student Treatment Session Soap 8Dokument9 SeitenStudent Treatment Session Soap 8api-340625860100% (1)
- Clients Goals To Address in SessionDokument8 SeitenClients Goals To Address in Sessionapi-436429414Noch keine Bewertungen
- Soap 11Dokument4 SeitenSoap 11api-436429414Noch keine Bewertungen
- Occupational Profile Intervention PlanDokument17 SeitenOccupational Profile Intervention Planapi-264481356Noch keine Bewertungen
- Evaluation ReportDokument3 SeitenEvaluation Reportapi-547360536Noch keine Bewertungen
- Occupational Therapy Discharge SummaryDokument3 SeitenOccupational Therapy Discharge Summaryapi-3806812240% (1)
- Occupational Performance History Interview PDFDokument2 SeitenOccupational Performance History Interview PDFBrad0% (4)
- CO-OP: Brief Description of Cognitive Orientation to Daily Occupational Performance ProtocolDokument17 SeitenCO-OP: Brief Description of Cognitive Orientation to Daily Occupational Performance ProtocolCarol Alvarado100% (2)
- Occupational Therapy AssessmentDokument3 SeitenOccupational Therapy AssessmentEllySaleh100% (1)
- Occupational Therapy Toolbox Study GuideDokument44 SeitenOccupational Therapy Toolbox Study GuideKristian ShumateNoch keine Bewertungen
- Occupational Profile Intervention PlanDokument19 SeitenOccupational Profile Intervention Planapi-263353704Noch keine Bewertungen
- Occupational Therapy Evaluation Report and Initial Intervention PlanDokument12 SeitenOccupational Therapy Evaluation Report and Initial Intervention Planapi-488383880100% (1)
- Functional Intervention Occupational Therapy Kit DescriptionDokument3 SeitenFunctional Intervention Occupational Therapy Kit Descriptionapi-404615775Noch keine Bewertungen
- Activity Analysis Yoga and PilatesDokument24 SeitenActivity Analysis Yoga and Pilatesapi-290348341100% (3)
- Dick, Elisa - Occupational ProfileDokument10 SeitenDick, Elisa - Occupational Profileapi-234536968Noch keine Bewertungen
- Occupational Therapy Discharge SummaryDokument4 SeitenOccupational Therapy Discharge Summaryapi-518285126Noch keine Bewertungen
- Occupation Based InterventionsDokument16 SeitenOccupation Based Interventionsapi-293182319100% (1)
- Kristen Kincaid Occupational Analysis & Intervention PlanDokument23 SeitenKristen Kincaid Occupational Analysis & Intervention Planapi-282525755100% (1)
- Sample OT Reports Adult AllDokument22 SeitenSample OT Reports Adult AllDanielle Stella N'Luca50% (2)
- Client Initial Evaluation Soap NoteDokument8 SeitenClient Initial Evaluation Soap Noteapi-582889983Noch keine Bewertungen
- Soap Note 2 Community ClientDokument12 SeitenSoap Note 2 Community Clientapi-271984934Noch keine Bewertungen
- AOTA Occupational Profile TemplateDokument2 SeitenAOTA Occupational Profile TemplateVIJAYA DHARSHINI M Bachelor in Occupational Therapy (BOT)Noch keine Bewertungen
- Double Time Docs Sample Evaluation OT SchoolDokument10 SeitenDouble Time Docs Sample Evaluation OT SchoolAlyssa BalverdeNoch keine Bewertungen
- Occupational Therapy: Skills For LivingDokument14 SeitenOccupational Therapy: Skills For Livingkalik67% (3)
- 15 Ot Sop Aota Exam PrepDokument46 Seiten15 Ot Sop Aota Exam PrepJarred AdamsNoch keine Bewertungen
- 2001 Candidate Handbook: National Board For Certification in Occupational Therapy, Inc. (Nbcot)Dokument54 Seiten2001 Candidate Handbook: National Board For Certification in Occupational Therapy, Inc. (Nbcot)engshi18Noch keine Bewertungen
- OT Practice FrameworkDokument12 SeitenOT Practice Frameworkenrico_aguila100% (2)
