Beruflich Dokumente
Kultur Dokumente
COPD CaseStudy
Hochgeladen von
Sex & Gender Women's Health CollaborativeOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
COPD CaseStudy
Hochgeladen von
Sex & Gender Women's Health CollaborativeCopyright:
Verfügbare Formate
Focus on COPD (Issue I)
Funding for this newsletter series was provided by
Pulmonary Practice Pearls for Primary Care Physicians
5-part eNewsletter series
Vol 1, Issue 1
Primary care physicians routinely see patients with chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD).
Although treatment guidelines are available, we still need practical information that translates guidelines and other evidence into diagnosing and managing
these diseases. Each issue in the Pulmonary Practice Pearls for Primary Care Physicians eNewsletter series will focus on a key topic in the management of
COPD or asthma within the context of current national guidelines and clinical practice. Topics will be brought to life through the presentation of clinical cases,
and an emphasis will be placed on applying key learnings to clinical practice.
Series author Recognizing and Managing COPD in Patients With Multiple Morbidities
In 2007, the United States had the second highest death rate for COPD among 16 industrialized nations.1 Most cases
of COPD are caused by cigarette smoking2 and are associated with chronic, often progressively worsening, airflow
limitation resulting from reversible and irreversible changes in central and peripheral airways.3 Together with other
less common chronic lower respiratory diseases, COPD is the fourth leading cause of death in the United States,
behind heart disease, cancer, and stroke.1 In 2007, approximately 12 million men and women in the United States
were diagnosed with COPD, and a similar number of people may have undiagnosed COPD.1
The number of women self-reporting symptoms of COPD increased in the second half of the 20th century,4 potentially
because smoking habits between men and women are now similiar.5 Since the early 1980s, the prevalence of COPD
Barbara P. Yawn, in women has been higher compared with men.1,4 Although COPD-related mortality rates in men decreased slowly in
MD, MSc, FAAFP the 1990s, then sharply decreased in 1999, rates in women increased in the 1990s, and plateaued in 2006.1
Director of Research
Olmsted Medical Center COPD and Multiple Morbidities
Rochester, Minnesota
A complication both for the diagnosis and management of COPD is that most individuals with COPD have multiple
Dr. Yawn disclosed that she other morbidities.6 Consider the case below:
serves on advisory boards for
Boehringer Ingelheim and
Novartis and has received
grant support from Novartis,
Boehringer Ingelheim, and
Merck.
Roland Tacke, PhD, and
Marissa Buttaro, MPH, of
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (1 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
Scientific Connexions in
Newtown, Pennsylvania, CASE
provided medical writing
support for this article through Mary is a 58-year-old accountant and grandmother who visits you for follow-up of her third "bad cold"
funding from AstraZeneca LP. this winter. She feels that she always gets the worst colds of "anyone around," and it takes her 3 or 4
weeks to get over the cough and congestion. "It isn't fair," she tells you." I gave up smoking 2 years
ago, but I still get these colds, and I'm afraid that I will cough so hard that I will break a rib with my
Printer-Friendly version
thin bones." On questioning, Mary admits that she hasn't been "back to normal" for several years.
She can no longer walk as far—or as fast—as her friends, and she easily gets short of breath when
climbing stairs. Lately, she’s been staying home more—even passing up opportunities to see her
Visit other newsletters
grandchildren—because she's too tired. Mary is taking a once-a-month medication and calcium plus
in this series vitamin D for her osteoporosis. She is also taking a statin for her elevated cholesterol levels.
Occasionally, she wonders whether she might need nitroglycerin like her husband. In your
conversations with Mary, you also get the sense that she may be depressed. Mary's history of
smoking, her frequent prolonged colds, and her decreased exercise capacity suggest she may have
COPD—though heart disease is also a possibility. She undergoes a cardiac workup, but her
electrocardiogram and stress test are normal. She then undergoes spirometry to test her lung
function and a chest X-ray to rule out lung cancer. There are no signs of lung cancer, but her
postbronchodilator spirometry result is consistent with moderate, but closely approaching severe,
COPD as described in the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines
(http://www.goldcopd.com/Guidelineitem.asp?l1=2&l2=1&intId=989) (FIGURE 1): a
postbronchodilator forced expiratory volume in 1 second (FEV1) of 54% of predicted normal and a
FEV1/forced vital capacity (FVC) of 0.63.3
Note: This is a hypothetical case description for teaching purposes.
