Beruflich Dokumente
Kultur Dokumente
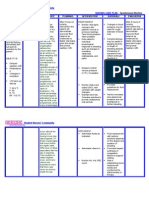
NCP Background, Demographic Data, Dordon's Functional Health, Drug Study SAint Louis University
Hochgeladen von
pa3kmedinaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NCP Background, Demographic Data, Dordon's Functional Health, Drug Study SAint Louis University
Hochgeladen von
pa3kmedinaCopyright:
Verfügbare Formate
I.
Patient’s Profile:
Full name: ?
Patient’s Nick name: ?
Sex: FEMALE
Civil Status: SINGLE
Age 25 YEARS OLD
Birth date: NOVEMBER 12, 1984
Birth place: DAMARTIS, LA UNION
Address NATIONAL HIGHWAY DAMARTIS, LA
UNION
Occupation: UNEMPLOYED
Weight: 115 POUNDS
Height 4 FEET; 11 INCHES
Payee: MOTHER AND FATHER
Religion: ROMAN CATHOLIC
Nationality: FILIPINO
Cultural Affinity: ILOCANO
Languages spoken: TAGALOG, ENGLISH, ILOCANO
Language Understood: TAGALOG, ENGLISH, ILOCANO
Date admitted: ?
Time admitted: 4:35 pm
Chief Complaint: FEVER AND COUGH
Ward: ?
Latest Hospitalization/admission: JANUARY 2010
II. Health History
A. Chief Complaint:
Upon ?’s admission on February 22, 2010 at 4:35 pm in Saint Louis Hospital of
Sacred Heart, her chief complaints were fever and cough. The patient had pale
conjunctiva and mucosa upon her arrival in the institution.
B. History of Present Illness:
?’s condition started one week prior to admission when she had productive cough
with yellowish color phlegm. She also experienced difficulty of breathing particularly
every night. There was no medication taken by the patient during the incident.
Three days prior to admission, the patient had fever with chills. She was able to
reach temperature of 38 degrees Celsius. Because of this, she had taken paracetamol 500
mg and salbutamol expectorant syrup which offered slight relief of her condition. 1 day
prior to hospitalization, she still had fever. She continued taking her medications.
However the condition persisted therefore she sought for consultation and was admitted
to Saint Louis University Hospital of Sacred Heart.
C. History of Past Illness:
In year 2000, the patient was diagnosed with hemolytic anemia. Because of this,
she maintained folic acid therapy. She was taking the drug once a day. She was
hospitalized for about ten times already.1 year ago, the patient had undergone blood
transfusion. The patient easily gets tired whenever she was performing any activity.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
1
According to the patient and her sister, her immunizations are adequate and
appropriate with the Expanded Program on Immunization and correct age as the bases.
She already received DPT1, DPT2, DPT3, OPV1, OPV2, OPV3, Hepa B1, Hepa B2,
Hepa B3, and Anti Measles1, from a Health center without any physiologic adverse
reaction to him.
1st dose 2nd dose 3rd dose Place Reaction
BCG Given; can’t Health center none
remember
DPT Given; can’t Given; can’t Given; can’t Health center none
remember remember remember
OPV Given; can’t Given; can’t Given; can’t Health Center none
remember remember remember
Hepa B Given; can’t Given; can’t Given; can’t Health Center none
remember remember remember
Anti Measles Given; can’t Health Center none
remember
D. Family Health History and social/ environment history:
? is the second child of the Oropilla family. Her mother has gravid para score of
G2P2 (2-0-0-2-0). Her mother and father are the decision makers of the family hence
they were a combination type of family. Her parents are the breadwinners. The patient
lives in a concrete type of house with family. They had no other companion in their non-
congested house. Their house consisted of two rooms and located on a non-congested
area. Their toilet is not a flush type. They don’t have any pet and there garbages are
collected weekly. There primary source of drinking water came from refilling station
while their domestic water came from water district.
The patient is non alcoholic and non smoker.
The patient noted no history of asthma, hypertension, diabetes mellitus, heart
disease, cancer or other heredo-familial disease.
*Course of Confinement:
?’s condition started a week PTA when she had experienced productive cough
with yellowish color phlegm and difficulty of breathing every night. 3 PTA, the patient
had fever with chills hence she had taken paracetamol 500 mg and salbutamol
expectorant syrup which provided slight relief of her condition. The patient’s condition
persisted therefore she sought for consultation and was admitted to SLU-HSH last
February 22, 2010 at 4:35 pm. Upon admission, she appears weak and had slender body
built, neat appearance, dry skin, calm emotional status, alert mental status, and fully
awake level of consciousness. The nurses hooked IVF of PNSS started as an infusion.
The health workers monitored her vital signs, assessed her capillary refill and level of
consciousness, regulated IVF at 16 hours and performed TSB. The nurses’ initial
diagnosis to the patient was risk for infection.
Throughout her confinement, she had undergone various diagnostic test like 4
CBC, 1 Urinalysis, 1 Ultrasound, 1 X-ray, 1 Creatinine Test, 1 BUN test, 1 SGOT and
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
2
SGPt test, B1, B2 test, 1 alkPO4 test and 1 parasitology. The medications given to the
patient were salbutamol neb now, ketorolac 30g IV now, ↑ acetylceistine 200 mg 1 sachet
TID, cefuroxime 750 mg IV q 8°, Paracetamol 1 amp IV q 4° PRN for headache and
fever, omeprazole 20 mg 1 tab OD, flic acid 5 mg 1 cap OD, azithromycin 500 mg 1 tab
OD, ketonoine, cefuroxime 500 mg 1 tab PRN, prednisone 20 g 1 tab OD, hydrocortisone
100 mg IV now then q 12° and dulcolax. 10 bottles of PNSS, 2 bottles of D5W and 2
packed RBCs were infused. The nursing diagnoses identified were risk for infection,
impaired peripheral tissue perfusion, ineffective peripheral tissue perfusion, disturbed
sleeping pattern, and acute pain. Some of the nursing interventions done were monitoring
of the vital signs, assessment of the general status, assessment of sleep pattern, provision
of rest periods, administration of the prescribed medications, positioning the patient in
semi fowler’s position, provision of comfort, encouragement of verbalization of feelings
and discomfort, emphasis on the importance of adequate rest, teaching proper hand
washing and teaching of DBE and CE. Last March 1, 2010, the patient had a may go
home order with final diagnosis of hemolytic anemia s/p blood transfusion, polysinusitis,
pneumonia in immunocompromised host and related disorder.
III. Gordon’s Health Pattern:
1. Health perception and management
The patient had a chief complaint of cough and fever upon admission to the
hospital. Latest diagnostics of the patient revealed that Neutrophil is 44.2 (low) and
lymphocyte was 46.3 (high). This indicates that the patient is prone to infection. She is
alert, responsive, coherent and oriented to time, place and person. According to her, she
is willing to do proper hand washing in order to prevent infection. She go to check-up
only if sign of disease is felt. She visits the dentist at least twice a year. The patient
understood the therapeutic regimens and diagnosis of the physician. This was confirmed
by her S.O. who said “Alam naman niya yung sakit niya e kaya nga siya nandito”.
Thorough health history was not given by her during the data gathering hence
confirmation and validation were done to her S.O. She had very limited and der response
to the questions asked to her. The patient complied on the therapeutic regimens and
medications although there were times wherein she was not taking her medications on
time. She doesn’t want to be disturbed when she was sleeping. However there was no
other difficulty in therapeutic regimen noted. She was capable of relating the progression
of illness in detail. According to the patient, she had completed her immunization and it
was complete and adequate based on Expanded Program on Immunization of DOH. This
was validated by her SO. According to the patient when she was home, she always
washed her hands before eating and took a bath daily. During observation, the patient did
not wash her hands prior to eating. During her confinement, she did facial wash daily.
