Beruflich Dokumente
Kultur Dokumente
Sleeping Dif Culties in Relation To Depression and Anxiety in Elderly Adults
Hochgeladen von
Dian Isti AngrainiOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Sleeping Dif Culties in Relation To Depression and Anxiety in Elderly Adults
Hochgeladen von
Dian Isti AngrainiCopyright:
Verfügbare Formate
Sleeping dif culties in relation to depression and anxiety in elderly adults
LENA MALLON, JAN-ERIK BROMAN, JERKER HETTA
Mallon L, Broman J-E, Hetta J. Sleeping dif culties in relation to depression and anxiety in elderly adults. Nord J Psychiatry 2000;54:355 360. Oslo. ISSN 0803-9488. This study examines the prevalence of sleeping dif culties and their relationship to depression and anxiety in 1328 subjects aged 57 79 years by means of a questionnaire. Dif culties initiating sleep (DIS), dif culties maintaining sleep (DMS), early morning awakenings (EMA), and nightmares were assessed with The Uppsala Sleep Inventory (USI) and depression and anxiety with The Hospital Anxiety and Depression Scale (HAD scale). A total of 20.4% reported severe sleeping dif culties (DIS, DMS, or EMA), with a female preponderance. On the basis of the HAD scale we found that 3.4% ful lled the criteria for de nite depression and 10.1% ful lled the criteria for possible depression. The prevalence of de nite and possible pure anxiety (anxiety without depression) was 2.7% and 8.1%, respectively. There was no sex difference in reports of depression, but women more often reported pure anxiety. Altogether, 24.3% of the sample had either depression or anxiety. Nightmares were reported by 2.2% of the sample and associated with both depression and anxiety. We found that 39% of respondents with de nite depression and 45.2% with de nite pure anxiety reported sleeping dif culties. Depression emerged as the variable most consistently associated with sleeping dif culties when depression, pure anxiety, age, and sex were considered simultaneously. Habitual sleeping pill use was reported by 31.1% of the subjects with de nite depression, whereas only 24.4% received antidepressive medication. These ndings indicate that sleeping dif culties often are associated with psychiatric symptoms, especially depression. Anxiety, Depression, Elderly, Epidemiology, Sleeping dif culties. Lena Mallon, Psychiatric Clinic, Falun Hospital, SE-791 82 Falun, Sweden; Accepted: 19 July 1999.
ith advancing age there is an increase in sleeping dif culties and in the use of sleep medication, especially among women (1 3). Overall, from epidemiological surveys 15% 35% of elderly subjects report sleep problems (4 6). Sleeping dif culties are traditionally classi ed as dif culties initiating sleep (DIS), dif culties maintaining sleep (DMS), or early morning awakenings (EMA). Sleeping dif culties and nightmares have been found to be associated with both depression and anxiety (6 10). Estimates of the prevalence of depression among the elderly have been the focus of many studies, but there is a considerable variation in reported prevalence rates. In community-based surveys using different screening instruments the prevalence of depression generally varies between 10% and 17% (7, 11), whereas studies using the DSM criteria for major depression report lower prevalence rates, about 2% 8% (12 14). Anxiety has been thought to be less common among the elderly (15), but surveys (16 18) have found that anxiety disorders have a preva 2000 Taylor & Francis
lence rate of about 13% 18% among the elderly, similar to the rates of depression in the same populations. Methodological differences such as survey methods and diagnostic criteria may account for some of the variability in reported prevalence rates of depression and anxiety. One factor relevant to this discrepancy in the prevalence is the overlap between the two conditions. If a clinical state is characterized by both depression and anxiety, it is classi ed as depression, and anxiety is only diagnosed when depression is absent, the so-called hierarchical approach to diagnosis. Consequently, using the hierarchical approach in diagnosing will yield lower prevalence rates for anxiety than a non-hierarchical approach. It is still not clear how advancing age, sex, depression, and anxiety together might affect sleep. The aim of the present study was to assess the prevalence of sleeping dif culties and nightmares in elderly adults and investigate their association with depression and anxiety.
355
L M ALLON
ET AL.
Materials and Methods
Subjects
From the population register 1792 elderly adults, aged 57 79 years, were randomly selected from the County of Dalarna, Sweden, and asked to participate in a questionnaire survey. The study was performed in December 1995. The questionnaire was initially completed by 1117 subjects, and one reminder resulted in another 211 questionnaires. No signi cant differences were found in age, demographic characteristics, symptoms of depression, anxiety, or sleeping dif culties between early and late responders. The total response rate was 74.1%, and of the 1328 responders 623 were men and 705 were women. The mean age was about the same for men and women, 67 9 6 years versus 68 9 6 years.
