Beruflich Dokumente
Kultur Dokumente
Gastrointestinal Stromal Tumors
Hochgeladen von
polygoneCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Gastrointestinal Stromal Tumors
Hochgeladen von
polygoneCopyright:
Verfügbare Formate
Gastrointestinal Stromal Tumors
1 of 12
http://emedicine.medscape.com/article/179669-overview
Today
News
Reference
Education
Log In
Register
Gastrointestinal Stromal Tumors
Author: Nancy S Behazin, MD; Chief Editor: Julian Katz, MD more...
Updated: Mar 11, 2013
Practice Essentials
Gastrointestinal stromal tumors (GISTs) account for less than 1% of gastrointestinal tumors, but they are the most
common mesenchymal neoplasms of the gastrointestinal tract. GISTs are usually found in the stomach or small
intestine but can occur anywhere along the GI tract and rarely have extra-GI involvement.
Essential update: FDA approves regorafenib for GIST
Regorafenib (Stivarga) received FDA approval for locally advanced, unresectable GISTs that no longer respond to
imatinib or sunitinib. The pivotal phase III GRID trial of 199 patients with metastatic or unresectable GIST showed
that regorafenib plus best supportive care (BSC) significantly improved progression-free survival (PFS) compared to
placebo plus BSC. Patients were treated with BSC and randomized in a 2:1 ratio to either regorafenib (160 mg daily
for 3 weeks followed by a 1-week break) or placebo. Median PFS was 4.8 months for regorafenib and 0.9 months for
placebo.
[1, 2]
Signs and symptoms
Up to 75% of GISTs are discovered when they are less than 4 cm in diameter and are either asymptomatic or
associated with nonspecific symptoms. They are frequently diagnosed incidentally during radiologic studies or
endoscopic or surgical procedures performed to investigate GI tract disease or to treat an emergent condition such
as hemorrhage, obstruction, or perforated viscus. Clinical manifestations of GISTS are as follows:
Vague, nonspecific abdominal pain or discomfort (most common)
Early satiety or a sensation of abdominal fullness
Palpable abdominal mass (rare)
Malaise, fatigue, or exertional dyspnea with significant blood loss
Focal or widespread signs of peritonitis (with perforation)
Obstructive signs and symptoms of GISTs can be site-specific, as follows:
Dysphagia with an esophageal GIST
Constipation and a distended, tender abdomen with a colorectal GIST
Obstructive jaundice with a duodenal GIST
See Clinical Presentation for more detail.
Diagnosis
No laboratory test can specifically confirm or rule out the presence of a GIST. The following tests are generally
ordered in the workup of patients who present with nonspecific abdominal symptoms; abdominal pain; or
complications of a GIST-like hemorrhage, obstruction, or perforation:
Complete blood cell count
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
2 of 12
http://emedicine.medscape.com/article/179669-overview
Coagulation profile
Serum chemistry studies
BUN and creatinine
Liver function tests and amylase and lipase values
Type and screen, type and crossmatch
Serum albumin
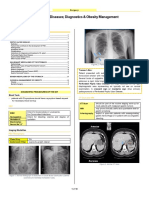
Imaging studies
Plain abdominal radiography:
Nonspecific
May be part of an emergent workup
Abnormal gas patterns, including dilated loops of bowel or free extraluminal air, may be seen with bowel
obstruction or perforation
Barium and air (double-contrast) series:
Frequently provides only limited information
Can usually detect GISTs that have grown to a size sufficient to produce symptoms
Barium swallow for patients with dysphagia
Barium enema for patients with constipation, decreased stool caliber, or colonic manifestations
[3]
GISTs appear as an elevated, sharply demarcated filling defect
The overlying mucosa typically has a smooth contour unless ulceration has developed
Computed tomography scans of the abdomen and pelvis:
Important in the diagnosis and staging of GISTs
Provides comprehensive information regarding the size and location of the tumor and its relationship to
adjacent structures
Can also be used to detect the presence of multiple tumors and of metastatic spreadCT characteristics of small
[4]
GISTs (< 5 cm) are as follows
Sharply demarcated
Homogeneous density
Mainly exhibit intraluminal growth patterns
[4]
CT characteristics of intermediate GISTs (5-10 cm) are as follows
Irregular shape
Heterogeneous density
An intraluminal and extraluminal growth pattern
Signs of biological aggression, sometimes including adjacent organ infiltration
[4]
CT characteristics of large GISTs (>10 cm) are as follows
[4]
Irregular margins
Heterogeneous densities
Locally aggressive behavior
Distant and peritoneal metastases
[5]
CT criteria associated with high-grade histology and increased mortality
Tumor larger than 11.1 cm
Irregular surface contours
Indistinct margins
Adjacent organ invasion
Heterogeneous enhancement
Hepatic or peritoneal metastasis
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
3 of 12
http://emedicine.medscape.com/article/179669-overview
Magnetic resonance imaging:
Like CT scanning, MRI can depict tumors and yield information about surrounding structures
Can also be used to detect the presence of multiple tumors and metastases
[6]
Less well studied than CT for diagnosing GISTs, but appears equally sensitive
[7]
GISTs may appear hypointense on T2-weighted images
Positron emission tomography scanning with 2-[F-18]-fluoro-2-deoxy-D-glucose has the following uses:
Detection metastatic disease
Monitoring of response to adjuvant therapy (eg, imatinib mesylate)
Endoscopy:
Frequently performed early in the workup of patients with GI bleeding, abdominal pain, or GI obstructive
symptoms from GISTs
Endoscopic features of GISTs include the suggestion of a smooth submucosal mass displacing the overlying
mucosa
[8]
Ulceration or bleeding of the overlying mucosa from pressure necrosis may be present
Problematic for biopsy specimen collection because of the submucosal location of GISTs
Endoscopic biopsy results yield a diagnosis in less than 50% of cases
Obtaining a repeat biopsy in the same site as a prior biopsy may increase the diagnostic yield
Endoscopic ultrasonography (EUS):
Allows localization of lesions and their characterization by ultrasonography
Fine-needle aspiration biopsy specimens may be obtained under sonographic guidance
GISTs typically appear as a hypoechoic mass in the layer corresponding to the muscularis propria
[9]
Complementary with CT
More accurate than CT in differentiating benign from malignant lesions
Allows a more comprehensive evaluation of the mass and the surrounding structures than CT
[10]
EUS characteristics of malignant GISTs include the following
Size larger than 4 cm (the only independent predictor)
Heterogeneous echogenicity
Internal cystic areas
Irregular borders on the extraluminal surfaces
[11]
EUS features that may help differentiate gastric GISTs from leiomyomas are as follows
Inhomogenicity
Hyperechogenic spots
A marginal halo
Higher echogenicity than the surrounding muscle layer
Aspects of EUS-guided biopsy are as follows:
Biopsy provides definitive diagnosis
Biopsy may be required when preoperative therapy is needed in cases where the tumor is unresectable or
only marginally resectable
Biopsy may not be necessary if the tumor is surgically resectable and preoperative medical therapy is not
required
See Workup for more detail.
