Beruflich Dokumente
Kultur Dokumente
Differential Antiplatelet Effects
Hochgeladen von
Negreanu AncaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Differential Antiplatelet Effects
Hochgeladen von
Negreanu AncaCopyright:
Verfügbare Formate
Clin Res Cardiol 95:212216 (2006) DOI 10.
1007/s00392-006-0363-1
ORIGINAL PAPER
D. Skowasch A. Viktor M. Schneider-Schmitt B. Lderitz G. Nickenig G. Bauriedel
Differential antiplatelet effects of angiotensin converting enzyme inhibitors
Comparison of ex vivo platelet aggregation in cardiovascular patients with ramipril, captopril and enalapril
Received: 3 May 2005 Accepted: 22 December 2005 Published online: 17 February 2006
Dr. Dirk Skowasch ()) Achim Viktor Melanie Schneider-Schmitt Prof. Dr. Dr. h.c. Berndt Lderitz Prof. Dr. Georg Nickenig Prof. Dr. Gerhard Bauriedel Department of Internal Medicine II Cardiology Heart Center University of Bonn Sigmund-Freud-Str. 25 53105 Bonn, Germany E-Mail: Dirk.Skowasch@ukb.uni-bonn.de
n Summary Background Increasing evidence suggests that angiotensin converting enzyme (ACE) inhibitors exert antithrombotic effects. Based on the assumption of differential effects of various ACE inhibitors on coagulation, the aim of the present study was to evaluate the coagulative activities of cardiovascular (CV) patients treated with either ramipril, captopril, and enalapril, and to compare these with patients treated with established antithrombotics such as aspirin (ASA) and clopidogrel or none of these medication. Methods Blood samples of 320 CV patients with coronary artery disease and/or arterial hypertension were analyzed by wholeblood aggregometry. Platelet aggregation was determined by measuring the increase in impedance across paired electrodes in response to the aggregatory agents collagen and adenosine diphosphate (ADP), respectively. These data were correlated with medical treatment. Results Platelet aggre-
gation was attenuated ex vivo by ramipril and captopril as well as by ASA and clopidogrel. While collagen-induced platelet aggregation was significantly reduced by ramipril (35%; P < 0.01) and captopril (27%; P = 0.01), no change was seen with enalapril. After induction with ADP, platelet aggregation was reduced in the presence of captopril therapy by 46% (P < 0.05). There was a trend of inhibition with ramipril (32%, P = n.s.), whereas no antithrombotic effect was seen with enalapril. Conclusion Our findings demonstrate that ACE inhibitors decrease platelet aggregation ex vivo. The differential antiaggregatory profile may explain at least in part different effects of ACE inhibitors on cardiovascular endpoints as observed in large clinical trials. n Key words ACE inhibitors atherosclerosis arterial hypertension platelet aggregation
Introduction
Angiotensin-converting enzyme (ACE) inhibitors are widely used in patients with various cardiovascular diseases [4, 14]. ACE inhibitor therapy has been shown to reduce the incidence of acute myocardial infarction (MI) in patients with left ventricular dysfunction [11, 19]. In addition, mortality was lower
in subgroups of these patients post myocardial infarction [68, 16]. Likewise, the Heart Outcomes Prevention Evaluation (HOPE) study showed a 22% reduction in cardiovascular death, stroke, and MI with ramipril in patients with high cardiovascular risk in the absence of heart failure or left ventricular dysfunction [17]. The EURopean trial On reduction of cardiac events with Perindopril in stable coronary
D. Skowasch et al. Differential antiplatelet effects of ACE inhibitors
213
Artery disease (EUROPA) demonstrated a 20% relative reduction in the combined primary endpoint cardiovascular mortality, non-fatal myocardial infarction, and resuscitated cardiac arrest [3]. Recently, we and others demonstrated attenuated platelet aggregation with ACE inhibitor therapy, which might at least partly explain the pleiotropic beneficial effects of this drug class on cardiovascular events [1, 13]. Since individual ACE inhibitors differ substantially in their physiochemical properties, enzymebinding kinetics, pharmacokinetic profile, organ specific affinity and selectivity, the purpose of the present study was to evaluate different ACE inhibitors versus aspirin and clopidogrel as classical antithrombotics in their effect on platelet aggregation, by use of whole-blood aggregometry in patients with cardiovascular disease.
