Beruflich Dokumente
Kultur Dokumente
Filariasis
Hochgeladen von
paulinus sayoriCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Filariasis
Hochgeladen von
paulinus sayoriCopyright:
Verfügbare Formate
Filarial Nematodes
John H. Cross
General Concepts
Lymphatic Filariae
Clinical Manifestations
Disease manifestations include inflammation of lymph nodes
(lymphadenitis), irregular fevers, and lymphedema. Repeated,
chronic infection may result in elephantiasis.
Structure
Adults are elongate and threadlike. Microfilariae are 250 to 300 m
long, equal in diameter to a red blood cell, and sheathed.
Classification
Filariae are nematodes (roundworms). They are vectored by
arthropods; mature and mate in specific host tissues; and produce
microfilariae. The lymphatic filariae Wuchereria bancrofti and Brugia
malayi reside in lymphatics.
Multiplication and Life Cycle
Adult female worms produce microfilariae. Feeding vector
mosquitoes ingest microfilariae from the bloodstream. In the
mosquito the microfilariae mature to infective larvae, which migrate
to the mosquito's mouth-parts, enter a new host via the vector's
puncture wound, migrate to the lymphatics, mature, and mate.
Pathogenesis
Disease manifestations are due to lymphatic dysfunction resulting
from the presence of living and dead worms, lymph thrombi,
inflammation, and immune reactions to worms and worm products.
Host Defenses
Inflammatory reactions result in cellular infiltration and fibrosis of
lymphatics. Damage to vessel walls result in endothelial cell
proliferation. It is not yet clear to what extent circulating antibodies
to filariae are protective.
Epidemiology
Lymphatic filariasis is prevalent in many tropical and subtropical
countries where the vector mosquitoes are common.
Diagnosis
Diagnosis is suggested clinically by lymphangitis and irregular fever;
definitive diagnosis depends on demonstrating microfilariae in thick
blood smears.
Control
There is no consistently effective treatment to kill adult worms.
Control is by avoiding or reducing vector mosquitoes and by treating
individuals with microfilariacides.
Onchocerca Volvulus
Clinical Manifestations
Patients present with subcutaneous nodules, dermatitis, and eye
lesions.
Structure
Long, thread-like adult worms live coiled in subcutaneous nodules
and produce microfilariae that are slightly smaller than those of
lymphatic filariae and are not sheathed.
Classification
Onchocerca volvulus is a typical filarial nematode that is primarily a
parasite of humans.
Multiplication and Life Cycle
Adult worms live in subcutaneous nodules. Microfilariae wander
through the skin, where they may be picked up by a feeding vector
blackfly. In the blackfly they mature to infective larvae, which may
enter a new host when the blackfly feeds. The larvae then move to
the subcutaneous tissues, mature, mate, and produce microfilariae.
Pathogenesis
Reaction to worms and microfilariae causes dermatitis with loss of
skin elasticity and the formation of fibrotic subcutaneous nodules.
Living and dead microfilariae in the eye cause trauma and reactions
that can result in blindness.
Host Defenses
There is an inflammatory and immune response to living and dead
parasites and to antigen-antibody complexes. Adult worms are
localized in the subcutaneous tissues, surrounded by fibrotic
nodules and ultimately calcify.
Epidemiology
Onchocerciasis is common in Africa; foci also occur in South and
Central America and Mexico. The blackfly vectors breed in oxygenrich water; thus, the disease characteristically is associated with
fast-flowing streams.
Diagnosis
The clinical picture is indicative; final diagnosis is made by
identifying microfilariae in skin snips.
Control
Individuals may be treated by removal of nodules and by
administering microfilariacides that kill microfilariae. Control of
vector blackflies minimizes reinfection.
Minor Filariae
Several other minor filarial nematodes parasitize humans; the
pathology depends on the tissues preferred by the worms. In
addition, humans occasionally are infected with dog heartworm
larvae, which are unable to mature in human tissues but can cause
lesions.
INTRODUCTION
The filariae are thread-like parasitic nematodes (roundworms) that
are transmitted by arthropod vectors. The adult worms inhabit
specific tissues where they mate and produce microfilariae, the
characteristic tiny, thread-like larvae. The microfilariae infect vector
arthropods, in which they mature to infective larvae. Filarial
diseases are a major health problem in many tropical and
subtropical areas. The disease produced by a filarial worm depends
on the tissue locations preferred by adults and microfilariae. The
adults of the lymphatic filariae inhabit lymph vessels, where
blockage and host reaction can result in lymphatic inflammation and
dysfunction, and eventually in lymphedema and fibrosis. Repeated,
prolonged infection with these worms can lead to elephantiasis, a
buildup of excess tissue in the affected area. Other filariae mature in
the skin and subcutaneous tissues, where they induce nodule
formation and dermatitis; migrating filariae of these species can
cause ocular damage. Table 92-1 summarizes the filarial infections
of humans.