The questionnaire
The questionnaire Sleep and Health consisted of 89 questions that covered demographic characteristics, sleep habits, sleeping dif culties, physical illnesses, symptoms of depression and anxiety, and medication. A description of the questionnaire has been published previously (19). In the present paper we investigated data concerning sleeping dif culties, depression, anxiety, and related medication usage. Sleeping dif culties were assessed by using questions from The Uppsala Sleep Inventory (USI), which has previously been used in studies to assess sleeping dif culties (20 22). Subjects were asked about dif culties initiating sleep (DIS), dif culties maintaining sleep (DMS), and early morning awakenings (EMA), and the questions were to be answered on a ve-point scale (1 no problems, 2 minor problems, 3 moderate problems, 4 severe problems, and 5 very severe problems). For the current analyses scores of 4 and 5 were considered to represent complaints, and sleeping dif culties were de ned as complaints of DIS, DMS, or EMA. Subjects were asked about nightmares and sleeping pill usage, and these questions were also to be answered on a ve-point scale (1 never, 2 seldom, 3 sometimes, 4 often, and 5 very often). Responders were classi ed as having nightmares or being habitual sleeping pill users if they reported nightmares or usage often or very often (scores of 4 and 5). There was also an open-ended question about the use of medication. Depression and anxiety were assessed by using the Hospital Anxiety and Depression Scale (HAD scale). This is a self-rating scale in which the overall severity of depression and anxiety is rated on a four-point scale (0 to 3). Seven questions are related to depression (HADD) and seven to anxiety (HAD-A), both with a score range of 0 21. The items of the scale have been chosen so as to be in uenced as little as possible by concomi-
tant physical illness, and the depression subscale does not include sleeping dif culties. Zigmond & Snaith (23) have recommended two cut-off points: 8 for possible cases and 11 for de nite cases. The HAD scale has been shown to be a reliable instrument for screening depression and anxiety (24 26). When assessing the prevalence of depression and anxiety, scores of 8 10 on either subscale were de ned as possible cases of depression or anxiety, and scores of 11 and more on either subscale as de nite cases of depression or anxiety. We also assessed the prevalence of anxiety without depression, so-called pure anxiety and de ned this as having scores of 0 7 on the HAD-D and scores of 8 10 (possible cases of pure anxiety) or ] 11 (de nite cases of pure anxiety) on the HAD-A. To test the validity of the two HAD subscales, factor analysis was conducted. The analysis yielded two factors (eigenvalue \ 1.0), corresponding to the HAD-A and HAD-D. All items were loading on the appropriate factor, except one item, which was found to load on both factors. The Cronbach alpha was 0.83 for HAD-A and 0.73 for HAD-D.
Procedure
A questionnaire, a stamped, addressed envelope, and a letter explaining the purpose of the study were mailed to each subject. Subjects were encouraged to call the investigator if they had any questions. Full anonymity protection was ensured. The study protocol was approved by the Ethics Committee of the Faculty of Medicine at Uppsala University in Sweden.
Statistical analysis
The statistical analyses were performed on a Macintosh computer, using the statistical analysis program SPSS 6.1. Standard methods have been used to calculate mean values and standard deviations. For comparison between categorical variables the chi-square test was used. The in uence of multiple variables was analysed using multiple logistic regression analysis, and the results are presented as an adjusted odds ratio (OR) with 95% con dence interval (95% CI). The P B0.05 level was adopted as a reference point for considering results to be statistically signi cant.
Results
Prevalence of sleeping dif culties, depression, and anxiety
Table 1 presents the prevalence of sleeping dif culties, nightmares, depression, and anxiety by sex. Of the total sample 8.0% reported DIS, 10.4% DMS, and 12.1% EMA. Altogether, 20.4% reported sleeping dif culties de ned as having DIS, DMS, or EMA. There was a female preponderance in reports of DIS and in having sleeping dif culties. Having nightmares was reported by
NORD J PSYCHIATRY VOL 54 NO 5 2000
356
SLEEPIN G
DIFF ICULTIES IN ELDERLY
2.2% of the respondents, with no sex difference. The criterion level indicating de nite depression was ful lled by 3.4% of the sample, and that of possible depression by 10.1%. The corresponding gures for de nite and possible anxiety were 6.6% and 11.6%, respectively. We also investigated the prevalence of pure anxiety and included only subjects with anxiety but without depression. In accordance with these criteria, 2.7% ful lled the criteria for de nite pure anxiety and 8.1% the criteria for possible pure anxiety. There was no sex difference in reports of depression, but women more often reported both anxiety and pure anxiety.
15.3% had sleeping dif culties, and the corresponding gure for de nite cases of pure anxiety was 45.2% (chi-square 31.8; PB 0.001). Table 3 summarizes the results of multiple logistic regression analyses to determine the independent association of de nite depression, de nite pure anxiety, sex, and age with sleeping dif culties and nightmares. The data showed that de nite depression was signi cantly and independently associated with DIS, DMS, EMA, and nightmares, whereas de nite pure anxiety was associated with DIS and nightmares. Female sex was a signi cant predictor of DIS, whereas older age did not give rise to increased odds in any of the variables.
Sleeping dif culties and their relation to depression and anxiety
In the following analyses we included only subjects with pure anxiety when evaluating anxiety. In Table 2 it can be seen that the most common sleeping dif culty for subjects with de nite depression was EMA, 33.3%, whereas the most common problem for subjects with de nite pure anxiety was DIS, 22.9%. Subjects with possible depression or possible pure anxiety more often reported DIS, DMS, and EMA than non-subjects. However, there was no signi cant difference in any of the sleeping dif culties between possible and de nitive cases of depression and pure anxiety. Having nightmares, habitual use of sleeping pills, and use of antidepressants were all more often reported in de nite cases of depression than in possible cases of depression. De nite cases of pure anxiety reported more often nightmares than possible cases of pure anxiety. Moreover, of the non-depressed, 17.2% reported sleeping dif culties, and of the de nite cases of depression 39.0% reported sleeping dif culties (chi-square 31.1; P B0.001). Of subjects without pure anxiety
Discussion
The rst main nding of the present study was that the prevalence of severe sleeping dif culties was 20.4%, with a female preponderance. The second main nding was that, on the basis of the HAD scale, 24.3% had either depression or anxiety. The third important nding was that depression emerged as the variable most consistently associated with sleeping dif culties. With an almost 75% response rate and with the same age and sex distribution among the responders as in the population in the county of Dalarna at the time of the study (27), we consider our results to be representative and valid with regard to sex and age characteristics. However, it seems quite plausible that the most disabled elderly adults are overrepresented among non-responders. Thus, our reported rates of morbidity may be somewhat underestimated. One main nding in the present study was that the point prevalence of sleeping dif culties was 20.4% when de ning sleeping dif culties as severe or very severe
Table 1. Prevalence (in percentage) of sleeping dif culties, depression, and anxiety in men and women.
