Beruflich Dokumente
Kultur Dokumente
Nursing Care Plan For Appendectomy
Hochgeladen von
vanessajane09Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Care Plan For Appendectomy
Hochgeladen von
vanessajane09Copyright:
Verfügbare Formate
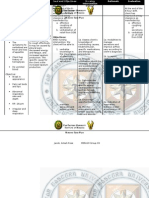
ASSESSMENT O: -Dressing on surgical site -Pale
DIAGNOSIS Risk for infection related to incision/suture in the right lower abdominal area.
PLANNING Short Term Goal: At the end of the shift, the client will identify interventions to prevent or reduce risk of infection. Long Term Goal: Within hospitalization, the client will achieve timely wound healing; be free of purulent drainage.
INTERVENTION
1. Note risk factors for occurrence of infection (e.g., skin/tissue wounds)
RATIONALE
EXPECTED OUTCOME
2. Stress proper hand hygiene by all caregivers between therapies and clients. 3. Assess and document skin conditions, noting inflammation and drainage. 4. Cleanse incision site per facility control with appropriate solution. 5. Administer or monitor medication regimen. 6. Emphasize necessity of taking antibiotics as directed.
To assess At the end of the shift causative/contributing the client will identify factors. interventions to prevent or reduce risk of A first-line defense infection like initiating against healthcare change of dressing on associated infections. surgical site and verbalizing the importance of daily hand washing. Within hospitalization the client will achieve timely wound healing as marked by absence of secretions in the dressing and verbalizing of the healing wound.
To reduce potential for catheter-related blood-stream infections. To determine effectiveness of therapy/presence of side effects.
ASSESSMENT S: -Pain scale of 7/10 O: -Dressing on surgical site -Pale -Facial grimacing
DIAGNOSIS Acute pain related to presence of surgical incision as manifested by facial grimacing.
PLANNING Short Term Goal: At the end of the shift, the client will report pain is relieved and controlled. Long Term Goal: Within hospitalization, the client will verbalize nonpharmacologic methods that provide relief.
INTERVENTION
1. Note clients
RATIONALE To assess etiology/precipitating contributing factors.
EXPECTED OUTCOME At the end of the shift the client will report pain is relived and controlled by verbalizing that his pain scale from 7/10 becomes 2/10 after taking medication. Within hospitalization the client will verbalize nonpharmacologic methods that provide relief like use of diversional activities such as TV, radio and socialization with others.
age/developmental level and condition affecting ability to report pain parameters. 2. Note location of surgical procedures. 3. Assess for referred pain, as appropriate. 4. Obtain clients assessment of pain to include location, characteristics, quality, intensity, etc. 5. Instruct an use of relaxation techniques (e.g., focused breathing) and diversional activities. 6. Administer analgesics as indicated to maximum dosage, as needed.
Influence the amount of post operative pain experienced. To help determine possibility of underlying condition. To rule out worsening of underlying condition/development of complication.
To distract attention and reduce tention.
To maintain acceptable level of pain. Notify physician if regimen is inadequate to meet pain control goal.
ASSESSMENT O: -With surgical incision at right lower abdominal area
DIAGNOSIS Impaired skin integrity related to destruction of skin/tissue layers.
PLANNING Short Term Goal: At the end of the shift, the client will display timely healing of skin lesions/wounds without complication Long Term Goal: After hospitalization, the client will participate in prevention measures and treatment program.
INTERVENTION
1. Determine nutritional
RATIONALE
EXPECTED OUTCOME
To assess At the end of the shift status potential for causative/contributing the client will display delayed healing factors. timely healing of skin exacerbated by lesions/wounds without malnutrition. complication by manifesting intact 2. Evaluate client with To identify risk for sutures and dry wound impaired cognition, injury/safety dressing. need/use of restraints, requirements. long term immobility. After hospitalization, the client will 3. Periodically remeasure To monitor progress participate in wound and observe for of wound healing. prevention measures complications. and treatment program like participating in in 4. Keep area clean/dry, passive range of motion carefully dress wounds, To assess bodys exercises. support incision. natural process of repair. 5. Encourage early Promotes circulation ambulation/mobilization. and reduces risks associated with immobility. 6. Assist the client/SO(s) Enhances in understanding and ff. commitment to plan, medical regimen and optimizing outcomes. daily maintenance.