In many regards, Mary is a typical patient with COPD; she’s in her late 50s, with undiagnosed COPD and multiple
additional morbidities—in her case osteoporosis, hypercholesterolemia, and possibly depression. (See Case.)
Patients with COPD have a higher frequency of morbidities than age-, sex-, and geographically matched control
samples.7 In particular, COPD patients are at increased risk for pneumonia,8 osteoporosis,8 respiratory infections,8
lung cancer,9 and heart disease.9,10
Results of a US national telephone survey of 1003 patients with COPD showed that nearly 50% of patients with
COPD had 6 to10 additional morbidities, approximately 25% had 11 to 15 morbidities, and about 7% had 16 to 25
morbidities.11 There also was a preponderance of cardiovascular diseases among both sexes and a 39% prevalence
of osteoporosis among surveyed women.11
Similarly, a retrospective analysis of data from more than 20,000 participants of 2 cohort studies conducted by the
National Institutes of Health demonstrated a significant association between COPD and the presence of
cardiovascular disease, hypertension, and diabetes.6 Importantly, results of a large case-control study of
approximately 90,000 US patients followed for an average of 3 years showed that the presence of COPD was
associated with significantly increased risks of hospitalization and mortality from cardiovascular diseases, including a
5-fold increased risk of death from congestive heart failure.12
Coincidental—or Not? What's Behind the Other Morbidities
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (2 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
Some concurrent morbidities in patients with COPD may be coincidental, whereas others may relate to underlying
pathophysiology or complications of the disease.3 Depression and anxiety may be unrelated to COPD’s underlying
pathogenesis3 but affect about 40% of patients with COPD and contribute to increased functional disability.13 In
contrast, lung cancer and ischemic heart disease may share a common etiology with COPD: smoking.3,14 Systemic
inflammation has been suspected as a pathogenic link between COPD and extrapulmonary morbidities such as
cachexia, osteoporosis, cardiovascular disease, and perhaps depression (FIGURE 2).14,15 An interaction between
COPD and heart disease is also suggested by a recent post hoc analysis of data from the European Respiratory
Society study on Chronic Obstructive Pulmonary Disease (EUROSCOP).16 Three years of therapy with inhaled
budesonide, an inhaled corticosteroid, was associated with a significant reduction in the incidence of ischemic cardiac
events, including angina pectoris and myocardial infarction, among smokers with mild COPD not currently receiving
treatment with a beta-blocker.16
Why Does COPD Go Undiagnosed in So Many Patients?
Many concurrent morbidities in patients with COPD (eg, hypertension) are more easily diagnosed than early-stage
COPD, or are so serious (eg, heart disease) that they dominate a patient’s symptom profile and may absorb a
physician’s attention at the expense of seemingly less serious symptoms. This dynamic may explain the findings of a
Spanish population study that showed that at least 60% of patients with cardiovascular disease and spirometrically
confirmed airflow limitations received no respiratory treatment.17
Another impediment to the timely diagnosis of COPD is that the clinical manifestations of COPD are highly variable.18
Furthermore, some COPD symptoms (eg, dyspnea) are similar to those of asthma2 and overlap with those of left
ventricular heart failure.19 An evaluation of lung function by prebronchodilator and postbronchodilator spirometry is
most important for the diagnosis of COPD in any patient with persistent respiratory problems (TABLE 1). Smokers
with concomitant cardiovascular disease should also have spirometry testing, unless contraindicated due to unstable
angina or recent myocardial infarction.20 However, a definitive diagnosis of COPD often requires additional tests (eg,
electrocardiogram, B-natriuretic peptide, eosinophils) to distinguish between COPD, asthma, and heart failure.2,19
Comanagement of COPD and Concurrent Morbidities: Medication Challenges
Comanagement of COPD and concurrent morbidities poses significant challenges for the treating physician. The
possibility of drug−disease state interactions may preclude preferred therapeutic options for the treatment of patients
with multiple morbidities.