Variable* DIS DMS EMA Sleeping dif culties Nightmares Depression De nite Possible Anxiety De nite Possible Pure anxiety De nite Possible Total (n1328) 8.0 10.4 12.1 20.4 2.2 3.4 10.1 6.6 11.6 2.7 8.1 Men (n 623) 4.7 9.4 12.4 17.5 2.0 2.9 8.8 3.4 6.8 1.5 4.9 Women (n705) 10.9 11.3 11.9 23.2 2.4 3.9 11.3 9.4 16.0 4.7 13.6 Chi-square test, P value B0.001 NS NS B0.05 NS NS NS B0.001 B0.001 B0.01 B0.001
* DIS dif culties initiating sleep; DMSdif culties maintaining sleep; EMAearly morning awakenings; Sleeping dif culties DIS, DMS, or EMA; de nite depression HAD-D score ]11; possible depression, HAD-D score 810; de nite anxiety, HAD-A score ]11; possible depression, HAD-A score 810; de nite pure anxiety, HAD-D score 07 and HAD-A ]11; and possible pure anxiety, HAD-D score 07 and HAD-A score 810.
NORD J PSYCHIATRY VOL 54 NO 5 2000
357
L M ALLON
ET AL.
Table 2. Prevalence (in percentage) of sleeping dif culties and related variables in relation to depression and pure anxiety.
Depression Nondepressed (N) 6.4 8.7 10.0 1.8 4.2 2.5 Possible depression (P) 15.8 18.3 23.4 2.3 15.8 9.7 De nite depression (D) 20.0 28.6 33.3 11.4 31.1 24.4 Nonanxiety (N) 5.0 7.7 8.7 1.2 2.8 1.6 Pure anxiety Possible pure anxiety (P) 14.2 14.7* 17.7 2.8 15.0 9.3 De nite pure anxiety (D) 22.9 18.2 21.9 17.1 11.4 8.3
Variable DIS DMS EMA Nightmares Sleeping pills Antidepressants
Total 8.0 10.4 12.1 2.2 6.3 4.1
Difference between N and P: * PB0.05, PB0.01, P B0.001; difference between P and D: PB0.05, PB0.01, PB0.001. DIS dif culties initiating sleep; DMSdif culties maintaining sleep; EMAearly morning awakenings. Non-depressed HAD-D score 07; possible depression HAD-D score 810; de nite depression HAD-D score ]11. Non- anxiety HAD-D score 07 and HAD-A score 07, possible pure anxiety HAD-D score 07 and HAD-A score 810, de nite pure anxiety HAD-D score 07 and HAD-A ]11.
problems with DIS, DMS, or EMA. Studies using relatively narrow criteria in the de nition of sleeping dif culties, like ours, have reported similar prevalence rates: 18% 22% (8, 28, 29). As a screening instrument for depression and anxiety we used the HAD scale, which was developed to detect emotional disturbances among physically ill patients (23). We found that the prevalence of at least possible depression was 13.5%, and the prevalence of at least possible pure anxiety was 10.8%. The prevalence of both disorders together was 24.3% that is, about onefourth of elderly adults had either depression or anxiety. In this study 3.4% ful lled the criteria for de nite depression, and 10.1% the criteria for possible depression, the latter re ecting milder forms of depressive symptoms. Our prevalence rate of de nite depression in accordance with the HAD scale is similar to prevalence rates of depressive disorders based on the DSM classi cation reported from community surveys (13, 14). Studies assessing the prevalence of depression using other screening instruments generally report higher prevalence rates, 10% 39% (7, 11, 18, 30). In our survey 6.6% ful lled the criteria for de nite anxiety, and 11.6% ful lled the criteria for possible anxiety, most common among women. These ndings show that symptoms of anxiety are common among elderly adults. The prevalence rate of at least possible anxiety (18.2%) in the present survey is similar to community surveys among elderly, where anxiety is measured without hierarchical rules (16 18). When we applied a hierarchical procedure and excluded possible cases of depression, the prevalence rates of de nite and possible pure anxiety were 2.7% and 8.1%, respectively. In other studies using hierarchical rules among subjects aged 65 or more, the prevalence of anxiety range between 4% and 10% (31, 32). Disturbed sleep is a core symptom of both depression and anxiety disorders (33, 34), and sleeping dif culties
are common in the depressed elderly (7, 35). In a longitudinal study of elderly subjects (36) depression was related positively to sleep disturbance even when age, sex, and health status were considered simultaneously, and early morning awakening was the sleep symptom most consistently associated with depression. In the present study we found that severe sleeping dif culties were about twice as common in subjects with de nite depression as in the non-depressed. Furthermore, depression was strongly associated with sleeping dif culties and nightmares.
Table 3. Variables related to sleeping dif culties and nightmares, analysed by using multiple logistic regression analyses.
Dependent variable DIS Independent variable* Depression Pure anxiety Female Age Depression Pure anxiety Female Age Depression Pure anxiety Female Age Depression Pure anxiety Female Age OR (95% CI) 3.2 3.4 2.3 1.1 3.7 2.1 1.2 0.9 4.1 2.3 0.9 1.1 8.9 15.0 0.9 0.9 (1.57.1) (1.57.8) (1.43.6) (0.91.4) (1.97.6) (0.85.1) (0.81.7) (0.81.1) (2.18.0) (0.95.5) (0.61.3) (0.91.2) (3.125.4) (5.441.8) (0.42.1) (0.61.2) P value B0.01 B0.01 B0.001 NS B0.001 NS NS NS B0.001 NS NS NS B0.001 B0.001 NS NS
DMS
EMA
Nightmares
DIS dif culties initiating sleep; DMSdif culties maintaining sleep, EMAearly morning awakenings. * The independent variables examined are de nite depression, de nite pure anxiety, female sex, and age (in 5-year strata). The results are presented as an adjusted OR with 95% CI. OR odds ratio; CI con dence interval. OR calculated for a 5-year increase in age.