Methods
We prospectively enrolled 320 stable cardiovascular patients, between February 2000 and February 2003. These patients were recruited from consecutive patients who presented at our Heart Center. All participants gave informed consent before enrollment. Inclusion criteria were coronary artery disease, arterial hypertension, or both [1]. Treatment with glycoprotein II b/IIIa receptor blockers, aspirin as analgesic therapy within the last four weeks, angiotensin II type 1 receptor antagonists or combined antithrombotic/ACE inhibitor medication led to study exclusion. At the baseline study visit, detailed demographic data and a background medication profile were collected (Table 1). Patients were classified into five groups of study participants: group A, patients with cardiovascular disease who were not taking ACE inhibitors or antithrombotic medication (control group); group B, patients taking aspirin (100 to 300 mg/d) and/or clopidogrel (75 mg/d); group C, patients taking ramipril; group D, patients taking captopril; group E, patients taking enalapril. Of the patients with ACE inhibitor medication, 21 were treated with ramipril (2.510 mg/d, mean 5.5 3.0 mg/d), 33 were treated with captopril (6.25-150 mg/d; mean 45.3 23.4 mg/d) and 25 with enalapril (2.5-20 mg/d; mean 9.6 6.2 mg/d); patients received ACE inhibitors for a minimum of 2 weeks. After recruitment of the patients, venous blood samples were collected in plastic tubes containing a 1 : 10 volume of acid citrate anticoagulant (2 parts of 0.1 mol/l citic acid to 3 parts of 0.1 mol/l trisodium citrate) and subsequently (between 30 min and 5 h) processed, as recently described [1]. Platelet aggregation in whole blood samples were examined by an
impedance aggregometer (Model 560, Chrono-Log, Havertown, PA, USA). Measurements were performed at 37 8C and a stirring speed of 900 rpm. According to the recommendations of the manufacturer, citrate blood (500 ll) was diluted 1-to-1 with 0.9% NaCl and prewarmed for 5 min at 37 8C. After the electrode was placed, aggregation was induced by the stimulatory agents collagen (final concentration 2 lg/ml) and adenosine diphosphate (ADP; final concentration 5 lmol/ml). Collagen and ADP were purchased from Nobis (Endingen, Germany). Platelet aggregation was monitored continually for 6 min, and responses were recorded as electrical impedance across paired electrodes (in Ohm). Inhibition of aggregation was evaluated as the percentage comparing the extent of aggregation in the presence (groups B-E) or absence (group A) of the antiaggregatory regimens studied. Baseline demographics, use of medication, and data of whole-blood aggregometry were compared. Group comparisons were performed by one-way analysis of variance (ANOVA) with a Bonferroni post hoc test. P values < 0.05 were considered to be statistically significant. Data are given as mean SD.