An example of possible treatment conflicts is the comanagement of COPD and osteoporosis. The reasons for the
association of COPD and increased risk of osteoporosis are multifactorial and poorly understood. Although
recognized risk factors such as smoking and older age increase the risk of osteoporosis in COPD patients, it has
been suggested that COPD-related systemic inflammation and corticosteroid use may further increase this risk.21,22 A
large observational study conducted in Italy identified inhaled and oral corticosteroid use as significant independent
risk factors that doubled the risk of osteoporosis, with a 3-fold increase in risk for combined oral and inhaled
therapy.22 In contrast, 3-year data from the EUROSCOP study showed no effect of inhaled corticosteroid use on
vertebral fracture.23
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (3 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
Although the 2 studies investigated different end points, their results exemplify the complexity associated with
comanaging COPD that requires chronic inhaled corticosteroids and recurrent bursts of oral corticosteroids in women
with osteoporosis.
Another possible treatment conflict exists with beta-blockers and bronchodilators. Although beta-blockers are
recommended after an acute myocardial infarction, use may compromise the pulmonary effects of β2-adrenergic
agonists used as bronchodilators in COPD.24 Fortunately, advances in the availability of β1-selective blockers (ie,
cardioselective)25 and recent studies showing benefits with these agents in COPD patients who underwent major
vascular surgery26 or recently experienced a myocardial infarction have nearly obviated this concern.27 These findings
allow for appropriate comanagement of COPD with long-acting β2-adrenergic agonists and cardiovascular disease
with β1-selective blockers.
Guidelines seldom provide recommendations for the comanagement of COPD and multiple other morbidities. Thus,
family physicians and other primary care physicians have to manage these diseases based on each patient’s clinical
history and coordinate specialty care when needed to ensure optimal management of their patients.
Management Guidelines
Comprehensive guidelines for the diagnosis and management of COPD have been provided by the GOLD guidelines.
Based on spirometric characteristics, GOLD distinguishes between 4 stages of COPD (FIGURE 1)3 and has
established the following goals of disease management3:
● symptom relief
● prevention of disease progression
● improvement of exercise tolerance
● improvement of health status
● prevention/treatment of complications
● prevention/treatment of exacerbations
● reduction of mortality
To achieve these goals, the GOLD guidelines recommend active reduction of risk factors, including smoking
cessation and influenza vaccination, for patients at all 4 stages.3 The Centers for Disease Control’s Advisory
Committee on Immunization Practices recommends pneumococcal (polysaccharide) vaccination and tetanus,
diphtheria, and acellular pertussis (Td/Tdap) vaccination for adults,28 but the role of these vaccines in COPD
management remains unclear. Based on a limited body of evidence from randomized controlled trials, the GOLD
guidelines recommend the pneumococcal vaccine for COPD patients 65 years and older and for COPD patients
younger than age 65 with an FEV1 <40% predicted.3
Short-acting bronchodilators should be prescribed for as-needed use. Daily therapy with long-acting bronchodilators
is recommended for moderate to very severe COPD, and an inhaled corticosteroid should be added for patients with
severe or very severe COPD and repeated exacerbations.
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (4 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
Two landmark trials in COPD, the TOwards a Revolution in COPD Health (TORCH) and the Understanding Potential
Long-Term Impacts on Function with Tiotropium (UPLIFT) studies, permitted inclusion of patients with a coexisting
nonrespiratory disease that was not unstable or severe enough to interfere with study participation.29-31 Recent results
of the TORCH study showed that the combination of a long-acting β2-adrenergic agonist (salmeterol) and an inhaled
corticosteroid (fluticasone) for patients with moderate to severe COPD reduced the annual rate of acute
exacerbations and improved health status and lung function.32 Importantly, adverse event data indicated no increased
probability of bone fractures with combination therapy.32
Results of the 4-year UPLIFT trial showed that treatment with tiotropium (an inhaled anticholinergic) significantly
reduced not only the risk of exacerbations and delayed first hospitalizations but also reduced the risk of serious
events of angina, respiratory failure, congestive heart failure, and myocardial infarction.30
Based on this information, then, what is the appropriate therapy for Mary?
CASE
According to the GOLD guidelines, Mary has moderate, but closely approaching severe, COPD.3
While a cutoff FEV1 of 50% of predicted normal is a good guideline for initiating or adding inhaled
corticosteroid therapy, no guideline should be considered an absolute. Because Mary appears to
have frequent exacerbations and an FEV1 of 54% of predicted normal, a combination of an inhaled
corticosteroid and a long-acting bronchodilator is recommended. The use of oral corticosteroid
bursts several times a year to treat acute exacerbations generally should be avoided in order to
minimize the risk of aggravating her existing osteoporosis.