ASSESSMENT O: -With surgical incision at right lower abdominal area
DIAGNOSIS Activity intolerance related to presence of surgical incision as manifested by limited mobility.
PLANNING Short Term Goal: At the end of the shift, the client will verbalize understanding of potential loss of ability in relation to existing condition. Long Term Goal: After hospitalization, the client will participate in conditioning and rehabilitation program to enhance ability to perform.
INTERVENTION
1. Note presence of
RATIONALE This may have potential for interfering with clients ability to perform at a desired level of activity. Provides baseline for comparison and opportunity to track changes.
EXPECTED OUTCOME At the end of the shift the client will verbalize understanding of potential loss of ability in relation to existing condition like verbalizing
habits and lifestyle that is appropriate to his condition.
medical diagnosis/ regimens.
2. Determine current activity level/physical condition with observation, exercise tolerance testing. 3. Implement physical therapy exercise with client and team members. 4. Instruct client in unfamiliar activities and alternate ways of doing familiar activities. 5. Assist client/SO(s) with planning for changes that may become necessary, such as use of supplemental oxygen.
Coordination of program enhances likelihood of success.
To conserve energy and promote safety.
After hospitalization, the client will participate in conditioning and rehabilitation program to enhance ability to perform like doing ROMEx, and relaxation techniques.
To improve clients ability to participate in desired activities.
ASSESSMENT O: -With surgical incision at right lower abdominal area -weight loss
DIAGNOSIS Imbalanced nutrition: less than body requirements related to nausea and vomiting, loss of appetite and decrease peristalsis as manifested by loss of weight.
PLANNING Short Term Goal: At the end of the shift, the client will demonstrate progressive weight gain toward goal. Long Term Goal: After hospitalization, the client will demonstrate behaviors, lifestyle changes to regain and/or maintain appropriate weight.
INTERVENTION 1. Determine clients ability to chew, swallow and taste food. 2. Discuss eating habits, including food preferences, intolerances/aversions. 3. Assess weight; measure/calculate body fat/muscle wasting, etc. 4. Evaluate total daily food intake, patterns and times of eating. 5. Consult dietician/nutritional team, as indicated. 6. Administer vitamin/mineral supplements as indicated. 7. Assist client/SO(s) to learn how to blenderize food.
RATIONALE All factors that can affect ingestion and/or digestion of nutrients. To appeal to clients like and dislikes.
EXPECTED OUTCOME At the end of the shift the client will demonstrate progressive weight gain toward goal by verbalizing to take in nutrients to meet metabolic needs. After hospitalization, the client will demonstrate behaviors, lifestyle changes to regain and/or maintain appropriate weight like taking adequate food, increase in appetite and interest in food.
May indicate proteinenergy malnutrition.
May have changes that could be made in clients intake. To implement interdisciplinary team management.
Supervision/home nutrition therapy.