Results
Patient characteristics such as age, gender, cardiovascular risk factors and medication did not differ between groups and are presented in Table 1. Platelet aggregation was significantly attenuated by aspirin/ clopidogrel as well as by ramipril and captopril. Specifically, patients receiving aspirin/clopidogrel (group B) showed a 28% decrease in collagen-induced platelet aggregation (P < 0.001), indicated by a lower impedance increase compared with that of the untreated patients of group A (Fig. 1 a). With ramipril therapy (group C), the increase in impedance was reduced by 35% (P = 0.005), with captopril (group D) by 27% (P = 0.014), whereas no effect was seen with enalapril (group E, P = 1.0). Likewise, ADP-induced platelet aggregation was found to be significantly attenuated with aspirin/clopidogrel (group B) by 35% (P = 0.032; Fig. 1 b). The decrease in platelet aggregation averaged 46% with captopril (group D, P = 0.047). With ramipril therapy (group C), there was a trend of inhibition (32%; P = 0.96). No change in impedance was seen with enalapril (group E, P = 1.0). A subgroup analysis of group B was performed to evaluate specific inhibition pathways of the established antithrombotics. As expected, the increase in impedance after collagen-induction was reduced by 27% by aspirin monotherapy (n = 67; P = 0.01) and
214
Clinical Research in Cardiology, Volume 95, Number 4 (2006) Steinkopff Verlag 2006
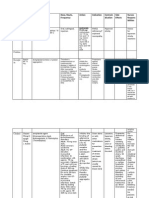
Table 1 Baseline characteristics of patients Group No. Age (yr) Male sex CAD Previous MI Hypertension Systolic BP (mmHg) Diastolic BP (mmHg) Other risk factors Diabetes Hyperlipidemia Current smoker Familial disposition Obesity Medication Aspirin/clopidogrel ACE inhibitors Nitrates b-blockers Calcium channel bl. Statins A 151 61 16 70 (46) 71 (47) 21 (24) 90 (60) 139 16 80 10 17 73 50 38 31 (11) (48) (33) (25) (21) B 90 63 12 45 (50) 58 (64) 19 (21) 58 (64) 138 15 79 11 21 55 38 25 17 (23) (61) (42) (28) (21) C 21 67 10 8 (38) 11 (52) 5 (24) 14 (67) 143 19 83 9 7 (33) 12 (57) 6 (29) 5 (24) 5 (24) 0 21 (100) 9 (43) 11 (52) 4 (19) 10 (48) D 33 65 9 12 (36) 15 (44) 7 (21) 19 (58) 141 17 81 12 5 (15) 16 (48) 10 (30) 13 (39) 4 (12) 0 33 (100) 10 (30) 14 (42) 6 (18) 11 (33) E 25 68 11 14 (56) 18 (72) 7 (21) 18 (72) 141 18 81 10 8 (32) 16 (60) 11 (44) 5 (20) 5 (20) 0 25 (100) 10 (40) 14 (56) 4 (16) 10 (40)
0 0 40 (26) 62 (41) 22 (15) 42 (28)
90 (100) 0 27 (30) 46 (51) 15 (17) 41 (46)
Baseline characteristics [number of patients (%) or mean SD]. A cardiovascular patients without ACE inhibitors or antithrombotic medication; B patients with aspirin/clopidogrel; C patients with ramipril; D patients with captopril; E patients with enalapril; ACE angiotensin converting enzyme; CAD coronary artery disease; MI myocardial infarction
a
Fig. 1 Influence of established antithrombotics and angiotensin-converting enzyme (ACE) inhibitors on platelet aggregation. Impedance changes in Ohm after induction with collagen (a) or with adenosine diphosphate (b) in pa-
b
tients not receiving antithrombocyte or ACE inhibitor medication (group A), in patients receiving aspirin/clopidogrel (group B), and in participants receiving ramipril (C), captopril (D) or enalapril (E). n.s. not significant
by 47% by clopidogrel monotherapy (n = 12; P = 0.19). After ADP induction, platelet aggregation was reduced by 22% with aspirin (P = 0.01) and by 72% with clopidogrel (P = 0.02).