Lymphatic Filariae Wuchereria Bancrofti and Brugia Malayi
Clinical Manifestations
In lymphatic filariasis, disease is caused by the presence of worms
in the regional lymphatic vessels and, particularly, by the host
response to the worms and worm products. The microfilariae are
released into the blood. Infections involving small numbers of worms
are often asymptomatic. Early symptoms of lymphatic filariasis
4
consist of intermittent fever and enlarged, tender lymph nodes. The
inguinal lymph nodes are very often involved. The lymphatic vessels
that drain into the lymph nodes and that harbor the developing and
adult worms also become inflamed and painful. In more chronic
infections, there may be pain also in the epididymis and testes.
Swollen lymphatics may burst and drain into the genitourinary
system; the resulting chyluria is sometimes the symptom that brings
the patient to a doctor.
In a small number of chronic cases, permanent lymphatic
dysfunction caused by repeated exposure to infection over a
number of years results in the massive lymphedema and
accumulation of excess tissue known as elephantiasis.
Structure and Classification
Adult Wuchereria and Brugia are elongated and slender (30 to 100
mm by 100 to 300 m); males are about half the size of females.
Microfilariae are the diameter of a red blood cell and 250 to 300 m
long. They are enclosed in a characteristic sheath. In addition to B
malayi, some other, related Brugia species can infect humans or
animals; they resemble B malayi in structure and life cycle, and are
not discussed here. B timori, found only in Indonesia, is similar to B
malayi, but is larger.
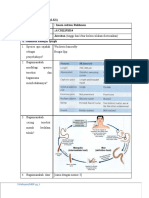
Multiplication and Life Cycle
The filariae require an intermediate arthropod host to complete their
life cycle (Fig. 92-1). However, no multiplication takes place in the
intermediate host. Adult male and female worms live in regional
lymphatic vessels, where the female produces a large number of
microfilariae, which circulate in the blood and may be ingested by a
feeding vector mosquito. The female worms show a circadian
periodicity in microfilaria production. The time of peak production
varies among the species and geographic strains of worms and
usually corresponds to the peak feeding period of the vector
mosquitoes. Microfilariae ingested by a vector mosquito migrate out
of the midgut to the thoracic muscles, where they develop, molt
several times, and finally migrate to the mouthparts of the mosquito
as infective larvae. As the infective mosquito feeds on another host,
the larvae leave the proboscis and enter the puncture wound made
by the mosquito. Larvae quickly migrate to the lymphatics, where
they mature, mate, and produce microfilariae in the new host. The
time from infection until microfilariae can be detected in the blood
varies from 3 to many months. There is no reliable information on
the average life span of adult worms; however, humans who leave
endemic areas have been observed to have circulating microfilariae
for several years.
FIGURE 92-1 Life cycle of Wuchereria and Brugia
Pathogenesis
Infective larvae from a feeding vector mosquito migrate to the
regional lymphatic vessels and by inducing a host inflammatory
reaction cause the eventual blockage and edema characteristic of W
bancrofti and B malayi infections (Fig. 92-1). The pathology varies
greatly from one individual to another, and the exact mechanisms
are not completely understood. The host reaction to the parasite is
considerable and worsens when the worms molt, when the females
first begin to produce microfilariae, and when the worms die and
degenerate. Lymphatic vessels are often partially or completely
blocked by lymph thrombi, by masses of dead worms, or by
endothelial proliferation, fibrin deposition, and granulomatous
reactions. Lymph stasis favors secondary bacterial and mycotic
infection. The initial inflammation of regional lymph nodes and
major lymphatic vessels may be followed by a prolonged
asymptomatic period and then by recurring attacks of lymphangitis
and "filarial fever" over a period of years. Figure 92-2 shows an
example of elephantiasis, a grotesque enlargement of the infected
area that develops when recurring attacks of lymphangitis result in
permanent lymphatic blockage and lymphedema. The exact cause
of elephantiasis is not understood; however, repeated exposure
appears to lead to production of abnormally large amounts of
collagenous material and to fibrosis of the tissue around the
affected lymphatics.
FIGURE 92-2 Elephantiasis of leg caused by chronic infection
with the filarial nematode Wuchereria bancrofti. (Courtesy of
Shoyei Yamauchi, Honolulu, HI.)
Host Defenses
The reaction to developing and adult worms results in endothelial
cell proliferation and thrombus formation within the lymphatic
vessels. Some aspects of the wide disease spectrum seen in
lymphatic filariasis can be correlated with host immune responses.