The patient wanted to improve her condition thus she seeked for health workers. The
patient did not noted any family history of disease. She was a non alcohol drinker and
non-smoker. Last February 28, 2010, she appears week however on March 1, 2010, the
condition improved since she was capable of mobilizing herself by her own without
assistance. She had participated and undergone various diagnostics such as CBC,
Urinalysis, Ultrasound, X-ray, Creatinine Test, BUN test, SGOT and SGPT test, B1, B2
test, alkPO4 test and parasitology. He had undergone blood transfusion twice during her
confinement. According to the patient, this was her 10th hospitalization.
>Vital Signs (March 1, 2010)
PR: 70 beats/minutes
Temperature (Axilla) 36.5 degree Celsius
BP: 110/70 mmHg, R, lying
RR: 21 cycles/minute
2. Nutrition and metabolism
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
3
The patient presently weighs 115 kilograms with height of 4 ‘ 11 “ according to
the patient. The patient has ectomorph body type. According to the patient, she had lost
weight however she can no longer recall the amount of body weight loss. The patient’s
temperature (axilla) is 36.5 degrees Celsius. No nausea and vomiting noted during her
confinement. Usually, her breakfast, lunch and dinner are composed of rice and viand.
The viand that she prefers is vegetables. His usual snacks include bread, biscuit or
sandwich. The last meal she had taken is adobo and rice. She prefers vegetable and
fruits. She eats less meat because according to her S.O. “Baka sawa nay an sa meat kasi
nagtitinda kami ng karne”. She drinks soft drinks but not alcohol. The patient took about
adequate amount of water daily about 10 glasses of water. She doesn’t drinks liquor. The
patient doesn’t smoke. Her previous weakness, fever, coughs and difficulty of breathing
affects her nutrition. During those times, she had less appetite in eating. She was taking
iron for her dietary supplement. She complies with her medications. She has good skin
turgor however she has pale conjunctiva and mucous membrane. No evidence of edema
noted. His capillary refill takes about 2 seconds. She has complete sets of yellow teeth.
No scale nor dandruff noted on patient’s head. She has pale conjunctiva and mucous
membrane. Hematoma was seen on the right arm of the patient. No tenderness noted on
her abdomen upon palpation.
3. Elimination
No episodes of vomiting noted. The patient had no frequency in urine. Usually,
every 1 hour she urinates 200 cc of urine with a usual color of white or yellow. She
urinates depends upon her intake. Last urine voided is white. She is able to control urine.
The last stool of patient noted is color brown and watery. There is no difficulty in passing
stool. The patient is in the IV therapy: D5W 1 L x 16 hours.
I&0 last March 1, 2010 (7:00-3:00 shift)
INPUT OUTPUT
Oral Infusion Total Urine Total
1050 500 1550 1000 1000
Urine: 5 times
Stool: 1 time (watery)
4. Activity and exercise pattern
The patient does not work. She usually performed the household chores such as
cleaning the house. Her hobby is watching television. She is frequently in sleep.
According to her S.O, this serves as her relaxation activity. She is not member of any
type of organization. According to the patient, she easily experiences fatigue, and
weakness. She is a non-smoker and non-alcoholic. The patient is cooperative in
performing deep breathing exercises and coughing exercises. She can mobilize on her
own and doesn’t need assistance in performing activities of daily living.
RR=21 CPM
PR=70BPM
5. Cognition and perception
Eye (Vision):
The patient is not using eye glasses. According to her, she has no difficulty in
seeing. She has symmetry eyebrows. No dryness and scaling of the eyebrows noted. No
tenderness palpated on the eyebrows. No tearing observed. She has pale conjunctiva.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
4
Ears (Hearing):
The patient has light brown ears proportionate to the head and face. No lumps or
lesions observed. No discharges noted. The patient responded immediately during the
interview. She is not irritable.
Nose (Olfactory):
The patient has symmetrical nose. No deformities and lesions noted. No
discharges or flaring from nose seen. The patient has no difficulty in breathing.
Productive cough is observed to occur at few times.
Mouth:
The patient has symmetrical closure in the mouth. She has color light pale lips.
She incomplete sets of light yellow teeth. No lesions noted in the lips.
The patient is oriented to time, place and person. She can speak and understand
Tagalog, English and Ilocano.
6. Sleep and rest
Last February 15, 2010, the patient slept from 9:00 pm up to 7 am. According to
the patient, she infrequently experienced insomnia. The patient frequently experiences
interruptions in sleeping that’s why she has incomplete sleep at night. She was easily got
disturbed while on sleep. The patient usually takes naps every morning and afternoon.
She also spent time watching television as a form of his rest. She is frequently in sleep.
She is cooperative in performing deep breathing exercises and coughing exercises.
7. Self-perception and self-concept
The patient is coherent, alert and responsive. Sometimes she has eye to eye
contact during interview. She has no foul smell. She walks normally, stands and sits
straightly. Her dress is appropriate to situation and climate. She was cooperative during
interventions like vital signs taking and interview although sometimes she gives short
responses on questions asked to her. She responded in some of our questions during the
interview. She was not irritable during data gathering. She has a soft voice and looks shy.
8. Roles and relationships
The patient lives with her family in a concrete, non congested house with two
rooms. The patient is sometimes sociable to her neighbors however sometimes she likes
to be alone. According to her, she has good relationship with the neighborhoods. She is
also closed to his family at the same time. She is unemployed. She is a non-smoker and
non-alcoholic person. She usually spent time to hang out with her friends.
9. Sexuality and reproduction
The patient is single and she doesn’t have boy friend yet. She doesn’t experience
difficulty in urinating and passing stool. She has regular menstrual cycle and doesn’t
experience any abnormalities like dysmenorrhea.
10. Coping and stress management
When problem comes, the patient together with her family immediately does an
action to find solution. To cope when stress, she sleeps and watches TV to relax herself.
The patient doesn’t drink beer or smoke. The support system comes from her mother and
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
5
father who works as meat vendors. She participates and complies to the prescribed
medicines and other treatment given to her like blood transfusion and IV therapy. She is
cooperative in performing DBE and CE.
11. Values and beliefs
The patient is part of the Roman Catholic religion. She never consulted any herbal
doctor, “maghihilot” or “albularyo” yet. The patient has no belief that could affect the
provision of health care delivery system. She said that she follows the Filipino culture in
living just like using “po” and “opo”.
***Diagnostics:
1. CBC (March 01, 2010)
WBC 7.45 10 e9 / L 5-10
44.2 %N 45-70
46.3 %L 20-40
7.86 %M 0-12
0.839 %E 0-8
RBC 5.19 (4.50 – 6)
HGB 131 g/L (110-150)
HCT .377 L (.37-.47)
MCV 72.7 fL (76-96)
MCH 25.2 pg (27-32)
McHc 346 g/L (320-360)
Implication:
White blood cell (WBC) count is a count of the actual number of white blood
cells per volume of blood. Both increases and decreases can be significant. Neutrophils
function is for phagocytosis thus low neutophils indicates susceptibility to bacterial
infection. There is high lymphocytes which may indicate presence of infection because of
its increase response against infectious attack.. When the general defense systems of the
body have been penetrated by dangerous invading microorganisms, lymphocytes help
provide a specific response to attack the invading organisms.
NURSING CONSIDERATION: limit visitors because they are susceptible to infection,
hand washing because it is the most effective way of eradicating microbes, do not
swallow the sputum to prevent infection
2. VARIOUS TEST
February 22, 2010
TEST VALUE REF RANGE
ALK P: 99.0 35-129
CREA G .6 .6-1.3
ASAT 58.3 0-38
ALAT 197 0-41
UREA 3.0 2.5-6
D Bili .19 0-.30
TBIL-G 1.19 .1-1.20
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
6
Implication:
High ALAT and ASAT may indicate damage to patient’s red Blood cell. This
happens because the patient was diagnosed with hemolytic anemia. The enzymes are
release due to massive RBC destruction.