In light of your suspicions, you ask Mary also to complete the Patient Health Questionnaire-9 Item
(PHQ-9) to screen for depression.2 If she is found to be depressed, you may need to put her on an
antidepressant to improve her mood and motivation sufficiently to allow her to enter a pulmonary
rehabilitation program, which is recommended for moderate and severe COPD.3
Although cardiovascular disease was previously ruled out, Mary should be periodically monitored
given her history of hypercholesterolemia and COPD. Treating her COPD and decreasing the risk of
exacerbations is likely to improve her overall health status and may mitigate her other morbidities,
including osteoporosis, and depression. Her continued use of statins for hypercholesterolemia also
may slow the decline in lung function33 and decrease the risk of death.34,35
Treating patients like Mary who have COPD and multiple other morbidities is a common occurrence in primary care.
Maximizing the care you provide to these patients hinges on making an early diagnosis, taking steps to reduce risk,
and considering the consequences for concurrent morbidities when developing a COPD treatment plan.
References
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (5 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
1. National Heart, Lung, and Blood Institute. National Institutes of Health. Morbidity and mortality: 2009 chart book on cardiovascular, lung,
and blood diseases. http://www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf. Accessed September 21, 2010.
2. Yawn BP, Keenan JM. COPD—the primary care perspective: addressing epidemiology, pathology, diagnosis, treatment of smoking's
multiple morbidities and the patient's perspective. COPD. 2007;4:67–83.
3. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of COPD.
Updated 2010. http://www.goldcopd.com/Guidelineitem.asp?l1=2&l2=1&intId=989. Accessed April 7, 2011.
4. Mannino DM, Homa DM, Akinbami LJ, et al. Chronic obstructive pulmonary disease surveillance–United States, 1971–2000. MMWR
Morb Mortal Wkly Rep. 2002;51(SS06):1-16.
5. Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370:765-773.
6. Mannino DM, Thorn D, Swensen A, et al. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD.
Eur Respir J. 2008;32:962–969.
7. Yu-Isenberg KS, Vanderplas A, Chang EY, et al. Utilization and medical care expenditures in patients with chronic obstructive
pulmonary disease: a managed care claims data analysis. Dis Manage Health Outcomes. 2005;13:405–412.
8. Soriano JB, Visick GT, Muellerova H, et al. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest.
2005;128:2099–2107.
9. GarcÌa RodrÌguez LA, Wallander M-A, MartÌn-Merino E, et al. Heart failure, myocardial infarction, lung cancer and death in COPD
patients: a UK primary care study. Respir Med. 2010;104:1691–1699.
10. Schneider C, Bothner U, Jick SS, et al. Chronic obstructive pulmonary disease and the risk of cardiovascular diseases. Eur J Epidemiol.
2010;25:253–260.
11. Barr RG, Celli BR, Mannino DM, et al. Comorbidities, patient knowledge, and disease management in a national sample of patients with
COPD. Am J Med. 2009;122:348–355.
12. Sidney S, Sorel M, Quesenberry CP Jr, et al. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser
Permanente Medical Care Program. Chest. 2005;128:2068–2075.
13. Yohannes AM, Willgoss TG, Baldwin RC, et al. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary
disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25:1209-1221.
14. Barnes PJ. Chronic obstructive pulmonary disease: effects beyond the lungs. PLoS Med. 2010;7(3):e1000220.
15. Sin DD, Anthonisen NR, Soriano JB, et al. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28:1245–1257.
16. Löfdahl CG, Postma DS, Pride NB, et al. Possible protection by inhaled budesonide against ischaemic cardiac events in mild COPD.
Eur Respir J. 2007;29:1115–1119.
17. Soriano JB, Rigo F, Guerrero D, et al. High prevalence of undiagnosed airflow limitation in patients with cardiovascular disease. Chest.
2010;137:333–340.
18. Agusti A, Calverley PMA, Celli B, et al. Characterization of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122.
19. Rutten FH, Cramer MJ, Lammers JW, et al. Heart failure and chronic obstructive pulmonary disease: An ignored combination? Eur J
Heart Fail. 2006;8:706–711.
20. Miller MR, Crapo R, Hankinson J, et al. General considerations for lung function testing. Eur Respir J. 2005;26:153–161.
21. Jørgensen NR, Schwarz P. Osteoporosis in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2008;14:122–127.
22. Maggi S, Siviero P, Gonnelli S, et al for the EOLO Study Group. Osteoporosis risk in patients with chronic obstructive pulmonary
disease: the EOLO study. J Clin Densitom. 2009;12:345–352.