Das könnte Ihnen auch gefallen
- Nursing Care Plan For Appendicitis NCPDokument2 SeitenNursing Care Plan For Appendicitis NCPderic77% (43)
- NCP AppendicitisDokument2 SeitenNCP Appendicitisdon-timothy-abenojar-795686% (7)
- NCP-S/P AppendectomyDokument6 SeitenNCP-S/P Appendectomytinatin989100% (7)
- Nursing Care Plan AppendicitisDokument2 SeitenNursing Care Plan Appendicitisderic95% (57)
- Appendectomy NCPDokument6 SeitenAppendectomy NCPLeah Fe Ariete Adtoon67% (3)
- Nursing Care Plan For Appendectomy - NCPDokument2 SeitenNursing Care Plan For Appendectomy - NCPderic86% (7)
- NCP AppendectomyDokument9 SeitenNCP Appendectomyken100% (3)
- NCP Post Op AppendectomyDokument3 SeitenNCP Post Op AppendectomyHakam Attawneh100% (2)
- Acute Pain Management Post AppendectomyDokument6 SeitenAcute Pain Management Post AppendectomyDaryl Valerio Francisco100% (1)
- Nursing Care for Post-Appendectomy PainDokument3 SeitenNursing Care for Post-Appendectomy PainChristian Karl B. LlanesNoch keine Bewertungen
- NCP Acute AppendicitisDokument2 SeitenNCP Acute AppendicitisJane Arian Berzabal100% (1)
- 4 Appendectomy Nursing Care PlansDokument8 Seiten4 Appendectomy Nursing Care PlansMarin Andrei100% (1)
- NCP AppendicitisDokument8 SeitenNCP AppendicitisAaron_Kim_Vela_4636Noch keine Bewertungen
- Final NCP AppendicitisDokument4 SeitenFinal NCP AppendicitisCha Ry100% (1)
- Nursing Care Plan For AppendicitisDokument2 SeitenNursing Care Plan For AppendicitisMarife Lipana Reyes80% (5)
- Assess Patient with Suspected AppendicitisDokument6 SeitenAssess Patient with Suspected AppendicitisRirin Ajeng Kartiningsih100% (1)
- Appendectomy Nursing Care Plan - Risk For InfectionDokument2 SeitenAppendectomy Nursing Care Plan - Risk For InfectionChebz Zy0% (1)
- NCP AppendicitisDokument5 SeitenNCP Appendicitismike_steven12100% (2)
- Appendectomy NCPDokument2 SeitenAppendectomy NCPQueency Vanguardia0% (1)
- Discharge Plan For AppendicitisDokument2 SeitenDischarge Plan For Appendicitismclubert100% (3)
- Appendectomy CSDokument30 SeitenAppendectomy CSMASIINoch keine Bewertungen
- Case Study of AppendicitisDokument14 SeitenCase Study of AppendicitisArvin Ian Penaflor89% (27)
- Post Appendectomy NCPDokument1 SeitePost Appendectomy NCPJharene BasbañoNoch keine Bewertungen
- Nursing Responsibilities For METRONIDAZOLEDokument1 SeiteNursing Responsibilities For METRONIDAZOLEIsrael Soria Espero63% (8)
- Case Study - AppendectomyDokument34 SeitenCase Study - Appendectomypuchay_chiepipaiiNoch keine Bewertungen
- Nursing Diagnosis for TonsillitisDokument3 SeitenNursing Diagnosis for TonsillitisVaneca Go67% (9)
- Acute Pain Related To Inflammation of Tissues Secondary To AppendicitisDokument2 SeitenAcute Pain Related To Inflammation of Tissues Secondary To AppendicitisRachel SaavedraNoch keine Bewertungen
- A Case Study On Acute AppendicitisDokument56 SeitenA Case Study On Acute AppendicitisIvy Mae Evangelio Vios92% (13)
- AppendectomyDokument4 SeitenAppendectomyKyre LandinginNoch keine Bewertungen
- Appendectomy/ Appendicitis Case StudyDokument15 SeitenAppendectomy/ Appendicitis Case StudyApril93% (30)
- Appendicitis Case StudyDokument21 SeitenAppendicitis Case Studyshayne100% (13)
- Nursing Care Plans For AppendicitisDokument2 SeitenNursing Care Plans For AppendicitisRodnie Insauriga GonzalesNoch keine Bewertungen
