Beruflich Dokumente
Kultur Dokumente
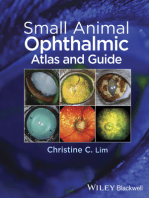
Differences between ocular manifestations of diabetes and vitamin A deficiency
Hochgeladen von
Param KahalOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Differences between ocular manifestations of diabetes and vitamin A deficiency
Hochgeladen von
Param KahalCopyright:
Verfügbare Formate
Differences between conjunctival and ciliary congestion
S. no. Feature Conjunctival congestion Ciliary congestion 1. Site More marked in the fornices More marked around the limbus 2. Colour Bright red Purple or dull red 3. Arrangement of vessels Superficial and branching Deep and radiating from limbus 4. On moving conjunctiva Congested vessels also move Congested vessels do not move 5. On mechanically squeezing out Vessels fill slowly from Vessels fill rapidly from the blood vessels fornix towards limbus limbus towards fornices 6. Blanching, i.e., on putting one Vessels immediately blanch Do not blanch drop of 1 in 10000 adrenaline 7. Common causes Acute conjunctivitis Acute iridocyclitis, keratitis (corneal ulcer)
Ocular Manifestations Of Diabetes mellitus
Ocular involvement in diabetes is very common. Structure-wise ocular lesions are as follows: 1. Lids. Xanthelasma and recurrent stye or internal hordeolum 2. Conjunctiva. Telangiectasia, sludging of the blood in conjunctival vessels and subcon-junctival haemorrhage 3. Cornea. Pigment dispersal at back of cornea, decreased corneal sensations (due to trigeminal neuropathy), punctate kerotapathy, Descemets folds, higher incidence of infective corneal ulcers and delayed epithelial healing due to abnormality in epithelial basement membrane 4. Iris. Rubeosis iridis (neovascularization) 5. Lens. Snow-flake cataract in patients with IDDM, posterior subcapsular cataract, early onset and early maturation of senile cataract 6. Vitreous. Vitreous haemorrhage and fibre- vascular proliferation secondary to diabetic retinopathy 7. Retina. Diabetic retinopathy and lipaemia retinalis (see page 259). 8. Intraocular pressure. Increased incidence of POAG, neovascular glaucoma and hypotony in diabetic ketoacidosis (due to increased plasma bicarbonate levels) 9. Optic nerve. Optic neuritis 10. Extraocular muscles. Ophthalmoplegia due to diabetic neuropathy 11. Changes in refraction. Hypermetropic shift in hypoglycemia, myopic shift in hyperglycemia and decreased accommodation
XEROPHTHALMIA
They term xerophthalmia is now reserved (by a joint WHO and USAID Committee, 1976) to cover all the ocular manifestations of vitamin A deficiency, including not only the structural changes affecting the conjunctiva, cornea and occasionally retina, but also the biophysical disorders of retinal rods and cones functions. Etiology
It occurs either due to dietary deficiency of vitamin A or its defective absorption from the gut. It has long been recognised that vitamin A deficiency does not occur as an isolated problem but is almost invariably accompanied by protein-energy malnutrition (PEM) and infections. WHO classification (1982) The new xerophthalmia classification (modification of original 1976 classification) is as follows: XN Night blindness X1A Conjunctival xerosis X1B Bitots spots X2 Corneal xerosis X3A Corneal ulceration/keratomalacia affecting less than one-third corneal surface X3B Corneal ulceration/keratomalacia affecting more than one-third corneal surface. XS Corneal scar due to xerophthalmia XF Xerophthalmic fundus. Clinical features 1. X N (night blindness). It is the earliest symptom of xerophthalmia in children. It has to be elicited by taking detailed history from the guardian or relative. 2. X1A (conjunctival xerosis). It consists of one or more patches of dry, lustreless, nonwettable conjunctiva (Fig. 19.1), which has been well described as emerging like sand banks at receding tide when the child ceases to cry. These patches almost always involve the inter-palpebral area of the temporal quadrants and often the nasal quadrants as well. In more advanced cases, the entire bulbar conjunctiva may be affected. Typical xerosis may be associated with conjunctival thickening, wrinkling and pigmentation. 3. X1B (Bitots spots). It is an extension of the xerotic process seen in stage X1A. The Bitots spot is a raised, silvery white, foamy, triangular patch of keratinised epithelium, situated on the bulbar conjunctiva in the inter-palpebral area (Fig. 19.2). It is usually bilateral and temporal, and less frequently nasal. 4. X2 (corneal xerosis). The earliest change in the cornea is punctate keratopathy which begins in the lower nasal quadrant, followed by haziness and/or granular pebbly dryness (Fig. 19.3). Involved cornea lacks lustre. 5. X3A and X3B (corneal ulceration/keratomalacia), Stromal defects occur in the late stage due to colliquative necrosis and take several forms. Small ulcers (1-3 mm) occur peripherally; they are characteristically circular, with steep margins and are sharply demarcated (Fig. 19.4). Large ulcers and areas of necrosis may extend centrally or involve the entire cornea. If appropriate therapy is instituted immediately, stromal defects involving less than one-third of corneal surface (X3A) usually heal, leaving some useful vision. However, larger stromal defects (X3B) (Fig. 19.5) commonly result in blindness.