NORD J PSYCHIATRY VOL 54 NO 5 2000
358
SLEEPIN G
DIFF ICULTIES IN ELDERLY
Epidemiological data also support linkage between sleep disturbances and anxiety in the elderly (6, 8). In the present study severe sleeping dif culties were about 2.8 times as common in subjects with de nite pure anxiety as in those without anxiety. In our study pure anxiety was related to DIS and nightmares when age, sex, depression, and pure anxiety were considered simultaneously. A considerably high percentage of de nite cases of depression, 31.1%, used sleeping pills habitually. This nding emphasizes the need to keep depression in mind when evaluating sleeping dif culties among elderly adults. Moreover, it is noteworthy that only 24.4% of subjects with de nite depression received antidepressive medication. A similarly low gure has been reported by Skoog et al. (37), who found that among 85-year-olds in Goteborg, Sweden, 19.4% of those with any depres sive disorder received antidepressant medication. Livingston et al. (7) also found that only 13% of depressives were receiving antidepressants of subjects aged 65 and more in London. These ndings indicate that depression, for the most part, is untreated among the elderly. Because our study is cross-sectional we cannot establish any cause-and-effect relationship. It might be argued that it is a shortcoming that our sleep data are based only on self-reports of disturbed sleep. However, subjective data have been found to be largely consistent with polysomnographic ndings (38 40), and subjective complaints are particularly relevant because they re ect the persons beliefs and attitudes about sleep, and these conceptions decide whether the person seeks professional help or advice (41). In conclusion, about one- fth of elderly adults reported severe sleeping dif culties, about one-forth had depression or anxiety, and depression emerged as the variable most consistently associated with sleeping dif culties.
AcknowledgementsThis study was supported nancially by the Swedish Medical Research Council (Project 06869), the Dalarna Research Institute, the Swedish Psychiatric Association, the Marta and Nicke Nasvells Foundation, and the Swedish Lundbeck Foundation.
References
1. Karacan I, Thornby JI, Williams RL. Sleep disturbance: a community survey. In: Guilleminault C, Lugaresi E, editors. Sleep:wake disorders: natural history, epidemiology and longterm evolution. New York: Raven Press; 1983. p. 37 60. 2. Welstein L, Dement WC, Redington D, Guilleminault C, Mitler MM. Insomnia in the San Francisco Bay area: a telephone survey. In: Guilleminault C, Lugaresi E, editors. Sleep: wake disorders: natural history, epidemiology and long-term evolution. New York: Raven Press; 1983. p. 73 85. 3. Ohayon M. Epidemiogical study on insomnia in the general population. Sleep 1996;19:7 15. 4. Maggi S, Langlois JA, Minicuci N, et al. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. J Am Geriatr Soc 1998;46:161 8. 5. Gislason T, Reynisdottir H, Kristbjarnarson H, Benediktsdottir B. Sleep habits and sleep disturbances among elderly an epidemiological survey. J Intern Med 1993;234:31 9.
6. Henderson S, Jorm AF, Mackinnon AJ, Christensen H, Korten AE. Insomnia in the elderly: Its prevalence and correlates in the general population. Med J Aust 1995;162:22 4. 7. Livingston G, Hawkins A, Graham N, Blizard B, Mann A. The Gospel Oak Study: prevalence rates of dementia, depression and activity limitation among elderly residents in Inner London. Psychol Med 1990;20:137 46. 8. Morgan K, Dallasso H, Ebrahim S, Arie T, Fentem PH. Characteristics of subjective insomnia in the elderly living at home. Age Ageing 1988;17:1 7. 9. Morin CM, Gramling SE. Sleep patterns and aging: Comparisons of older adults with and without insomnia complaints. Psychol Aging 1989;4:290 4. 10. Ohayon MM, Morselli PL, Guilleminault C. Prevalence of nightmares and their relationship to psychopathology and daytime functioning in insomnia subjects. Sleep 1997;20:340 8. 11. Kennedy GJ, Kelman HR, Thomas C. Persistence and remission of depressive symptoms in late life. Am J Psychiatry 1991;148:174 8. 12. Palsson S, Skoog I. The epidemiology of affective disorders in the elderly: a review. Int Clin Psychopharmacol 1997;12:3 13. 13. Bland RC, Newman SC, Orn H. Prevalence of psychiatric disorders in the elderly in Edmonton. Acta Psychiatr Scand 1988;338:57 63. 14. Lobo A, Saz P, Marcos G, Dia J-L, De-la-Camara C. The prevalence of dementia and depression in the elderly community in a southern European population. The Zaragoza Study. Arch Gen Psychiatry 1995;52:497 506. 15. Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry 1994;151:640 9. 16. Lindesay J, Briggs K, Murphy E. The Guys:Age Concern survey: prevalence rates of cognitive impairment, depression and anxiety in an urban elderly community. Br J Psychiatry 1989;155:317 29. 17. Manela M, Katona C, Livingston G. How common are the anxiety disorders in old age? Int J Geriatr Psychiatry 1996;11:65 70. 18. Kirby M, Bruce I, Radic A, Coakley D, Lawlor BA. Mental disorders among the community-dwelling elderly in Dublin. Br J Psychiatry 1997;171:369 72. 19. Mallon L, Hetta J. A survey of sleep habits and sleeping dif culties in an elderly Swedish population. Upsala J Med Sci 1997;102:185 97. 20. Gislason T, Almqvist M. Somatic diseases and sleep complaints: an epidemiological study of 3201 Swedish men. Acta Med Scand 1987;221:475 81. 21. Liljenberg B, Almqvist M, Hetta J, Roos B, Agren H. Age and prevalence of insomnia in adulthood. Eur J Psychiatry 1989;3:5 12. 22. Lindberg E, Janson C, Gislason T, Svardsudd C, Hetta J, Bo man G. Snoring and hypertension a 10-year follow-up. Eur Resp J 1998;11:884 9. 23. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361 70. 24. Hopewood P, Howell A, Maguire P. Screening for psychiatric morbidity in patients with advanced breast cancer: validation of two self-report questionnaires. Br J Cancer 1991;64:353 6. 25. Wilkinson M, Barczak P. Psychiatric screening in general practise: comparison of the General Health Questionnaire and the Hospital Anxiety Depression Scale. J R Coll Gen Pract 1988;38:311 3. 26. Upadhyaya AK, Stanley I. Detection of depression in primary care: comparison of two self-administered scales. Int J Geriatr Psychiatry 1997;12:35 7. 27. Swedish National Central Bureau of Statistics. Yearbook 1995 (Statistisk Arsbok). Stockholm: The Bureau; 1996. 28. Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Arch Gen Psychiatry 1985;42:225 32. 29. Ganguli M, Reynolds CF, Gilby JE. Prevalence of sleep complaints in a rural older community sample: the MoVIS projects. J Am Geriatr Soc 1996;44:778 84. 30. Kivela S-L, Pahkala K, Tervo R-R. Prevalence of depressive symptoms among an elderly Finnish population. Nord J Psychiatry 1986;40:45 50. 31. Larkin BA, Copeland JRM, Dewey ME, et al. The natural history of neurotic disorder in an elderly urban population: ndings from the Liverpool longitudinal study of continuing health in the community. Br J Psychiatry 1992;60:681 6.
