Beruflich Dokumente
Kultur Dokumente
Hand Therapy Program For Muscular Dystrophy 1
Hochgeladen von
api-291380671Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Hand Therapy Program For Muscular Dystrophy 1
Hochgeladen von
api-291380671Copyright:
Verfügbare Formate
OTI 12 (1) crc
14
2/18/05
1:44 PM
Page 14
Occupational Therapy International, 12(1), 14-27, 2005 Whurr Publishers Ltd
Effects of a hand training
programme in five patients with
myotonic dystrophy type 1
ANNA SANDIN ALDEHAG Karolinska University Hospital, Stockholm,
Sweden
HANS JONSSON Karolinska Institute, Stockholm, Sweden
TOR ANSVED Karolinska Institute, Stockholm, Sweden
ABSTRACT: The aim of this study was to evaluate hand function and self-rated
occupational performance before and after specific hand training in five participants
with myotonic dystrophy (MD) type 1. MD is the commonest of the muscular
dystrophies with adult onset and is associated with muscle weakness, wasting and
myotonia. Compensatory techniques and strategies are mostly offered as the only
intervention therapy. In the present study, the participants were their own controls
using pre- and post-test measures. Each participant was tested at intervals a total of
nine times before and nine times after hand training. A hand-held myometer
(Microfet2), Grippit, Purdue Pegboard and self-rated myotonia were used as
outcome measures. Occupational performance was assessed pre- and post-test using
the Canadian Occupational Performance Measurement (COPM) in which the
participants rated their own performance and satisfaction in five self-chosen occupational performance areas. The participants performed hand training for a total of
three months, three times per week using a specific resistance training programme
including Theraputty, a silicone-based putty.
Hand function was significantly increased and a positive change in self-rated
occupational performance was noted after the training period. This study indicates
that hand training has a positive effect on hand function, i.e. motor function and
occupational performance. The present results need to be replicated in a controlled
study including a larger number of patients and over a longer period of time.
Key words: myotonic dystrophy, hand training, occupational performance
Introduction
Muscular dystrophies are a heterogeneous group of inherited disorders, which
are characterized by muscle weakness and wasting, but the severity and distrib-
OTI 12 (1) crc
2/18/05
1:44 PM
Page 15
Myotonic dystrophy and hand training
ution of symptoms may vary considerably (Adams et al., 1997; Zimmermann et
al., 1996; Emery and Rimoin, 1990). Myotonic dystrophy (MD) is the
commonest of the muscular dystrophies with adult onset and is associated with
muscle weakness, wasting and myotonia (Harper, 2001; Swash and Schwartz,
1999). There are at least two phenotypically similar syndromes, MD type 1
(MD1) and MD type 2. Unlike other muscular dystrophies, the progressive
muscle wasting in both forms is not the result of a mutation in a structural
protein-encoding gene, but the exact pathophysiological mechanism is still
unknown (Ansved, 2003). MD is a multisystemic disease, which not only
affects striated muscles but also heart muscle and the smooth muscles of the
gastro-intestinal tract. Cataract and baldness, testicular atrophy, daytime
somnolence, increased insulin resistance, tiredness and cognitive deficits are
common symptoms (Harper, 2001; Swash and Schwartz, 1999).
MD patients have a decreased functional capacity due to muscle weakness
and wasting which negatively affects their activities of daily living (ADL).
The distribution and the severity of functional deficits determine the ADL
problems (Ntterlund, 2001). In this study, patients with MD1 were included.
The few existing studies on the effects of strength training on lower extremities in patients with MD1 show conflicting results (Tollbck et al., 1999;
Lindeman et al., 1995; Wright et al., 1996), but there are no indications of
increased muscle deterioration as a result of training in the short term.
Although low to moderate intensity resistance and endurance training has
been suggested to have a beneficial effect, there is still no evidence that
training can influence the evolution of MD in the long term (Ansved, 2003).
There are no published studies regarding the effects of hand training in
patients with MD. The interventions offered in occupational therapy for
treating MD patients are mostly concentrated on compensatory and adaptive
techniques and strategies. The patients themselves often request hand
training. Therefore it is important not only to elucidate possible positive and
negative effects of training on hand function and everyday activities but also
to implement interventional programmes that are evidence based. The aim of
the present study was to evaluate hand function, i.e. motor function and selfrated occupational performance, in five patients with MD1. The study was
approved by the local ethics committee.