6. XS (corneal scars). Healing of stromal defects results in corneal scars of different densities and sizes which may or may not cover the pupillary area (Fig. 19.6). A detailed history is required to ascertain the cause of corneal opacity. 7. XFC (Xerophthalmic fundus). It is characterized by typical seed-like, raised, whitish lesions scattered uniformly over the part of the fundus at the level of optic disc (Fig. 19.7). Treatment It includes local ocular therapy, vitamin A therapy and treatment of underlying general disease. 1. Local ocular therapy. For conjunctival xerosis artificial tears (0.7 percent hydroxypropyl methyl cellulose or 0.3 percent hypromellose) should be instilled every 3-4 hours. In the stage of keratomalacia, full-fledged treatment of bacterial corneal ulcer should be instituted (see pages 120-123). 2. Vitamin A therapy. Treatment schedules apply to all stages of active xerophthalmia viz. XN, X1A, X1B, X2, X3A and X3B. Oral administration is the recommended method of treatment. However, in the presence of repeated vomiting and severe diarrhoea, intramuscular injections of water-miscible preparation should be preferred. The WHO recommended schedule is as given below: i. All patients above the age of 1 year (except women of reproductive age): 200,000 IU of vitamin A orally or 100,000 IU by intramuscular injection should be given immediately on diagnosis and repeated the following day and 4 weeks later. ii. Children under the age of 1 year and children of any age who weigh less than 8 kg should be treated with half the doses for patients of more than 1 year of age. iii. Women of reproductive age, pregnant or not: (a) Those having night blindness (XN), conjunctival xerosis (X1A) and Bitots spots (X1B) should be treated with a daily dose of 10,000 IU of vitamin A orally (1 sugar coated tablet) for 2 weeks. (b) For corneal xerophthalmia, administration of full dosage schedule (described for patients above 1 year of age) is recommended. 3. Treatment of underlying conditions such as PEM and other nutritional disorders, diarrhoea, dehydration and electrolyte imbalance, infections and parasitic conditions should be considered simultaneously. Prophylaxis against xerophthalmia The three major known intervention strategies for the prevention and control of vitamin A deficiency are: 1. Short-term approach. It comprises periodic administration of vitamin A supplements. WHO recommended, universal distribution schedule of vitamin A for prevention is as follows: i. Infants 6-12 100,000 IU orally every months old and 3-6 months. any older children
who weigh less than 8 kg. ii. Children over 200,000 IU orally every 1 year and under 6 months. 6 years of age iii. Lactating 20,000 IU orally once at mothers delivery or during the next 2 months. This will raise the concentration of vitamin A in the breast milk and therefore, help to protect the breastfed infant. iv. Infants less 50,000 IU orally should than 6 months be given before they old, not being attain the age of 6 breastfed. months. A revised schedule of vitamin A supplements being followed in India since August 1992, under the programme named as Child Survival and Safe Motherhood (CSSM) is as follows: First dose (1 lakh I.U.)at 9 months of age along with measles vaccine. Second dose (2 lakh I.U.)at 18 months of age along with booster dose of DPT/OPV. Third dose (2 lakh I.U.)at 2 years of age. 2. Medium-term approach. It includes food fortification with vitamin A. 3. Long-term approach. It should be the ultimate aim. It implies promotion of adequate intake of vitamin A rich foods such as green leafy vegetables, papaya and drum- sticks (Fig. 19.8). Nutritional health education should be included in the curriculum of school children.