- Nursing Care Plan Fever AssessmentDokument1 SeiteNursing Care Plan Fever AssessmentLuis Romnic Vinuya100% (2)
- NCP AppendicitisDokument2 SeitenNCP Appendicitismnms0708100% (2)
- NCP MastectomyDokument2 SeitenNCP MastectomyDoc Duday100% (2)
- Sample Nursing Care Plan For Typhoid Fever (Risk)Dokument2 SeitenSample Nursing Care Plan For Typhoid Fever (Risk)Rhae Raynog100% (11)
- Nursing Care Plan: IndependentDokument2 SeitenNursing Care Plan: IndependentAdhaNoch keine Bewertungen
- Drug Study, NCP, and Discharge Plan For AppendectomyDokument12 SeitenDrug Study, NCP, and Discharge Plan For AppendectomyApril80% (5)
- Case Study On AppendicitisDokument15 SeitenCase Study On AppendicitisKristelle BonitaNoch keine Bewertungen
- HerniaDokument6 SeitenHerniahani alzo3bi100% (7)
- HerniasDokument64 SeitenHerniasKalpana SubediNoch keine Bewertungen
- AppendectomyDokument2 SeitenAppendectomyJoshua Triumfante De Vera IIINoch keine Bewertungen
- Delayed Surgical Recovery Nursing Care PlanDokument3 SeitenDelayed Surgical Recovery Nursing Care PlanMichala100% (3)
- NCP GrandcaseDokument5 SeitenNCP GrandcaseSaima BataloNoch keine Bewertungen
- NCP Cataract SurgeryDokument5 SeitenNCP Cataract SurgeryKristaJaneCelmarBagcatNoch keine Bewertungen
- NCPDokument8 SeitenNCPJose Benit DelacruzNoch keine Bewertungen
- Objectives of The Case StudyDokument5 SeitenObjectives of The Case StudyChristian TayagNoch keine Bewertungen
- Nursing Management of CVA and NIDDMDokument12 SeitenNursing Management of CVA and NIDDMKaloy KamaoNoch keine Bewertungen
- NCPs For ParotidectomyDokument12 SeitenNCPs For ParotidectomyCarla Manaloto50% (2)
- Nursing Care Plan for Skin Integrity Post-SurgeryDokument3 SeitenNursing Care Plan for Skin Integrity Post-SurgeryChristy BerryNoch keine Bewertungen
- NCPDokument10 SeitenNCPbabycheska08Noch keine Bewertungen
- Nursing Care PlanDokument9 SeitenNursing Care PlanjmichaelaNoch keine Bewertungen
- NCPDokument5 SeitenNCProxybabes100% (3)
- NCPs For ParotidectomyDokument8 SeitenNCPs For ParotidectomyAcohCChao100% (1)
- NCPDokument6 SeitenNCPAngelaTrinidadNoch keine Bewertungen
- Super Final NCPDokument16 SeitenSuper Final NCPNessaly Jane PrestoNoch keine Bewertungen
- Nursing Outline and Discharge PlanningDokument3 SeitenNursing Outline and Discharge PlanningEugene Gian-Mendro Alcoseba ZabateNoch keine Bewertungen
- Burns - Knowledge, DeficientDokument2 SeitenBurns - Knowledge, Deficientmakyofrancis20Noch keine Bewertungen
- Cues Nursing Diagnosis Scientific Reason Planning Intervention Rationale EvaluationDokument6 SeitenCues Nursing Diagnosis Scientific Reason Planning Intervention Rationale EvaluationKatrina Ponce86% (7)
- NCPDokument4 SeitenNCPNeil GoNoch keine Bewertungen
- Đề thi Tuyển sinh Chuyên Anh Phổ Thông Năng Khiếu 2017-2018 (Mã đề 567)Dokument14 SeitenĐề thi Tuyển sinh Chuyên Anh Phổ Thông Năng Khiếu 2017-2018 (Mã đề 567)William Phoenix67% (9)
- PNG Native Chicken Production ProposalDokument5 SeitenPNG Native Chicken Production ProposalNathan RukuNoch keine Bewertungen
- Whipple ComplicationDokument34 SeitenWhipple ComplicationMike Hugh100% (1)
- XS Energy DrinkDokument17 SeitenXS Energy DrinkCatalin GhinescuNoch keine Bewertungen
- E-Feed Formulation TemplateDokument19 SeitenE-Feed Formulation Templatemel CidNoch keine Bewertungen
- Blood Glucose MonitorDokument1 SeiteBlood Glucose MonitorCarolina TessandoriNoch keine Bewertungen