3. URINALYSIS
Fevruary 9, 2010
Physical examination Chemical examination Other examination
Color: lightyellow Albumin: Negative Pregnancy test: - - -
Reaction: Acidic Sugar: Negative Method: - - -
Appearance: turbid Acetone: - - - Others: - - -
Specific gravity: 1.005 Others : - - - Bacteria: few
Pus cells: 0-3/hpf Crystals: Negative Amorphous Urates:
Negative
Mucus threads: occasioanl Casts: Negative Yeast cells: neg
Epithelial cell: few
RBC-0-1/hpf
Implication:
It is important to get the urinalysis in order to determine the presence of blood in
urine. The patient has 0-1 hpf in urine which might indicate that RBC escape through
urine in the course of brisk hemolysis (Uthman,2004)
4. PARASITOLOGY
FEB. 24, 2010
Color: Black
Consistency: Formed
Method Ova / parasite Cyst
Direct fecal smear neg neg
RBC- negative
Pus cells - negative
Parasites could be one of the causative factors of CAP hence its presence on the
body of the patient is determined to determine of the parasites already multiply.
The patient’s stool is color black. She is suspected of anemia. This is one way to
trace whether the patient is excreting blood through stool in order to do immediate
correction and management.
5. UTZ and X-RAY
2/11/10
>Steaky densities are seen in both lower lung zones
>Cardiac shadow is enlarged
>Intact diaphragm
>A convexity to left of upper thoracic segment is noted have Cobb’s angle of 30 degrees
>Soft tissue shadows
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
7
Impression: Bibasal Pneumonia.
Implication:
These findings give impression of pneumonia. The patient was diagnosed with
CAP with the aid of this diagnostic test.
++Drug Analysis
A. omeprazole 20 mg 1 tab OD
Generic name:
• omeprazole
Brand name:
• Losec
Drug classes
• Antisecretory agent
• Proton pump inhibitor
Therapeutic actions
• Gastric acid-pump inhibitor: Suppresses gastric acid secretion by specific
inhibition of the hydrogen-potassium ATPase enzyme system at
the secretory surface of the gastric parietal cells; blocks the final step of acid
production.
Indications
• Long-term therapy: Treatment of pathologic hypersecretory conditions
Contraindications and cautions
• Contraindicated with hypersensitivity to omeprazole or its components.
• Use cautiously with pregnancy, lactation.
Adverse effects
• CNS: Headache, dizziness, asthenia, vertigo, insomnia, apathy,
anxiety, paresthesias, dream abnormalities
• Dermatologic: Rash, inflammation, urticaria, pruritus, alopecia, dry skin
• GI: Diarrhea, abdominal pain, nausea, vomiting, constipation, dry mouth, tongue
atrophy
• Respiratory: URI symptoms, cough, epistaxis
• Other: Cancer in preclinical studies, back pain, fever
Interactions
Drug-drug
• WARNING: Increased serum levels and potential increase in toxicity of
benzodiazepines, phenytoin, warfarin; if these combinations are used, monitor
patient very closely
• Decreased absorption with sucralfate; give these drugs at least 30 min apart
Nursing considerations
Assessment
• History: Hypersensitivity to omeprazole or any of its components; pregnancy,
lactation
• Physical: Skin lesions; T; reflexes, affect; urinary output, abdominal
examination; respiratory auscultation
Interventions
• before meals. Caution patient to swallow capsules whole—not to open, chew, or
crush them. If using oral suspension, empty packet into a small cup containing 2
tbsp of water. Stir and have patient drink immediately; fill cup with water and
have patient drink this water. Do not use any other diluent.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
8
• WARNING: Arrange for further evaluation of patient after 8 wk of therapy
for gastroreflux disorders; not intended for maintenance therapy. Symptomatic
improvement does not rule out gastric cancer, which did occur in preclinical
studies.
• Administer antacids, if needed.
Teaching points
• Take the drug before meals. Swallow the capsules whole; do not chew, open, or
crush them. If using the oral suspension, empty packet into a small cup containing
2 tablespoons of water. Stir and drink immediately; fill cup with water and drink
this water. Do not use any other liquid or food to dissolve the packet. This drug
will need to be taken for up to 8 weeks (short-term therapy) or for a prolonged
period (> 5 years in some cases).
• Have regular medical follow-up visits.
• You may experience these side effects: Dizziness (avoid driving or performing
hazardous tasks); headache (request medications); nausea, vomiting, diarrhea
(maintain proper nutrition); symptoms of upper respiratory tract infection, cough
(do not self-medicate; consult with your health care provider if uncomfortable).
• Report severe headache, worsening of symptoms, fever, chills.
B. Folic acid 5 g 1 cap OD
Generic name:
• folic acid (folate)
Brand name:
• Folvite
Drug class
• Folic acid
• Vitamin supplement
Therapeutic actions
• Required for nucleoprotein synthesis and maintenence of normal erythropoiesis.
Indications
• Treatment of anemias due to sprue, nutritional deficiency,
Contraindications and cautions
• Contraindicated with allergy to folic acid preparations;
pernicious, aplastic, normocytic anemias.
• Use cautiously during lactation.
Adverse effects
• Hypersensitivity: Allergic reactions
• Local: Pain and discomfort at injection site
Interactions
Drug-drug
• Decrease in serum phenytoin and increase in seizure activity with folic acid
preparations
• Decreased absorption with sulfasalazine, aminosalicyclic acid
Nursing considerations
Assessment
• History: Allergy to folic acid preparations;
pernicious, aplastic, normocytic anemias; lactation
• Physical: Skin lesions, color; R, adventitious sounds; CBC, Hgb, Hct,
serum folate levels, serum vitamin B12 levels, Schilling test
Interventions
• Administer orally if at all possible. With severe GI malabsorption or very severe
disease, give IM, IV, or subcutaneously.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
9
• Test using Schilling test and serum vitamin B12 levels to rule out pernicious
anemia. Therapy may mask signs of pernicious anemia while
the neurologic deterioration continues.
• WARNING: Use caution when giving the parenteral preparations to premature
infants. These preparations contain benzyl alcohol and may produce a fatal
gasping syndrome in premature infants.
• WARNING: Monitor patient for hypersensitivity reactions, especially if drug
previously taken. Keep supportive equipment and emergency drugs readily
available in case of serious allergic response.
Teaching points
• When the cause of megaloblastic anemia is treated or passes (infancy, pregnancy),
there may be no need for folic acid because it normally exists in sufficient
quantities in the diet.
• Report rash, difficulty breathing, pain or discomfort at injection site.
C. Fluimucil 300 mg 1 sachet TID
Brand name:
• Fluimucil
Generic name:
• Acetylcysteine
Indication:
• CAP
Drug Classification:
• Mucolytic agent
Mechanism of Action:
• Exerts mucolytic action through its free sulfhydryl group which opens up the
disulfide bonds in the mucoproteins thus lowering mucous viscosity. The exact
mechanism of action in acetaminophen toxicity is unknown. It is thought to act by
providing substrate for conjugation with the toxic metabolite.
Adverse Effects:
• Hypersensitivity reactions have been reported in patients receiving acetylcysteine,
including bronchospasm, angioedema, rashes and pruritus, may occur. Other
adverse effects reported include nausea and vomiting, fever, syncope, sweating,
arthralgia, blurred vision, disturbances of liver function.
Contraindication:
• MAO inhibitor therapy within 14 days initiating therapy; severe hypertension;
severe. Coronary artery disease, hypersensitivity to pseudoedephrine, acrivastine
or any component; renal impairment.
Nursing Responsibilities:
• Monitor effectiveness of therapy and advent of adverse/allergic effects. Instruct
patient in appropriate use and adverse effects to report.