PUPILLARY REFLEXES AND THEIR ABNORMALITIES
PUPILLARY REFLEXES Light reflex When light is shone in one eye, both the pupils constrict. Constriction of the pupil to which light is shone is called direct light reflex and that of the other pupil is called consensual (indirect) light reflex. Light reflex is initiated by rods and cones. Pathway of light reflex (Fig. 12.6). The afferent fibres extend from retina to the pretectal nucleus in the midbrain. These travel along the optic nerve to the optic chiasma where fibres from the nasal retina decussate and travel along the opposite optic tract to terminate in the contralateral pretectal nucleus. While the fibres from the temporal retina remain uncrossed and travel along the optic tract of the same side to terminate in the ipsilateral pretectal nucleus. Internuncial fibres connect each pretectal nucleus with Edinger-Westphal nuclei of both sides. This connection forms the basis of consensual light reflex. Efferent pathway consists of the parasympathetic fibres which arise from the Edinger-Westphal nucleus in the mid-brain and travel along the third (oculomotor) cranial nerve. The preganglionic fibres
enter the inferior division of the third nerve and via the nerve to the inferior oblique reach the ciliary ganglion to relay. Post-ganglionic fibres travel along the short ciliary nerves to innervate the sphincter pupillae. Near reflex Near reflex occurs on looking at a near object. It consists of two components: (a) convergence reflex, i.e., contraction of pupil on convergence; and (b) accommodation reflex, i.e., contraction of pupil associated with accommodation. Pathway of convergence reflex (Fig. 12.7). Its afferent pathway is still not elucidated. It is assumed that the afferents from the medial recti travel centrally via the third nerve to the mesencephalic nucleus of the fifth nerve, to a presumptive convergence centre in the tectal or pretectal region. From this the impulse is relayed to the Edinger-Westphal nucleus and the subsequent efferent pathway of near reflex is along the 3rd nerve. The efferent fibres relay in the accessory ganglion before reaching the sphincter pupillae. Pathway of accommodation reflex (Fig. 12.7). The afferent impulses extend from the retina to the parastriate cortex via the optic nerve, chiasma, optic tract, lateral geniculate body, optic radiations, and striate cortex. From the parastriate cortex the impulses are relayed to the Edinger- Westphal nucleus of both sides via the occipito-mesencephalic tract and the pontine centre. From the Edinger-Westphal nucleus the efferent impulses travel along the 3rd nerve and reach the sphincter pupillae and ciliary muscle after relaying in the accessory and ciliary ganglions. Psychosensory reflex It refers to dilatation of the pupil in response to sensory and psychic stimuli. It is very complex and its mechanism is still not elucidated. ABNORMALITIES OF PUPILLARY REACTIONS 1. Amaurotic light reflex. It refers to the absence of direct light reflex on the affected side (say right eye) and absence of consensual light reflex on the normal side (i.e., left eye). This indicates lesions of the optic nerve or retina on the affected side (i.e., right eye), leading to complete blindness. In diffuse illumination both pupils are of equal size. 2. Efferent pathway defect. Absence of both direct and consensual light reflex on the affected side (say right eye) and presence of both direct and consensual light reflex on the normal side (i.e., left eye) indicates efferent pathway defect (sphincter paralysis). Near reflex is also absent on the affected side. Its causes include: effect of parasympatholytic drugs (e.g., atropine, homatropine), internal ophthalmoplegia, and third nerve paralysis. 3. Wernickes hemianopic pupil. It indicates lesion of the optic tract. In this condition light reflex (ipsilateral direct and contralateral consensual) is absent when light is thrown on the temporal half of
the retina of the affected side and nasal half of the opposite side; while it is present when the light is thrown on the nasal half of the affected side and temporal half of the opposite side. 4. Marcus Gunn pupil. It is the paradoxical response of a pupil of light in the presence of a relative afferent pathway defect (RAPD). It is tested by swinging flash light test. For details see page 474. 5. Argyll Robertson pupil (ARP) . Here the pupil is slightly small in size and reaction to near reflex is present but light reflex is absent, i.e., there is light near dissociation (to remember, the acronym ARP may stand for accommodation reflex present). Both pupils are involved and dilate poorly with mydriatics. It is caused by a lesion (usually neurosyphilis) in the region of tectum. 6. The Adies tonic pupil. In this condition reaction to light is absent and to near reflex is very slow and tonic. The affected pupil is larger (anisocoria). Its exact cause is not known. It is usually unilateral, associated with absent knee jerk and occurs more often in young women. Adies pupil constricts with weak pilocarpine (0.125%) drops, while normal pupil does not.