Materials and methods
Participants
Five consecutive participants, as required in single-case design (Franklin et al.,
1997), were asked to participate from the outpatient clinic of the Karolinska
University Hospital. The five participants who entered the study all had
clinical symptoms of MD and had previously been diagnosed as having MD1
with a pathological CTG-expansion at the myotonic dystrophy protein kinase
15
OTI 12 (1) crc
16
2/18/05
1:44 PM
Page 16
Sandin Aldehag, Jonsson and Ansved
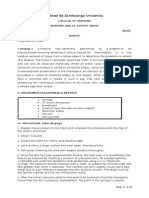
TABLE 1. Clinical data from the five MD1 participants who undertook the 12-week hand
training programme
Subject Age Sex CTG
MMT
in peripheral of the
blood
hand
ext/flex
MMT Occupational Physical
of the activity
activity
wrist
level
ext/flex
Cognitive
impairment
No
67
600900
3/5
4/5
2
3
28
54
M
F
500800
600700
3/5
4/5
4/5
4/5
4
5
56
57
F
F
200300
40145
4/5
3/5
4/5
4/5
Retired
training
Full time
Half time
training
Full time
ERP
Regular
No training No
Regular
No
No training No
No training No
MMT = Manual Muscle Test, ERP = early retirement pension
gene locus on chromosome 19q13.3. They all had a classical MD1 phenotype
including moderate to severe weakness and atrophy of distal limb muscles and
facial muscles, with varying degrees of myotonia (Table 1). The inclusion
criteria were: (1) no other diagnosis that could have an effect on hand function
and, (2) a score of at least 3 out of 5 on the Manual Muscle Test (MMT; 05
scale) in wrist and hand muscles, i.e. the participants were able to demonstrate
a full range of motion against gravity (Hishop and Montgomery, 1995). The
participants included two males (participants 1 and 2) and three females
(participants 3, 4 and 5). The mean age was 52 years (range 2867). Three
participants (2, 3 and 4) were working 50100% of the time, the other two were
either retired or had an early retirement pension (Table 1). Two of the participants (1 and 3) were engaged in regular sport activities prior to and during the
study. They were instructed not to change their training regime during their
participation as their sport activities involved general exercise and could
influence the results of the study. All participants were right-hand dominated
and did not show any obvious cognitive disturbance that would have a negative
effect on participation in the study.
Participant 3
Participant 3 is the only participant for whom individual and descriptive data
are presented, whereas all participants (15) are compared as a group for statistical analyses. Participant 3 represents the group very well with regard to
functional capacity and choice of occupational problems. Participant 3 was a
54-year-old woman who was working part-time in a public library. She was
married and had two grown-up children. Prior to the study she regularly went
to the gym and water-gymnastics once a week and she continued to do so
during the hand training period.
OTI 12 (1) crc
2/18/05
1:44 PM
Page 17
Myotonic dystrophy and hand training
FIGURE 1. Assessing wrist extensor force (left) and finger flexor force (right) with a hand-held
myometer using the break test.
Design
A changing-criterion single-case design was used (Franklin et al., 1997;
Kazdin, 1982). The distinguishing feature of changing-criterion design is that
the participant is required to meet changing criteria of performance, specified
by the therapist, in this case one additional set of repetitions every fourth
week. Conclusions regarding effectiveness of the treatment were made based
on how well the participants performance matched the changing criterion in
addition to pre-test and post-test comparisons (Kazdin, 1982).
Measurements and procedures
The measurements of hand function were performed a total of nine times each
before and after the training period. The pre- and post-tests were performed
three times a week (every other day), one week for pre- and one for post-test.
Each day included three measurements, three times each, i.e. one in the
morning, one at lunchtime and one in the afternoon, approximately 23 hours
apart. However, the measurements for occupational performance and
myotonia were only performed once before and once after training. The
measurements included the following.
Hand-held myometer (Microfet2, Hoggan Industries, Utah, USA)
Wrist and finger extensors and flexors (excluding thumb) were measured with
break-force and three maximum contractions for each muscle group tested.
The break-test was administered and the highest value of three was used.
Measurements were performed nine times pre-training and nine times posttraining. The break-test involved the participant exerting a maximum force
against a hand-held myometer and the examiner applying sufficient resistance
to just overcome the force exerted by the participant (Beverly et al., 2000).
The force of wrist extensors and flexors was assessed with each participant
sitting in front of a table with his or her arm aligned and the elbow flexed in a
80900 angle with the forearm resting on a table on a small pillow either fully
17
OTI 12 (1) crc
18
2/18/05
1:44 PM
Page 18
Sandin Aldehag, Jonsson and Ansved
supinated for flexion or fully pronated for extension (see Figure 1). When the
force of finger extensors was assessed, the participant kept the body and arm
positioned as above in pronation with the wrist in a neutral position with fully
extended fingers. The hand-held myometer was placed over the proximal
interphalangeal (PIP) joints (dorsal side) of the index, long and ring finger, as
the transducer measures 5cm in circumference. When force of finger flexors
was measured, the participant kept his or her body and arm positioned as
above, but supinated with the metacarpophalangeal (MCP) joints 900 flexed
(PIP and distal interphalangeal joints extended). The pressure was put on the
PIP-joints (palmar side) of the index, long and ring finger (Figure 1).