A. Salbutamol 1 neb q 8 hours
Generic name:
• Albuterol sulfate
Brand name:
• Salbutamol
Classification:
• Bronchodilators
Action:
• Relaxes bronchial, uterine, and vascular smooth muscle by stimulating beta2
receptors
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
10
• Binds to beta2-adrenergic receptors in airway smooth muscle, leading to
activation of adenylcyclase and increased levels of cyclic-3', 5'-adenosine
monophosphate (cAMP). Increases in cAMP activate kinases, which inhibit the
phosphorylation of myosin and decrease intracellular calcium. Decreased
intracellular calcium relaxes smooth muscle airways.
• Relaxation of airway smooth muscle with subsequent bronchodilation
Indication:
• Used as a bronchodilator in the management of CAP
Contraindication:
• Use cautiously in patients w/ CV disorders, hyperthyroidism, or diabetes mellitus
and in those who are unusually responsive to adrenergics.
Adverse effect:
• CNS: nervousness, restlessness, tremor, headache, insomnia.
• CV: chest pain palpitations, angina, arrhythmias, hypertension.
• GI: nausea, vomiting.
• Endo: hyperglycemia.
• F and E: hypokalemia.
• Neuro: tremor
NURSING CONSIDERATION:
BEFORE:
• Assess lung sounds, pulse, and blood pressure before administration and during
peak of medication. Note amount, color, and character of sputum produced.
• Monitor pulmonary function tests before initiating therapy and periodically
throughout course to determine effectiveness of medication.
DURING:
• Observe for paradoxical bronchospasm (wheezing). If condition occurs, withhold
medication and notify physician or other health care professional immediately.
• Instruct mother to take missed dose as soon as remembered, spacing remaining
doses at regular intervals. Do not double doses or increase the dose or frequency
of doses.
AFTER:
• Inform the mother not to smoke near the child and to avoid respiratory irritants.
• Advise the mother to rinse the child’s mouth with water after each inhalation dose
to minimize dry mouth.
D. Paracetamol 1 amp IV q 4 hours PRN for headache and fever
PARACETAMOL 500 mg 1 tab q 6 hours PRN (>37.8)
Generic Name:
• paracetamol
Brand Name:
• Aceta
Drug classes:
• Antipyretic/Analgesic (nonopioid)
Therapeutic actions
• Reduces fever by acting directly on the hypothalamic heat-regulating center to
cause vasodilation and sweating, which helps dissipate heat.
• Analgesic: Site and mechanism of action unclear.
Indications
• Fever
Contraindications and cautions
• Contraindicated with allergy to acetaminophen.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
11
•
Use cautiously with impaired hepatic function, chronic alcoholism,
pregnancy, lactation.
Adverse effects
• CNS: Headache
• CV: Chest pain, dyspnea, myocardial damage when doses of 5–8 g/day are
ingested daily for several weeks or when doses of 4 g/day are ingested for
1 yr
• GI: Hepatic toxicity and failure, jaundice
• GU: Acute kidney failure, renal tubular necrosis
• Hematologic: Methemoglobinemia—cyanosis; hemolytic anemia—
hematuria, anuria; neutropenia, leukopenia, pancytopenia,
thrombocytopenia, hypoglycemia
• Hypersensitivity: Rash, fever
Drug-drug Interactions
• Increased toxicity with long-term, excessive ethanol ingestion
• Increased hypoprothrombinemic effect of oral anticoagulants
• Increased risk of hepatotoxicity and possible decreased therapeutic effects
with barbiturates, carbamazepine, hydantoins, rifampin, sulfinpyrazone
• Possible delayed or decreased effectiveness with anticholinergics
• Possible reduced absorption of acetaminophen with activated charcoal
• Possible decreased effectiveness of zidovudine
Nursing considerations
Assessment
• History: Allergy to acetaminophen, impaired hepatic function, chronic
alcoholism, pregnancy, lactation
• Physical: Skin color, lesions; T; liver evaluation; CBC, LFTs, renal
function tests
Interventions
• Do not exceed the recommended dosage.
• Consult physician if needed for children < 3 yr; if needed for longer than
10 days; if continued fever, severe or recurrent pain occurs (possible
serious illness).
• Avoid using multiple preparations containing acetaminophen. Carefully
check all OTC products.
• Give drug with food if GI upset occurs.
• Discontinue drug if hypersensitivity reactions occur.
• Treatment of overdose: Monitor serum levels regularly, N-acetylcysteine
should be available as a specific antidote; basic life support measures may
be necessary.
Teaching points
• Do not exceed recommended dose; do not take for longer than 10 days.
• Take the drug only for complaints indicated; it is not an anti-inflammatory
agent.
• Avoid the use of other over-the-counter preparations. They may contain
acetaminophen, and serious overdosage can occur. If you need an over-
the-counter preparation, consult your health care provider.
• Report rash, unusual bleeding or bruising, yellowing of skin or eyes,
changes in voiding patterns
F. Dulcolax
Generic name:
• Bisacodyl
Brand name:
• Dulcolax
MIMS Class :
• Laxatives, Purgatives
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
12
Mechanism of Action:
• Bisacodyl acts mainly in the large intestine by increasng its motility to effect bowel
evacuation.
• Stimulates peristalsis by directly irritating the smooth muscle of the intestine,
possibly the colonic intramural plexus; alters water and electrolyte secretion
producing net intestinal fluid accumulation and laxation
• Stimulant laxatives encourage bowel movements by acting on the intestinal wall.
They increase the muscle contractions that move along the stool mass. Stimulant
laxatives are a popular type of laxative for self-treatment. However, they also are
more likely to cause side effects. One of the stimulant laxatives, dehydrocholic acid,
may also be used for treating certain conditions of the biliary tract
Indication:
• empty the bowels before surgery and examinations such as X-ray
Contraindications:
• Acute surgical abdomen or intestinal obstruction, severe dehydration, faecal
impaction, chronic use.
• Ileus, intestinal obstruction, acute surgical abdominal conditions like appendicitis,
acute inflammatory bowel diseases, intestinal rectal, or stomach bleeding, and in
severe dehydration. Hypersensitivity to the drug.
Special Precautions:
• Swallow the tab whole. Pregnancy; inflammatory bowel disease.
Side effect:
• stomach cramps
• upset stomach
• diarrhea
• stomach and intestinal irritation
• faintness
• irritation or burning in the rectum (from suppositories)
Nursing Considerations:
• Take Dulcolax by mouth with or without food.
• Take Dulcolax with a full glass of water (8 oz/240 mL).
• Swallow Dulcolax whole. Do not break, crush, or chew before swallowing.
• Do not take Dulcolax within 1 hour after taking an antacid or milk.
• Use Dulcolax with caution in the ELDERLY; they may be more sensitive to its
effects.
• Dulcolax should not be used in CHILDREN younger than 6 years old; safety and
effectiveness in these children have not been confirmed.
Patient Teaching:
• If you miss a dose of Dulcolax and are taking it regularly, take it
as soon as possible. If it is almost time for your next dose, skip
the missed dose and go back to your regular dosing schedule. Do
not take 2 doses at once.
• Do not use for longer than 1 week without checking with your
doctor. Using Dulcolax for a long time may result in loss of
normal bowel function.
• Do not take additional laxatives or stool softeners with Dulcolax
unless directed by your doctor.
• Rectal bleeding or failure to have a bowel movement within 12 hours
after use of a laxative may be a sign of a serious condition. Stop use and
contact your doctor.
• If you notice a sudden change in bowel habits that lasts for 2 weeks or
more, do not continue using Dulcolax . Instead, check with your doctor.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
13
• PREGNANCY and BREAST-FEEDING: If you become pregnant,
contact your doctor. You will need to discuss the benefits and risks of
using Dulcolax while pregnant. It is not known if Dulcolax is found in
breast milk. If you are or will be breast-feeding take Dulcolax , check
with your doctor. Discuss any possible risks to your baby.