Das könnte Ihnen auch gefallen
- Systemic Ophthalmology Disorders GuideDokument4 SeitenSystemic Ophthalmology Disorders GuideAslesa Wangpathi Pagehgiri100% (1)
- Vitamin A Deficiency Guide: Causes, Signs, TreatmentDokument35 SeitenVitamin A Deficiency Guide: Causes, Signs, TreatmentSemina LimbuNoch keine Bewertungen
- Fat Soluble Vitamin RevisedDokument80 SeitenFat Soluble Vitamin RevisedsumitNoch keine Bewertungen
- 5.vit A DeficiencyDokument21 Seiten5.vit A DeficiencyDominic SkskNoch keine Bewertungen
- Xerophthalmia 190715182114Dokument31 SeitenXerophthalmia 190715182114Murali DharanNoch keine Bewertungen
- Eye Surgery Techniques and Common ConditionsDokument17 SeitenEye Surgery Techniques and Common ConditionsRasyid ridhoNoch keine Bewertungen
- Ophthalmology - Systemic - Community OphthalmologyDokument7 SeitenOphthalmology - Systemic - Community OphthalmologyjbtcmdtjjvNoch keine Bewertungen
- Vernal Keratoconjunctivitis: Why Is Allergic Eye Disease A Problem For Eye Workers?Dokument3 SeitenVernal Keratoconjunctivitis: Why Is Allergic Eye Disease A Problem For Eye Workers?darendraabimayuNoch keine Bewertungen
- Dental Management of Patient With Leukemia PedoDokument26 SeitenDental Management of Patient With Leukemia PedoFourthMolar.comNoch keine Bewertungen
- Dental Management of Patient With Leukemia PedoDokument26 SeitenDental Management of Patient With Leukemia PedoFourthMolar.com100% (1)
- Eye & ENTDokument12 SeitenEye & ENTShandar SadafNoch keine Bewertungen
- A Clinicopathological Study of Vernal Conjunctivitis in Urban and Rural Areas of Eastern India: A Hospital Based StudyDokument8 SeitenA Clinicopathological Study of Vernal Conjunctivitis in Urban and Rural Areas of Eastern India: A Hospital Based StudyMuhammad AbdillahNoch keine Bewertungen
- UveitisDokument24 SeitenUveitisJoan GarzónNoch keine Bewertungen
- Uveal Tract - DR SisonDokument7 SeitenUveal Tract - DR SisonJOv'z AnayasanNoch keine Bewertungen
- Tuberculous Posterior Scleritis Case ReportDokument6 SeitenTuberculous Posterior Scleritis Case ReportInayatul muthmainnahNoch keine Bewertungen
- Veterinary Clinics: Canine and Feline UveitisDokument24 SeitenVeterinary Clinics: Canine and Feline UveitisAdrian RamirezNoch keine Bewertungen
- OpthaDokument5 SeitenOpthavarun2k6Noch keine Bewertungen
- Orbital Cellulitis: Causes, Symptoms and TreatmentDokument42 SeitenOrbital Cellulitis: Causes, Symptoms and Treatmentmuhammad iqbalNoch keine Bewertungen
- PHCN Practical RecordDokument35 SeitenPHCN Practical RecordDola KalyanNoch keine Bewertungen
- Refrat: Pembimbing: DR - Rahmad Syuhada SP.MDokument26 SeitenRefrat: Pembimbing: DR - Rahmad Syuhada SP.MIzza TanzihulNoch keine Bewertungen
- Seasonal Monthly Variation Amongst Reported Cataract Surgeries in IndiaDokument92 SeitenSeasonal Monthly Variation Amongst Reported Cataract Surgeries in IndiafriendsofindiaNoch keine Bewertungen