- Occupational Profile and Intervention Plan FinalDokument21 SeitenOccupational Profile and Intervention Plan Finalapi-293223028Noch keine Bewertungen
- Eval Soap Note 2Dokument9 SeitenEval Soap Note 2api-435763096Noch keine Bewertungen
- Stroke Occupational Profile Paper - 651Dokument21 SeitenStroke Occupational Profile Paper - 651api-290919325100% (1)
- OT Theories (In A Nutshell)Dokument8 SeitenOT Theories (In A Nutshell)TaraJane House100% (1)
- Category Ot Goals.Dokument11 SeitenCategory Ot Goals.adelitaperez100% (3)
- Canadian Occupational Performance Measure (COPM) : 4 EditionDokument3 SeitenCanadian Occupational Performance Measure (COPM) : 4 EditionDulcea LoredanaNoch keine Bewertungen
- AOTA Occupational Profile Template PDFDokument2 SeitenAOTA Occupational Profile Template PDFCrys Paola Alvarez Gonzalez100% (1)
- Occupational Profile & Intervention PlanDokument20 SeitenOccupational Profile & Intervention Planapi-262531856Noch keine Bewertungen
- CMOP-E occupational model overviewDokument16 SeitenCMOP-E occupational model overviewAnca-Maria Vlad100% (2)
- Occupational Therapy ProcessDokument3 SeitenOccupational Therapy Processapi-339841373100% (1)
- Fieldwork Case Study Treatment Plan AssignmentDokument11 SeitenFieldwork Case Study Treatment Plan Assignmentapi-398892840Noch keine Bewertungen
- Pediatric Treatment PlanDokument11 SeitenPediatric Treatment PlanKayla Jensen100% (1)
- Occupational Therapy's Role in Diabetes Self ManagementDokument2 SeitenOccupational Therapy's Role in Diabetes Self ManagementThe American Occupational Therapy AssociationNoch keine Bewertungen
- Occupation-Based ReflectionDokument2 SeitenOccupation-Based Reflectionapi-293253519Noch keine Bewertungen
- Final Evidence TableDokument21 SeitenFinal Evidence Tableapi-293253519Noch keine Bewertungen
- Social Justice ReflectionDokument2 SeitenSocial Justice Reflectionapi-293253519Noch keine Bewertungen
- Leadership ReflectionDokument2 SeitenLeadership Reflectionapi-293253519Noch keine Bewertungen
- Natasha Evelyn Final PosterDokument1 SeiteNatasha Evelyn Final Posterapi-293253519Noch keine Bewertungen
- Multisensory Approach To HandwritingDokument8 SeitenMultisensory Approach To Handwritingapi-293253519Noch keine Bewertungen
- Resume Eve BabsDokument2 SeitenResume Eve Babsapi-293253519Noch keine Bewertungen
- Evidence-Based Practice ReflectionDokument2 SeitenEvidence-Based Practice Reflectionapi-293253519Noch keine Bewertungen
- Weebly ReferencesDokument1 SeiteWeebly Referencesapi-293253519Noch keine Bewertungen
- My BrandDokument2 SeitenMy Brandapi-293253519Noch keine Bewertungen
- J 1469-8749 2007 00312 XDokument6 SeitenJ 1469-8749 2007 00312 XMinkushNoch keine Bewertungen
- Eval 52787348Dokument4 SeitenEval 52787348api-293253519Noch keine Bewertungen
- La Food Bank DocumentDokument1 SeiteLa Food Bank Documentapi-293253519Noch keine Bewertungen
- Article 2-Handwriting Without Tears-PortfolioDokument4 SeitenArticle 2-Handwriting Without Tears-Portfolioapi-293219537Noch keine Bewertungen
- Aces Final DraftDokument3 SeitenAces Final Draftapi-293253519Noch keine Bewertungen
- Case Study PresentationDokument23 SeitenCase Study Presentationapi-293253519Noch keine Bewertungen
- Home EvaluationDokument5 SeitenHome Evaluationapi-293253519Noch keine Bewertungen
- Eval AngelaDokument4 SeitenEval Angelaapi-293253519Noch keine Bewertungen
- Level Iia EvalDokument7 SeitenLevel Iia Evalapi-293253519Noch keine Bewertungen
- Touro University Nevada Occupational TherapyDokument4 SeitenTouro University Nevada Occupational Therapyapi-292814113Noch keine Bewertungen