Grippit (Detector AB, Gteborg, Sweden)
Maximum grip force and pinch grip (tip position) was maintained for 10 seconds
and the mean value registered. Grippit is an electronic instrument that measures
isometric grip and pinch force from 0 to 999 Newtons and registration is during
10 seconds. The participant sat in front of a table with both arms resting on the
table; the arm tested was placed in the forearm support of the Grippit fixed on a
wooden board. Hence, the shoulder was adducted and placed in neutral rotation
and the elbow in 80900 flexion with the forearm in neutral and the wrist at
100200 in dorsiflexion with the hand gripped around the elliptical handles (also
fixed on the wooden board). The same position was kept when assessing pinch
grip (tip position). The forearm support of the Grippit made possible a consistent
positioning of the arm from test to test (Wallstrm and Nordenskild, 2001).
Purdue Pegboard Model 32020 (Lafayette Instrument, Lafayette, USA)
Fine motor control of the right and left hand was measured by counting the
number of pins placed on the Pegboard over 30 seconds. The participant was
seated at a table with the Pegboard directly in front of him/her and picked one
pin at a time as fast as possible. Participants were given the opportunity to
practise before the timed test to ensure that they had understood the instructions (Buddenberg and Davis, 2000).
COPM (Canadian Occupational Performance Measure)
A semi-structured interview was performed using the COPM. The occupational problems addressed in self-care, productivity and leisure were then rated
by each participant on a 110 scale with regard to their relative importance.
The participants then chose the five most important self-rated occupational
problems and then rated each on a scale of 110 for both performance and
satisfaction, where 1= not able to perform/not satisfied at all and 10 =
performed extremely well/extremely satisfied (Townsend, 2002). The semistructured interview took approximately 20 minutes per participant.
OTI 12 (1) crc
2/18/05
1:45 PM
Page 19
Myotonic dystrophy and hand training
FIGURE 2. Exercise with mass finger flexion (left) and isolated exercise of thumb flexion (right)
using Theraputty.
Self-rated myotonia
The participants rated the degree of myotonia in their hands both during rest
and during activities on a 110 visual analogue scale, where 1= no myotonia
and 10 = maximal myotonia.
Training
The participants performed hand training three times a week for 12 weeks and
were offered one training session guided by an occupational therapist every
third week. The participants followed a general exercise programme, which
included different exercises with isolated (1-2-3 sets of 3 repetitions or 1-2-3
sets of 5 repetitions) and mass (1-2-3 sets of 10 repetitions or 1-2-3 sets of 15
repetitions) movements with a silicone-based putty, Theraputty (North
Coast Medical, USA), for resistance training (Figure 2). The choice of which
resistance putty to use for each participant and at what initial number of
repetitions was based on participants initial measurements and their ability to
squeeze the resistance putty by demonstrating full finger flexion in all repetitions. Each participant started with 1 set of 35 repetitions in isolated
movements and 1 set of 1015 repetitions in mass movements. An isolated
movement refers to the exercise of one individual finger and mass movements
refer to the exercise of all fingers together except the thumb. The number of
sets was increased by one every fourth week starting with one set of repetitions
during the first week. A stretching programme was also included and
performed after each training session. The stretching programme involved
stretching flexor and extensor muscles in the forearm, hand and fingers. The
training programme was designed to focus on participants functional difficulties, i.e. wrist flexion and extension, finger flexion and extension and
thumb and finger abduction-adduction and also thumb opposition. The
exercise programme was focused on endurance training at low resistance with
a duration of approximately 45 minutes excluding stretching. During both
supervised training and self-training, the participants were seated in front of a
table with the arms aligned and with the elbows flexed at a 900 angle, i.e. with
19
OTI 12 (1) crc
20
2/18/05
1:45 PM
Page 20
Sandin Aldehag, Jonsson and Ansved
the forearms resting on the table surface either in full supination or full
pronation. The exercises included:
1. Wrist exercises (extension/flexion): the participants hand was hanging
over the edge of the table; supinated when performing wrist flexion and
pronated when performing wrist extension.
2. Finger exercises (extension/flexion): the participants forearm was placed
on the table surface in full supination for both finger flexion and extension.
The putty was then placed in the hand (palmar side) when performing
flexion and placed over the distal joints (dorsal side) when performing
extension (Figure 2).
3. Isolated finger movements (index little finger): half of the putty was used. To
perform finger abduction and adduction, the participants forearm was resting
on the table in full pronation. For adduction, the putty was placed between
the fingers, and for abduction it was put around the fingers. For isolated finger
flexion the putty was placed in the palm and the finger to be exercised was
squeeze into it, and wrapped around for extension with finger flexed as the
starting position.
4. Isolated thumb movements (flexion/extension/abduction/adduction): half
of the putty was used (Figure 2). For opposition exercises the putty was
placed on the table, i.e. to enable opposition against the index, middle, ring
and little finger.
The participants were instructed to record all training sessions in a training
diary. The diary was also used by the participants to write down other daily life
tasks that might have an effect on their hand function, i.e. gardening and
baking. The training diary was sent to the therapist weekly to assess
compliance with the hand training programme. The therapist telephoned each
participant once a week to answer questions regarding the training and for
verbal encouragement in order to maintain motivation for maximal performance during the whole training period. The training included a total of 36
training sessions, i.e. three sessions a week for 12 weeks. On average, the
training diaries showed that the participants completed 95% of all training
sessions including the guided training by the occupational therapist as well as
the self-training.