23. Pauwels RA, Löfdahl CG, Laitinen LA, et al for the European Respiratory Society Study on Chronic Obstructive Pulmonary Disease.
Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. N Engl
J Med. 1999;340:1948–1953.
24. van der Woude HJ, Zaagsma J, Postma DS, et al. Detrimental effects of beta-blockers in COPD: a concern for nonselective beta-
blockers. Chest. 2005;127:818–824.
25. van Gestel YR, Hoeks SE, Sin DD, et al. Impact of cardioselective beta-blockers on mortality in patients with chronic obstructive
pulmonary disease and atherosclerosis. Am J Respir Crit Care Med. 2008;178:695–700.
26. van Gestel Y RBM, Hoeks SE, Sin DD, et al. Beta-blockers and health-related quality of life in patients with peripheral arterial disease
and COPD. Int J COPD. 2009;4:177–183.
27. Chen J, Radford MJ, Wang Y, et al. Effectiveness of beta-blocker therapy after acute myocardial infarction in elderly patients with
chronic obstructive pulmonary disease or asthma. J Am Coll Cardiol. 2001;37:1950–1956.
28. Centers for Disease Control and Prevention. Recommended adult immunization schedule—United States, 2010. MMWR Quick Guide.
2010;59(1):1-4. www.cdc.gov/mmwr/PDF/wk/mm5901-immunization.pdf. Accessed December 2, 2010.
29. Vestbo J, the TORCH Study Group. The TORCH (TOwards a Revolution in COPD Health) survival study protocol. Eur Respir J.
2004;24:206–210.
30. Tashkin DP, Celli B, Senn S, et al for the UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary
disease. N Engl J Med. 2008;359:1543–1554.
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (6 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
31. Tashkin DP. Impact of tiotropium on the course of moderate-to-very severe chronic obstructive pulmonary disease: the UPLIFT trial.
Expert Rev Resp Med. 2010;4:279–289.
32. Calverley PMA, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary
disease. N Engl J Med. 2007;356:775–789.
33. Keddissi JI, Younis WG, Chbeir EA, et al. The use of statins and lung function in current and former smokers. Chest. 2007;132:1764–
1771.
34. Søyseth V, Brekke PH, Smith P, et al. Statin use is associated with reduced mortality in COPD. Eur Respir J. 2007;29:279–283.
35. Frost FJ, Petersen H, Tollestrup K, et al. Influenza and COPD mortality protection as pleiotropic, dose-dependent effects of statins.
Chest. 2007;131:1006–1012.
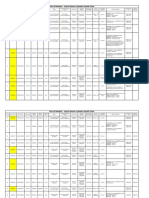
TABLE 1. Is it COPD? Key indicators to watch for
Consider chronic obstructive pulmonary disease (COPD) and perform spirometry, if any of these indicators are present in
an individual over age 40. These indicators are not diagnostic themselves, but the presence of multiple key indicators
increases the probability of a diagnosis of COPD. Spirometry is needed to establish a diagnosis of COPD.
Progressive (worsens over time)
Usually worse with exercise
Dyspnea that is:
Persistent (present every day)
Described by the patient as an “increased effort to breathe,” “heaviness,”
“air hunger,” or “gasping”
Chronic cough: May be intermittent and may be unproductive
Chronic sputum
Any pattern of chronic sputum production may indicate COPD
production:
Tobacco smoke
History of exposure to risk
Occupational dusts and chemicals
factors, especially:
Smoke from home cooking and heating fuels
SOURCE: Global Strategy for Diagnosis, Management, and Prevention of COPD. Global Initiative for Chronic Obstructive
Lung Disease (GOLD). Updated 2010. http://www.goldcopd.com/Guidelineitem.asp?l1=2&l2=1&intId=989. Accessed April
7, 2011. Reprinted with permission.
Figure 1. Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations*
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (7 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
*Postbronchodilator FEV1 is recommended for the diagnosis and assessment of severity of chronic obstructive pulmonary
disease.
SOURCE:Global Strategy for Diagnosis, Management, and Prevention of COPD. Global Initiative for Chronic Obstructive
Lung Disease (GOLD). Updated 2010. http://www.goldcopd.com/Guidelineitem.asp?l1=2&l2=1&intId=989. Accessed April
7, 2011. Reprinted with permission.