Management
Surgery is the definitive therapy for patients with GISTs, as follows:
Radical and complete surgical extirpation offers the only chance for cure
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
4 of 12
http://emedicine.medscape.com/article/179669-overview
Surgery is also indicated in symptomatic patients with locally advanced or metastatic disease
Debulking large lesions is helpful when adjuvant therapy is contemplated
Laparoscopic resection has improved and is a more frequently considered option
Imatinib mesylate is used in GIST as follows:
Adjuvant therapy post complete surgical resection in patients with high-risk tumors
Neoadjuvant therapy with goal of tumor shrinkage prior to surgical resection
Other tyrosine kinase inhibitors used when imatinib is not tolerated or not effective are as follows:
Sunitinib: Less specific than imatinib; approved as a second-line agent for advanced GIST
Sorafenib: Investigational second-generation agent
Dasatinib: Investigational second-generation agent
Nilotinib: Investigational second-generation agent
See Treatment and Medication for more detail.
Background
Gastrointestinal stromal tumors (GISTs) account for less than 1% of gastrointestinal tumors, however, are the most
common mesenchymal neoplasms of the gastrointestinal tract. GISTs are usually found in the stomach or small
intestine but can occur anywhere along the gastrointestinal tract and rarely have extragastrointestinal
[12]
involvement.
GISTs rank a distant third in prevalence behind adenocarcinomas and lymphomas among the
histologic types of gastrointestinal tract tumors.
Historically, these lesions were classified as leiomyomas or leiomyosarcomas because they possessed smooth
muscle features when examined under light microscopy. In the 1970s electron microscopy found little evidence of the
smooth muscle origin of these tumors. In the 1980s, with the advent of immunohistochemistry, it was shown that
these tumors did not have immunophenotypic features of smooth muscle cells and rather expressed antigens related
to neural crest cells. Mazur and Clark in 1983, and Schaldenbrand and Appleman in 1984 were the first to describe
"stromal tumors" as a separate entity.
According to the work of Kindblom and associates reported in 1998, the actual cell of origin of GISTs is a
[13]
pluripotential mesenchymal stem cell programmed to differentiate into the interstitial cell of Cajal.
These are GI
pacemaker cells found in the muscularis propria and around the myenteric plexus and are largely responsible for
initiating and coordinating GI motility. This finding led Kindblom and coworkers to suggest the term GI pacemaker cell
[13]
tumors.
Additional studies found that interstitial cells of Cajal express KIT and are developmentally dependent on
stem cell factor, which is regulated through KIT kinase. Perhaps the most critical development that distinguished
GISTs as a unique clinical entity was the discovery of c-kit proto-oncogene mutations in these tumors in by Hirota
and colleagues in 1998.
[14]
These advances have led to the classification of GISTs as an entity separate from smooth muscle tumors, helped
elucidate their etiology and pathogenesis at a molecular level, and led to the development of molecular-targeted
therapy for this disease.
Pathophysiology
GISTs can occur anywhere in the gastrointestinal tract. They are submucosal lesions, which most frequently grow
endophytically in parallel with the lumen of the affected structure. GISTs may also manifest as exophytic extraluminal
excrescences. These tumors have been reported ranging in size from smaller than 1 cm to as large as 40 cm in
[15]
diameter.
Approximately 50-70% of GISTs originate in the stomach. The small intestine is the second most
common location, with 20-30% of GISTs arising from the jejunoileum. Less frequent sites of occurrence include the
colon and rectum (5-15%) and esophagus (< 5%). Primary pancreatic, omental, or mesenteric GISTs have been
reported but are very rare.
[12]
Frequency
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
5 of 12
http://emedicine.medscape.com/article/179669-overview
United States
Roughly 5000 new cases of gastrointestinal stromal tumors are diagnosed annually in the United States.
International
Population-based studies from Iceland, the Netherlands, Spain, and Sweden report annual incidence rates ranging
from 6.5 to 14.5 cases per million.
Mortality/Morbidity
Outcomes in patients with GISTs are highly dependent on the clinical presentation and the histopathological features
of the tumor. The overall 5-year survival rate ranges from 28-60%. This can be stratified for patients presenting with
localized primary disease and those presenting with metastatic or recurrent disease. The median survival rate in the
former group is 5 years, while the median survival rate in the latter group is approximately 10-20 months. Larger
GISTs are associated with complications such as GI hemorrhage, GI obstruction, and bowel perforation. This is
discussed further in Surgical Care and Complications.
Tumors can be classified into high and low-risk categories based on size, location, and mitotic activity. The
implications of these tumor characteristics are discussed in Prognosis and Histologic Findings.
Race
GISTs have no known racial proclivity. However, Cheung et al reported that out of 3795 patients diagnosed with
mesenchymal tumors from the Surveillance, Epidemiology, and End Results (SEER) database from 1992-2005,
more than 88% of tumors were identified as GIST with patient demographics as follows: 72.2% Caucasians, 15.6%
[3]
African Americans, and 9.1% Hispanics.
Sex
SEER (Surveillance, Epidemiology, and End Results) data from 1992-2000 report a slightly higher prevalence in
[4]
males versus females, at 54% and 46%, respectively.
Age
GISTs have been reported in all age groups including infants. It is extremely rare in patients younger than 30 years.
[15]
In a study of 1765 gastric GISTs, the median age at diagnosis was 63 years.
In a series consisting of 906 jejunal
[5]
and ileal GISTs, the mean age was 59 years. In the latter 2 series, only 2.7% of gastric GISTs and 0.6% of small
bowel GISTs were detected in patients younger than 21 years.
Contributor Information and Disclosures
Author
Nancy S Behazin, MD Fellow, Department of Gastroenterology, Scott and White Hospital, Texas A&M Health
Science Center College of Medicine
Nancy S Behazin, MD is a member of the following medical societies: American College of Gastroenterology,
American College of Physicians, American Medical Association, American Society of Gastrointestinal Endoscopy,
and Texas Medical Association
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College
of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Noel Williams, MD Professor Emeritus, Department of Medicine, Dalhousie University, Halifax, Nova Scotia,
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
6 of 12
http://emedicine.medscape.com/article/179669-overview
Canada; Professor, Department of Internal Medicine, Division of Gastroenterology, University of Alberta,
Edmonton, Alberta, Canada
Noel Williams, MD is a member of the following medical societies: Royal College of Physicians and Surgeons of
Canada
Disclosure: Nothing to disclose.
Alex J Mechaber, MD, FACP Senior Associate Dean for Undergraduate Medical Education, Associate Professor
of Medicine, University of Miami Miller School of Medicine
Alex J Mechaber, MD, FACP is a member of the following medical societies: Alpha Omega Alpha, American
College of Physicians-American Society of Internal Medicine, and Society of General Internal Medicine
Disclosure: Nothing to disclose.
Chief Editor
Julian Katz, MD Clinical Professor of Medicine, Drexel University College of Medicine
Julian Katz, MD is a member of the following medical societies: American College of Gastroenterology, American
College of Physicians, American Gastroenterological Association, American Geriatrics Society, American Medical
Association, American Society for Gastrointestinal Endoscopy, American Society of Law, Medicine & Ethics,
American Trauma Society, Association of American Medical Colleges, and Physicians for Social Responsibility
Disclosure: Nothing to disclose.
Additional Contributors
Robert A Decker, MD Clinical Assistant Professor, Department of Medicine, University of Hawaii at Manoa: Chief,
Gastroenterology Service, Kaiser Permanente Medical Center of Honolulu
Disclosure: Nothing to disclose.