Data analysis
Descriptive data from a single individual (participant 3) representing repetitive measures are presented in Figures 35 with regard to changes in levels or
trend (Franklin et al., 1997). Similar analyses were made for each of the other
participants (not shown). Paired t-test was used for comparisons of mean
values pre- and post-test for the five participants. The level of significance was
set at p < 0.05.
OTI 12 (1) crc
2/18/05
1:45 PM
Page 21
Myotonic dystrophy and hand training
Myometer
W ext R
Newton
150
W ext L
100
W flex R
W flex L
50
F ext R
0
F ext L
1
9 11 13 15 17
No. of Measurements
F flex R
F flex L
FIGURE 3. Muscle force of wrist extensors and flexors and finger extensors and flexors in
participant 3 (R = right, L = left, W = wrist, F = finger, flex = flexors and ext = extensors).
Grippit
Newton
200
Grip Mean R
150
Grip Mean L
100
Pinch Mean R
50
Pinch Mean L
0
1 3
5 7
9 11 13 15 17
No. of Measurements
FIGURE 4. Mean value for grip force and pinch grip in participant 3 (R = right,
L = left, Grip = grip force, Pinch = pinch grip).
Purdue Pegboard
No. of Pins
18
16
R hand
L hand
14
12
10
1
9 11 13 15 17
No. of Measurements
FIGURE 5. Fine motor control in participant 3 (R = right, L = left).
21
OTI 12 (1) crc
22
2/18/05
1:45 PM
Page 22
Sandin Aldehag, Jonsson and Ansved
TABLE 2. Muscle force measured with hand-held myometer in the five participants
Myometer (Newton)
Pre-test
(meanSD)
Post-test
(meanSD)
p value
Right wrist extensors
Left wrist extensors
Right wrist flexors
Left wrist flexors
Right finger extensors
Left finger extensors
Right finger flexors
Left finger flexion
84.220.8
82.216.6
70.320.1
65.015.5
23.94.6
24.23.6
55.514.1
59.313.6
121.821.0
122.818.0
86.215.0
86.315.4
49.911.9
37.318.2
76.018.0
82.317.4
0.0002
0.0004
0.047
0.027
0.0071
0.183*
0.0004
0.0003
* Not significant
TABLE 3. Grip force and pinch grip (tip position) measured with Grippit in the five
participants
Grippit
(Newton)
Pre-test
(meanSD)
Post-test
(meanSD)
p value
Right grip force
Left grip force
Right pinch grip
Left pinch grip
107.328.6
103.922.8
13.310.8
12.48.4
112.927.5
109.018.2
15.711.7
15.28.3
0.099*
0.311*
0.239*
0.062*
* Not significant
Results
Muscle force as measured with myometer
There was a significant increase in muscle force of wrist extensors and flexors
and finger extensors and flexors, except finger extensors of left hand (Table 2).
These results are further illustrated in Figure 3 in which the increase in muscle
force is presented for participant 3. The same trend was also seen in the other
four participants (not shown).
Grip force as measured with Grippit
No statistical significant difference was found regarding grip force or pinch grip
(tip position) measured with Grippit (Table 3). When analysing data for each
individual, an increase in both grip force and pinch grip was noted for participants 4 and 5 (not shown), but not for the others, i.e. participants 1, 2 and 3
(Figure 4).
OTI 12 (1) crc
2/18/05
1:45 PM
Page 23
Myotonic dystrophy and hand training
TABLE 4. Fine motor control measured with Purdue Pegboard in the five participants
Purdue Pegboard
Pre-test
(meanSD)
Post-test
(meanSD)
p value
13.22.1
12.41.9
14.62.0
13.91.8
0.005
0.003
Right hand
Left hand
TABLE 5. Self-rated occupational performance and satisfaction in participant 3 pre- and
post-training
Self-rated ADL problems
Carry bags
Open cans/jars
Vacuum cleaning
Knitting/sewing
Gardening
Mean value
Postpre (mean value)
Performance
(pre)
Performance
(post)
Satisfaction
(pre)
Satisfaction
(post)
3
3
4
1
4
3
4
4
4
4
5
4.2
1
1
1
1
1
1
1
1
1
1
1
1
4.23 = 1.2
11 = 0
Fine motor control
An improved fine motor control, as measured with the Purdue Pegboard, was
obtained after the period of training for both right and left hand (Table 4).
Similar results were noted when individual data for each participant was
analysed (Figure 5).
Occupational performance
The majority of the occupational problems that were chosen by the five participants were areas involving both fine motor control, grip strength and pinch
grip. After the training, all five participants rated higher performance of their
self-rated problems in occupational performance and participants 1, 2, 4 and 5
rated higher satisfaction. The mean ratings of performance increased by 1.7
(range 0.43.8), whereas the mean rating of satisfaction increased by 2.7 (range
06.3). Participant 3 rated her performance slightly higher but the satisfaction
was unchanged (Table 5). When asked, she stated she would only be satisfied
was when she performed as any healthy individual unaffected by MD.