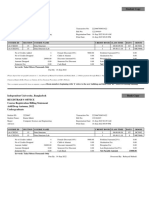
Figure 2. Exploring the Link Between COPD and Extrapulmonary Morbidities
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (8 of 9)4/13/11 4:51 PM
Focus on COPD (Issue I)
Patients with chronic obstructive pulmonary disease (COPD) have peripheral lung inflammation that may extend into
systemic circulation, leading to skeletal muscle weakness and cachexia and increasing propensity for cardiovascular,
metabolic, and bone diseases, and depression.
CCF, congestive cardiac failure; CRP, C-reactive protein; IHD, ischemic heart disease; IL, interleukin; SAA, serum amyloid
A; TNF, tumor necrosis factor.
SOURCE: Barnes PJ. Chronic obstructive pulmonary disease: effects beyond the lungs. PLoS Med. 2010;7(3):e1000220.
http://newsletter.qhc.com/jfp/JFP_COPDissue1.htm (9 of 9)4/13/11 4:51 PM
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- TOGAF 9 Foundation Part 1 Exam Preparation GuideDokument114 SeitenTOGAF 9 Foundation Part 1 Exam Preparation GuideRodrigo Maia100% (3)
- Photographing Shadow and Light by Joey L. - ExcerptDokument9 SeitenPhotographing Shadow and Light by Joey L. - ExcerptCrown Publishing Group75% (4)
- Report On Diversifying Clinical TrialsDokument79 SeitenReport On Diversifying Clinical TrialsSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- HTN and WomenDokument10 SeitenHTN and WomenSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Implantable Defrib Rill at orDokument8 SeitenImplantable Defrib Rill at orSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Report On Diversifying Clinical TrialsDokument79 SeitenReport On Diversifying Clinical TrialsSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Hayes EditorialDokument3 SeitenHayes EditorialSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- IJWH 7155 Optimal Management of Perimenopausal Depression 060810Dokument9 SeitenIJWH 7155 Optimal Management of Perimenopausal Depression 060810Sex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Womens Health Dental School Curriculum 2012Dokument81 SeitenWomens Health Dental School Curriculum 2012Sex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Women's Health Curriculum For Internal Medicine ResidentsDokument6 SeitenWomen's Health Curriculum For Internal Medicine ResidentsSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Pharmacy CurriculumDokument55 SeitenPharmacy CurriculumSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- ICSIDokument1 SeiteICSISex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Intro Gender Men MedDokument1 SeiteIntro Gender Men MedSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- MentaryDokument2 SeitenMentarySex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Integrating Gender Into Health Curriculum For Health ProfessionasDokument39 SeitenIntegrating Gender Into Health Curriculum For Health ProfessionasSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Hayes EditorialDokument3 SeitenHayes EditorialSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- HTTPDokument1 SeiteHTTPSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- HTN and WomenDokument10 SeitenHTN and WomenSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Gender Whats The DifferenceDokument5 SeitenGender Whats The DifferenceSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- HTNreviewDokument6 SeitenHTNreviewSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- GENDER GAPS in Medication 3.11.12Dokument1 SeiteGENDER GAPS in Medication 3.11.12Sex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Gender Perspective in MedicineDokument9 SeitenGender Perspective in MedicineSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- GenderBasic Final ReportDokument2 SeitenGenderBasic Final ReportSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- AMWA Gender Specific Position StatementDokument3 SeitenAMWA Gender Specific Position StatementSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- FDA - draftGuidanceonMedical DevicesDokument4 SeitenFDA - draftGuidanceonMedical DevicesSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- EvidenceDokument2 SeitenEvidenceSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Framework For SexAndGenderDokument1 SeiteFramework For SexAndGenderSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Expanding Frontiers UsDokument2 SeitenExpanding Frontiers UsSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Draft Guidance For Medical DevicesDokument16 SeitenDraft Guidance For Medical DevicesSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- Journal of The American College of Cardiology, Volume 43, Issue 5, Pages 900-921Dokument1 SeiteJournal of The American College of Cardiology, Volume 43, Issue 5, Pages 900-921Sex & Gender Women's Health CollaborativeNoch keine Bewertungen