Discussion
Beyond confirming the antiaggregatory effects of the established antithrombotics aspirin and clopidogrel, the present study shows that ACE inhibitors attenu-
D. Skowasch et al. Differential antiplatelet effects of ACE inhibitors
215
ate platelet aggregation and thereby demonstrates a differential antiaggregatory profile of different ACE inhibitors. While ramipril and captopril therapy reduced ex vivo platelet aggregation, no antithrombotic effect was seen with enalapril. The underlying mechanisms remain unclear so far. It has been hypothesized that tissue affinity might be responsible for some of the beneficial cardiovascular properties of ACE inhibitors. However, the present findings suggest that tissue ACE inhibitor affinity does not affect the antithrombotic effects of ACE inhibitors, since ramipril is a tissue-ACE inhibitor, and captopril and enalapril are non-tissue-ACE inhibitors. Likewise, others have not found a correlation between tissue-ACE affinity and risk of myocardial infarction in patients with arterial hypertension [12]. Possible mechanisms for reduced platelet aggregation with ACE inhibitor therapy are decreased tissue factor expression with ACE inhibition [20], lowered concentrations of circulating tissue factor [10], and reduced vascular [5] and systemic inflammation [9]. At first glance, parallel implications may result from the present ex vivo study and recent data from HOPE [17] and other trials [68, 11, 15, 16, 19]. The HOPE trial tested ramipril in patients with atherosclerosis in the absence of heart failure or left-ventricular dysfunction, and showed a significant decrease in the combined end point of cardiovascular death, myocardial infarction, and stroke, but not in unstable angina with electrocardiographic changes or in hospitalization rate [17]. One may conclude that clinical end points caused by total thrombotic vascular occlusion, but not those by incomplete coronary obliteration are significantly influenced. Beyond normalization of endothelial dysfunction and plaque stabilization, which were both discussed as being responsible for the clinical benefit of ramipril [17], our results support the concept of an additional antithrombotic effect of ramipril. Although it is unclear whether the benefits of ramipril can be extrapolated to other ACE inhibitors, data from unselected patients of the prospective multicenter registry MITRA PLUS suggested that ramipril has more beneficial effects on cardiovascular events than treatment with other ACE inhibitors [18]. The cardioprotective findings seen in HOPE and EUROPA do not necessarily presume a cardiovascular class effect of ACE inhibitors. The Prevention of Events with An-
giotensin Converting Enyzme Inhibition (PEACE) trial failed to provide any further benefit in terms of death from cardiovascular causes, myocardial infarcion, or coronary revascularization among a large cohort of patients with stable coronary disease treated with the ACE inhibitor trandolapril [2]. To date, several well-controlled clinical trials involving post-MI patients with left ventricular dysfunction have been performed with the different ACE inhibitors studied in the present work. The reduction in all-cause mortality observed in shortterm trials (CCS-1 [8] and ISIS-4 [7] with captopril) has been very modest, and in the CONSENSUS II trial there was even an increase in mortality with enalapril [15]. In long-term studies (SAVE [11] with captopril, AIRE [16] and AIREX [6] with ramipril), post-MI patients with left ventricular dysfunction and/or clinical signs and symptoms of heart failure were included and followed up for a longer period. The reduction in all-cause mortality observed in these studies was even greater compared to that in the short-term trials. One may speculate that antithrombotic effects of ramipril and captopril, as observed in the present study, were, at least in part, responsible for these beneficial effects, whereas no antithrombotic effect was seen with enalapril in the present study, analogous to an increase in mortality in the CONSENSUS II trial [15]. The concept of our present study was to screen the impact on platelet aggregation brought in by basic drug prescription in cardiovascular patients as seen in daily practice. Of course, there are several limitations of the study. No information can be drawn regarding the clinical relevance of ACE inhibitor reduced platelet aggregation. In remains open how long and in what dosage ACE inhibitors should be taken to achieve antithrombotic effects. In this study, medication use was based on answers to questionnaires; drug levels or pill counts were not performed. In summary, the present study demonstrates a differential antiaggregatory profile among different ACE inhibitors, which may explain at least in part different effects on cardiovascular events as observed in large clinical trials. Further head-to-head investigations with equivalent dosages of different ACE inhibitors may be warranted in large-scale studies to fully elucidate clinical differences and similarities among ACE inhibitors.