Myotonia
All five participants rated 1 out of 10, i.e. no hand myotonia at rest both preand post-training. Self-rated myotonia during activity was not significantly
23
OTI 12 (1) crc
24
2/18/05
1:45 PM
Page 24
Sandin Aldehag, Jonsson and Ansved
changed by the hand training and was rated 36 out of 10 (mean 3.2) before
and 26 out of 10 (mean 3.0) after the period of training. No participant stated
that his/her myotonia limited performance, either of daily living tasks or
during the hand training with the Theraputty.
Discussion
An increased hand function, i.e. increased motor function as measured by the
hand-held myometer and Purdue Pegboard, was obtained after the period of
training, and a positive change in self-rated occupational problems was also
noted. The findings suggest that a three month hand training regime is safe
and beneficial for hand function in individuals with MD1. However, as the
results are derived from only five participants further research is needed to
confirm these findings.
The authors of the present study emphasize that a single-case design
including repetitive measurements is preferable in this type of patient group as
these patients may fluctuate in function between days, and also between hours,
as seen in this study. To use single-case designs is also preferable in order to get a
better understanding of the effect for each individual. The inclusion criteria, i.e.
for the participants to demonstrate a score of at least 3 out of 5 on the MMT, is
also an important clinical measure when deciding whether it will be worthwhile
for patients to engage in any form of training. If a patient is unable to demonstrate full hand flexion, due to severe atrophy and weakness, resistance training
is unlikely to be beneficial. However, if the individual demonstrates a full range
of motion and some residual muscle strength, there will still be a substantial
amount of functioning muscle fibres left and the patient may be a candidate for
training (Ansved, 2001). Another important issue when deciding if training
might be beneficial is the patients overall life situation, i.e. type of occupation
and engagement in other training activities, hobbies, etc., which may all
influence hand function. The patient may already have a high training level in
which case additional training may be deleterious due to overwork.
Training compliance, as measured by the diary, was high with the participants completing 95% of all training sessions. The training diary, which was
sent to the occupational therapist weekly, the supervised training that was
performed every third week and the weekly phone calls, probably encouraged
the participants to maintain their interest in complying with the training
protocol. Tollbck and associates (1999) noted, in their 12-week study of knee
extension training, that patients with MD1 needed continuous supervision
and verbal encouragement in order to continue the training.
The authors believe that the measurements used to evaluate hand function
in the present study such as the hand-held myometer (Microfet), Grippit and
Purdue Pegboard are good measures of hand function since they assess both
wrist force, grip force, pinch grip and endurance in addition to fine motor
control. One explanation that the Grippit measurements showed some, but
OTI 12 (1) crc
2/18/05
1:45 PM
Page 25
Myotonic dystrophy and hand training
not statistically significant improvements, may be that Grippit measures grip
force mostly generated between the MCP-joints and the thenar muscles of the
thumb (elliptical handle 12.5cm in circumference when assessing grip force).
Microfet, on the other hand, which revealed a statistically significant change
after training, measures the muscle force more distally as the pressure is put on
the distal finger joints, i.e. PIP and DIP joints. Hand training with the Theraputty included mass finger flexion and extension in which the distal joints, i.e.
PIP and DIP joints are specifically exercised.
In future studies the Grip Ability Test (GAT; Dellhag and Bjelle, 1995)
will be used in addition to the Purdue Pegboard to evaluate the effect on hand
function with regard to gross motor function and the ability to handle
different objects.
The visual analogue scale that was used to rate participants myotonia
shows that hand training did not affect participants ability to immediately
relax their muscles after contraction. However, myotonia was not a major
complaint of any of the participants and was not regarded an obstacle in ADL.
The majority of participants rated low myotonia when performing activities
and none during rest. Instead of using a subjective measure one might consider
using different timed tests of myotonia, however evaluation of myotonia was
not a major objective of this study.
The positive change in the participants self-rated occupational problems as
measured by the COPM is an important result, since the end point of any
training study should be improved function, performance and satisfaction in
everyday activities. However, the participants rated occupational performance
subjectively and no objective measures were used. In future studies, objective
measures such as the activities of daily living assessment, Assessment of Motor
and Process Skills (Fisher, 1997), should be considered in addition to the
COPM. Nevertheless, the present results in which the participants chose the
most important occupational problems and then, following functional
training, rated them higher in, for example, performance, is an important
observation, despite the lack of unbiased objective measures. Some participants had difficulties reporting problems in occupational performance even
though they demonstrated decreased hand function. An explanation might be
that they previously had already lost sustained hand function or had become
used to using compensatory strategies and thus remained somewhat unaware of
their functional deficits.