Individuals living in endemic areas and frequently bitten by infective
mosquito vectors vary in clinical manifestations. Patients with
characteristic symptoms such as recurring fever and regional
lymphangitis may or may not have microfilariae in peripheral blood.
Although antibodies to microfilariae and adult worms may be
present, they do not seem to prevent reinfection or disease, since in
endemic areas the proportion of exposed individuals who have
microfilariae or clinical symptoms may increase until middle age. As
a general rule, adults not previously infected with lymphatic filariae
will show symptoms, but not circulating microfilariae, following
infection with large numbers of infective larvae. Patients with
elephantiasis also usually do not have circulating microfilariae. They
do, however, have high levels of antibody to microfilariae and
increased lymphocyte proliferative responses to adult worm
antigens.
Epidemiology
Wuchereria bancrofti is prevalent in many parts of the tropics and
subtropics. Species from three major genera of mosquitoes that
serve as vectors are the common house mosquito Culex pipiens
quinquefasciatus (C fatigans) in many urban centers, Aedes species
in the South Pacific islands, and Anopheles species in more isolated
rural areas. The relation between the degree and frequency of
infection and the development of the disease is still not fully
understood; severe disease such as elephantiasis develops
gradually as a result of repeated exposure. Circulating microfilariae
may persist for many years in the absence of specific symptoms.
Humans previously were assumed to be the only hosts for W
bancrofti; however, studies have shown that several species of
monkeys can be infected experimentally with infective stage W
bancrofti larvae recovered from mosquitoes allowed to feed on
infected human volunteers. No naturally infected reservoirs other
than humans have been identified.
Brugia malayi differs somewhat from W bancrofti in epidemiology.
Whereas W bancrofti is prevalent in tropical areas all over the world,
B malayi is found mainly in Southeast Asia. In contrast to W
bancrofti, which is transmitted by mosquitoes of the three major
genera, the principal mosquito vectors of B malayi belong to the
genus Mansonia. B malayi is less host-specific than W bancrofti; it
has been recovered from naturally infected monkeys, cats, and
dogs, and has been maintained in several laboratory animals.
Diagnosis
Enlarged and tender lymph nodes, especially in the inguinal region,
or inflammation of lymphatic vessels in the extremities should alert
physicians in an endemic area to filariasis. Definitive diagnosis may
be accomplished by identifying microfilariae in thick blood smears
(Fig. 92-1). Species identification is based on the presence of a
sheath and the position of terminal nuclei and the size of the
cephalic space. Because of the nocturnal periodicity of microfilariae,
blood smears are better made at night when microfilarial levels are
usually higher. Light infections may be detected by using one of
several concentration methods.
Unfortunately, microfilariae may not be present in the blood during
the early and late stages of the disease. When microfilariae are not
detectable, a history of recurrent episodes of lymphangitis and
lymphadenitis may form the basis for a presumptive diagnosis. Skin
tests have been largely unsatisfactory, and commercial antigen is
not widely available. Serologic tests are useful in epidemiologic
studies, but to date have had limited value in the management of
individual cases. Molecular cloning of antigens and antigen capture
techniques are showing promise. New developments in
ultrasonography and lymphoangioscintigraphy may also contribute
to diagnosis.
Control
Attempts to reduce the prevalence of lymphatic filariae include
vector control and mass treatment campaigns using
diethylcarbamazine citrate. Some mass treatment programs have
used table salt medicated with diethylcarbamazine. This drug
significantly reduces the level of microfilariae in the blood. However,
it must be given over a prolonged period, and frequent side effects,
such as fever, vertigo, headaches, nausea, and lymphatic
inflammation, discourage patient cooperation. Ivermectin, a drug
that has recently been shown to be effective in the treatment of
onchocerciasis, is being evaluated for use in lymphatic filariasis.
Neither drug is very effective at killing adult worms. Combinations of
diethylcarbamazine and ivermectin are being tested. In some areas
single doses of these drugs in combination or singly are also being
evaluated. Fewer side effects are experienced with the shorter
treatments.
Onchocerca Volvulus
Onchocerca volvulus is a filarial worm that is transmitted to humans
by blackflies (Simulium). Mature worms live in the subcutaneous
tissues and produce microfilariae that migrate through the skin and
connective tissues.
Clinical Manifestations
Changes in skin pigmentation are often the first obvious signs of
Onchocerca infection. Later stages of dermatitis present as atrophy
and loss of skin elasticity. Although lymph nodes may become
involved in onchocerciasis, involvement is not as prominent as with
the lymphatic filariae. The subcutaneous nodules that harbor adult
Onchocerca are usually firm and non-tender. They vary in size and
location but usually are easily recognized when they occur in
geographic areas where the disease is endemic. However, in some
geographic regions, nodules may be in deeper tissue, and thus not
easily palpable.