F. Ketorolac 30 g IV now
GENERIC NAME:
• Ketorolac
BRAND NAME:
• Toradol
CLASSIFICATION:
• Nonsteroidal anti-inflammatory agents, nonopioid analagesics
MECHANISM OF ACTION:
• Inhibits prostaglandin synthesis, producing peripherally mediated
analgesia
• Also has antipyretic and anti-inflammatory properties.
• Therapeutic effect:Decreased pain
INDICATION:
• Short term management of pain (not to exceed 5 days total for all routes
combined)
CONTRAINDICATIONS:
• Hypersensitivity
• Cross-sensitivity with other NSAIDs may exist¨Pre- or perioperative use
• Known alcohol intoleranceUse cautiously in:
1) History of GI bleeding
2) Renal impair-ment (dosage reduction may be required)
3) Cardiovascular disease
SIDE EFFECTS/ ADVERSE EFFECTS:
- CNS:
1) drowsiness
2) abnormal thinking
3) dizziness
4) euphoria
5) headache-
- RESP:
1) asthma
2) dyspnea
- CV:
1) edema
2) pallor
3) vasodilation
- GI:
1) GI Bleeding
2) abnormal taste
3) diarrhea
4) dry mouth
5) dyspepsia
6) GI pain
7) nausea
- GU:
1) oliguria
2) renal toxicity
3) urinary frequency
NURSING IMPLICATIONS/RESPONSIBILITIES:
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
14
• Patients who have asthma, aspirin-induced allergy, and nasal polyps are at
increased risk for developing hypersensitivity reactions. Assess for
rhinitis, asthma, and urticaria.
• Assess pain (note type, location, and intensity) prior to and 1-2 hr
following administration.
• Ketorolac therapy should always be given initially by the IM or IV route.
Oral therapy should be used only as a continuation of parenteral therapy.
• Caution patient to avoid concurrent use of alcohol, aspirin, NSAIDs,
acetaminophen, or other OTC medications without consulting health care
professional.
• Advise patient to consult if rash, itching, visual disturbances, tinnitus,
weight gain, edema, black stools, persistent headche, or influenza-like
syndromes (chills,fever,muscles aches, pain) occur.
• Effectiveness of therapy can be demonstrated by decrease in severity of
pain. Patients who do not respond to one NSAIDs may respond to another.
G. Cefuroxime 500 mg 1 tab now
GENERIC NAME:
• Cefuroxime
BRAND NAME:
• Ceftin
CLASSIFICATION
• Antibacterial
Mechanism of Action:
• Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-
binding proteins (PBPs) which in turn inhibits the final transpeptidation step of
peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall
biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall
autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is
arrested.
Contraindications:
• Hypersensitivity to cefuroxime, any component of the formulation, or other
cephalosporins
• Patients with known allergy to penicillins or cephalosphorins
iNDICATION :
• in treating infections of Upper and Lower respiratory tract
ADVERSE REACTIONS :
• Anaphylaxis, pseudomembranous colitis, nausea and vomiting, transient elevation
of liver enzymes.
Adverse Reactions
GI
• Nausea; vomiting; diarrhea; anorexia; abdominal pain or cramps; flatulence;
colitis, including pseudomembranous colitis.
Genitourinary
• Pyuria; renal dysfunction; dysuria; reversible interstitial nephritis; hematuria;
toxic nephropathy.
Hematologic
• Eosinophilia; neutropenia; lymphocytosis; leukocytosis; thrombocytopenia;
decreased platelet function; anemia; aplastic anemia; hemorrhage.
Hepatic
• Hepatic dysfunction; abnormal LFT results.
Miscellaneous
• Hypersensitivity, including Stevens-Johnson syndrome, erythema multiforme,
toxic epidermal necrolysis; candidal overgrowth; serum sickness–like reactions
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
15
(eg, skin rashes, polyarthritis, arthralgia, fever); phlebitis, thrombophlebitis,
and pain at injection site.
H. Hyrdrocortisone 100 mg IV now q 12 hours
Generic Name
• Hydrocortisone
Trade Name
• Cortef, Solu-Cortef, Hydrocortone, Cortenema
Pharmacologic Class
• Adrenal cortical steroid
• Corticosteroid
• Glucocorticoid
MOA:
Enters target cells and binds to cytoplasmic receptor; initiates many complex reactions
that are responsible for its anti-inflammatory, immunosuppressive (glucocorticoid), and
salt-retaining (mineralocorticoid) actions. Some actions may be undesirable, depending
on drug use.
Indication
• -Replacement therapy in adrenal cortical insufficiency
o Hematologic disorders
Side effects:
• Vertigo, headache, paresthesias, insomnia, seizures, psychosis
Nursing consideration:
Before
- Assess for contraindications.
- Assess body weight, skin color, V/S, urinalysis, serum electrolytes, X-rays, CBC.
- Arrange for increased dosage when patient is subject to unusual stress.
- Do not give live vaccines with immunosuppressive doses of hydrocortisone.
- Observe the 15 rights of drug administration.
During
- Give daily before 9am to mimic normal peak diurnal corticosteroid levels.
- Space multiple doses evenly throughout the day.
- Use minimal doses for minimal duration to minimize adverse effects.
- Do not give IM injections if patient has thrombocytopenic purpura.
- Taper doses when discontinuing high-dose or long-term therapy.
After
- Monitor client for at least 30 minutes.
- Educate client on the side effects of the medication and what to expect.
- Instruct client to report pain at injection site.
- Instruct client to take drug exactly as prescribed.
- Dispose of used materials properly.
- Document that drug has been given.
I. Azithromysin 500 mg 1 tab OD
Generic name:
• azithromycin
Brand name:
• Zithromax
Drug class
• Macrolide antibiotic
Therapeutic actions
• Bacteriostatic or bactericidal in susceptible bacteria.
Indications
• CAP
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
16
Contraindications and cautions
• Contraindicated with hypersensitivity to azithromycin, erythromycin, or any
macrolide antibiotic.
• Use cautiously with gonorrhea or syphilis, pseudomembranous colitis, hepatic
or renal impairment, lactation.
Adverse effects
• CNS: Dizziness, headache, vertigo, somnolence, fatigue
• GI: Diarrhea, abdominal pain, nausea, dyspepsia, flatulence, vomiting,
melena, pseudomembranous colitis
• Other: Superinfections, angioedema, rash, photosensitivity, vaginitis
Interactions
Drug-drug
• Decreased serum levels and effectiveness of azithromycin with aluminum and
magnesium-containing antacids
• Possible increased effects of theophylline
• Possible increased anticoagulant effects of warfarin
Drug-food
• Food greatly decreases the absorption of azithromycin
Nursing considerations
Assessment
• History: Hypersensitivity to azithromycin, erythromycin, or any macrolide
antibiotic; gonorrhea or syphilis, pseudomembranous colitis, hepatic or renal
impairment, lactation
• Physical: Site of infection; skin color, lesions; orientation, GI output, bowel
sounds, liver evaluation; culture and sensitivity tests of infection, urinalysis,
liver and renal function tests
Interventions
• Culture site of infection before therapy.
• Administer on an empty stomach 1 hr before or 2–3 hr after meals. Food
affects the absorption of this drug.
• Counsel patients being treated for STDs about appropriate precautions and
additional therapy.
Teaching points
• Take this drug on an empty stomach 1 hr before or 2–3 hr after meals; it
should never be taken with food. Take the full course prescribed. Do not take
with antacids.
• These side effects may occur: Stomach cramping, discomfort, diarrhea;
fatigue, headache (medication may help); additional infections in the mouth or
vagina (consult with health care provider for treatment).
• Report severe or watery diarrhea, severe nausea or vomiting, rash or itching,
mouth sores, vaginal sores.