Functional training that addresses only the actual benefits in range of
movement or muscle strength are suggested to be too narrow a focus in occupational therapy (Fisher, 1998). However, if functional training is outlined and
evaluated in the perspective of impact on everyday living it can be considered as
occupational readiness training (Schkade and Schultz, 1992). In this perspective
functional training plays an important role in the rehabilitation process with the
aim that the patient should be as functionally ready as possible to enter their
world of everyday living.
25
OTI 12 (1) crc
26
2/18/05
1:45 PM
Page 26
Sandin Aldehag, Jonsson and Ansved
When comparing the results of each participant it was noted that those
who were not engaged in other training activities, i.e. had a sedentary lifestyle,
showed the best improvement in functional capacity and in self-rated occupational performance as compared to those with active lifestyles prior to and
during the training period. This suggests that the participants who had been
participating regularly in any form of training or in daily living tasks using
hand muscles prior to the study might be closer to their maximum functional
level. However, these participants also improved in both hand function and
self-rated occupational performance, as seen in participant 3, although the
improvement was less pronounced. The present study was not aimed at discovering the mechanisms behind the improved hand function. However, neuronal
adaptation is likely to be a major contributing factor, although purely muscular
factors cannot be ruled out.
In summary, this is the first study of hand training in patients with MD1.
The results suggest that hand function as well as self-rated occupational performance can improve after a three-month training period focused on endurance
and low resistance training. The present results need to be confirmed in a
larger group of MD1 patients. Whether this type of exercise regime has
positive long-term effects needs to be clarified in future studies.
Acknowledgements
This study was supported by grants from Mediciniskt utvecklingsarbete (2002)
at Karolinska Hospital, Forskningsnmnd vrd (2001) and Centrum fr
vrdforskning (2002) at Karolinska Institutet and the Swedish Medical
Research Council no. 3875. Special thanks to Anne Sderlund PhD Reg PT
for helpful advice regarding study design, Claes Cederfjll, PhD Reg Nurse for
statistical assistance, and to Harriet Pandis, Head of the Occupational Therapy
Department, Karolinska Hospital, Sweden.
References
Adams RD, Victor M, Robber AH (1997). Principles of Neurology (6th edn.). New York:
McGraw-Hill, pp. 141431.
Ansved T (2001). Muscle training in muscular dystrophies. Acta Physiologica Scandinavica
171: 35966.
Ansved T (2003). Muscular dystrophies: Influence of physical conditioning on the disease
evolution. Current Opinions in Clinical Nutrition and Metabolic Care 6: 4359.
Beverly A, Sing K, Frank L (2000). Muscle force measured using break testing with a hand-held
myometer in normal subjects aged 20 to 69 years. Archives in Physical Medical Rehabilitation 81: 65361.
Buddenberg LA, Davis C (2000). Test-retest reliability of the Purdue Pegboard Test. American
Journal of Occupational Therapy 54(5): 5558.
Dellhag B, Bjelle A (1995). A Grip Ability Test (GAT) for use in rheumatology practice.
Journal of Rheumatology 22(8): 155965.
Emery AEH, Rimoin DL (1990). Principles and Practice of Medical Genetics (2nd edn.).
OTI 12 (1) crc
2/18/05
1:45 PM
Page 27
Myotonic dystrophy and hand training
Edinburgh: Churchill Livingstone, pp. 53956.
Fisher AG (1997). Assessment of Motor and Process Skills (2nd edn.). Fort Collins, CO: Three
Stars Press.
Fisher AG (1998). United practice and theory in occupational framework. American Journal of
Occupational Therapy 52: 50921.
Franklin R, Allison D, Gorman B (1997). Design and Analysis of Single-Case Research.
Mahwah, NJ: Lawrence Erlbaum Associates.
Hishop HJ, Montgomery J (1995). Daniels and Worthinghams Muscle Testing Techniques of
Manual Examination (6th edn.). Philadelphia, PA: WB Saunders,
Harper P-S (2001). Myotonic Dystrophy (3rd edn.). London: WB Saunders.
Kazdin A (1982). Single-Case Research Designs. Methods for clinical and applied settings. New
York, Oxford: Oxford University Press.
Lindeman E, Leffers P, Spaans F, Drukker J, Kerchkhoffs M, Koke A (1995). Strength training
in patients with myotonic dystrophy and hereditary motor and sensory neuropathy: A
randomized clinical trial. Archives of Physical Medical Rehabilitation 76: 61220.
Ntterlund B (2001). Living with Muscular Dystrophy Illness Experience, Activities of Daily
Living, Coping, Quality of Life and Rehabilitation. Dissertation. Acta Universitatis
Upsaliensis, Uppsala.
Schkade JK, Schultz S (1992). Occupational adaptation. Toward a holistic approach for
contemporary practice. Part 1. American Journal of Occupational Therapy 46: 91725.
Swash M, Schwartz MS (1999). Neuromuscular Diseases A Practical Approach to Diagnosis
and Management (3rd edn.). London: Springer.
Tollbck A, Eriksson S, Wredenberg A, Vargas R, Borg K, Ansved T (1999). Effects of high
resistance training in patients with myotonic dystrophy. Scandinavian Journal of Rehabilitation Medicine 31: 916.