The most serious clinical manifestation of onchocerciasis is
blindness, caused by microfilariae that wander into the eye. In
endemic areas, corneal opacities resulting from the reaction to
dying microfilariae often suggest onchocercal infection.
Alternatively, active living microfilariae may be seen when the eye is
examined with a slit lamp.
Structure
Adult Onchocerca may be up to 60 cm long, but are usually coiled in
subcutaneous nodules. The microfilariae are slightly smaller than
those of W bancrofti and B malayi and differ from them in lacking a
sheath, having a different nuclear arrangement, and not usually
being found in the blood.
Multiplication and Life Cycle
Figure 92-3 shows the life cycle of Onchocerca. The microfilariae
produced by adult female worms in subcutaneous nodules migrate
into the skin and connective tissue; they do not generally enter the
circulatory system. Microfilariae are ingested by vector blackflies,
develop to the infective stage in the muscles of the flies, and then
migrate to the mouth parts. When the infected flies feed on a new
host, the larvae leave the mouth parts and enter the wound
produced by the biting fly. Developing male and female worms
congregate in subcutaneous tissue where they usually induce
formation of a nodule.
10
FIGURE 92-3 Life cycle of Onchocerca.
Pathogenesis
Adult worms in the subcutaneous tissues cause varying degrees of
inflammation and may induce subcutaneous nodules. Nodules
appear 3 to 4 months after infection, but microfilariae are not
generally detectable until I year after infection. Adult worms may be
surrounded by an inflammatory response that progresses to
granuloma formation and fibrosis or calcification, depending on the
condition of the worm and age of the nodule (Fig. 92-3).
Microfilariae appear to move upward, and in chronic heavy
infections may be seen in the eye. Ocular damage is thought to be
due both to the trauma caused by living microfilariae and to a
hypersensitivity reaction to dead ones. A major problem in the
management of onchocerciasis patients is the acute inflammatory
response to dying microfilariae in the eye during treatment. Antigenantibody complexes probably play a role in the development of eye
lesions resulting from microfilariae.
Host Defenses
Nodules containing adult worms are surrounded by inflammatory
cells that are replaced by collagen and fibrotic tissue, thereby
localizing the worms. A study of nodules has shown that they are
11
areas of high cellular activity. Some microfilariae appear to be killed
before they ever leave the nodules where they are produced by the
female worm. Obviously many others escape the chronic
inflammatory responses and the granulomas commonly seen
surrounding nematodes in tissue. The exact composition of the
nodules varies, depending on the distance from the adult worms
and the age of the nodule. In general, neutrophils are followed by
eosinophils and macrophages. The involvement of eosinophils in
killing microfilariae in untreated patients suggests specific immune
reactions similar to those reported in other helminth infections. The
fibrous outer layer of the nodule contains blood vessels, which may
be surrounded in older nodules by cellular infiltrates that include
plasma cells and eosinophils.
Epidemiology
Transmission occurs through bites of vector blackflies in the family
Simuliidae. Although a few vector species breed in slow-moving
streams, most require fast-flowing, highly oxygenated streams or
rivers. For this reason, ocular onchocerciasis is often called "river
blindness."
Onchocerciasis is prevalent in many parts of tropical Africa and has
been reported in a few places in the Middle East. In the Western
hemisphere, it is an important and widespread infection in
Guatemala and the southern states of Mexico. It also appears in
other areas of Central America, and a few foci have been found in
Venezuela, Colombia, Surinam, Brazil, and Ecuador.
Diagnosis
Onchocerciasis is suggested by subcutaneous nodules or by the
characteristic scaly dermatitis in individuals living in endemic areas.
Positive diagnosis is usually made by identifying microfilariae in a
superficial skin biopsy made with a scalpel or an appropriate punch.
The skin samples, which are usually taken from the shoulder, are
placed in a drop of saline or distilled water on a microscope slide,
incubated for 30 minutes, and examined (Fig. 92-3). The diagnosis
may also be made by finding adult worms in nodules or by
observing microfilariae in the eye. Serologic tests are being
developed to aid in diagnosis when microfilariae cannot be detected
but onchocerciasis is suspected.
Control
Three main measures - vector control, nodule removal, and drug
treatment - provide limited control of onchocerciasis. Control of
blackfly vectors is difficult because most species breed in fastflowing streams to which insecticides cannot easily be applied.