J. Prednisone 1omg a tab OD
Generic name:
• prednisone
Brand name:
• Winpred
Drug classes
• Corticosteroid (intermediate acting)
• Glucocorticoid
• Hormone
Therapeutic actions
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
17
• Enters target cells and binds to intracellular corticosteroid receptors, thereby
initiating many complex reactions that are responsible for its anti-inflammatory
and immunosuppressive effects.
Indications
• CAP (inflammation
Adverse effects
• CNS: Vertigo, headache, paresthesias, insomnia, seizures, psychosis,
cataracts, increased IOP, glaucoma (long-term therapy); euphoria,
depression
• CV: Hypotension, shock, hypertension and CHF secondary to fluid
retention, thromboembolism, thrombophlebitis, fat embolism, cardiac
arrhythmias
• Electrolyte imbalance: Na+ and fluid retention, hypokalemia,
hypocalcemia
• Endocrine: Amenorrhea, irregular menses, growth retardation,
decreased carbohydrate tolerance, diabetes mellitus, cushingoid state
(long-term effect), increased blood sugar, increased serum cholesterol,
decreased T3 and T4 levels, HPA suppression with systemic therapy
longer than 5 days
• GI: Peptic or esophageal ulcer, pancreatitis, abdominal distention,
nausea, vomiting, increased appetite, weight gain (long-term therapy)
• Hypersensitivity: Hypersensitivity or anaphylactoid reactions
• Musculoskeletal: Muscle weakness, steroid myopathy, loss of muscle
mass, osteoporosis, spontaneous fractures (long-term therapy)
• Other: Immunosuppression, aggravation or masking of infections;
impaired wound healing; thin, fragile skin; petechiae, ecchymoses,
purpura, striae; subcutaneous fat atrophy
Interactions
Drug-drug
• Increased therapeutic and toxic effects with troleandomycin,
ketoconazole
• Increased therapeutic and toxic effects of estrogens, including hormonal
contraceptives
• Risk of severe deterioration of muscle strength in myasthenia gravis
patients who also are receiving ambenonium, edrophonium,
neostigmine, pyridostigmine
• Decreased steroid blood levels with barbiturates, phenytoin, rifampin
• Decreased effectiveness of salicylates
Nursing considerations
Assessment
• History: Infections; renal or liver disease, hypothyroidism, ulcerative colitis with
impending perforation, diverticulitis, active or latent peptic ulcer, inflammatory
bowel disease, CHF, hypertension, thromboembolic disorders, osteoporosis,
seizure disorders, diabetes mellitus; hepatic disease; lactation
• Physical: Weight, T, reflexes and grip strength, affect and orientation, P, BP,
peripheral perfusion, prominence of superficial veins, R, adventitious sounds,
serum electrolytes, blood glucose
Interventions
• Administer once-a-day doses before 9 AM to mimic normal peak corticosteroid
blood levels.
• Increase dosage when patient is subject to stress.
• WARNING: Taper doses when discontinuing high-dose or long-term therapy to
avoid adrenal insufficiency.
• Do not give live virus vaccines with immunosuppressive doses of corticosteroids.
Teaching points
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
18
• Do not stop taking the drug without consulting your health care provider.
• Avoid exposure to infections.
• Report unusual weight gain, swelling of the extremities, muscle weakness, black
or tarry stools, fever, prolonged sore throat, colds or other infections, worsening
of the disorder for which the drug is being taken.
X. List of Prioritized Diagnosis and Rationale:
PRIORITIZATION: ACTUAL OR POTENTIAL
1. Ineffective airway clearance r/t presence of ACTUAL
secretion secondary to CAP
2. Risk for infection r/t loss of secondary defense ACTUAL
secondary to CAP
3.5. Impaired gas exchange r/t airway constriction POTENTIAL
secondary to CAP
3.5. Impaired gas exchange r/t occluded airway POTENTIAL
secondary to CAP
5. fluid volume deficit r/t decreased hemoglobin POTENTIAL
6.5. Acute pain r/t inflammatory process secondary POTENTIAL
to polysinusitis
6.5. Acute pain r/t inflammatory process secondary POTENTIAL
to CAP
RATIONALE
Prioritization is done to be able to identify the different health problems of the
patient needs to be addressed first and given much focus. It is also the process of
establishing a preferential sequence for addressing nursing diagnoses and intervention. In
prioritizing the different nursing problems, theories are considered as rationale of the
prioritization.
NURSING DIAGNOSIS RATIONALE OF
PRIORITIZATION
1. Ineffective airway clearance r/t presence of Ineffective airway clearance is an
secretion secondary to CAP actual problem that must be addressed
first. According to the Maslow’s
Hierarchy of need, oxygen is part of the
physiologic need. According to
OFFTERAS, oxygen must be
addressed first. According to Kalish
Expanded Theory of Hierarchy, oxygen
must be prioritized first because its part
of the survival need.
2. Risk for infection r/t loss of secondary This is an actual problem and presently
defense secondary to CAP existing. The patient could be of risk of
infection due to low Neutrophils count.
Preventive interventions are still
applicable in order to prevent the
presence of infection.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
19
Impaired gas exchange is an actual
problem that must be addressed next.
Balancing the oxygen supply of the
patient is managed through
oxygenation which is readily available
in the institution hence it’s prioritized
second because the previous nursing
diagnosis requires more nursing
interventions. Based on Maslow’s
Hierarchy of need, oxygen is part of the
physiologic need. According to
OFFTERAS, oxygen must be
addressed first. According to Kalish
Gas exchange disorders are highly
prioritized because they are life
threatening.
3.5. Impaired gas exchange r/t airway This is a potential problem and
constriction secondary to CAP presently not existing however such
may occur particularly if there will be
complication of CAP.
Based on Maslow’s Hierarchy of need,
oxygen is part of the physiologic need.
According to OFFTERAS, oxygen
must be addressed first. According to
Kalish Gas exchange disorders are
highly prioritized because they are life
threatening.
3.5. Impaired gas exchange r/t occluded This is a potential problem. It is not
airway secondary to CAP presently existing however it may
happen if airway occlusion will occur.
According to Maslow’s Hierarchy of
need, oxygen is part of the physiologic
need. Based on OFFTERAS, oxygen
must be addressed first. According to
Kalish Gas exchange disorders are
highly prioritized because they are life
threatening.
5. fluid volume deficit r/t decreased This is a potential problem because the
hemoglobin patient has hemolytic anemia. Fluid
related problem is prioritized next to
oxygen problem in relation to
OFFTERAS. Fluid is one of the
physiologic needs according to
Maslow.
6.5. Acute pain r/t inflammatory process This is a potential problem since this
secondary to polysinusitis problem doesn’t exist however it may
occur based on pathophysiologic
occurrence. According to Maslow if the
physiologic needs are into met, it can
result to pain.
6.5. Acute pain r/t inflammatory process This is a potential problem since this
secondary to CAP problem doesn’t exist however it may
occur based on pathophysiologic
occurrence. According to Maslow if the
physiologic needs are into met, it can
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
20
result to pain.