- Final CatDokument13 SeitenFinal Catapi-293253519Noch keine Bewertungen
- 527 ADokument4 Seiten527 Aapi-292814113Noch keine Bewertungen
- Wheelchair Bball Minker Complex March 14-15 2015 1Dokument1 SeiteWheelchair Bball Minker Complex March 14-15 2015 1api-293253519Noch keine Bewertungen
- Professional Development Plan Evelyn BabaroudiDokument17 SeitenProfessional Development Plan Evelyn Babaroudiapi-293253519Noch keine Bewertungen
- Evelyn Babaroudi Assistive Technology PaperDokument11 SeitenEvelyn Babaroudi Assistive Technology Paperapi-293253519Noch keine Bewertungen
- Mindfulness and Self-Esteem - Quant ResearchDokument8 SeitenMindfulness and Self-Esteem - Quant Researchapi-290919325Noch keine Bewertungen
- Occupational Profile and Intervention Plan AutosavedDokument19 SeitenOccupational Profile and Intervention Plan Autosavedapi-293253519Noch keine Bewertungen
- Evidence SynthesisDokument13 SeitenEvidence Synthesisapi-293253519Noch keine Bewertungen
- Liz - A Case Study On A Child With Down SyndromeDokument20 SeitenLiz - A Case Study On A Child With Down Syndromeapi-28870699650% (4)
- Vitamin C. USAGE, FUNCTIONDokument20 SeitenVitamin C. USAGE, FUNCTIONANURAG ALOKNoch keine Bewertungen
- Urban HealthDokument10 SeitenUrban HealthKailash NagarNoch keine Bewertungen
- Myanmar HealthcareDokument8 SeitenMyanmar Healthcarezawminn2Noch keine Bewertungen
- Schwartz M. William. Pedoman Klinis Pediatri. Jakarta: Penerbit Buku Kedokteran. ECG. 2005Dokument2 SeitenSchwartz M. William. Pedoman Klinis Pediatri. Jakarta: Penerbit Buku Kedokteran. ECG. 2005Muhammad Rifky Ersadian NoorNoch keine Bewertungen
- Procedure Investigation AnalysisDokument7 SeitenProcedure Investigation AnalysisLisa SwansonNoch keine Bewertungen
- Go Ms 38 Private Hospital Within and Outside State PDFDokument3 SeitenGo Ms 38 Private Hospital Within and Outside State PDFsivaNoch keine Bewertungen
- Ayurveda Tongue Analysis Dr. Rama PrasadDokument34 SeitenAyurveda Tongue Analysis Dr. Rama PrasadSanjay Soni100% (2)
- Vitamin KDokument456 SeitenVitamin KSamy AbdelazizNoch keine Bewertungen
- Managing Opioid DependenceDokument56 SeitenManaging Opioid DependenceNoval RumbiyanNoch keine Bewertungen
- Why You Should Eat A Healthy Breakfast?Dokument2 SeitenWhy You Should Eat A Healthy Breakfast?Lea WaskitoNoch keine Bewertungen
- Class 13 - TreatmentDokument18 SeitenClass 13 - TreatmentDaniela Pérez MartínezNoch keine Bewertungen
- USCE Database Compiled by Usmlesarthi TeamDokument12 SeitenUSCE Database Compiled by Usmlesarthi Teamagar agarNoch keine Bewertungen
- F1000research 8 20413Dokument7 SeitenF1000research 8 20413miss betawiNoch keine Bewertungen
- 02 - Risk Management & AssessmentDokument102 Seiten02 - Risk Management & AssessmentsharkozakNoch keine Bewertungen
- Noise PollutionDokument13 SeitenNoise PollutionSubhendu Ghosh70% (10)
- How To Prevent Diabetes - A Guide For Those With PrediabetesDokument26 SeitenHow To Prevent Diabetes - A Guide For Those With PrediabetesDiabetes CareNoch keine Bewertungen
- Jaundice-Review of Clinical Features, Differential Diagnosis and RemediesDokument13 SeitenJaundice-Review of Clinical Features, Differential Diagnosis and RemediesDr-Dalya ShakirNoch keine Bewertungen
- Live Guide Powerpoint v3Dokument43 SeitenLive Guide Powerpoint v3jonesNoch keine Bewertungen
- Collection, Transportation, Treatment & Disposal of Laboratory WasteDokument51 SeitenCollection, Transportation, Treatment & Disposal of Laboratory WasteYuresh TwayanaNoch keine Bewertungen