- Experimental Study On Cryotherapy For Fungal Corneal Ulcer: Researcharticle Open AccessDokument9 SeitenExperimental Study On Cryotherapy For Fungal Corneal Ulcer: Researcharticle Open AccessSusPa NarahaNoch keine Bewertungen
- Disorders of The EyeDokument16 SeitenDisorders of The Eyelisette_sakuraNoch keine Bewertungen
- Trachoma: Ayalu Getinet June 1 2007Dokument50 SeitenTrachoma: Ayalu Getinet June 1 2007Yoseph DemisseNoch keine Bewertungen
- The Conjunctiva: Lecture One DR - Ali.a.taqiDokument56 SeitenThe Conjunctiva: Lecture One DR - Ali.a.taqiJorge Esteban Novelo PavíaNoch keine Bewertungen
- Botox in Ophthalmology: Mechanism, Applications and ComplicationsDokument60 SeitenBotox in Ophthalmology: Mechanism, Applications and ComplicationsJP OmerNoch keine Bewertungen
- PHCN PracticalDokument33 SeitenPHCN PracticalDola KalyanNoch keine Bewertungen
- Common Conjunctival LesionsDokument4 SeitenCommon Conjunctival LesionsSri AgustinaNoch keine Bewertungen
- Clinical Pathogenesis and Treatment of XEROPHTHALMIADokument1 SeiteClinical Pathogenesis and Treatment of XEROPHTHALMIARavan WidiNoch keine Bewertungen
- C CA AS SC CL Liin Niiq QU UE E // C CA AS SE ER RE EP PO OR RT TDokument7 SeitenC CA AS SC CL Liin Niiq QU UE E // C CA AS SE ER RE EP PO OR RT TG Virucha Meivila IINoch keine Bewertungen
- Guidelines For The Management of Corneal Ulcer WHODokument36 SeitenGuidelines For The Management of Corneal Ulcer WHOichalledhaNoch keine Bewertungen
- ICU Eye Care Guidelines for Preventing DiseaseDokument6 SeitenICU Eye Care Guidelines for Preventing DiseaseKiki dwi PratiwiNoch keine Bewertungen
- Cirugía de Senos y Globo OcularDokument21 SeitenCirugía de Senos y Globo Ocularjorge pradaNoch keine Bewertungen
- Sal Agar 2015Dokument2 SeitenSal Agar 2015occcNoch keine Bewertungen
- CNLDO Guide: Symptoms, Examination, ManagementDokument6 SeitenCNLDO Guide: Symptoms, Examination, ManagementKhairul FitrahNoch keine Bewertungen
- Treating Corneal Ulceration in Dogs Part 2 Deep UlcersDokument16 SeitenTreating Corneal Ulceration in Dogs Part 2 Deep UlcersAndreea MayaNoch keine Bewertungen
- Feline UveitesDokument9 SeitenFeline UveitesErick ConfickeerzNoch keine Bewertungen
- Abnormalities of EyeDokument74 SeitenAbnormalities of EyeHikmat UllahNoch keine Bewertungen
- OzaenaDokument4 SeitenOzaenaArdi PratamaNoch keine Bewertungen
- Hemifacial Spasm: Essam A. El Toukhy and Bryan R. CostinDokument3 SeitenHemifacial Spasm: Essam A. El Toukhy and Bryan R. CostinMinca CristinaNoch keine Bewertungen
- Case Discussion - GlaucomaDokument5 SeitenCase Discussion - GlaucomatwelvefeetNoch keine Bewertungen
- Orbital CellulitisDokument42 SeitenOrbital CellulitisDita HannaNoch keine Bewertungen
- Dipake Lamellar Ichthyosis enDokument6 SeitenDipake Lamellar Ichthyosis enprajnamitaNoch keine Bewertungen
- And Treatment Blepharokeratoconjunctivitis in Children: DiagnosisDokument5 SeitenAnd Treatment Blepharokeratoconjunctivitis in Children: DiagnosislordaponkNoch keine Bewertungen