Nursing care plan Submitted by: MEDINA, PATRICK LUIS
21
Das könnte Ihnen auch gefallen
- LEARN MAT 12 ACTIVITIES: RLE Activity 1 - Applying the Nursing Process to Identify Diagnoses and GoalsDokument12 SeitenLEARN MAT 12 ACTIVITIES: RLE Activity 1 - Applying the Nursing Process to Identify Diagnoses and GoalsChelsea Aquino0% (1)
- No. 10 SANAANI Topic For Esophagogastric Balloon Tamponade Tubes Billroth 1 and 11Dokument12 SeitenNo. 10 SANAANI Topic For Esophagogastric Balloon Tamponade Tubes Billroth 1 and 11Nur SanaaniNoch keine Bewertungen
- Or NCP (Impaired Elimination)Dokument1 SeiteOr NCP (Impaired Elimination)Nikki M. ArapolNoch keine Bewertungen
- CHN and OBDokument91 SeitenCHN and OBJoshua Christian GanNoch keine Bewertungen
- Case Study: Gastrointestinal System of Older People Case Scenario: LapayDokument1 SeiteCase Study: Gastrointestinal System of Older People Case Scenario: LapayAriaNoch keine Bewertungen
- Nursing Care Plan for Cholelithiasis Patient Undergoing ECGDokument2 SeitenNursing Care Plan for Cholelithiasis Patient Undergoing ECGJenny Ajoc0% (1)
- Assignment For Oxy. Online BasedDokument5 SeitenAssignment For Oxy. Online BasedNurhassem Nor AkangNoch keine Bewertungen
- ReflectionDokument42 SeitenReflectionRaidis PangilinanNoch keine Bewertungen
- Nursing care plan for patient with meningiomaDokument3 SeitenNursing care plan for patient with meningiomaShaira TillahNoch keine Bewertungen
- Nursing Responsibilities For Oxygen AdministrationDokument3 SeitenNursing Responsibilities For Oxygen AdministrationJahseh WolfeNoch keine Bewertungen
- 2nd Case Scenario BronchitisDokument5 Seiten2nd Case Scenario BronchitisKasandra Dawn Moquia BerisoNoch keine Bewertungen
- Cu 10Dokument2 SeitenCu 10gabbyNoch keine Bewertungen
- Discharge PlanDokument2 SeitenDischarge PlanRoxanne_Buenaf_5285Noch keine Bewertungen
- Acute Renal Failure Comprehensive Case AnalysisDokument7 SeitenAcute Renal Failure Comprehensive Case Analysisate NarsNoch keine Bewertungen
- NCP HyperthermiaDokument1 SeiteNCP HyperthermiaLeo_Rabacca_3610100% (1)
- Cell Ab ActivitiesDokument7 SeitenCell Ab ActivitiesJanelle Cabida Supnad100% (1)
- Patricia Mae T. Miranda: Assessment Family Nursing Care Diagnoses Planning Implementation EvaluationDokument2 SeitenPatricia Mae T. Miranda: Assessment Family Nursing Care Diagnoses Planning Implementation EvaluationPatricia Mae MirandaNoch keine Bewertungen
- Midyr Case Study NewDokument18 SeitenMidyr Case Study NewAndres Ham Samson BernabeNoch keine Bewertungen
- Nursing Care Plan for Acute Pain ManagementDokument3 SeitenNursing Care Plan for Acute Pain ManagementSheene Lysethea Sioteco AguilosNoch keine Bewertungen
- Upon Admission (15 PTS) in The Intensive Care Unit (15 PTS) : ? (5 Pts Each Parameter A Total of 15 Points)Dokument5 SeitenUpon Admission (15 PTS) in The Intensive Care Unit (15 PTS) : ? (5 Pts Each Parameter A Total of 15 Points)Janelle Cabida SupnadNoch keine Bewertungen
- Concept Map FormatDokument2 SeitenConcept Map FormatIAN MAVERICK LIMNoch keine Bewertungen
- Saldana - Fdar Lung CancerDokument2 SeitenSaldana - Fdar Lung CancerMika SaldañaNoch keine Bewertungen
- Assessment (Cues) Subjective/Objective Nursing Diagnosis Nursing Objectives Nursing Interventions Rationale Evaluation SubjectiveDokument2 SeitenAssessment (Cues) Subjective/Objective Nursing Diagnosis Nursing Objectives Nursing Interventions Rationale Evaluation SubjectiveJellaine Reyes AbarroNoch keine Bewertungen
- Discharge Plan CapDokument3 SeitenDischarge Plan Capalexander abasNoch keine Bewertungen
- HNP Case Scenario For Case StudyDokument2 SeitenHNP Case Scenario For Case StudyDeinielle Magdangal RomeroNoch keine Bewertungen
- History of Past IllnessDokument4 SeitenHistory of Past IllnesspachichoyNoch keine Bewertungen
- NCP Micu Hascvd Cad - RioDokument5 SeitenNCP Micu Hascvd Cad - RioRio BonifacioNoch keine Bewertungen
- NCP EsrdDokument2 SeitenNCP EsrdAziil LiizaNoch keine Bewertungen
- Essential care universally available at affordable cost defined as primary health careDokument11 SeitenEssential care universally available at affordable cost defined as primary health careAngelina Janiya NicoleNoch keine Bewertungen
- EsophagomyotomyDokument3 SeitenEsophagomyotomySamVelascoNoch keine Bewertungen
- Post Test - Renal Fabs - Prof. Garino - SCDokument2 SeitenPost Test - Renal Fabs - Prof. Garino - SCKristen FajilanNoch keine Bewertungen
- NAME: Aubrey Rose A. Vidon Section: BSN 2Y0-2 Course Unit #14Dokument2 SeitenNAME: Aubrey Rose A. Vidon Section: BSN 2Y0-2 Course Unit #14AriaNoch keine Bewertungen
- Ineffective Tissue Perfusion - NCPDokument7 SeitenIneffective Tissue Perfusion - NCPVianah Eve EscobidoNoch keine Bewertungen
- Goal/s: After 20 Minutes of Nurse-Client Interaction, Client Will Be Knowledgeable About Newly Diagnosed Condition (Acute Appendicitis)Dokument3 SeitenGoal/s: After 20 Minutes of Nurse-Client Interaction, Client Will Be Knowledgeable About Newly Diagnosed Condition (Acute Appendicitis)Rhn pjtNoch keine Bewertungen
- NCP CvaDokument7 SeitenNCP CvaEmerson SilverioNoch keine Bewertungen
- Sample (Concept Map)Dokument1 SeiteSample (Concept Map)NMDNMSSDNoch keine Bewertungen
- NcpsDokument10 SeitenNcpskotoirNoch keine Bewertungen
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Dokument5 SeitenSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNoch keine Bewertungen
- Nursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationDokument2 SeitenNursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationGrace MellaineNoch keine Bewertungen
- Assessment: Nutrition Diagnosis Nutrition Intervention Monitoring and Evaluation of Nutritional Status Goals: Goals MetDokument3 SeitenAssessment: Nutrition Diagnosis Nutrition Intervention Monitoring and Evaluation of Nutritional Status Goals: Goals MetIvan PogiNoch keine Bewertungen
- Nursing Care Plan Spontaneous AbortionDokument2 SeitenNursing Care Plan Spontaneous AbortionAbigael Rubio de LeonNoch keine Bewertungen
- The Story of GregorioDokument2 SeitenThe Story of GregorioKelly LegaspiNoch keine Bewertungen
- Acute Respiratory FailureDokument25 SeitenAcute Respiratory FailurejohnleeeNoch keine Bewertungen
- Nursing care for anticipatory grieving after pregnancy lossDokument1 SeiteNursing care for anticipatory grieving after pregnancy lossYsabelle GutierrezNoch keine Bewertungen
- Study Log 1 Objective CheckDokument3 SeitenStudy Log 1 Objective CheckWindi Dawn SallevaNoch keine Bewertungen
- NP4 Nursing Board ExamDokument7 SeitenNP4 Nursing Board ExamNewb TobikkoNoch keine Bewertungen