NORD J PSYCHIATRY VOL 54 NO 5 2000
359
L M ALLON
ET AL.
32. Ulenhuth EH, Balter MB, Mellinger GD, Cisin IH, Clinthorne J. Symptom checklist syndromes in the general population: Correlations and psychotherapeutic drug use. Arch Gen Psychiatry 1983;40:1167 73. 33. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. (DSM-IV), Washington (DC): American Psychiatric Association; 1994. 34. World Health Organization. The ICD-10 classi cation of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. 35. Brabbins CJ, Dewey ME, Copeland RM, et al. Insomnia in the elderly: prevalence, gender differences and relationships with morbidity and mortality. Int J Geriatr Psychiatry 1993;8:473 80. 36. Rodin J, McAvay G, Timko C. A longitudinal study of depressed mood and sleep disturbances in elderly adults. J Gerontol 1988;43:45 53. 37. Skoog I, Nilsson L, Landahl S, Steen B. Mental disorders and
38. 39.
40. 41.
the use of psychotropic drugs in an 85-year old urban population. Int Psychogeriatr 1993;5:33 48. Hoch CC, Reynolds CF, Kupfer DJ, Berman SR, Houck PR, Starck JA. Empirical note: self-reports versus recorded sleep in helthy seniors. Psychophysiology 1987;24:293 9. Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quanti cation of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 1991;14:331 8. Trinder J. Subjective insomnia without objective ndings: a pseudo diagnostic classi cation. Psychol Bull 1988;103:87 94. Webb W. Age-related changes in sleep. Clin Geriatric Med 1989;5:259 74.
Lena Mallon, M.D.; Jan-Erik Broman, Dr. Med. Sci.; and Jerker Hetta, M.D., Ph.D., Sleep Disorders Unit, Department of Neuroscience, Psychiatry, University Hospital, SE-751 85 Uppsala, Sweden.
360
NORD J PSYCHIATRY VOL 54 NO 5 2000
Das könnte Ihnen auch gefallen
- Sleep Disorders in Selected Psychiatric Settings: A Clinical CasebookVon EverandSleep Disorders in Selected Psychiatric Settings: A Clinical CasebookImran S. KhawajaNoch keine Bewertungen
- Complementary and Alternative Medical Lab Testing Part 12: NeurologyVon EverandComplementary and Alternative Medical Lab Testing Part 12: NeurologyNoch keine Bewertungen
- Comorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFDokument24 SeitenComorbid Anxiety and Depression - Epidemiology, Clinical Manifestations, and Diagnosis PDFdreaming0% (1)
- Barrett Impulsiveness Scale (BIS-11)Dokument10 SeitenBarrett Impulsiveness Scale (BIS-11)andr3yl0Noch keine Bewertungen
- Apego Transgeneracional y AnorexiaDokument9 SeitenApego Transgeneracional y AnorexiaadriNoch keine Bewertungen
- 1 s2.0 S152550502300135X MainDokument8 Seiten1 s2.0 S152550502300135X MainilonaskorinNoch keine Bewertungen
- A Survey of Sleep Habits and Sleeping Difficulties in An Elderly Swedish PopulationDokument14 SeitenA Survey of Sleep Habits and Sleeping Difficulties in An Elderly Swedish PopulationPriyanshuNoch keine Bewertungen
- Epidemiology of Insomnia: Prevalence and Risk FactorsDokument22 SeitenEpidemiology of Insomnia: Prevalence and Risk Factorsshf.mxlikNoch keine Bewertungen
- Prevalence of Psychiatric Disorders in Infertile Women and Men Undergoing in Vitro Fertilization TreatmentDokument8 SeitenPrevalence of Psychiatric Disorders in Infertile Women and Men Undergoing in Vitro Fertilization TreatmentMaria Galia Elias QuirogaNoch keine Bewertungen
- Ansiedad y DepresionDokument21 SeitenAnsiedad y DepresionEdgar AvilésNoch keine Bewertungen
- 2011 - IJCHP - The Leyton Obsessional Inventory-Child VersionDokument16 Seiten2011 - IJCHP - The Leyton Obsessional Inventory-Child VersionEsteysi Villarroel BernalesNoch keine Bewertungen
- Demencia en Gente Muy MayorDokument6 SeitenDemencia en Gente Muy MayorJimenaNoch keine Bewertungen
- Anxiety Disorders Among Adolescents Referred To General Psychiatry For Multiple Causes: Clinical Presentation, Prevalence, and ComorbidityDokument10 SeitenAnxiety Disorders Among Adolescents Referred To General Psychiatry For Multiple Causes: Clinical Presentation, Prevalence, and ComorbidityRatu CalistaNoch keine Bewertungen
- Research Articles: Childhood Adversity and Vulnerability To Mood and Anxiety DisordersDokument7 SeitenResearch Articles: Childhood Adversity and Vulnerability To Mood and Anxiety DisordersMifta 'hera' Khaerati IINoch keine Bewertungen
- Cannabis Paper 2Dokument6 SeitenCannabis Paper 2Carlos Eduardo Jorquera GonzálezNoch keine Bewertungen