- Investigatory Science 10Dokument15 SeitenInvestigatory Science 10Kai KimatoNoch keine Bewertungen
- Daily Lesson Log on Lifestyle and Weight ManagementDokument8 SeitenDaily Lesson Log on Lifestyle and Weight ManagementNoel Isaac Maximo100% (2)
- Hospital AdventistDokument6 SeitenHospital AdventistGina Hong HongNoch keine Bewertungen
- HC Fruits VeggiesDokument4 SeitenHC Fruits VeggiesshallovesuNoch keine Bewertungen
- UN Millennium Development GoalDokument1 SeiteUN Millennium Development GoalEugene SmithNoch keine Bewertungen
- Components of A CommunityDokument4 SeitenComponents of A Communitydominicjimenez33% (3)
- SHS Applied - Inquiries, Investigations and Immersions CG - Spideylab - Com - 2017Dokument4 SeitenSHS Applied - Inquiries, Investigations and Immersions CG - Spideylab - Com - 2017Lexis Anne BernabeNoch keine Bewertungen
- JSS Guide for Community HIV Care and Treatment ActivityDokument47 SeitenJSS Guide for Community HIV Care and Treatment Activityishdo ishdoNoch keine Bewertungen
- Nursing Informatics and Healthcare Policy: Information, and Computer Sciences To Manage andDokument2 SeitenNursing Informatics and Healthcare Policy: Information, and Computer Sciences To Manage andSOLIVEN KING JAMESNoch keine Bewertungen
- Ground Floor (Basement) : Lucile Packard Children's Hospital Stanford HospitalDokument1 SeiteGround Floor (Basement) : Lucile Packard Children's Hospital Stanford Hospitalsamawi ramudNoch keine Bewertungen
- Health Perception and Lifestyle Factors SurveyDokument5 SeitenHealth Perception and Lifestyle Factors SurveyRichie VilaNoch keine Bewertungen
- No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems ModelVon EverandNo Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems ModelBewertung: 5 von 5 Sternen5/5 (2)
- The Millionaire Fastlane: Crack the Code to Wealth and Live Rich for a LifetimeVon EverandThe Millionaire Fastlane: Crack the Code to Wealth and Live Rich for a LifetimeBewertung: 4 von 5 Sternen4/5 (1)
- The 7 Habits of Highly Effective People: The Infographics EditionVon EverandThe 7 Habits of Highly Effective People: The Infographics EditionBewertung: 4 von 5 Sternen4/5 (2475)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNoch keine Bewertungen
- Seeing What Others Don't: The Remarkable Ways We Gain InsightsVon EverandSeeing What Others Don't: The Remarkable Ways We Gain InsightsBewertung: 4 von 5 Sternen4/5 (288)
- The Compound Effect by Darren Hardy - Book Summary: Jumpstart Your Income, Your Life, Your SuccessVon EverandThe Compound Effect by Darren Hardy - Book Summary: Jumpstart Your Income, Your Life, Your SuccessBewertung: 5 von 5 Sternen5/5 (456)
- The 5 Second Rule: Transform your Life, Work, and Confidence with Everyday CourageVon EverandThe 5 Second Rule: Transform your Life, Work, and Confidence with Everyday CourageBewertung: 5 von 5 Sternen5/5 (7)
- Indistractable: How to Control Your Attention and Choose Your LifeVon EverandIndistractable: How to Control Your Attention and Choose Your LifeBewertung: 3.5 von 5 Sternen3.5/5 (4)
- Eat That Frog!: 21 Great Ways to Stop Procrastinating and Get More Done in Less TimeVon EverandEat That Frog!: 21 Great Ways to Stop Procrastinating and Get More Done in Less TimeBewertung: 4.5 von 5 Sternen4.5/5 (3223)
- Uptime: A Practical Guide to Personal Productivity and WellbeingVon EverandUptime: A Practical Guide to Personal Productivity and WellbeingNoch keine Bewertungen