216
Clinical Research in Cardiology, Volume 95, Number 4 (2006) Steinkopff Verlag 2006
References
1. Bauriedel G, Skowasch D, Schneider M, Andri R, Jabs A, Lderitz B (2003) Antiplatelet effects of angiotensin-converting enzyme inhibitors compared with aspirin and clopidogrel: a pilot study with whole-blood aggregometry. Am Heart J 145:343 348 2. Braunwald E, Domanski MJ, Fowler SE, PEACE Trial Investigators (2004) Angiotensin-converting-enzyme inhibitors in stable coronary artery disease. N Engl J Med 351:20582068 3. Fox KM; EURopean trial on reduction of cardiac events with Perindopril in stable coronary Artery disease Investigators (2003) Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, doubleblind, placebo-controlled, multicentre trial (the EUROPA study). Lancet 362:782788 4. Genoni M, Malacrida R, Sessa F, Siegrist P, Maggioni AP, Mocceti T (2000) Long-term safety of an early ACE-inhibitor treatment of patients with acute myocardial infartion: results of the 3 year follow-up period on 696 Swiss patients randomized to the ISIS-4 trial. Z Kardiol 89:8183 5. Gross CM, Gerbaulet S, Quensel C, Krmer J, Mittelmeier HO, Luft FC, Dietz R (2002) Angiotensin II type 1 receptor expression in human coronary arteries with variable degrees of atherosclerosis. Basic Res Cardiol 97:327333 6. Hall AS, Murray GD, Ball SG, on behalf of AIREX study investigators (1997) Follow-up study of patients randomly allocated ramipril or placebo for heart failure after acute myocardial infarction: AIRE Extension (AIREX) study. Lancet 349:14931497 7. ISIS-4 Collaborative Group. Fourth International Study of Infarct Survival (1995) A randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58 050 patients with suspected acute myocardial infarction. Lancet 345:669685 8. Lisheng L, Liu LS, Wang W, for the Chinese Cardiac Study Collaborative Group (1995) Oral captopril versus placebo among 13,634 patients with suspected myocardial infarction: interim report from the Chinese Cardiac Study (CCS-1). Lancet 345:686687 9. Mitrovic V, Klein HH, Krekel N, Kreuzer J, Fichtlscherer S, Schirmer A, Paar WD, Hamm CW (2005) Influence of the angiotensin converting enzyme inhibitor ramipril on highsensitivity C-reactive protein (hsCRP) in patients with documented atherosclerosis. Z Kardiol 94:336342 10. Napoleone E, Di Santo A, Camera M, Tremoli E, Lorenzet R (2000) Angiotensin-converting enzyme inhibitors downregulate tissue factor synthesis in monocytes. Circ Res 86:139143 11. Rutherford J, Pfeffer M, Moye LA, Davis B, Flaker G, Kowey PR, Lamas GA, Miller HS, Packer M, Rouleau JL, Braunwald E (1994) Effects of captopril on ischemic events after myocardial infarction: results of the Survival and Ventricular Enlargement trial: SAVE Investigators. Circulation 90: 17311738 12. Sauer WH, Baer JT, Berlin JA, Kimmel SE (2004) Class effect of angiotensin-converting enzyme inhibitors on prevention of myocardial infarction. Am J Cardiol 94:11711173 13. Schieffer B, Bnte C, Witte J, Hoeper K, Bger RH, Schwedhelm E, Drexler H (2004) Comparative effects of AT1antagonism and angiotensin-converting enzyme inhibition on markers of inflammation and platelet aggregation in patients with coronary artery disease. J Am Coll Cardiol 44:362 368 14. Smith WH, Ball SG (2000) ACE inhibitors in heart failure: an update. Basic Res Cardiol 95(Suppl 1):I814 15. Swedberg K, Held P, Kjekshus J, Rasmussen K, Ryden L, Wedel H, on behalf of the CONSENSUS II study group (1992) Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med 327:678684 