- C SCL-90: Onfiabilidad Y Validez DE LA EN LA Evaluación DE Psicopatología EN MujeresDokument9 SeitenC SCL-90: Onfiabilidad Y Validez DE LA EN LA Evaluación DE Psicopatología EN MujeresGarcía JuanNoch keine Bewertungen
- Cancer Information Overload and Death Anxiety Predict Health AnxietyDokument8 SeitenCancer Information Overload and Death Anxiety Predict Health AnxietyRobynNoch keine Bewertungen
- Lehtinen 1994Dokument4 SeitenLehtinen 1994HARINI KNoch keine Bewertungen
- Anxiety Disorder Symptoms in Children and Adolescents: Differences by Age and Gender in A Community SampleDokument6 SeitenAnxiety Disorder Symptoms in Children and Adolescents: Differences by Age and Gender in A Community SampleJesús Rafael Méndez NateraNoch keine Bewertungen
- Barlow Et Al 1984Dokument19 SeitenBarlow Et Al 1984290971Noch keine Bewertungen
- Swinkels PscychopathologieDokument16 SeitenSwinkels PscychopathologiesezalwickNoch keine Bewertungen
- Rosario V-1 - Agosto20Dokument8 SeitenRosario V-1 - Agosto20Lupita LópezNoch keine Bewertungen
- Behavioral and Emotional Effects of Repeated General Anesthesia in Young ChildrenDokument1 SeiteBehavioral and Emotional Effects of Repeated General Anesthesia in Young ChildrenRogger MagallanesNoch keine Bewertungen
- Depression, Alzheimer, Family CaregiversDokument13 SeitenDepression, Alzheimer, Family CaregiversCathy Georgiana HNoch keine Bewertungen
- An Investigation of Irrational Beliefs and Death Anxiety As A Function of Hiv StatusDokument18 SeitenAn Investigation of Irrational Beliefs and Death Anxiety As A Function of Hiv StatusDana PascuNoch keine Bewertungen
- Affective DisordersDokument37 SeitenAffective Disordersveronicaine91Noch keine Bewertungen
- Anxiety Symptoms in Adolescents at RiskDokument5 SeitenAnxiety Symptoms in Adolescents at RiskifclarinNoch keine Bewertungen
- Anxiety and Depression Are Risk Factors Rather Than Consequences of Functional Somatic Symptoms in A General Population of Adolescents - The TRAILS StudyDokument9 SeitenAnxiety and Depression Are Risk Factors Rather Than Consequences of Functional Somatic Symptoms in A General Population of Adolescents - The TRAILS StudyJPCP 2014Noch keine Bewertungen
- Depressive Disorders in Epilepsy: SummaryDokument4 SeitenDepressive Disorders in Epilepsy: SummaryRadi PdNoch keine Bewertungen
- Suicidal Intension Among Depresssion pts.-1Dokument18 SeitenSuicidal Intension Among Depresssion pts.-1Firdouse ShajiNoch keine Bewertungen
- Identification and Pychological Treament of Adolescent Panic Disorder 2020Dokument8 SeitenIdentification and Pychological Treament of Adolescent Panic Disorder 2020Almudena RodriguezNoch keine Bewertungen
- Álvarez Et Al (2011) ChildabuseDokument6 SeitenÁlvarez Et Al (2011) ChildabuseAra Moreno EscaladaNoch keine Bewertungen
- Anxiety and Mood Disorders in Narcolepsy: A Case - Control StudyDokument8 SeitenAnxiety and Mood Disorders in Narcolepsy: A Case - Control StudyDesyifa Annisa MursalinNoch keine Bewertungen
- Prev Ans Depr CanverDokument6 SeitenPrev Ans Depr CanverÉrico AugustoNoch keine Bewertungen
- Kurre 2012 - Gender Perceived Disability Anxiety Depression 1472-6815-12-2Dokument12 SeitenKurre 2012 - Gender Perceived Disability Anxiety Depression 1472-6815-12-2Ikhsan JohnsonNoch keine Bewertungen
- Duration of Depressive Symptoms and Mortality Risk The English Longitudinal Study of Ageing ElsaDokument6 SeitenDuration of Depressive Symptoms and Mortality Risk The English Longitudinal Study of Ageing ElsaAishwarya PuttaNoch keine Bewertungen
- Art 3A10.1007 2Fs10862 011 9224 yDokument8 SeitenArt 3A10.1007 2Fs10862 011 9224 yastrimentariNoch keine Bewertungen
- 4 Gotlib2014Dokument18 Seiten4 Gotlib2014Javiera Luna Marcel Zapata-SalazarNoch keine Bewertungen
- Ansiedad Comorbilidad en Epi KannerDokument2 SeitenAnsiedad Comorbilidad en Epi Kannerkarina fontanezNoch keine Bewertungen
- Marital Status and Risk For Late LifeDokument13 SeitenMarital Status and Risk For Late LifeHargo PsyNoch keine Bewertungen
- Depression in Children AdolescentsDokument7 SeitenDepression in Children AdolescentstoddhavelkaNoch keine Bewertungen
- Suicide Epilepsy CohortDokument10 SeitenSuicide Epilepsy CohortDiana SelaruNoch keine Bewertungen
- JournalDokument6 SeitenJournalWisnu AdhanantyoNoch keine Bewertungen