- Vit A DeficiencyDokument27 SeitenVit A DeficiencyNatnaelNoch keine Bewertungen
- common ophthalmic problem in childrenDokument68 Seitencommon ophthalmic problem in childrenJoel ChongNoch keine Bewertungen
- Prevention of Blindness in Leprosy: An Overview of The Relevant Clinical and Programme-Planning IssuesDokument9 SeitenPrevention of Blindness in Leprosy: An Overview of The Relevant Clinical and Programme-Planning IssuesBudi KhangNoch keine Bewertungen
- EchothiophateDokument5 SeitenEchothiophaterarasNoch keine Bewertungen
- Iritis 8Dokument14 SeitenIritis 8Alvis KurniawanNoch keine Bewertungen
- English Premium Exam: Filial de Ciencias Médicas of BaracoaDokument9 SeitenEnglish Premium Exam: Filial de Ciencias Médicas of BaracoaDouglas Soslan Reyes FiffeNoch keine Bewertungen
- OPTHALMIA NEONATORUM: Is An Eye Infection That Occurs at Birth or During The First MonthDokument4 SeitenOPTHALMIA NEONATORUM: Is An Eye Infection That Occurs at Birth or During The First Monthcharuz_092823Noch keine Bewertungen
- Post-op Cataract Complications GuideDokument7 SeitenPost-op Cataract Complications GuideSurendar KesavanNoch keine Bewertungen
- Rehabilitation of A Complete Maxillectomy Patient: A Case Report of Osteomyelitis of MaxillaDokument6 SeitenRehabilitation of A Complete Maxillectomy Patient: A Case Report of Osteomyelitis of MaxillajoephinNoch keine Bewertungen
- Group ADokument41 SeitenGroup ASushant GyawaliNoch keine Bewertungen
- Orbital Cellulitis As A Complication of Odontogenic InfectionDokument5 SeitenOrbital Cellulitis As A Complication of Odontogenic InfectionCikal Abyan Nur 1417Noch keine Bewertungen
- Entropion and Ectropion: Disease-a-MonthDokument6 SeitenEntropion and Ectropion: Disease-a-MonthWILMER HUANGANoch keine Bewertungen
- 1 - Vitamins A, B1, B3 & CDokument8 Seiten1 - Vitamins A, B1, B3 & CIbrahim RamizNoch keine Bewertungen
- Spina Bifida Anatomy, Causes, and Nursing CareDokument5 SeitenSpina Bifida Anatomy, Causes, and Nursing Careroseavy100% (1)
- Complications in UveitisVon EverandComplications in UveitisFrancesco PichiNoch keine Bewertungen
- TYPIST BRAND GUIDES Rough DraftDokument16 SeitenTYPIST BRAND GUIDES Rough DraftDaniella OzairNoch keine Bewertungen
- How To Calibrate Your Equipment Using Color BarsDokument6 SeitenHow To Calibrate Your Equipment Using Color BarsAnirban GhoseNoch keine Bewertungen
- Standard recipe for printing pasteDokument3 SeitenStandard recipe for printing pasteRahmah IdrisNoch keine Bewertungen
- 2 Color in FoodDokument44 Seiten2 Color in FoodAbdul RahmanNoch keine Bewertungen
- Bresser NV 5x50 Digital Night VisionDokument5 SeitenBresser NV 5x50 Digital Night VisionSparklight JackNoch keine Bewertungen
- DD Exophthalmos-Buphthalmos-Proptosis PDFDokument3 SeitenDD Exophthalmos-Buphthalmos-Proptosis PDFsoff4ikaNoch keine Bewertungen