Townsend E (ed.) (2002). Enabling Occupation An Occupational Therapy Perspective.
Ottawa: Canadian Association of Occupational Therapists.
Wallstrm A, Nordenskild U (2001). Assessing hand grip endurance with repetitive maximal
isometric contractions. Journal of Hand Therapy 14(4): 27985.
Wright NC, Kilmer DD, McCrory MA, Aitkens SG, Holcomb BJ, Bernauer EM (1996). Arobic
walking in slowly progressive neuromuscular diseases: Effect of a 12-week program. Archives
of Physical Medical Rehabilitation 77: 649.
Zimmermann CW, Munsat TL, Danek A (1996). Neurological Disorders: Course and
Treatment. San Diego: Academic Press, pp. 97181.
Address correspondence to Anna Sandin Aldehag, Karolinska University Hospital, SOLNA,
Department of Occupational Therapy, Division of Neurology, S-171 76 Stockholm, Sweden.
Tel: + 46 8 517 720 21. E-mail: anna.aldehag@karolinska.se
27
Das könnte Ihnen auch gefallen
- Evidence-Based Final ReflectionDokument2 SeitenEvidence-Based Final Reflectionapi-291380671Noch keine Bewertungen
- Leadership Final ReflectionDokument2 SeitenLeadership Final Reflectionapi-291380671Noch keine Bewertungen
- Aota Goal WritingDokument1 SeiteAota Goal Writingapi-291380671Noch keine Bewertungen
- Nota VolunteeringDokument1 SeiteNota Volunteeringapi-291380671Noch keine Bewertungen
- Kta ArticleDokument6 SeitenKta Articleapi-291380671Noch keine Bewertungen
- 651 A EvaluationDokument5 Seiten651 A Evaluationapi-291380671Noch keine Bewertungen
- Comparison of Occupation-Based Vs Impairment-Based TreatmentDokument12 SeitenComparison of Occupation-Based Vs Impairment-Based Treatmentapi-291380671Noch keine Bewertungen
- Occupation-Based Final ReflectionDokument2 SeitenOccupation-Based Final Reflectionapi-291380671Noch keine Bewertungen
- Rabideau Kitchen Eval AjotDokument8 SeitenRabideau Kitchen Eval Ajotapi-291380671Noch keine Bewertungen
- Defining Cultural CompetenceDokument10 SeitenDefining Cultural Competenceapi-291380671Noch keine Bewertungen
- Leadership Dsosn CertificateDokument1 SeiteLeadership Dsosn Certificateapi-291380671Noch keine Bewertungen
- Fe Course Leadership CertDokument1 SeiteFe Course Leadership Certapi-291380671Noch keine Bewertungen
- Trans PTTDokument43 SeitenTrans PTTapi-292815157100% (1)
- F Kronenberg PteDokument12 SeitenF Kronenberg Pteapi-291380671Noch keine Bewertungen
- Occt 643 Cat Paper-Does Music Therapy Intervention Help Improve Socialization and Communication Skills in Children With Autism Spectrum DisordersDokument11 SeitenOcct 643 Cat Paper-Does Music Therapy Intervention Help Improve Socialization and Communication Skills in Children With Autism Spectrum Disordersapi-291380671Noch keine Bewertungen
- Occt 643 Cat Evidence TableDokument18 SeitenOcct 643 Cat Evidence Tableapi-291380671Noch keine Bewertungen
- Shaping The Goal Setting Process in OtDokument16 SeitenShaping The Goal Setting Process in Otapi-291380671Noch keine Bewertungen
- Edited Home Assessment Melody and KelseyDokument10 SeitenEdited Home Assessment Melody and Kelseyapi-291380671Noch keine Bewertungen
- What Is The Role of The OtDokument15 SeitenWhat Is The Role of The Otapi-291380671Noch keine Bewertungen
- 651 A EvaluationDokument4 Seiten651 A Evaluationapi-291380671Noch keine Bewertungen
- 527a EvaluationDokument4 Seiten527a Evaluationapi-291380671Noch keine Bewertungen
- ResumeDokument3 SeitenResumeapi-291380671Noch keine Bewertungen
- Occt 649-Assistive Technology Paper - The Brush BuddyDokument13 SeitenOcct 649-Assistive Technology Paper - The Brush Buddyapi-291380671Noch keine Bewertungen
- Occupational Profile and Intervention Plan TimDokument20 SeitenOccupational Profile and Intervention Plan Timapi-291380671Noch keine Bewertungen
- 526a EvaluationDokument5 Seiten526a Evaluationapi-291380671Noch keine Bewertungen
- Occt 506 - Occupational Analysis Intervention PlanDokument21 SeitenOcct 506 - Occupational Analysis Intervention Planapi-291380671Noch keine Bewertungen
- 630a EvaluationDokument6 Seiten630a Evaluationapi-291380671Noch keine Bewertungen