Sandeep Mukherjee, MB, BCh, MPH, FRCPC Associate Professor, Department of Internal Medicine, Section of
Gastroenterology and Hepatology, University of Nebraska Medical Center; Consulting Staff, Section of
Gastroenterology and Hepatology, Veteran Affairs Medical Center
Sandeep Mukherjee, MB, BCh, MPH, FRCPC is a member of the following medical societies: Royal College of
Physicians and Surgeons of Canada
Disclosure: Merck Honoraria Speaking and teaching; Ikaria Pharmaceuticals Honoraria Board membership
Michael AJ Sawyer, MD Consulting Staff, Department of Surgery, Southwestern Medical Center; Consulting
Staff, Department of Surgery, Comanche County Memorial Hospital; Consulting Staff, Great Plains Surgical Clinic,
Inc
Michael AJ Sawyer, MD is a member of the following medical societies: American College of Surgeons, Society
for Surgery of the Alimentary Tract, Society of American Gastrointestinal and Endoscopic Surgeons, and Society
of Laparoendoscopic Surgeons
Disclosure: Nothing to disclose.
References
1. Demetri GD, Reichardt P, Kang YK, Blay JY, Rutkowski P, Gelderblom H, et al. Efficacy and safety of
regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an
international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. Jan 26
2013;381(9863):295-302. [Medline].
2. Chustecka Z. Regorafenib Approved for Gastrointestinal Stromal Tumors. Available at
http://www.medscape.com/viewarticle/779854. Accessed March 5, 2013.
3. Cheung MC, Zhuge Y, Yang R, Koniaris LG. Disappearance of racial disparities in gastrointestinal stromal
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
7 of 12
http://emedicine.medscape.com/article/179669-overview
tumor outcomes. J Am Coll Surg. Jul 2009;209(1):7-16. [Medline].
4. Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis
of 1,458 cases from 1992 to 2000. Am J Gastroenterol. Jan 2005;100(1):162-8. [Medline].
5. Miettinen M, Makhlouf H, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the jejunum and ileum: a
clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with
long-term follow-up. Am J Surg Pathol. Apr 2006;30(4):477-89. [Medline].
6. Nilsson B, Bumming P, Meis-Kindblom JM, Oden A, Dortok A, Gustavsson B. Gastrointestinal stromal
tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era--a
population-based study in western Sweden. Cancer. Feb 15 2005;103(4):821-9. [Medline].
7. Heinrich MC, Corless CL, Demetri GD, et al. Kinase mutations and imatinib response in patients with
metastatic gastrointestinal stromal tumor. J Clin Oncol. Dec 1 2003;21(23):4342-9. [Medline].
8. Ghanem N, Altehoefer C, Furtwangler A, et al. Computed tomography in gastrointestinal stromal tumors.
Eur Radiol. Jul 2003;13(7):1669-78. [Medline].
9. Zhou HY, Zhang XM, Zeng NL, Jian SH, Tang W. Use of conventional MR imaging and diffusion-weighted
imaging for evaluating the risk grade of gastrointestinal stromal tumors. J Magn Reson Imaging. Dec
2012;36(6):1395-401. [Medline].
10. Tateishi U, Hasegawa T, Satake M, Moriyama N. Gastrointestinal stromal tumor. Correlation of computed
tomography findings with tumor grade and mortality. J Comput Assist Tomogr. Sep-Oct 2003;27(5):792-8.
[Medline].
11. Shojaku H, Futatsuya R, Seto H, Tajika S, Matsunou H. Malignant gastrointestinal stromal tumor of the
small intestine: radiologic-pathologic correlation. Radiat Med. May-Jun 1997;15(3):189-92. [Medline].
12. Zhao X, Yue C. Gastrointestinal stromal tumor. J Gastrointest Oncol. Sep 2012;3(3):189-208. [Medline].
[Full Text].
13. Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor
(GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal.
Am J Pathol. May 1998;152(5):1259-69. [Medline]. [Full Text].
14. Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal
tumors. Science. Jan 23 1998;279(5350):577-80. [Medline].
15. Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic,
immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg
Pathol. Jan 2005;29(1):52-68. [Medline].
16. Yamashita F, Sasatomi E, Kiyama M, et al. Radiographic observation of a case of gastrointestinal stromal
tumor in stomach. Kurume Med J. 2001;48(3):233-6. [Medline].
17. Stroobants S, Goeminne J, Seegers M, et al. 18FDG-Positron emission tomography for the early prediction
of response in advanced soft tissue sarcoma treated with imatinib mesylate (Glivec). Eur J Cancer. Sep
2003;39(14):2012-20. [Medline].
18. Pidhorecky I, Cheney RT, Kraybill WG, Gibbs JF. Gastrointestinal stromal tumors: current diagnosis, biologic
behavior, and management. Ann Surg Oncol. Oct 2000;7(9):705-12. [Medline].
19. Chak A, Canto MI, Rosch T, et al. Endosonographic differentiation of benign and malignant stromal cell
tumors. Gastrointest Endosc. Jun 1997;45(6):468-73. [Medline].
20. Belloni M, De Fiori E, Mazzarol G, Curti A, Crosta C. Endoscopic ultrasound and Computed Tomography in
gastric stromal tumours. Radiol Med. Jan-Feb 2002;103(1-2):65-73. [Medline].
21. Kim GH, Park do Y, et al. Is it possible to differentiate gastric GISTs from gastric leiomyomas by EUS?.
World J Gastroenterol. Jul 21 2009;15(27):3376-81. [Medline]. [Full Text].
22. Gordon BM, Herlong J, Uflacker R, Gordon L. Recurrent lower gastrointestinal hemorrhage: ileal neoplasm
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
8 of 12
http://emedicine.medscape.com/article/179669-overview
diagnosed by scintigraphy with Tc 99m red blood cells and angiography. South Med J. Dec
1996;89(12):1204-7. [Medline].
23. Au VW, Peh WC. Clinics in diagnostic imaging (16). Lower gastrointestinal bleeding caused by ileal tumour.
Singapore Med J. Aug 1996;37(4):434-7. [Medline].
24. Nakagawa M, Akasaka Y, Kanai T, et al. Extragastrointestinal stromal tumor of the greater omentum: case
report and review of the literature. Hepatogastroenterology. May-Jun 2003;50(51):691-5. [Medline].
25. Suzuki K, Kaneko G, Kubota K, et al. Malignant tumor, of the gastrointestinal stromal tumor type, in the
greater omentum. J Gastroenterol. 2003;38(10):985-8. [Medline].
26. Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: A consensus
approach. Hum Pathol. May 2002;33(5):459-65. [Medline].
27. Koh Y, Lee HE, Oh DY, et al. The lack of CD34 expression in gastrointestinal stromal tumors is related to
cystic degeneration following imatinib use. Jpn J Clin Oncol. Nov 2012;42(11):1020-7. [Medline].
28. Woodall CE 3rd, Brock GN, Fan J, et al. An evaluation of 2537 gastrointestinal stromal tumors for a
proposed clinical staging system. Arch Surg. Jul 2009;144(7):670-8. [Medline].
29. Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced
gastrointestinal stromal tumors. N Engl J Med. Aug 15 2002;347(7):472-80. [Medline].
30. Dematteo RP, Ballman KV, Antonescu CR, Maki RG, Pisters PW, Demetri GD. Adjuvant imatinib mesylate
after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebocontrolled trial. Lancet. Mar 28 2009;373(9669):1097-104. [Medline].