- EvidenceDokument2 SeitenEvidenceSex & Gender Women's Health CollaborativeNoch keine Bewertungen
- CAS-GEC04 Module11 Food-SecurityDokument6 SeitenCAS-GEC04 Module11 Food-SecurityPermalino Borja Rose AnneNoch keine Bewertungen
- Whisper Flo XF 3 PhaseDokument16 SeitenWhisper Flo XF 3 Phasehargote_2Noch keine Bewertungen
- India: Kerala Sustainable Urban Development Project (KSUDP)Dokument28 SeitenIndia: Kerala Sustainable Urban Development Project (KSUDP)ADBGADNoch keine Bewertungen
- Nursing Care Management of a Client with Multiple Medical ConditionsDokument25 SeitenNursing Care Management of a Client with Multiple Medical ConditionsDeannNoch keine Bewertungen
- Petty Cash Vouchers:: Accountability Accounted ForDokument3 SeitenPetty Cash Vouchers:: Accountability Accounted ForCrizhae OconNoch keine Bewertungen
- Chem 102 Week 5Dokument65 SeitenChem 102 Week 5CAILA CACHERONoch keine Bewertungen
- Sri S T Kalairaj, Chairman: Income Tax TaxesDokument3 SeitenSri S T Kalairaj, Chairman: Income Tax TaxesvikramkkNoch keine Bewertungen
- Wasserman Chest 1997Dokument13 SeitenWasserman Chest 1997Filip BreskvarNoch keine Bewertungen
- CMC Ready ReckonerxlsxDokument3 SeitenCMC Ready ReckonerxlsxShalaniNoch keine Bewertungen
- Unit 1 TQM NotesDokument26 SeitenUnit 1 TQM NotesHarishNoch keine Bewertungen
- Evaluating MYP Rubrics in WORDDokument11 SeitenEvaluating MYP Rubrics in WORDJoseph VEGANoch keine Bewertungen
- AATCC 100-2004 Assesment of Antibacterial Dinishes On Textile MaterialsDokument3 SeitenAATCC 100-2004 Assesment of Antibacterial Dinishes On Textile MaterialsAdrian CNoch keine Bewertungen
- DNA Gel Electrophoresis Lab Solves MysteryDokument8 SeitenDNA Gel Electrophoresis Lab Solves MysteryAmit KumarNoch keine Bewertungen
- Why Genentech Is 1Dokument7 SeitenWhy Genentech Is 1panmongolsNoch keine Bewertungen
- Report Emerging TechnologiesDokument97 SeitenReport Emerging Technologiesa10b11Noch keine Bewertungen
- Guidelines On Occupational Safety and Health in Construction, Operation and Maintenance of Biogas Plant 2016Dokument76 SeitenGuidelines On Occupational Safety and Health in Construction, Operation and Maintenance of Biogas Plant 2016kofafa100% (1)
- Propiedades Grado 50 A572Dokument2 SeitenPropiedades Grado 50 A572daniel moreno jassoNoch keine Bewertungen
- Os PPT-1Dokument12 SeitenOs PPT-1Dhanush MudigereNoch keine Bewertungen
- Conv VersationDokument4 SeitenConv VersationCharmane Barte-MatalaNoch keine Bewertungen
- AFNOR IPTDS BrochureDokument1 SeiteAFNOR IPTDS Brochurebdiaconu20048672Noch keine Bewertungen
- Water Jet CuttingDokument15 SeitenWater Jet CuttingDevendar YadavNoch keine Bewertungen
- Final Thesis Report YacobDokument114 SeitenFinal Thesis Report YacobAddis GetahunNoch keine Bewertungen
- Algorithms For Image Processing and Computer Vision: J.R. ParkerDokument8 SeitenAlgorithms For Image Processing and Computer Vision: J.R. ParkerJiaqian NingNoch keine Bewertungen
- Panel Data Econometrics: Manuel ArellanoDokument5 SeitenPanel Data Econometrics: Manuel Arellanoeliasem2014Noch keine Bewertungen
- TDS Sibelite M3000 M4000 M6000 PDFDokument2 SeitenTDS Sibelite M3000 M4000 M6000 PDFLe PhongNoch keine Bewertungen
- Reg FeeDokument1 SeiteReg FeeSikder MizanNoch keine Bewertungen
- Family Service and Progress Record: Daughter SeptemberDokument29 SeitenFamily Service and Progress Record: Daughter SeptemberKathleen Kae Carmona TanNoch keine Bewertungen
- ERP Complete Cycle of ERP From Order To DispatchDokument316 SeitenERP Complete Cycle of ERP From Order To DispatchgynxNoch keine Bewertungen