- Original Paper Comorbidity of Epilepsy and Depression in Al Husseini Teaching Hospital in Holy Kerbala /iraq in 2018Dokument9 SeitenOriginal Paper Comorbidity of Epilepsy and Depression in Al Husseini Teaching Hospital in Holy Kerbala /iraq in 2018sarhang talebaniNoch keine Bewertungen
- Psychiatric Comorbidities Among Adolescents With and Without Anxiety Disorders: A Community StudyDokument6 SeitenPsychiatric Comorbidities Among Adolescents With and Without Anxiety Disorders: A Community StudyLiliana PonteNoch keine Bewertungen
- Yahia2013 Article PredictorsOfAnxietyAndDepressiDokument6 SeitenYahia2013 Article PredictorsOfAnxietyAndDepressiamasoud96 amasoud96Noch keine Bewertungen
- Prevalence and Predictors of Depression Amongst ElderlyDokument4 SeitenPrevalence and Predictors of Depression Amongst ElderlyDr.Wajid Habib (Doxxsab)Noch keine Bewertungen
- Antipsychotic Medication Induced Movement Disorders: The Case of Amanuel Specialized Mental Hospital, Addis Ababa, EthiopiaDokument7 SeitenAntipsychotic Medication Induced Movement Disorders: The Case of Amanuel Specialized Mental Hospital, Addis Ababa, Ethiopiael egendNoch keine Bewertungen
- Schizophr Bull 1994 Gordon 697 712Dokument16 SeitenSchizophr Bull 1994 Gordon 697 712EdwardVargasNoch keine Bewertungen
- Alfano, Ginsburg, & Kingery (2007) SleepDokument9 SeitenAlfano, Ginsburg, & Kingery (2007) SleepJanuaryska SaraswatiNoch keine Bewertungen
- Do Different Orthodontic Malocclusions Affect Patients' Self-Concept and Psychosocial Status?Dokument4 SeitenDo Different Orthodontic Malocclusions Affect Patients' Self-Concept and Psychosocial Status?Claypella MaskNoch keine Bewertungen
- Correlatos Del Maltrato Físico en La Infancia en Mujeres Adultas Con Trastorno Distímico o Depresión MayorDokument8 SeitenCorrelatos Del Maltrato Físico en La Infancia en Mujeres Adultas Con Trastorno Distímico o Depresión MayormagdaNoch keine Bewertungen
- Content ServerDokument11 SeitenContent ServerTriismyNoch keine Bewertungen
- Definition of InsomniaDokument10 SeitenDefinition of Insomniaeka yusrianaNoch keine Bewertungen
- 87-5 Retardasi MentalDokument7 Seiten87-5 Retardasi MentalShalawatyAbdkarimNoch keine Bewertungen
- Psychopharmacology of AutismDokument17 SeitenPsychopharmacology of AutismMichelle2Noch keine Bewertungen
- Chang 2018Dokument14 SeitenChang 2018spaciugNoch keine Bewertungen
- Visual Height Intolerance and Acrophobia: Distressing Partners For LifeDokument8 SeitenVisual Height Intolerance and Acrophobia: Distressing Partners For LifeAnonymous OCVES8U7Noch keine Bewertungen
- Social Science & Medicine: ReviewDokument17 SeitenSocial Science & Medicine: ReviewNabellaNoch keine Bewertungen
- The Developmental Epidemiology of Anxiety Disorders Phenomenology, Prevalence, and ComorbityDokument18 SeitenThe Developmental Epidemiology of Anxiety Disorders Phenomenology, Prevalence, and ComorbityShirleuy GonçalvesNoch keine Bewertungen
- Resveratrol and Glucose ControlDokument10 SeitenResveratrol and Glucose ControlDian Isti AngrainiNoch keine Bewertungen
- Breastfeeding en Women WorkDokument7 SeitenBreastfeeding en Women WorkDian Isti AngrainiNoch keine Bewertungen
- Resveratrol and CA ColonDokument6 SeitenResveratrol and CA ColonDian Isti AngrainiNoch keine Bewertungen
- Jurnal-3-Naskah 5 JURNAL PDGI Vol 59 No 1Dokument5 SeitenJurnal-3-Naskah 5 JURNAL PDGI Vol 59 No 1Bruno Adiputra Patut IINoch keine Bewertungen
- Epilepsi JaksonDokument1 SeiteEpilepsi JaksonDian Isti AngrainiNoch keine Bewertungen
- All About InjectionDokument24 SeitenAll About InjectionDian Isti AngrainiNoch keine Bewertungen
- Poststroke EpilepsyDokument5 SeitenPoststroke EpilepsyDian Isti AngrainiNoch keine Bewertungen
- Poststroke EpilepsyDokument5 SeitenPoststroke EpilepsyDian Isti AngrainiNoch keine Bewertungen
- Seizstroke in ChildDokument6 SeitenSeizstroke in ChildDian Isti AngrainiNoch keine Bewertungen
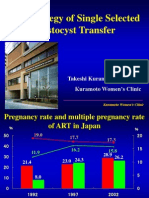
- The Strategy of Single Selected Blastocyst Transfer: Takeshi Kuramoto MD, PHD Kuramoto Women'S ClinicDokument43 SeitenThe Strategy of Single Selected Blastocyst Transfer: Takeshi Kuramoto MD, PHD Kuramoto Women'S ClinicDian Isti AngrainiNoch keine Bewertungen
- Malnutrition Elderly Quick Ref GuideDokument4 SeitenMalnutrition Elderly Quick Ref GuideDian Isti AngrainiNoch keine Bewertungen