12
Nodules harboring adult worms are usually removed, which
presumably reduces the rate at which microfilariae are produced
and thus the risk to the eyes (as well as the number of microfilariae
available to vectors). Mass treatment poses difficulties, because
suramin, the drug of choice for killing adult worms, must be given
intravenously and is toxic. Diethylcarbamazine kills microfilariae but
has limited efficacy against adult worms and has the disadvantage
that some patients experience a severe reaction, which may
exacerbate eye damage, to dying microfilariae. Ivermectin, a
semisynthetic macrolide antibiotic, has recently been shown to be
more effective and to produce fewer side effects than
diethylcarbamazine.
Minor Filarial Infections
Human filarial parasites of minor importance include the following
(Table 92-1):
Loa loa, limited in distribution to tropical Africa, best known for its
superficial migration under the conjunctiva of the eye and for the
presence of "fugitive" or "calabar" temporary swellings
Mansonella (syn. Dipetalonema or Acanthoceilonema) streptocerca,
also limited to tropical Africa and frequently presenting as a chronic
itching dermatitis; both adult worms and microfilariae are present in
the skin
Mansonella (syn. Dipetalonema or Acanthoceilonema) perstans,
found in Africa and South America
Mansonella ozzardi, restricted to the western hemisphere
Dirofilaria Species
Dirofilaria immitis (the dog heartworm) is a worldwide filarial
parasite of dogs; adult worms (up to 30 cm long) usually are located
in the dog's heart. In heavy infections, or when adult worms die, the
parasites may be carried to the pulmonary vessels where they may
produce emboli. The worms do not mature to adulthood in humans,
but larval stages have been reported in cutaneous nodules (which
may be confused with tumors) and have sometimes produced
lesions in the lungs (coin lesions) or in breast tissue. Pulmonary
lesions may be asymptomatic or may cause coughing or chest
pains. Roentgenograms frequently show a discrete mass suggestive
of a tumor. Larvae of other Dirofilaria spp. that parasitize lower
animals occasionally may be found in the skin or eyes of humans.
Dracunculus Medinensis
13
Dracunculus medinensis, the guinea worm, is not a true filarial
worm, but is often grouped with the filariae. It is one of the oldest
known parasitic diseases of man. Some authors suggest that the
ancient technique of removing the adult female worm, which may
be more than 1 meter long, by winding it on a stick, may be the
origin of the medical emblem, the caduceus.
Dracunculiasis is still quite common in parts of Africa and Asia.
Humans acquire the infection when they swallow infected copepods
(genus Cyclops) in drinking water. Often, the first sign of infection is
the formation of a blister when the adult female worm migrates to
the subcutaneous tissue. On contact with water, the blister breaks
and the worm ruptures and discharges larvae into the water. The
larvae are ingested by Cyclops, in which they develop to the
infective stage.
The ultimate location of the adult worm determines the pathology,
since lesions develop in response to the worms. Frequent sites of
inflammation and abscess include knee and ankle joints, as well as
the subcutaneous tissues of the extremities.
REFERENCES
Amaral F, Dreyer G, Figueredo-Silva J, Noroes J, Cavalcanti A, Samico
SC, Santos A, Coutinho A: Live adult worms detected by
ultrasonography in human bancroftian filariasis. Am J Trop Med Hyg
50:753, 1994
Cross JH, Partona F, Hsu MYK, Ash LR, Oemijati S: Experimental
transmission of Wuchereria bancrofti to monkeys. Am J Trop Med
Hyg 28:55, 1979
Cross JH: Recent advances in epidemiological field techniques in
filariasis. Southeast Asian J Trop Med Pub Hlth 24(Suppl)40, 1993
Freedman DO, deAlmeido Filho PJ, Besh S, Maiaes Silva MC, Braga C,