31. Joensuu H, Eriksson M, Sundby Hall K, Hartmann JT, Pink D, Schutte J. One vs three years of adjuvant
imatinib for operable gastrointestinal stromal tumor: a randomized trial. JAMA. Mar 28
2012;307(12):1265-72. [Medline].
32. Demetri GD, von Mehren M, Antonescu CR, et al. NCCN Task Force report: update on the management of
patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. Apr 2010;8 Suppl 2:S1-41; quiz
S42-4. [Medline].
33. Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced
gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. Oct 14
2006;368(9544):1329-38. [Medline].
34. George S, Blay JY, Casali PG, Le Cesne A, Stephenson P, Deprimo SE. Clinical evaluation of continuous
daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib
failure. Eur J Cancer. Jul 2009;45(11):1959-68. [Medline].
35. Wu PC, Langerman A, Ryan CW, Hart J, Swiger S, Posner MC. Surgical treatment of gastrointestinal
stromal tumors in the imatinib (STI-571) era. Surgery. Oct 2003;134(4):656-65; discussion 665-6. [Medline].
36. Besana-Ciani I, Boni L, Dionigi G, Benevento A, Dionigi R. Outcome and long term results of surgical
resection for gastrointestinal stromal tumors (GIST). Scand J Surg. 2003;92(3):195-9. [Medline].
37. Chen YH, Liu KH, Yeh CN, et al. Laparoscopic resection of gastrointestinal stromal tumors: safe, efficient,
and comparable oncologic outcomes. J Laparoendosc Adv Surg Tech A. Oct 2012;22(8):758-63. [Medline].
38. El-Gendi A, El-Gendi S, El-Gendi M. Feasibility and oncological outcomes of limited duodenal resection in
patients with primary nonmetastatic duodenal GIST. J Gastrointest Surg. Dec 2012;16(12):2197-202.
[Medline].
39. Druker BJ, Tamura S, Buchdunger E, et al. Effects of a selective inhibitor of the Abl tyrosine kinase on the
growth of Bcr-Abl positive cells. Nat Med. May 1996;2(5):561-6. [Medline].
40. Druker BJ, Talpaz M, Resta DJ, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine
kinase in chronic myeloid leukemia. N Engl J Med. Apr 5 2001;344(14):1031-7. [Medline].
41. Buchdunger E, Zimmermann J, Mett H, et al. Inhibition of the Abl protein-tyrosine kinase in vitro and in vivo
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
9 of 12
http://emedicine.medscape.com/article/179669-overview
by a 2-phenylaminopyrimidine derivative. Cancer Res. Jan 1 1996;56(1):100-4. [Medline].
42. Heinrich MC, Griffith DJ, Druker BJ, Wait CL, Ott KA, Zigler AJ. Inhibition of c-kit receptor tyrosine kinase
activity by STI 571, a selective tyrosine kinase inhibitor. Blood. Aug 1 2000;96(3):925-32. [Medline].
43. Tuveson DA, Willis NA, Jacks T, et al. STI571 inactivation of the gastrointestinal stromal tumor c-KIT
oncoprotein: biological and clinical implications. Oncogene. Aug 16 2001;20(36):5054-8. [Medline].
44. Blanke CD, von Mehren M, Joensuu H, et al. Presented at: American Society of Clinical Oncology 37th
Annual Meeting. In: Evaluation of the safety and efficacy of an oral molecularly-targeted therapy, STI571, in
patients with unresectable or metastatic gastrointestinal stromal tumors expressing C-KIT. Vol 20. San
Francisco, Calif; 2001:abst 2.
45. van Oosterom AT, Judson IR, Verweij J, et al. Update of phase I study of imatinib (STI571) in advanced soft
tissue sarcomas and gastrointestinal stromal tumors: a report of the EORTC Soft Tissue and Bone Sarcoma
Group. Eur J Cancer. Sep 2002;38 Suppl 5:S83-7. [Medline].
46. Rink L, Skorobogatko Y, Kossenkov AV, et al. Gene expression signatures and response to imatinib
mesylate in gastrointestinal stromal tumor. Mol Cancer Ther. Aug 2009;8(8):2172-82. [Medline]. [Full Text].
47. Dematteo RP, Heinrich MC, El-Rifai WM, Demetri G. Clinical management of gastrointestinal stromal
tumors: before and after STI-571. Hum Pathol. May 2002;33(5):466-77. [Medline].
48. Crosby JA, Catton CN, Davis A, et al. Malignant gastrointestinal stromal tumors of the small intestine: a
review of 50 cases from a prospective database. Ann Surg Oncol. Jan-Feb 2001;8(1):50-9. [Medline].
49. Carney JA. Gastric stromal sarcoma, pulmonary chondroma, and extra-adrenal paraganglioma (Carney
Triad): natural history, adrenocortical component, and possible familial occurrence. Mayo Clin Proc. Jun
1999;74(6):543-52. [Medline].
50. Conlon KC, Casper ES, Brennan MF. Primary gastrointestinal sarcomas: analysis of prognostic variables.
Ann Surg Oncol. Jan 1995;2(1):26-31. [Medline].
51. Dougherty MJ, Compton C, Talbert M, Wood WC. Sarcomas of the gastrointestinal tract. Separation into
favorable and unfavorable prognostic groups by mitotic count. Ann Surg. Nov 1991;214(5):569-74.
[Medline].
52. Adams VR, Leggas M. Sunitinib malate for the treatment of metastatic renal cell carcinoma and
gastrointestinal stromal tumors. Clin Ther. Jul 2007;29(7):1338-53. [Medline].
53. Agaram NP, Wong GC, Guo T, et al. Novel V600E BRAF mutations in imatinib-naive and imatinib-resistant
gastrointestinal stromal tumors. Genes Chromosomes Cancer. Oct 2008;47(10):853-9. [Medline]. [Full Text].
54. Al-Batran SE, Hartmann JT, Heidel F, et al. Focal progression in patients with gastrointestinal stromal
tumors after initial response to imatinib mesylate: a three-center-based study of 38 patients. Gastric Cancer.
2007;10(3):145-52. [Medline].
55. Alam I, Kheradmand F, Alam S, Jamil A, Wilson I, Hurley M. Laparoscopic management of acutely
presenting gastrointestinal stromal tumors: a study of 9 cases and review of literature. J Laparoendosc Adv
Surg Tech A. Oct 2007;17(5):626-33. [Medline].
56. An JY, Choi MG, Noh JH, et al. Gastric GIST: a single institutional retrospective experience with surgical
treatment for primary disease. Eur J Surg Oncol. Oct 2007;33(8):1030-5. [Medline].
57. Antman K, Crowley J, Balcerzak SP, et al. An intergroup phase III randomized study of doxorubicin and
dacarbazine with or without ifosfamide and mesna in advanced soft tissue and bone sarcomas. J Clin
Oncol. Jul 1993;11(7):1276-85. [Medline].
58. Asakawa M, Sakamoto Y, Kajiwara T, et al. Simple segmental resection of the second portion of the
duodenum for the treatment of gastrointestinal stromal tumors. Langenbecks Arch Surg. Jul
2008;393(4):605-9. [Medline].
59. Badalamenti G, Rodolico V, Fulfaro F, et al. Gastrointestinal stromal tumors (GISTs): focus on
histopathological diagnosis and biomolecular features. Ann Oncol. Jun 2007;18 Suppl 6:vi136-40. [Medline].