- Jurnal PDFDokument10 SeitenJurnal PDFNayda FitrinaNoch keine Bewertungen
- 11821116Dokument10 Seiten11821116Dian Isti AngrainiNoch keine Bewertungen
- 1949 Winnicott Hate in The CountertransferenceDokument10 Seiten1949 Winnicott Hate in The CountertransferenceKevin McInnes100% (1)
- Name M Jalil Khan Reg No Bscn02161014 NCP (Insomnia) Assessment Diagnosis Planning Intervention Rational Evaluation Short TermDokument2 SeitenName M Jalil Khan Reg No Bscn02161014 NCP (Insomnia) Assessment Diagnosis Planning Intervention Rational Evaluation Short TermNargis MughalNoch keine Bewertungen
- Product Details: Medicine Mcqs For Medical Professionals PDFDokument2 SeitenProduct Details: Medicine Mcqs For Medical Professionals PDFUtkarsh SharmaNoch keine Bewertungen
- Spitzer, R. L. Et Al (2006) A Brief Measure For Assessing Generalized Anxiety Disorder - The GAD-7Dokument6 SeitenSpitzer, R. L. Et Al (2006) A Brief Measure For Assessing Generalized Anxiety Disorder - The GAD-7Kristopher MacKenzie BrignardelloNoch keine Bewertungen
- Assignment 40Dokument27 SeitenAssignment 40vasisth50Noch keine Bewertungen
- Annotated BibDokument6 SeitenAnnotated Bibapi-194035532Noch keine Bewertungen
- STOP, LOOK, AND LISTEN: The Challenge For Children With ADHDDokument13 SeitenSTOP, LOOK, AND LISTEN: The Challenge For Children With ADHDJFNoch keine Bewertungen
- Artigos Aaron BeckDokument32 SeitenArtigos Aaron BeckstragusrjNoch keine Bewertungen
- Donna Williams Interview PDFDokument8 SeitenDonna Williams Interview PDFDiego Yonathan Moreno RamirezNoch keine Bewertungen
- Substance Abuse Group ProjectDokument9 SeitenSubstance Abuse Group Projectapi-253915117Noch keine Bewertungen
- Pitman 2002 Biological-PsychiatryDokument4 SeitenPitman 2002 Biological-PsychiatryQwerty QwertyNoch keine Bewertungen
- NICHQ Vanderbilt Teacher RatingDokument3 SeitenNICHQ Vanderbilt Teacher RatingJanine Erica De LunaNoch keine Bewertungen
- A Mental Healthcare Model For Mass Trauma Survivors - M. Basoglu, Et. Al., (Cambridge, 2011) WW PDFDokument296 SeitenA Mental Healthcare Model For Mass Trauma Survivors - M. Basoglu, Et. Al., (Cambridge, 2011) WW PDFraulNoch keine Bewertungen
- PAAM LecturesDokument167 SeitenPAAM LecturesekyecNoch keine Bewertungen
- Attachment Trauma and Multiplicity Working With Dissociative Identity DisorderDokument241 SeitenAttachment Trauma and Multiplicity Working With Dissociative Identity DisorderDaedalusNoch keine Bewertungen
- Wender Utah Rating Scale (Wurs) : As A Child I Was (Or Had)Dokument2 SeitenWender Utah Rating Scale (Wurs) : As A Child I Was (Or Had)J31415Noch keine Bewertungen
- Girl InterruptedDokument7 SeitenGirl Interruptedapi-365678992Noch keine Bewertungen
- Mental Health Nurse CVDokument2 SeitenMental Health Nurse CVTimur UrakovNoch keine Bewertungen
- Name of The Hospital - Teaching Hospital, Karapitiya: Case 7 Puerperal PsychosisDokument13 SeitenName of The Hospital - Teaching Hospital, Karapitiya: Case 7 Puerperal PsychosisCharith Rukmal KodituwakkuNoch keine Bewertungen
- Clinical Ethics For The Treatment of Children and AdolescentsDokument15 SeitenClinical Ethics For The Treatment of Children and AdolescentsPierre AA100% (1)
- 7718 (07) Review of Cases - Anxiety DisordersDokument34 Seiten7718 (07) Review of Cases - Anxiety DisordersnewazNoch keine Bewertungen
- Theoretical Perspectives in CounselingDokument28 SeitenTheoretical Perspectives in CounselingGargi BishtNoch keine Bewertungen
- Ed WilliamsDokument39 SeitenEd WilliamsTamara BatesNoch keine Bewertungen
- CBT Labelling EmotionsDokument3 SeitenCBT Labelling Emotionskicaanu100% (1)
- Attachment Theory: Summary: Attachment Theory Emphasizes The Importance of A Secure and Trusting Mother-Infant BondDokument3 SeitenAttachment Theory: Summary: Attachment Theory Emphasizes The Importance of A Secure and Trusting Mother-Infant BondRessie Joy Catherine Felices100% (2)
- Mcmi Iii Report JamilDokument8 SeitenMcmi Iii Report Jamilshubhangi kapoor100% (1)
- 12steps To Creating Motivation When DepressedDokument3 Seiten12steps To Creating Motivation When DepressedAnonymous Ax12P2srNoch keine Bewertungen
- Phobia EssayDokument4 SeitenPhobia EssayEdna MartinezNoch keine Bewertungen
- Sensory Abnormalities in Children With Autism SpecDokument9 SeitenSensory Abnormalities in Children With Autism SpecceavilaNoch keine Bewertungen