Maciel AJ: Lymphoscintigraphic analysis in lymphatic abnormalities
in symptomatic and asymptomatic human filariasis. J Infect Dis
170:927,1994
Gelband H: Diethylcarbamazine salt in the control of lymphatic
filariasis. Am J Trop Med Hyg 50:655, 1994
Moulia-Pilot JP, Glaziou P, Nguyen LN, Chanteau S, Martin PM, Cartel
JL. Long-term efficacy of a single dose treatment with 400
micrograms.kg-1 of ivermectin in bancroftian filariasis: results at one
year. Trop Med Parasitol 44:333, 1993
14
Tawill SA, Kipp W, Lucius R, Gallin M, Erttmann KD, Buttner DW:
Immunodiagnostic studies on Onchocerca volvulus and Mansonella
perstans infections using a recombinant 33 kDa O volvulus protein
(Ov33). Trans Roy Soc Trop Med Hyg 89:51, 1995
Turner PF, Rockett KA, Ottesen EA, Francis H, Awadzi K, Clark IA:
Interlukin-6 and tumor necrosis factor in the pathogenesis of
adverse reactions after treatment of lymphatic filariasis and
onchocerciasis. J Infect Dis 169:1071, 1994
Wamae CN, Advances in the diagnosis of human lymphatic filariasis:
a review. East Afr Med J 71:171,1994
World Health Organization: Lymphatic Filariasis: The disease and its
Control. WHO Tech Rpt Ser 821, Geneva, 1992
15
Das könnte Ihnen auch gefallen
- 28 Sept 2016 Kuliah Filariasis BaruDokument31 Seiten28 Sept 2016 Kuliah Filariasis BaruRafif AmirNoch keine Bewertungen
- Guidelines Filariasis Elimination IndiaDokument108 SeitenGuidelines Filariasis Elimination IndiaegalivanNoch keine Bewertungen
- Harrison's Internal Medicine Chapter 211. Filarial and Related InfectionsDokument9 SeitenHarrison's Internal Medicine Chapter 211. Filarial and Related InfectionsGaniNoch keine Bewertungen
- Wu C Here Ria Bancroft IDokument3 SeitenWu C Here Ria Bancroft IMariamNoch keine Bewertungen
- A. Readings DefinitionDokument5 SeitenA. Readings DefinitionAisa ShaneNoch keine Bewertungen
- Filariasis Parasite Infection and TransmissionDokument60 SeitenFilariasis Parasite Infection and TransmissionDanielle Pecson100% (1)
- Danoor - S FilariasisDokument6 SeitenDanoor - S FilariasisSUfyan RaZiNoch keine Bewertungen
- Revision: Types of Life Cycle in Trematoda and CestodaDokument54 SeitenRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekNoch keine Bewertungen
- Lymphatic Filariasis: Disease ManagementDokument10 SeitenLymphatic Filariasis: Disease ManagementamyNoch keine Bewertungen
- FILARIASISDokument3 SeitenFILARIASISALDE, ROBERT JOHN A.Noch keine Bewertungen
- The Filariae: Lymphatic System, Subcutaneous and Deep Connective TissueDokument17 SeitenThe Filariae: Lymphatic System, Subcutaneous and Deep Connective TissueKaranja GitauNoch keine Bewertungen
- Blood Tissue NematodesDokument27 SeitenBlood Tissue NematodesAfif Mamen100% (1)
- Brugia MalayiDokument8 SeitenBrugia MalayiROn Ace DancelNoch keine Bewertungen
- Brugia MalayiDokument2 SeitenBrugia MalayilatusiasandraNoch keine Bewertungen
- FILARIASISDokument57 SeitenFILARIASISadekayo100% (6)
- Onchocerca Volvulus Onchocerca Ochengi Litomosoides Sigmodontis Brugia Malayi Wuchereria Bancrofti Litomosoides SigmodontisDokument2 SeitenOnchocerca Volvulus Onchocerca Ochengi Litomosoides Sigmodontis Brugia Malayi Wuchereria Bancrofti Litomosoides SigmodontisCristina L. JaysonNoch keine Bewertungen
- Erbil Polytechnic University Report on Filarial WormsDokument15 SeitenErbil Polytechnic University Report on Filarial WormsHawre NajmaddinNoch keine Bewertungen
- FILARIASISDokument2 SeitenFILARIASISChizza Mae PacisNoch keine Bewertungen
- Malayi, or Brugia Timori. Unlike Most Other HelminthiasesDokument4 SeitenMalayi, or Brugia Timori. Unlike Most Other HelminthiasesMarscha MaryuanaNoch keine Bewertungen
- Filariasis: Dr. Mejbah Uddin AhmedDokument19 SeitenFilariasis: Dr. Mejbah Uddin Ahmedapi-19969058Noch keine Bewertungen
- 1) FilariasisDokument25 Seiten1) FilariasisNorbatNoch keine Bewertungen