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
10 of 12
http://emedicine.medscape.com/article/179669-overview
60. Berthet B, Sugarbaker TA, Chang D, Sugarbaker PH. Quantitative methodologies for selection of patients
with recurrent abdominopelvic sarcoma for treatment. Eur J Cancer. Mar 1999;35(3):413-9. [Medline].
61. Blum MG, Bilimoria KY, Wayne JD, de Hoyos AL, Talamonti MS, Adley B. Surgical considerations for the
management and resection of esophageal gastrointestinal stromal tumors. Ann Thorac Surg. Nov
2007;84(5):1717-23. [Medline].
62. Brodsky SV, Gimenez C, Ghosh C, Melamed M, Ramaswamy G. Estrogen and progesterone receptors
expression in gastrointestinal stromal tumors and intramural gastrointestinal leiomyomas. Int J Gastrointest
Cancer. 2006;37(4):129-32. [Medline].
63. Bmming P, Nilsson O, Ahlman H, et al. Gastrointestinal stromal tumors regularly express synaptic vesicle
proteins: evidence of a neuroendocrine phenotype. Endocr Relat Cancer. Sep 2007;14(3):853-63.
[Medline].
64. Catena F, Di Battista M, Fusaroli P, et al. Laparoscopic treatment of gastric GIST: report of 21 cases and
literature's review. J Gastrointest Surg. Mar 2008;12(3):561-8. [Medline].
65. Chustecka Z. Surgery Is Beneficial Even When GIST Responds to Imatinib. Medscape Medical News.
January 23, 2013. Available at http://www.medscape.com/viewarticle/778033. Accessed February 5, 2013.
66. Corless CL, Heinrich MC. Molecular pathobiology of gastrointestinal stromal sarcomas. Annu Rev Pathol.
2008;3:557-86. [Medline].
67. Desai J, Shankar S, Heinrich MC, et al. Clonal evolution of resistance to imatinib in patients with metastatic
gastrointestinal stromal tumors. Clin Cancer Res. Sep 15 2007;13(18 Pt 1):5398-405. [Medline].
68. Dong C, Jun-Hui C, Xiao-Jun Y, et al. Gastrointestinal stromal tumors of the rectum: Clinical, pathologic,
immunohistochemical characteristics and prognostic analysis. Scand J Gastroenterol. Oct
2007;42(10):1221-9. [Medline].
69. Eilber FC, Rosen G, Forscher C, Nelson SD, Dorey F, Eilber FR. Recurrent gastrointestinal stromal
sarcomas. Surg Oncol. Aug 2000;9(2):71-5. [Medline].
70. Elias A, Ryan L, Sulkes A, Collins J, Aisner J, Antman KH. Response to mesna, doxorubicin, ifosfamide,
and dacarbazine in 108 patients with metastatic or unresectable sarcoma and no prior chemotherapy. J Clin
Oncol. Sep 1989;7(9):1208-16. [Medline].
71. Espinosa I, Lee CH, Kim MK, Rouse BT, Subramanian S, Montgomery K. A novel monoclonal antibody
against DOG1 is a sensitive and specific marker for gastrointestinal stromal tumors. Am J Surg Pathol. Feb
2008;32(2):210-8. [Medline].
72. Fernandez A, Sanguino A, Peng Z, et al. An anticancer C-Kit kinase inhibitor is reengineered to make it
more active and less cardiotoxic. J Clin Invest. Dec 2007;117(12):4044-54. [Medline]. [Full Text].
73. Fontana MG, Rossi E, Bassotti G, et al. Gastrointestinal stromal tumors: usefulness of
immunohistochemistry, flow cytometry and fluorescence in situ hybridization. J Gastroenterol Hepatol. Nov
2007;22(11):1754-9. [Medline].
74. Goettsch WG, Bos SD, Breekveldt-Postma N, Casparie M, Herings RM, Hogendoorn PC. Incidence of
gastrointestinal stromal tumours is underestimated: results of a nation-wide study. Eur J Cancer. Dec
2005;41(18):2868-72. [Medline].
75. Graham J, Debiec-Rychter M, Corless CL, Reid R, Davidson R, White JD. Imatinib in the management of
multiple gastrointestinal stromal tumors associated with a germline KIT K642E mutation. Arch Pathol Lab
Med. Sep 2007;131(9):1393-6. [Medline].
76. Gutierrez JC, De Oliveira LO, Perez EA, Rocha-Lima C, Livingstone AS, Koniaris LG. Optimizing diagnosis,
staging, and management of gastrointestinal stromal tumors. J Am Coll Surg. Sep 2007;205(3):479-91
(Quiz 524). [Medline].
77. Hassan I, You YN, Shyyan R, et al. Surgically managed gastrointestinal stromal tumors: a comparative and
prognostic analysis. Ann Surg Oncol. Jan 2008;15(1):52-9. [Medline].
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
11 of 12
http://emedicine.medscape.com/article/179669-overview
78. Holdsworth CH, Badawi RD, Manola JB, et al. CT and PET: early prognostic indicators of response to
imatinib mesylate in patients with gastrointestinal stromal tumor. AJR Am J Roentgenol. Dec
2007;189(6):W324-30. [Medline].
79. Issakov J, Jiveliouk I, Nachmany I, Klausner J, Merimsky O. A histopathological review of gastrointestinal
related mesenchymal tumors: the hidden GIST. Isr Med Assoc J. Nov 2007;9(11):810-2. [Medline].
80. Janeway KA, Liegl B, Harlow A, et al. Pediatric KIT wild-type and platelet-derived growth factor receptor
alpha-wild-type gastrointestinal stromal tumors share KIT activation but not mechanisms of genetic
progression with adult gastrointestinal stromal tumors. Cancer Res. Oct 1 2007;67(19):9084-8. [Medline].
81. Jeon SW, Park YD, Chung YJ, et al. Gastrointestinal stromal tumors of the stomach: endosonographic
differentiation in relation to histological risk. J Gastroenterol Hepatol. Dec 2007;22(12):2069-75. [Medline].
82. Kee D, Zalcberg JR. Current and emerging strategies for the management of imatinib-refractory advanced
gastrointestinal stromal tumors. Ther Adv Med Oncol. Sep 2012;4(5):255-70. [Medline]. [Full Text].
83. Kim KM, Kang DW, Moon WS, Park JB, Park CK, Sohn JH. PKCtheta expression in gastrointestinal stromal
tumor. Mod Pathol. Nov 2006;19(11):1480-6. [Medline].
84. Kobayashi K, Szklaruk J, Trent JC, et al. Hepatic arterial embolization and chemoembolization for imatinibresistant gastrointestinal stromal tumors. Am J Clin Oncol. Dec 2009;32(6):574-81. [Medline].
85. McAuliffe JC, Lazar AJ, Yang D, et al. Association of intratumoral vascular endothelial growth factor
expression and clinical outcome for patients with gastrointestinal stromal tumors treated with imatinib
mesylate. Clin Cancer Res. Nov 15 2007;13(22 Pt 1):6727-34. [Medline].
86. McWhinney SR, Pasini B, Stratakis CA. Familial gastrointestinal stromal tumors and germ-line mutations. N
Engl J Med. Sep 6 2007;357(10):1054-6. [Medline].