- 6-Egg Public HealthDokument48 Seiten6-Egg Public Healthhamad hamadNoch keine Bewertungen
- الملكيDokument123 SeitenالملكيGl HasnNoch keine Bewertungen
- FD Buttbible 2018 EbookDokument155 SeitenFD Buttbible 2018 Ebooktuti100% (1)
- Choosing The Right Fibre For Poultry Eubiotic LignocelluloseDokument2 SeitenChoosing The Right Fibre For Poultry Eubiotic LignocellulosevetbcasNoch keine Bewertungen
- Dengue Discharge PlanDokument1 SeiteDengue Discharge PlanChris Denver BancaleNoch keine Bewertungen
- US JanFeb10Dokument68 SeitenUS JanFeb10ERIK LABASTIDA MEDELLINNoch keine Bewertungen
- FERMENTATION OF SORGHUM USING YEAST (Saccharomyces Cerevisiae) AS A STARTER CULTURE FOR BURUKUTU PRODUCTIONDokument12 SeitenFERMENTATION OF SORGHUM USING YEAST (Saccharomyces Cerevisiae) AS A STARTER CULTURE FOR BURUKUTU PRODUCTIONwilolud2059100% (3)
- MKKDokument28 SeitenMKKMaithri Vidana KariyakaranageNoch keine Bewertungen
- Heal Your Eye Problems With Herbs, Minerals and VitaminsDokument117 SeitenHeal Your Eye Problems With Herbs, Minerals and VitaminsAadilNoch keine Bewertungen
- Natural Ramadan Fat Loss PDFDokument4 SeitenNatural Ramadan Fat Loss PDFAhmed KabeerNoch keine Bewertungen
- 18 Amazing Health Benefits From Honey and CinnamonDokument4 Seiten18 Amazing Health Benefits From Honey and Cinnamongladiola1100% (1)
- 2.7 AssessmentDokument6 Seiten2.7 AssessmentVani DeswalNoch keine Bewertungen
- Chris Thibaudeau. 9 Ways To Keep Getting BetterDokument2 SeitenChris Thibaudeau. 9 Ways To Keep Getting BetterPaolo AltoéNoch keine Bewertungen
- Cambridge Lower Secondary Science Learners Book 8 - Cambridge GO 2Dokument1 SeiteCambridge Lower Secondary Science Learners Book 8 - Cambridge GO 27dwg75s8mgNoch keine Bewertungen
- Promote Healthy Lifestyle Through Indoor Recreational ActivitiesDokument10 SeitenPromote Healthy Lifestyle Through Indoor Recreational ActivitiesRyahNeil Bohol Morales100% (1)
- Reading Comprehension Activity PDFDokument6 SeitenReading Comprehension Activity PDFSem KimNoch keine Bewertungen
- 90 Day Muscle Building Workout Plan Greatest Physiques PDFDokument12 Seiten90 Day Muscle Building Workout Plan Greatest Physiques PDFAli100% (1)
- Less Science, More Common SenseDokument11 SeitenLess Science, More Common SenseLan Pham PhuongNoch keine Bewertungen
- Factors That Affect LongevityDokument7 SeitenFactors That Affect LongevityPhan Thi Thanh LoanNoch keine Bewertungen
- Monounsaturated Fatty Acids and Immune FunctionDokument5 SeitenMonounsaturated Fatty Acids and Immune FunctionLucas PolizzeliNoch keine Bewertungen
- Swot and Pestle Analysis of SubwayDokument30 SeitenSwot and Pestle Analysis of Subwayhira waqas14100% (2)
- Manage Chronic Kidney Disease and Its ComplicationsDokument35 SeitenManage Chronic Kidney Disease and Its ComplicationsTresnanda Bellawana100% (1)
- Archives of Osteoporosis, 2021, 16, 102 - The Indian Society For Bone and Mineral Research (ISBMR) Position Statement For The DiagnosisDokument13 SeitenArchives of Osteoporosis, 2021, 16, 102 - The Indian Society For Bone and Mineral Research (ISBMR) Position Statement For The DiagnosisBHUENDOCRINE SRNoch keine Bewertungen
- Beggs Mechanotherapy Ortho / Orthodontic Courses by Indian Dental AcademyDokument130 SeitenBeggs Mechanotherapy Ortho / Orthodontic Courses by Indian Dental Academyindian dental academy100% (6)