- Wissmach Glass Color Code Chart and Product ListDokument16 SeitenWissmach Glass Color Code Chart and Product Listrhye999100% (1)
- 2020-21 - Nicolas Gracia - Photography - Unit 6 CTDokument4 Seiten2020-21 - Nicolas Gracia - Photography - Unit 6 CTNicolas Gracia MachadoNoch keine Bewertungen
- Identification and Treatment of Retinopathy of Prematurity Update 2017Dokument9 SeitenIdentification and Treatment of Retinopathy of Prematurity Update 2017G VenkateshNoch keine Bewertungen
- DSP Lab6Dokument10 SeitenDSP Lab6Yakhya Bukhtiar KiyaniNoch keine Bewertungen
- Digital Image ProcessingDokument57 SeitenDigital Image ProcessingYatish ChutaniNoch keine Bewertungen
- Photo ListDokument1.320 SeitenPhoto ListViju RajuNoch keine Bewertungen
- Ultrasonography AssignmentDokument5 SeitenUltrasonography AssignmentAkshay VasishtaNoch keine Bewertungen
- Empowerment Module 5Dokument12 SeitenEmpowerment Module 5Josh TaguinodNoch keine Bewertungen
- SALAZAR, Bealyn F. (Art Appreciation Module #2)Dokument3 SeitenSALAZAR, Bealyn F. (Art Appreciation Module #2)Bealyn Fernandez SalazarNoch keine Bewertungen
- Presentation - Colors Combinations and HarmonyDokument97 SeitenPresentation - Colors Combinations and HarmonySunil TalekarNoch keine Bewertungen
- Compostion PDFDokument4 SeitenCompostion PDFIrene Cano100% (1)
- 10040-00-131-Es-0008-Att01 Color Coding Summary Table Color Coding SummaryDokument1 Seite10040-00-131-Es-0008-Att01 Color Coding Summary Table Color Coding SummarybassamNoch keine Bewertungen
- Art Elements and Principles ExplainedDokument29 SeitenArt Elements and Principles ExplainedAlexa Dela CruzNoch keine Bewertungen
- 6 Lovell PDFDokument20 Seiten6 Lovell PDFJavier Martinez Cañal100% (1)
- The Sunny 16 RuleDokument24 SeitenThe Sunny 16 Ruleangulilla100% (2)
- Human Eye MCQDokument4 SeitenHuman Eye MCQGowri Venkat0% (1)
- Visual Pathway & Binocular Vision GuideDokument36 SeitenVisual Pathway & Binocular Vision Guideamaliaramadhani100% (1)
- An Image-Based Bone Fracture Detection Using AForge LibraryDokument4 SeitenAn Image-Based Bone Fracture Detection Using AForge LibraryWaseem Abbas HashmiNoch keine Bewertungen
- Binocular Vision - Easier Than You ThinkDokument13 SeitenBinocular Vision - Easier Than You ThinkJorge CarcacheNoch keine Bewertungen
- Free DSLR Beginners GuideDokument18 SeitenFree DSLR Beginners GuideMichael Zhang56% (18)
- Interinstrument Variability in Hertel-Type ExophthalmometersDokument4 SeitenInterinstrument Variability in Hertel-Type ExophthalmometersPande GustianaNoch keine Bewertungen
- Raster Data Model: A Seminor OnDokument42 SeitenRaster Data Model: A Seminor OnAmber Joy TingeyNoch keine Bewertungen
- Olympic (Brand Guidelines) (2022)Dokument129 SeitenOlympic (Brand Guidelines) (2022)Eric DelobelNoch keine Bewertungen
- p7-s1 Transition Art Design 1Dokument26 Seitenp7-s1 Transition Art Design 1api-253929641Noch keine Bewertungen