87. Meara RS, Cangiarella J, Simsir A, Horton D, Eltoum I, Chhieng DC. Prediction of aggressiveness of
gastrointestinal stromal tumours based on immunostaining with bcl-2, Ki-67 and p53. Cytopathology. Oct
2007;18(5):283-9. [Medline].
88. Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin
Diagn Pathol. May 2006;23(2):70-83. [Medline].
89. Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology,
prognosis, and differential diagnosis. Arch Pathol Lab Med. Oct 2006;130(10):1466-78. [Medline].
90. Nakajima K, Yasumasa K, Endo S, et al. A versatile dual-channel carbon dioxide (CO2) insufflator for
various CO2)applications. The prototype. Surg Endosc. Feb 2006;20(2):334-8. [Medline].
91. Nilsson B, Sjolund K, Kindblom LG, et al. Adjuvant imatinib treatment improves recurrence-free survival in
patients with high-risk gastrointestinal stromal tumours (GIST). Br J Cancer. Jun 4 2007;96(11):1656-8.
[Medline]. [Full Text].
92. Nishimura J, Nakajima K, Omori T, et al. Surgical strategy for gastric gastrointestinal stromal tumors:
laparoscopic vs. open resection. Surg Endosc. Jun 2007;21(6):875-8. [Medline].
93. Rubio J, Marcos-Gragera R, Ortiz MR, et al. Population-based incidenceand survival of gastrointestinal
stromal tumors (GIST) in Girona, Spain. Eur J Cancer. 2007;43:144-148.
94. Rutkowski P, Debiec-Rychter M, Nowecki ZI, et al. Different factors are responsible for predicting relapses
after primary tumors resection and for imatinib treatment outcomes in gastrointestinal stromal tumors. Med
Sci Monit. Nov 2007;13(11):CR515-522. [Medline].
95. Sepe PS, Brugge WR. A guide for the diagnosis and management of gastrointestinal stromal cell tumors.
Nat Rev Gastroenterol Hepatol. Jun 2009;6(6):363-71. [Medline].
96. Sevinc A, Camci C, Yilmaz M, Buyukhatipoglu H. The diagnosis of C-kit negative GIST by PDGFRA
staining: clinical, pathological, and nuclear medicine perspective. Onkologie. Dec 2007;30(12):645-8.
[Medline].
28-May-14 2:30 AM
Gastrointestinal Stromal Tumors
12 of 12
http://emedicine.medscape.com/article/179669-overview
97. Steigen SE, Straume B, Turbin D, et al. Clinicopathologic factors and nuclear morphometry as independent
prognosticators in KIT-positive gastrointestinal stromal tumors. J Histochem Cytochem. Feb
2008;56(2):139-45. [Medline]. [Full Text].
98. Takahashi T, Nakajima K, Nishitani A, et al. An enhanced risk-group stratification system for more practical
prognostication of clinically malignant gastrointestinal stromal tumors. Int J Clin Oncol. Oct
2007;12(5):369-74. [Medline].
99. Trent JC, Lazar AJ, Zhang W. Molecular approaches to resolve diagnostic dilemmas: the case of
gastrointestinal stromal tumor and leiomyosarcoma. Future Oncol. Dec 2007;3(6):629-37. [Medline].
100. Tryggvason G, Gislason HG, Magnusson MK, Jonasson JG. Gastrointestinal stromal tumors in Iceland,
1990-2003: the icelandic GIST study, a population-based incidence and pathologic risk stratification study.
Int J Cancer. Nov 1 2005;117(2):289-93. [Medline].
101. Tsukuda K, Hirai R, Miyake T, et al. The outcome of gastrointestinal stromal tumors (GISTs) after a surgical
resection in our institute. Surg Today. 2007;37(11):953-7. [Medline].
Medscape Reference 2011 WebMD, LLC
28-May-14 2:30 AM
Das könnte Ihnen auch gefallen
- Signs and Symptoms: RadiologyDokument8 SeitenSigns and Symptoms: RadiologyEman AyyadNoch keine Bewertungen
- Clinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateDokument31 SeitenClinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateCileni NuñezNoch keine Bewertungen
- Gastrointestinal Stromal Tumors (Gists) : Surgical Management Update 2009Dokument40 SeitenGastrointestinal Stromal Tumors (Gists) : Surgical Management Update 2009Rendy FitraNoch keine Bewertungen
- Gastrointestinal Stromal Tumor FirdausDokument8 SeitenGastrointestinal Stromal Tumor FirdausFarizka FirdausNoch keine Bewertungen
- Dr. Ranjan GuptaDokument29 SeitenDr. Ranjan GuptaRanjan GuptaNoch keine Bewertungen
- Clinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateDokument41 SeitenClinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateTatiana CumbicosNoch keine Bewertungen
- CRC Signs, Stages, TreatmentsDokument4 SeitenCRC Signs, Stages, TreatmentsSugar ZeñatnomNoch keine Bewertungen
- cLINICAL PRACTICE GUIDELINESDokument7 SeitencLINICAL PRACTICE GUIDELINESdrmolinammNoch keine Bewertungen
- UK GIST Guidelines2017Dokument10 SeitenUK GIST Guidelines2017Ramez AntakiaNoch keine Bewertungen
- UK Clinical Practice Guidelines For The Management of Gastrointestinal Stromal Tumours (GIST)Dokument10 SeitenUK Clinical Practice Guidelines For The Management of Gastrointestinal Stromal Tumours (GIST)emmyNoch keine Bewertungen
- Gallbladder CancerDokument5 SeitenGallbladder CancerandyjayaNoch keine Bewertungen
- Gist Clinical DiagnosisDokument41 SeitenGist Clinical DiagnosisTjendonohariantoNoch keine Bewertungen
- CCDuodenum Periampullary Neoplasms ChuDokument68 SeitenCCDuodenum Periampullary Neoplasms ChuSahirNoch keine Bewertungen
- Stomach CancerDokument7 SeitenStomach CancerSyazmin KhairuddinNoch keine Bewertungen
- Tumor GIT - Dr. Fanny 2020Dokument51 SeitenTumor GIT - Dr. Fanny 2020kintan 102017153Noch keine Bewertungen
- Surgical Management of GISTomasDokument13 SeitenSurgical Management of GISTomasCesar RcNoch keine Bewertungen
- Urogenital CancersDokument2 SeitenUrogenital CancerssdfNoch keine Bewertungen
- GIST4Dokument9 SeitenGIST4vickyarmasrudNoch keine Bewertungen
- Clinical Practice GuidelinesDokument7 SeitenClinical Practice GuidelinesMada IacobNoch keine Bewertungen
- Benign Liver LesionsDokument30 SeitenBenign Liver LesionstheintrovNoch keine Bewertungen
- Bladder NCCNDokument17 SeitenBladder NCCNJoriza TamayoNoch keine Bewertungen
- Small Renal Mass: Clinical PracticeDokument11 SeitenSmall Renal Mass: Clinical PracticeHarlina NurlitaNoch keine Bewertungen
- Gastric CancerDokument4 SeitenGastric Cancerphvega06Noch keine Bewertungen