- Occt 630-Occupational Profile Intervention PlanDokument19 SeitenOcct 630-Occupational Profile Intervention Planapi-291380671Noch keine Bewertungen
- Running Head: CASE STUDY 1Dokument20 SeitenRunning Head: CASE STUDY 1api-292536235Noch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Cardiac CycleDokument2 SeitenCardiac CycleU Than HanNoch keine Bewertungen
- Route of Administration PDFDokument45 SeitenRoute of Administration PDFBurhan MubasharNoch keine Bewertungen
- Subcutaneous MycosesDokument23 SeitenSubcutaneous Mycosessarguss14100% (1)
- Dental instruments for extracting teethDokument18 SeitenDental instruments for extracting teethKateryna BondarenkoNoch keine Bewertungen
- The Abc of Handover: E.D. Registrar A: Areas AllocationDokument1 SeiteThe Abc of Handover: E.D. Registrar A: Areas AllocationDiahNiatiNoch keine Bewertungen
- Care of High Risk Newborn - ChaboyDokument9 SeitenCare of High Risk Newborn - Chaboychfalguera0% (1)
- Growth PredictionDokument101 SeitenGrowth PredictionKristty Magallanes100% (1)
- Srinu Chemical Plaque ControlDokument80 SeitenSrinu Chemical Plaque ControlGorremuchu SrinivasNoch keine Bewertungen
- Development of Push-Pull Osmotic Pump Tablets For A SlightlyDokument4 SeitenDevelopment of Push-Pull Osmotic Pump Tablets For A SlightlyphamuyenthuNoch keine Bewertungen
- Anderson2008 Levofloxasin A ReviewDokument31 SeitenAnderson2008 Levofloxasin A ReviewFazdrah AssyuaraNoch keine Bewertungen
- R3 Vital Pulp Therapy With New MaterialsDokument7 SeitenR3 Vital Pulp Therapy With New MaterialsWening TyasNoch keine Bewertungen
- IM Injuction: Definition of Intramuscular InjectionDokument8 SeitenIM Injuction: Definition of Intramuscular InjectiondhanasundariNoch keine Bewertungen
- 148-Article Text-565-1-10-20211005Dokument11 Seiten148-Article Text-565-1-10-20211005sri wahyundari manikNoch keine Bewertungen
- Subfalcine Herniation Damages Cingulate GyrusDokument34 SeitenSubfalcine Herniation Damages Cingulate GyrusLorenzo FrancisNoch keine Bewertungen
- Ross University 2010-2011 Pre-Residency Planning GuideDokument61 SeitenRoss University 2010-2011 Pre-Residency Planning GuidescatteredbrainNoch keine Bewertungen
- Montelukast SodiumDokument10 SeitenMontelukast SodiumikhasilNoch keine Bewertungen
- Psycho Sexual 6ceu CourseDokument78 SeitenPsycho Sexual 6ceu CourseariizianaNoch keine Bewertungen
- Healthcare Financing in IndiADokument86 SeitenHealthcare Financing in IndiAGeet Sheil67% (3)
- Ateneo de Zamboanga University Nursing Skills Output (NSO) Week BiopsyDokument4 SeitenAteneo de Zamboanga University Nursing Skills Output (NSO) Week BiopsyHaifi HunNoch keine Bewertungen
- Phobiasgalore1 2Dokument2 SeitenPhobiasgalore1 2api-264827695Noch keine Bewertungen
- 37 Percent Formaldehyde Aqueous Solution Mixture of Hcho Ch3oh and H2o Sds p6224Dokument12 Seiten37 Percent Formaldehyde Aqueous Solution Mixture of Hcho Ch3oh and H2o Sds p6224Juan Esteban LopezNoch keine Bewertungen
- STG-General Hospital PDFDokument704 SeitenSTG-General Hospital PDFBirhane100% (1)
- 1583 - Intermediate Grammar Test 22Dokument4 Seiten1583 - Intermediate Grammar Test 22SabinaNoch keine Bewertungen
- Practice Quiz - Maternity & NewbornDokument4 SeitenPractice Quiz - Maternity & NewbornMS100% (1)
- Jan Marc Bulatao 10-Einstein BiologyDokument3 SeitenJan Marc Bulatao 10-Einstein BiologyNomer SenadorNoch keine Bewertungen
- High Level Technical Meeting On Health Risks at The Human-Animal-Ecosystems Interfaces Mexico City, Mexico 15-17 November 2011Dokument7 SeitenHigh Level Technical Meeting On Health Risks at The Human-Animal-Ecosystems Interfaces Mexico City, Mexico 15-17 November 2011d3bd33pNoch keine Bewertungen
- Medication - ALT-Template - Docusate SodiumDokument1 SeiteMedication - ALT-Template - Docusate SodiumNancyAmissahNoch keine Bewertungen
- Gas Transport 2Dokument29 SeitenGas Transport 2Charmaine LucNoch keine Bewertungen
- Aspirin: The widely used pain reliever and fever reducerDokument4 SeitenAspirin: The widely used pain reliever and fever reducerEithel EithelNoch keine Bewertungen