16. The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators (1993) Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 342:821828 17. The Heart Outcomes Evaluation (HOPE) Study Investigators (2000) Effects of an angiotensin-convertingenzyme inhibitor, ramipril on cardiovascular events in high-risk patients. N Engl J Med 342:145153 18. Wienbergen H, Schiele R, Gitt AK, Juenger C, Heer T, Meisenzahl C, Landgraf H, Bossaller C, Senges J, for the MITRA PLUS Study Group (2002) Impact of ramipril versus other angiotensin-converting enzyme inhibitors on outcome of unselected patients with ST-elevation acute myocardial infarction. Am J Cardiol 90:10451049 19. Yusuf S, Pepine C, Garces C, Pouleur H, Salem D, Kostis J, Benedict C, Rousseau M, Bournassa M, Pitt B (1992) Effect of enalapril on myocardial infarction and unstable angina in patients with low ejection fractions. Lancet 340:11731178 20. Zurbano MJ, Anguera I, Heras M, Roig E, Lozano M, Sanz G, Escolar G (1999) Captopril administration reduces thrombus formation and surface expression of platelet glycoprotein IIb/IIIa in early postmyocardial infarction stage. Arterioscler Thromb Vasc Biol 19:17911795
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- 2018 ESMO Handbook of Immuno OncologyDokument389 Seiten2018 ESMO Handbook of Immuno OncologyNegreanu Anca100% (1)
- ESHRE COS Guideline - For Stakeholder Review - Versie 2 PDFDokument134 SeitenESHRE COS Guideline - For Stakeholder Review - Versie 2 PDFNegreanu AncaNoch keine Bewertungen
- Suppression of Ovarian Activity With A Drospirenone-ContainingDokument10 SeitenSuppression of Ovarian Activity With A Drospirenone-ContainingNegreanu AncaNoch keine Bewertungen
- Bono Esmo 2018 Highlights FinalDokument43 SeitenBono Esmo 2018 Highlights FinalNegreanu AncaNoch keine Bewertungen
- Cancer PainDokument11 SeitenCancer PainNegreanu AncaNoch keine Bewertungen
- Slides at Enc14 13cng 07Dokument62 SeitenSlides at Enc14 13cng 07Negreanu AncaNoch keine Bewertungen
- Oncology and Basic ScienceDokument576 SeitenOncology and Basic ScienceNegreanu Anca100% (1)
- Update On The Incidence of Metamizole Sodium-Induced Blood Dyscrasias in PolandDokument7 SeitenUpdate On The Incidence of Metamizole Sodium-Induced Blood Dyscrasias in PolandNegreanu AncaNoch keine Bewertungen
- Czerwinski Et Al Calcif Tissue Int 2007 80 Suppl 1 s121 Abstract P316MDokument1 SeiteCzerwinski Et Al Calcif Tissue Int 2007 80 Suppl 1 s121 Abstract P316MNegreanu AncaNoch keine Bewertungen
- Bianchi Czerwinski DIVA 2011-11-14Dokument10 SeitenBianchi Czerwinski DIVA 2011-11-14Negreanu AncaNoch keine Bewertungen
- 319 FullDokument3 Seiten319 FullNegreanu AncaNoch keine Bewertungen
- Update On The Incidence of Metamizole Sodium-Induced Blood Dyscrasias in PolandDokument7 SeitenUpdate On The Incidence of Metamizole Sodium-Induced Blood Dyscrasias in PolandNegreanu AncaNoch keine Bewertungen
- Eur Heart J-2010 - 2369-429Dokument61 SeitenEur Heart J-2010 - 2369-429Negreanu AncaNoch keine Bewertungen
- Boniva (Ibandronate Sodium) Infusion OrderDokument1 SeiteBoniva (Ibandronate Sodium) Infusion OrderNegreanu AncaNoch keine Bewertungen
- Guidelines For The Adminstration of Drugs Via Enteral Feeding TubesDokument13 SeitenGuidelines For The Adminstration of Drugs Via Enteral Feeding TubesNegreanu AncaNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Tentative Scientific Program Hopecardis 2013Dokument1 SeiteTentative Scientific Program Hopecardis 2013Devi GirsangNoch keine Bewertungen
- Curriculum Vitae: Nama: Prof DR DR Hasan Sjahrir Sps (KDokument11 SeitenCurriculum Vitae: Nama: Prof DR DR Hasan Sjahrir Sps (KUKM MargaasihNoch keine Bewertungen