- Lymphatic FillairiasisDokument7 SeitenLymphatic FillairiasisRitche DamasinNoch keine Bewertungen
- FilariaDokument85 SeitenFilariaRajkishor YadavNoch keine Bewertungen
- Filarial NematodeDokument18 SeitenFilarial NematodeHawre NajmaddinNoch keine Bewertungen
- Filariasis A. Readings: CD ReportDokument6 SeitenFilariasis A. Readings: CD ReportAisa ShaneNoch keine Bewertungen
- Brugia malayi causes elephantiasis in Southeast AsiaDokument4 SeitenBrugia malayi causes elephantiasis in Southeast AsiaJericha IsidroNoch keine Bewertungen
- General Parasitology L6Dokument13 SeitenGeneral Parasitology L6kayse abtidoonNoch keine Bewertungen
- Filariasis: Tropmed Block Faculty Medicine USU 2016Dokument26 SeitenFilariasis: Tropmed Block Faculty Medicine USU 2016Tiurma SibaraniNoch keine Bewertungen
- Wuchereria Bancrofti: Aby Elijah L. BernardinoDokument22 SeitenWuchereria Bancrofti: Aby Elijah L. BernardinoAby Brr100% (1)
- Chapter 84Dokument38 SeitenChapter 84Naimon Kumon KumonNoch keine Bewertungen
- FILARIASIS PPT FINALDokument39 SeitenFILARIASIS PPT FINALBinita Shakya100% (1)
- Filaria - A Comprehensive StudyDokument63 SeitenFilaria - A Comprehensive StudyDayledaniel SorvetoNoch keine Bewertungen
- Brugia timori Epidemiology and Life CycleDokument6 SeitenBrugia timori Epidemiology and Life CycleNurul Farhana IsmailNoch keine Bewertungen
- FilariaDokument16 SeitenFilariaJessa MayNoch keine Bewertungen
- Samenvatting Infectie en InflammatieDokument169 SeitenSamenvatting Infectie en InflammatiejeskevandiemenNoch keine Bewertungen
- Report PARA Lymphatic Filarial Nematodes Group 2 Adalid Asug AustriaDokument28 SeitenReport PARA Lymphatic Filarial Nematodes Group 2 Adalid Asug AustriaDaniel AustriaNoch keine Bewertungen
- Parasitology - Blood & Tissue - W Bancrofti B Malayi - PresentationDokument43 SeitenParasitology - Blood & Tissue - W Bancrofti B Malayi - PresentationNicole ManogNoch keine Bewertungen
- Brugia MalayiDokument12 SeitenBrugia Malayimuga restunaeshaNoch keine Bewertungen
- Filariasis: Dr.T.V.Rao MDDokument62 SeitenFilariasis: Dr.T.V.Rao MDDipankar NathNoch keine Bewertungen
- Segi College Kuala Lumpur: Group Member Khamini IzaidahDokument17 SeitenSegi College Kuala Lumpur: Group Member Khamini Izaidahshally918Noch keine Bewertungen
- PD FilariasisDokument8 SeitenPD FilariasisNarisha SmaradhantiaNoch keine Bewertungen
- BIOLOGY PROJECTS CLASS 12 CBSE INVESTIGTORY Elephantiasis Causes Cures Prevention, Treatment, Causes and Case Studies..Dokument28 SeitenBIOLOGY PROJECTS CLASS 12 CBSE INVESTIGTORY Elephantiasis Causes Cures Prevention, Treatment, Causes and Case Studies..Gaurav Kumar63% (19)
- Filariasis - Causes, Types, Symptoms, and ManagementDokument6 SeitenFilariasis - Causes, Types, Symptoms, and ManagementChumaNoch keine Bewertungen
- ElephantiasisDokument23 SeitenElephantiasisNitin0% (1)
- Faculty of Health Sciences: DepartmentDokument35 SeitenFaculty of Health Sciences: DepartmentAbdirashiid Mahdi HirsiNoch keine Bewertungen
- Wuchereria BancroftiDokument6 SeitenWuchereria BancroftiAinur RohmahNoch keine Bewertungen
- FilariasisDokument4 SeitenFilariasisKASHYAPNoch keine Bewertungen
- Epidemiology: FilariasisDokument10 SeitenEpidemiology: Filariasisketty putriNoch keine Bewertungen
- Bacterial Pneumonia Causative Agents Transmission RoutesDokument7 SeitenBacterial Pneumonia Causative Agents Transmission RoutesRusselle BuyaNoch keine Bewertungen
- Epidemiology and Control of Filariasis: Reshma Ann MathewDokument59 SeitenEpidemiology and Control of Filariasis: Reshma Ann MathewHanna HonorisNoch keine Bewertungen
- Parasitology Lec 3.01b Blood and Tissue NematodesDokument15 SeitenParasitology Lec 3.01b Blood and Tissue NematodesEnaWahahaNoch keine Bewertungen
- Kvir 13 2074130Dokument33 SeitenKvir 13 2074130Robert StryjakNoch keine Bewertungen