- Gastric Cancer2Dokument24 SeitenGastric Cancer2intanpermatasari8Noch keine Bewertungen
- Colon CancerDokument14 SeitenColon Cancerrosalinda100% (1)
- Gastric CancerDokument7 SeitenGastric CancerMicah PingawanNoch keine Bewertungen
- GastriccancerDokument65 SeitenGastriccancerSHIVAJINoch keine Bewertungen
- Small BowelDokument28 SeitenSmall BowelpopNoch keine Bewertungen
- Collision TumourDokument5 SeitenCollision Tumoursiripuram naveen kumarNoch keine Bewertungen
- Primary Peritoneal Mesothelioma Case Series and Literature ReviewDokument7 SeitenPrimary Peritoneal Mesothelioma Case Series and Literature ReviewfvhgssfmNoch keine Bewertungen
- 009 - The-Perioperative-and-Operative-Management-of - 2023 - Surgical-Oncology-ClinicsDokument17 Seiten009 - The-Perioperative-and-Operative-Management-of - 2023 - Surgical-Oncology-ClinicsDr-Mohammad Ali-Fayiz Al TamimiNoch keine Bewertungen
- Gastro Intestinal Stromal Tumor (GIST)Dokument28 SeitenGastro Intestinal Stromal Tumor (GIST)Nazila HanaNoch keine Bewertungen
- Small Bowel CancerDokument16 SeitenSmall Bowel CancerFauzie MegantaraNoch keine Bewertungen
- Css CT Scan AbdomenDokument54 SeitenCss CT Scan AbdomenUlfa DiyaNoch keine Bewertungen
- Gastric Cancer NewDokument10 SeitenGastric Cancer NewArnicca Obligacion-BustamanteNoch keine Bewertungen
- Gastric Tumors (Notes)Dokument23 SeitenGastric Tumors (Notes)Priyanka GosaiNoch keine Bewertungen
- Esophageal Tumors: Diagnosis and Treatment OptionsDokument36 SeitenEsophageal Tumors: Diagnosis and Treatment OptionsbahtiarhabibiNoch keine Bewertungen
- Casestudy Gastric CarcinomaDokument53 SeitenCasestudy Gastric CarcinomaAngelaTrinidadNoch keine Bewertungen
- ESMO Testicular CancerDokument8 SeitenESMO Testicular CancerBernadetta ViaNoch keine Bewertungen
- Overview of The Management of Primary Colon Cancer - UpToDateDokument30 SeitenOverview of The Management of Primary Colon Cancer - UpToDateCaio AmaralNoch keine Bewertungen
- 04 Esophageal TumorsDokument36 Seiten04 Esophageal TumorsDetty NoviantyNoch keine Bewertungen
- tgh-03-2018 01 07Dokument11 Seitentgh-03-2018 01 07kiranNoch keine Bewertungen
- 172 - 04 101 13 PDFDokument8 Seiten172 - 04 101 13 PDFAlexandrosNoch keine Bewertungen
- Rectal Carcinoma Imaging: More..Dokument13 SeitenRectal Carcinoma Imaging: More..Priyanka Neeraj AroraNoch keine Bewertungen
- 直肠类癌临床病理分析_李征Dokument3 Seiten直肠类癌临床病理分析_李征kuangzhu820Noch keine Bewertungen
- Gastric Cancer by BalaDokument17 SeitenGastric Cancer by BalaArundeep AsaithambiNoch keine Bewertungen
- Colorectal CancerDokument7 SeitenColorectal Cancerjames garciaNoch keine Bewertungen
- Journal Reading SurgeryDokument21 SeitenJournal Reading Surgerydr.liraNoch keine Bewertungen
- Glimelius 2013Dokument8 SeitenGlimelius 2013Sofia SimpertigueNoch keine Bewertungen
- Managementofgastric Adenocarcinomaforgeneral Surgeons: Hisakazu HoshiDokument12 SeitenManagementofgastric Adenocarcinomaforgeneral Surgeons: Hisakazu HoshiNelson William UsnayoNoch keine Bewertungen
- بحث 8Dokument4 Seitenبحث 8Ossama Abd Al-amierNoch keine Bewertungen
- Casestudy Gastric CarcinomaDokument56 SeitenCasestudy Gastric CarcinomaMJ Amarillo92% (12)
- Surgical Management of Solid Tumor-4674Dokument7 SeitenSurgical Management of Solid Tumor-4674Theofhila AldelaNoch keine Bewertungen
- Kista LiverDokument16 SeitenKista LiverInomy ClaudiaNoch keine Bewertungen
- Current Diagnosis and Management of Retroperitoneal SarcomaDokument11 SeitenCurrent Diagnosis and Management of Retroperitoneal SarcomaMaximiliano TorresNoch keine Bewertungen
- Clinical Practice Guidelines: Gastric Cancer: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDokument12 SeitenClinical Practice Guidelines: Gastric Cancer: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpRachelle CorralNoch keine Bewertungen
- CPP PPPPPP PPPPPPPDokument4 SeitenCPP PPPPPP PPPPPPPJen Gacula OsinNoch keine Bewertungen
- Management of Urologic Cancer: Focal Therapy and Tissue PreservationVon EverandManagement of Urologic Cancer: Focal Therapy and Tissue PreservationNoch keine Bewertungen
- Cathepsin B Inhibitors For Targeted Cancer Therapy 1948 5956.1000302Dokument5 SeitenCathepsin B Inhibitors For Targeted Cancer Therapy 1948 5956.1000302polygoneNoch keine Bewertungen
- Fetal EchocardiographyDokument3 SeitenFetal EchocardiographypolygoneNoch keine Bewertungen
- Brief Coagulation CascadeDokument1 SeiteBrief Coagulation CascadepolygoneNoch keine Bewertungen
- Paracervical Block For Pain Control in First Trimester AbortionDokument8 SeitenParacervical Block For Pain Control in First Trimester AbortionpolygoneNoch keine Bewertungen
- Usg Normal PDFDokument14 SeitenUsg Normal PDFTia Amalia Puti RenaeryNoch keine Bewertungen
- Coagulation CascadeDokument1 SeiteCoagulation CascadepolygoneNoch keine Bewertungen
- Changes in Connective Tissue in Pelvic Organ ProlapseDokument14 SeitenChanges in Connective Tissue in Pelvic Organ ProlapsepolygoneNoch keine Bewertungen
- Assesing 1st Stage of Labor Progression and Its Relation To ComplicationDokument8 SeitenAssesing 1st Stage of Labor Progression and Its Relation To ComplicationpolygoneNoch keine Bewertungen
- Paracervical block technique and complicationsDokument4 SeitenParacervical block technique and complicationspolygoneNoch keine Bewertungen
- ICD X Kematian MaternalDokument3 SeitenICD X Kematian MaternalpolygoneNoch keine Bewertungen
- Secondary Amenorrhea Testing AlgorithmDokument1 SeiteSecondary Amenorrhea Testing AlgorithmpolygoneNoch keine Bewertungen
- Puerperal FeverDokument19 SeitenPuerperal FeverJosh Matthew RosalesNoch keine Bewertungen
- Diagnosis and Management of Adult Female Stress Urinary Incontinence 2010Dokument6 SeitenDiagnosis and Management of Adult Female Stress Urinary Incontinence 2010polygoneNoch keine Bewertungen
- The Physiological Mechanism of Uterine Contraction With Emphasis On Calcium IonDokument6 SeitenThe Physiological Mechanism of Uterine Contraction With Emphasis On Calcium IonpolygoneNoch keine Bewertungen