- Hemostatic and Thrombotic Considerations in The Diagnosis and ManagementDokument12 SeitenHemostatic and Thrombotic Considerations in The Diagnosis and Managementender izaguirreNoch keine Bewertungen
- High Sensitivity C-Reactive ProteinDokument100 SeitenHigh Sensitivity C-Reactive ProteinFast ComposersNoch keine Bewertungen
- Concise Manual of Cosmetic Dermatologic SurgeryDokument142 SeitenConcise Manual of Cosmetic Dermatologic SurgerynzsargaziNoch keine Bewertungen
- Chronic Limb IschemiaDokument27 SeitenChronic Limb IschemiaGarima SahuNoch keine Bewertungen
- DM + Gangren PedisDokument61 SeitenDM + Gangren Pedismegadama0Noch keine Bewertungen
- Bleeding Disorders Ce319Dokument25 SeitenBleeding Disorders Ce319cesimpsonNoch keine Bewertungen
- Treatment Strategies of Acute Myocardial Infarction Updates OnDokument11 SeitenTreatment Strategies of Acute Myocardial Infarction Updates OnLilasNoch keine Bewertungen
- Noncommunicable DiseasesDokument22 SeitenNoncommunicable DiseasesChintiya PutriNoch keine Bewertungen
- Society of Cardiovascular Anesthesiologists.9Dokument13 SeitenSociety of Cardiovascular Anesthesiologists.9Tatán VeylNoch keine Bewertungen
- Plavix (Clopidogrel)Dokument1 SeitePlavix (Clopidogrel)E50% (2)
- ClopidogrelDokument2 SeitenClopidogrelapi-3797941100% (2)
- Mayo ClinicDokument338 SeitenMayo Clinicrajkumarss87Noch keine Bewertungen
- Special Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersDokument6 SeitenSpecial Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersRatri ReswitadewiNoch keine Bewertungen
- 18 Consultative HematologyDokument40 Seiten18 Consultative HematologyJose Luis Gutierrez RamirezNoch keine Bewertungen
- Thoracic Post Op Complications PDFDokument169 SeitenThoracic Post Op Complications PDFMayang Nurul100% (1)
- DrugsDokument10 SeitenDrugsRebecca JolieNoch keine Bewertungen
- Ischemic StrokeDokument17 SeitenIschemic StrokejamalNoch keine Bewertungen
- Critical Appraisal: Iloilo Mission Hospital Internal Medicine DepartmentDokument40 SeitenCritical Appraisal: Iloilo Mission Hospital Internal Medicine DepartmentKarren Taquiqui PleteNoch keine Bewertungen
- Antiplatelet Drugs Cyclooxygenase Inhibitors Aspirin: MOA Clinical UsesDokument3 SeitenAntiplatelet Drugs Cyclooxygenase Inhibitors Aspirin: MOA Clinical UsesAsma AlfaouriNoch keine Bewertungen
- Peripocedural Anticoagulation LPDokument11 SeitenPeripocedural Anticoagulation LPlauraalvisNoch keine Bewertungen
- Perioperative Considerations and Management of Patients Receiving AnticoagulantsDokument7 SeitenPerioperative Considerations and Management of Patients Receiving Anticoagulantsdrvasantha 8Noch keine Bewertungen
- Duration of Dual Antiplatelet Therapy: Current ControversiesDokument8 SeitenDuration of Dual Antiplatelet Therapy: Current ControversiesRajendra ChavanNoch keine Bewertungen
- RECOVER Post Vaccine Protocol-2023-02-28Dokument60 SeitenRECOVER Post Vaccine Protocol-2023-02-28foxdog2Noch keine Bewertungen
- Acute Coronary SyndromeDokument8 SeitenAcute Coronary SyndromeMohammad Neyazur RahamanNoch keine Bewertungen
- Cardiovascular Disease Risk AssesmentDokument24 SeitenCardiovascular Disease Risk Assesmentaldrin zamoraNoch keine Bewertungen
- Aspirin (Plus Antiplatelet Medicines) - What Is Aspirin - PatientDokument9 SeitenAspirin (Plus Antiplatelet Medicines) - What Is Aspirin - Patientaasuman123Noch keine Bewertungen
- Drug Study ClopidogrelDokument1 SeiteDrug Study ClopidogrelBARRISTERFLOWERSEAURCHIN6Noch keine Bewertungen