- LKS Helminth kelenjar lymph dan pembuluh venaDokument25 SeitenLKS Helminth kelenjar lymph dan pembuluh venaMECNESIA Tutor 2Noch keine Bewertungen
- Malaria Is A: PlasmodiumDokument21 SeitenMalaria Is A: PlasmodiumRhea AndradeNoch keine Bewertungen
- Blood and Tissue NematodesDokument37 SeitenBlood and Tissue NematodesjelenaNoch keine Bewertungen
- Malaria in ChildrenDokument19 SeitenMalaria in ChildrenAngel Ellene MarcialNoch keine Bewertungen
- Blood & Tissue NematodesDokument96 SeitenBlood & Tissue NematodesruthNoch keine Bewertungen
- Malaria in PregnancyDokument9 SeitenMalaria in Pregnancyamarendra WardhanaNoch keine Bewertungen
- Filariasis: Causes, Tests, and Treatment OptionsVon EverandFilariasis: Causes, Tests, and Treatment OptionsBewertung: 5 von 5 Sternen5/5 (2)
- 911 Pigeon Disease & Treatment Protocols!Von Everand911 Pigeon Disease & Treatment Protocols!Bewertung: 4 von 5 Sternen4/5 (1)
- Film Izle, HD Film Izle, HD Film Sitesi, Tek Parça Izle, Filmi Full Izle, 720p Film Izle, Yeni Çıkan Filmler, 2014 Filmleri, Türkçe Dublaj Izle, Tek Part Izle, Full HD Izle, Ücretsiz IzleDokument8 SeitenFilm Izle, HD Film Izle, HD Film Sitesi, Tek Parça Izle, Filmi Full Izle, 720p Film Izle, Yeni Çıkan Filmler, 2014 Filmleri, Türkçe Dublaj Izle, Tek Part Izle, Full HD Izle, Ücretsiz IzlesinevadiNoch keine Bewertungen
- Zikir Dan Do'a Sholat FardhuDokument9 SeitenZikir Dan Do'a Sholat FardhuMas SivNoch keine Bewertungen
- Film Izle, HD Film Izle, HD Film Sitesi, Tek Parça Izle, Filmi Full Izle, 720p Film Izle, Yeni Çıkan Filmler, 2014 Filmleri, Türkçe Dublaj Izle, Tek Part Izle, Full HD Izle, Ücretsiz IzleDokument8 SeitenFilm Izle, HD Film Izle, HD Film Sitesi, Tek Parça Izle, Filmi Full Izle, 720p Film Izle, Yeni Çıkan Filmler, 2014 Filmleri, Türkçe Dublaj Izle, Tek Part Izle, Full HD Izle, Ücretsiz IzlesinevadiNoch keine Bewertungen
- Proposal TBM Fkui 2014 PDFDokument12 SeitenProposal TBM Fkui 2014 PDFBadruz ZamanNoch keine Bewertungen
- Advance Trauma Life SupportDokument13 SeitenAdvance Trauma Life SupportJoãoBrasil100% (5)
- Advance Trauma Life SupportDokument13 SeitenAdvance Trauma Life SupportJoãoBrasil100% (5)
- ATCN 2013 Faculty Update (July 23)Dokument15 SeitenATCN 2013 Faculty Update (July 23)Opi SaNg MadRidistas100% (1)
- DIURETIKDokument28 SeitenDIURETIKOpi SaNg MadRidistasNoch keine Bewertungen
- Alkalosis RespiratorikDokument24 SeitenAlkalosis RespiratorikOpi SaNg MadRidistasNoch keine Bewertungen
- Kuliah Melabsorbsi UnizarDokument165 SeitenKuliah Melabsorbsi UnizarOpi SaNg MadRidistasNoch keine Bewertungen
- Osa 130802100614 Phpapp02Dokument54 SeitenOsa 130802100614 Phpapp02Opi SaNg MadRidistasNoch keine Bewertungen
- 19 Asean Congress of Anesthesiologists 2015 Yogyakarta - IndonesiaDokument5 Seiten19 Asean Congress of Anesthesiologists 2015 Yogyakarta - IndonesiaOpi SaNg MadRidistasNoch keine Bewertungen
- Obstructive Sleep ApneaDokument29 SeitenObstructive Sleep ApneaOpi SaNg MadRidistasNoch keine Bewertungen
- Assignment Miss Nurul - Obi and DayatDokument1 SeiteAssignment Miss Nurul - Obi and DayatOpi SaNg MadRidistasNoch keine Bewertungen
- Fisiologi NeuronDokument39 SeitenFisiologi NeuronMuzayyanatulhayat ARNoch keine Bewertungen
- Osa 130802100614 Phpapp02Dokument54 SeitenOsa 130802100614 Phpapp02Opi SaNg MadRidistasNoch keine Bewertungen
- Rates of Serious Infection After Changes in Regimens For Medical AbortionDokument9 SeitenRates of Serious Infection After Changes in Regimens For Medical AbortionOpi SaNg MadRidistasNoch keine Bewertungen
- Penyembuhan LukaDokument1 SeitePenyembuhan LukaOpi SaNg MadRidistasNoch keine Bewertungen
- Penyembuhan LukaDokument1 SeitePenyembuhan LukaOpi SaNg MadRidistasNoch keine Bewertungen
- How Rain Happens and What is a TsunamiDokument1 SeiteHow Rain Happens and What is a TsunamiOpi SaNg MadRidistasNoch keine Bewertungen