- The Coaching Habit: Say Less, Ask More & Change the Way You Lead ForeverVon EverandThe Coaching Habit: Say Less, Ask More & Change the Way You Lead ForeverBewertung: 4.5 von 5 Sternen4.5/5 (186)
- The One Thing: The Surprisingly Simple Truth Behind Extraordinary ResultsVon EverandThe One Thing: The Surprisingly Simple Truth Behind Extraordinary ResultsBewertung: 4.5 von 5 Sternen4.5/5 (708)
- Summary of Atomic Habits: An Easy and Proven Way to Build Good Habits and Break Bad Ones by James ClearVon EverandSummary of Atomic Habits: An Easy and Proven Way to Build Good Habits and Break Bad Ones by James ClearBewertung: 4.5 von 5 Sternen4.5/5 (557)
- Summary: The 5AM Club: Own Your Morning. Elevate Your Life. by Robin Sharma: Key Takeaways, Summary & AnalysisVon EverandSummary: The 5AM Club: Own Your Morning. Elevate Your Life. by Robin Sharma: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (22)
- Own Your Past Change Your Future: A Not-So-Complicated Approach to Relationships, Mental Health & WellnessVon EverandOwn Your Past Change Your Future: A Not-So-Complicated Approach to Relationships, Mental Health & WellnessBewertung: 5 von 5 Sternen5/5 (85)
- Get to the Point!: Sharpen Your Message and Make Your Words MatterVon EverandGet to the Point!: Sharpen Your Message and Make Your Words MatterBewertung: 4.5 von 5 Sternen4.5/5 (280)
- What's Best Next: How the Gospel Transforms the Way You Get Things DoneVon EverandWhat's Best Next: How the Gospel Transforms the Way You Get Things DoneBewertung: 4.5 von 5 Sternen4.5/5 (33)
- How to Be Better at Almost Everything: Learn Anything Quickly, Stack Your Skills, DominateVon EverandHow to Be Better at Almost Everything: Learn Anything Quickly, Stack Your Skills, DominateBewertung: 4.5 von 5 Sternen4.5/5 (855)
- Quantum Success: 7 Essential Laws for a Thriving, Joyful, and Prosperous Relationship with Work and MoneyVon EverandQuantum Success: 7 Essential Laws for a Thriving, Joyful, and Prosperous Relationship with Work and MoneyBewertung: 5 von 5 Sternen5/5 (38)
- Think Faster, Talk Smarter: How to Speak Successfully When You're Put on the SpotVon EverandThink Faster, Talk Smarter: How to Speak Successfully When You're Put on the SpotBewertung: 5 von 5 Sternen5/5 (1)
- Summary of 12 Rules for Life: An Antidote to Chaos by Jordan B. PetersonVon EverandSummary of 12 Rules for Life: An Antidote to Chaos by Jordan B. PetersonBewertung: 5 von 5 Sternen5/5 (4)
- Mastering Productivity: Everything You Need to Know About Habit FormationVon EverandMastering Productivity: Everything You Need to Know About Habit FormationBewertung: 4.5 von 5 Sternen4.5/5 (21)
- Summary: Hidden Potential: The Science of Achieving Greater Things By Adam Grant: Key Takeaways, Summary and AnalysisVon EverandSummary: Hidden Potential: The Science of Achieving Greater Things By Adam Grant: Key Takeaways, Summary and AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (15)
- Brain Rules (Updated and Expanded): 12 Principles for Surviving and Thriving at Work, Home, and SchoolVon EverandBrain Rules (Updated and Expanded): 12 Principles for Surviving and Thriving at Work, Home, and SchoolBewertung: 4 von 5 Sternen4/5 (702)
- Growth Mindset: 7 Secrets to Destroy Your Fixed Mindset and Tap into Your Psychology of Success with Self Discipline, Emotional Intelligence and Self ConfidenceVon EverandGrowth Mindset: 7 Secrets to Destroy Your Fixed Mindset and Tap into Your Psychology of Success with Self Discipline, Emotional Intelligence and Self ConfidenceBewertung: 4.5 von 5 Sternen4.5/5 (561)