- Z9 D6 Q MG SH Hor V41 L SW1 Syerv RDokument20 SeitenZ9 D6 Q MG SH Hor V41 L SW1 Syerv RpolygoneNoch keine Bewertungen
- Triple P Procedure Cohort StudyDokument18 SeitenTriple P Procedure Cohort StudypolygoneNoch keine Bewertungen
- BallardScore ScoresheetDokument1 SeiteBallardScore ScoresheetIsabel BarradasNoch keine Bewertungen
- Pi Is 0020729214005359Dokument3 SeitenPi Is 0020729214005359polygoneNoch keine Bewertungen
- Adult Dehydration Guideline July 2015Dokument3 SeitenAdult Dehydration Guideline July 2015polygoneNoch keine Bewertungen
- ESHRE IVF Labs Guideline 15122015 FINALDokument30 SeitenESHRE IVF Labs Guideline 15122015 FINALpolygone100% (1)
- StruttinDokument5 SeitenStruttinpolygoneNoch keine Bewertungen
- Pap Test Specimen Collection InstructionsDokument9 SeitenPap Test Specimen Collection InstructionspolygoneNoch keine Bewertungen
- Frequency and Efect of 21 OH Gene Defect in CAH PatientsDokument11 SeitenFrequency and Efect of 21 OH Gene Defect in CAH PatientspolygoneNoch keine Bewertungen
- Increased Psychiatric Morbidity in Men With 21 OH DeficiencyDokument7 SeitenIncreased Psychiatric Morbidity in Men With 21 OH DeficiencypolygoneNoch keine Bewertungen
- Mortality Rate of GTN With FIGO Score More Than 13Dokument8 SeitenMortality Rate of GTN With FIGO Score More Than 13polygoneNoch keine Bewertungen
- Undergrad Obsgyn Medical Education: Why Are We Underrated and UnderappreciatedDokument3 SeitenUndergrad Obsgyn Medical Education: Why Are We Underrated and UnderappreciatedpolygoneNoch keine Bewertungen
- Guideline For Management of A Patient Undergoing HysterosDokument4 SeitenGuideline For Management of A Patient Undergoing HysterospolygoneNoch keine Bewertungen
- Maternal Early Warning Tool Reduces MorbidityDokument6 SeitenMaternal Early Warning Tool Reduces MorbiditypolygoneNoch keine Bewertungen
- An Update On Massive Tranfusion Protocol in ObstetricDokument5 SeitenAn Update On Massive Tranfusion Protocol in ObstetricpolygoneNoch keine Bewertungen
- To Read 1Dokument13 SeitenTo Read 1D BNoch keine Bewertungen
- Lung Cancer MCQsDokument23 SeitenLung Cancer MCQsskNoch keine Bewertungen
- ACG Clinical Guideline Diagnosis and Management.16Dokument13 SeitenACG Clinical Guideline Diagnosis and Management.16Alejandro OliveraNoch keine Bewertungen
- Fine Needle Aspiration Cytology (FNAC) of GISTDokument7 SeitenFine Needle Aspiration Cytology (FNAC) of GISTurfriendanshul100% (1)
- Human Pathology: Case Reports: Kankanamage Malinda Amesh Karasinghe, Kesavan SittampalamDokument5 SeitenHuman Pathology: Case Reports: Kankanamage Malinda Amesh Karasinghe, Kesavan SittampalammalindaNoch keine Bewertungen
- Stomach QuestionsDokument4 SeitenStomach QuestionsNica Lopez FernandezNoch keine Bewertungen
- 1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementDokument10 Seiten1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementLeo Mari Go LimNoch keine Bewertungen
- Surgery LMRP 2019Dokument65 SeitenSurgery LMRP 2019skNoch keine Bewertungen
- Stomach and Duodenal Ulcer Classification and TreatmentDokument79 SeitenStomach and Duodenal Ulcer Classification and Treatmentadversal8avrikNoch keine Bewertungen
- Pathology Checklist DR Preeti SharmaDokument5 SeitenPathology Checklist DR Preeti SharmaAvi Khanna100% (1)
- SFA 2011 Annual ReportDokument15 SeitenSFA 2011 Annual ReportSarcoma Foundation of AmericaNoch keine Bewertungen
- Gastrointestinal Stromal Tumor Early Detection, Diagnosis, and StagingDokument22 SeitenGastrointestinal Stromal Tumor Early Detection, Diagnosis, and StagingDekdesNoch keine Bewertungen
- Summary of Patient Database RecordDokument21 SeitenSummary of Patient Database RecordIka AyuNoch keine Bewertungen
- PUD Tan Study GuideDokument33 SeitenPUD Tan Study GuideErald PaderangaNoch keine Bewertungen
- Diagnosis and Treatment of Gastrointestinal CancersDokument230 SeitenDiagnosis and Treatment of Gastrointestinal CancersSoyPedroNoch keine Bewertungen
- Healthmedicinet Com II 2014 JanDokument326 SeitenHealthmedicinet Com II 2014 JanHeal ThmedicinetNoch keine Bewertungen
- Gastric Mucosa Protection MechanismsDokument45 SeitenGastric Mucosa Protection MechanismsNicole IoanidNoch keine Bewertungen
- 00 GIT NotesDokument81 Seiten00 GIT NotesHythem Hashim100% (1)
- Histologic findings in mandibular mass reveal ameloblastomaDokument65 SeitenHistologic findings in mandibular mass reveal ameloblastomaWilliam Tan CebrianNoch keine Bewertungen
- (23006676 - Current Issues in Pharmacy and Medical Sciences) Gastric LipomatosisDokument3 Seiten(23006676 - Current Issues in Pharmacy and Medical Sciences) Gastric LipomatosisPockets Ain't EmptyNoch keine Bewertungen
- Tumor of Small IntestineDokument27 SeitenTumor of Small IntestinePRUTHVI RAJ P SNoch keine Bewertungen
- Tumours and Inflammatory Lesions of The Anal Dawson2015Dokument12 SeitenTumours and Inflammatory Lesions of The Anal Dawson2015DannyNoch keine Bewertungen
- Common Gastrointestinal MalignanciesDokument56 SeitenCommon Gastrointestinal MalignanciesEC BaldzNoch keine Bewertungen
- ASC Abstracts 05Dokument110 SeitenASC Abstracts 0512345qwertasdfgzxcvbNoch keine Bewertungen
- Gastrointestinal Stromal TumoursDokument22 SeitenGastrointestinal Stromal TumoursThomas KlebNoch keine Bewertungen
- Causes of Upper Gastrointestinal Bleeding in Adults - UpToDateDokument37 SeitenCauses of Upper Gastrointestinal Bleeding in Adults - UpToDateAline MoraisNoch keine Bewertungen
- VvvvaaaaDokument6 SeitenVvvvaaaakoxNoch keine Bewertungen
- Brosuri Chimioterapie Update 2020 673 PDFDokument282 SeitenBrosuri Chimioterapie Update 2020 673 PDFAnna Dumitrache67% (3)
- Most Comon Questions Asked in NEET PG and DNBDokument12 SeitenMost Comon Questions Asked in NEET PG and DNBSubhajitPaul100% (2)
- KIT and PDGFRA Mutations in GISTs Guide TreatmentDokument22 SeitenKIT and PDGFRA Mutations in GISTs Guide TreatmentCarla CarolineNoch keine Bewertungen