- Nursing Care Plan NCP Group 3 Fatigue ..Dokument2 SeitenNursing Care Plan NCP Group 3 Fatigue ..Aerron Severus Secano ShuldbergNoch keine Bewertungen
- IDPS Chapter 15Dokument10 SeitenIDPS Chapter 15002Noch keine Bewertungen
- D."Parang Giniginaw Man Ako" As Verbalized, Patient CoversDokument1 SeiteD."Parang Giniginaw Man Ako" As Verbalized, Patient CoversSherena NicolasNoch keine Bewertungen
- Case Scenario: Hot Spells, Porous BonesDokument10 SeitenCase Scenario: Hot Spells, Porous Bonesjaira magbanua100% (1)
- FHP SampleDokument8 SeitenFHP SampleJade GordoncilloNoch keine Bewertungen
- Cefipime HCL (AXERA)Dokument2 SeitenCefipime HCL (AXERA)Kristine YoungNoch keine Bewertungen
- Nursing Prognosis Criteria DocumentDokument3 SeitenNursing Prognosis Criteria DocumentJaye DangoNoch keine Bewertungen
- NCP Knowledge DeficitDokument2 SeitenNCP Knowledge DeficitPrincess Faniega SugatonNoch keine Bewertungen
- Preoperative Nursing 2021Dokument18 SeitenPreoperative Nursing 2021Jmarie Brillantes Popioco100% (1)
- 4 NCP - Acute Pain FinalDokument3 Seiten4 NCP - Acute Pain FinalElisha Gine AndalesNoch keine Bewertungen
- The Body FinalDokument61 SeitenThe Body FinalMhargie RomanillosNoch keine Bewertungen
- Acute Respiratory Distress Syndrome Secondary to COVID-19Dokument50 SeitenAcute Respiratory Distress Syndrome Secondary to COVID-19Echuserang FrogletNoch keine Bewertungen
- ENT Dr. Angel Case 29 Jan 17.00Dokument85 SeitenENT Dr. Angel Case 29 Jan 17.00Cindy PrayogoNoch keine Bewertungen
- Comprehensive Nursing Health History (Adult)Dokument5 SeitenComprehensive Nursing Health History (Adult)Ciedelle Honey Lou DimaligNoch keine Bewertungen
- Ethic Ole Gal - FinalDokument79 SeitenEthic Ole Gal - Finalpa3kmedinaNoch keine Bewertungen
- Higher Algebra - Hall & KnightDokument593 SeitenHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Palliative Ward JuurnalDokument8 SeitenPalliative Ward Juurnalpa3kmedinaNoch keine Bewertungen
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDokument2 SeitenNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- ApleDokument1 SeiteAplepa3kmedinaNoch keine Bewertungen
- Pathophysiology Community Aquired Pneumonia and AnemiaDokument3 SeitenPathophysiology Community Aquired Pneumonia and Anemiapa3kmedina100% (2)
- Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDokument2 SeitenIneffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedinaNoch keine Bewertungen
- NCP Proper Infection Related To Loss of Secondary DefenseDokument2 SeitenNCP Proper Infection Related To Loss of Secondary Defensepa3kmedinaNoch keine Bewertungen
- Psych JournalDokument10 SeitenPsych Journalpa3kmedinaNoch keine Bewertungen
- Chicago Healthcare Inventory RFPDokument5 SeitenChicago Healthcare Inventory RFPnirmala goonesinghaNoch keine Bewertungen
- W01W0116 0005jgheenDokument6 SeitenW01W0116 0005jgheenAulia GaffarNoch keine Bewertungen
- Acetylsalicilic Acid 500mg (Aspirin 500)Dokument8 SeitenAcetylsalicilic Acid 500mg (Aspirin 500)asdwasdNoch keine Bewertungen
- Quiz2 1 Issue2Dokument2 SeitenQuiz2 1 Issue2Jazur AhamedNoch keine Bewertungen
- Knowledge, Attitude and Practice of Cervical Cancer Screening Through Visual Inspection With Acetic AcidDokument10 SeitenKnowledge, Attitude and Practice of Cervical Cancer Screening Through Visual Inspection With Acetic AcidIJPHSNoch keine Bewertungen
- Handwashing NarrativeDokument9 SeitenHandwashing NarrativeMaria Angelica BermilloNoch keine Bewertungen
- Legacy of Tuskegee Syphilis StudyDokument2 SeitenLegacy of Tuskegee Syphilis StudyLcgessamanNoch keine Bewertungen
- Epos2020 PDFDokument481 SeitenEpos2020 PDFHanifa YuniasariNoch keine Bewertungen
- Konsult Sip ReportDokument72 SeitenKonsult Sip ReportMohit AgarwalNoch keine Bewertungen
- Heal Yourself-The Natural WayDokument489 SeitenHeal Yourself-The Natural Waygemoregold100% (18)
- STROKE AND TRANSIENT ISCHEMIC ATTACK-dikonversi-dikonversiDokument5 SeitenSTROKE AND TRANSIENT ISCHEMIC ATTACK-dikonversi-dikonversiOcing TanNoch keine Bewertungen
- LUTSDokument9 SeitenLUTSHatem SadekNoch keine Bewertungen
- Wilfredo Mallari Resume Safety Supervisor UpdatedDokument1 SeiteWilfredo Mallari Resume Safety Supervisor Updatedwilly mallariNoch keine Bewertungen
- Pamti Who Wipo WtoDokument262 SeitenPamti Who Wipo WtoJorge Antonio CENoch keine Bewertungen
- Health Talk On ContraceptionDokument32 SeitenHealth Talk On Contraceptionvaishali TMU studentNoch keine Bewertungen
- STRDokument179 SeitenSTRJatin AnandNoch keine Bewertungen
- Patient Assessment Tutorials - A Step-By-Step Guide For The Dental Hygienist (4th Edition) - Gehrig 9781496335005Dokument909 SeitenPatient Assessment Tutorials - A Step-By-Step Guide For The Dental Hygienist (4th Edition) - Gehrig 9781496335005Yesi75% (4)
- Acute Care Surgery: Aryono D.Pusponegoro Warko KarnadihardjaDokument9 SeitenAcute Care Surgery: Aryono D.Pusponegoro Warko KarnadihardjaDimas ErlanggaNoch keine Bewertungen
- Personal Development: Understanding Yourself and Building RelationshipsDokument6 SeitenPersonal Development: Understanding Yourself and Building RelationshipsYelhsa Ramos100% (2)
- Development of Protein Rich Flavored BarDokument6 SeitenDevelopment of Protein Rich Flavored BarIJRASETPublicationsNoch keine Bewertungen
- TreadsDokument4 SeitenTreadsKimberly FajardoNoch keine Bewertungen
- Enhancing Your Skills in Stroke Quality Improvement and Data AnalysisDokument50 SeitenEnhancing Your Skills in Stroke Quality Improvement and Data AnalysisRaisha Klinik Vaksinasi YogyakartaNoch keine Bewertungen
- The New Jose L. Amante Emergency HospitalDokument29 SeitenThe New Jose L. Amante Emergency HospitalRiah Ramirez FojasNoch keine Bewertungen
- 0 Notes 190815 204331 f4b PDFDokument4 Seiten0 Notes 190815 204331 f4b PDFLovejeet KaurNoch keine Bewertungen
- De Cuong - Tieng Anh Chuyen Nganh - LOP DINH DUONG - CHINH QUYDokument12 SeitenDe Cuong - Tieng Anh Chuyen Nganh - LOP DINH DUONG - CHINH QUYNguyễn Loan PhươngNoch keine Bewertungen
- Pharmacology: A Career inDokument2 SeitenPharmacology: A Career insnikt7863443Noch keine Bewertungen
- Adult Health Nursing II Practicum Course Syllabus 2020-2021Dokument117 SeitenAdult Health Nursing II Practicum Course Syllabus 2020-2021Hajer AlowaisiNoch keine Bewertungen
- FT42 Broz PDFDokument8 SeitenFT42 Broz PDFahmrakNoch keine Bewertungen
- Prescription: Sudha Assistant Professor Gnit College of Pharmacy Greater NoidaDokument28 SeitenPrescription: Sudha Assistant Professor Gnit College of Pharmacy Greater NoidaNilanjan MukherjeeNoch keine Bewertungen