Beruflich Dokumente
Kultur Dokumente
Bs Vitamins
Hochgeladen von
rin_ndOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bs Vitamins
Hochgeladen von
rin_ndCopyright:
Verfügbare Formate
The B Vitamins
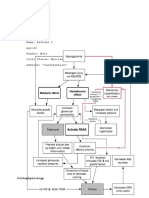
Thiamine Biochemical Functions: Thiamine pyrophosphate (TPP): involvement in energy metabolism functioning of the nervous system coenzyme (TPP) for aldehyde group metabolization with Mg. coenzyme (TPP) for pyruvate dehydrogenase and alpha keto glutarate dehydrogenase. needed to restore oxidized GSH Factors that decrease absorption: flavonoids, hydroxy-polyphenols, edema of small bowel (as in CHF), deficient folate or protein Nutrient interactions: High doses of thiamine may cause a relative deficiency of vitamin B6 or magnesium (Mg required to form TPP ) Thiamin depletion occurs from excess formaldehyde or any other items that go to aldehydes (alcohol, Candida, etc.) Candida and some raw fish put out Thiaminases that destroy thiamin in the gut. Thiamin deficiency increases the toxicity of PCB's, heptachlor and anilines. Food Sources: Whole-grain and enriched grain products, wheat germ, brewers yeast, organ meats, pork, legumes, seeds, nuts Deficiency Signs Neurological: General motor and sensory impairment: peripheral neuropathy (paresthesia), ataxia, decreased tendon reflexes Mental impairment: confabulation, disorientation, dementia Special Sensory Dysfunction: hypoguesesthesia, hyposmia , dysguesia, ophthalmoplegia Cardiovascular: Tachycardia, Heart Failure 20% of chemical sensitive pts. at the Environmental Health Center -Dallas were found to be deficient in thiamin Toxicity Signs: Thiamine is generally well tolerated. Several deaths (1 : 1.2 million) from intravenously administered thiamine have been reported, apparently from anaphylactic shock (acute Mg depletion? preservative?) Dosage and Administration: RDA: 1.4 mg qd range 50 200 mg
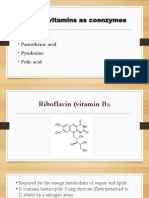
Riboflavin Riboflavin is a component of the coenzymes in various flavoprotein enzymes required for oxidation/reduction reaction. Biochemical Functions (FADH): involvement in carbohydrate metabolism cofactor for enzymes related to ocular tissues may help maintain tissue levels of reduced glutathione: used in glutathione reductase pathways which work with SOD to block free radical damage. works w/ Mb, Zn in oxidases and dehydrogenases (DH) necessary for the activation and conversion of many nutrients (see below) liver microsomal flavoproteins NADPH-cytochrome reductase supplies reducing equivalents to Cyto-P450 Factors that increase absorption: bile salts, HCl, Food Nutrient interactions: B6 activation folate N5methyl-THF Trp niacin retinal retinoic acid reduction of GSSGGSH (glutathione) choline metabolism: Choline DH, dimethylglycine (Deanol) DH, monomethylglycineDH Tyr dopamine dopamine, tyramine and histamine catabolism MAO Food Sources: milk, egg yolk, brewers yeast, royal jelly, meat, poultry, fish, dairy products, enriched bread and grain products Deficiency Signs: reddening of eyes, eyes that tire easily, bum, itch and are light sensitive, depression, hysteria, growth retardation Dermatological: alopecia, inflammation of mucus membranes of mouth: purple tinged glossitis, atrophic lingual papillae, angular cheilosis Deficiency is common with chronic alcoholism. 20% of chemical sensitivity pts at Environmental Health Center-Dallas have deficiency Toxicity Signs: None as riboflavin is generally well tolerated. Dosage and Administration: RDA: 1.2 mg qd range 50-400 mg Riboflavin excretion increases in DM, trauma, stress
Niacin/Niacinamide Niacin is involved in over 50 metabolic reactions that are related to energy release from carbohydrate. Nicotinamide is component of two related coenzymes NAD, NADP which are oxidized to NAD+ and NADP+, and are reduced to NADH and NADPH. Biochemical Functions: conversion from tryptophan GTF component energy metabolism: nicotinamide adenine dinucleotide (NAD+, NADH) normal brain function and serotonin metabolism. deamination of amino acids fatty acid synthesis Beta oxidation of fatty acids used in steroid formation drug metabolism Factors that increase absorption: folate Nutrient Interaction: combines with Glu for GTF reduces glutathione folate conversion Leuniacin synthesis by inhibited quinolinic acid synthesis from Trp niacin synthesis required vit B2, B6 DHAA AA isoniazid binds to phospholipoprotein pregnancy and oral contraceptives inhibit conversion from Trp Drug interaction: Concomitant use of HMG-CoA reductase inhibitors and high doses of niacin can cause rhabdomyolysis, particularly with atorvastatin (Lipitor) Pretreatment with aspirin may block the niacin flush. Niacin may potentiate the action of ganglionic blocking sgents and vasoactive drugs resulting in postural hypotension. Food sources: yeast, seeds Poultry, beef, fish, peanut butter, legumes, enriched and fortified grain products Deficiency Signs: The 4 Ds Dermatitis: Pigmentation, desquamation of sun-exposed areas; angular stomatitis, cheilosis, atrophic lingual papillae, glossitis Dementia Diarrhea Death Toxicity Signs: Niacin causes a transient skin flush with as little as 50 mg. Theoretically, niacin depletes available histamine with resulting in a decreased response with continued use (2 weeks or more). Large doses of niacin may increase or decrease blood sugar levels in some diabetics.
Elevated transaminases and, rarely, hepatitis may occur with doses of 3000 mg/day or more. Sustained release niacin is significantly more hepatotoxic than is regular niacin. Nausea may be an early warning sigh of hepatotoxicity in a patient on niacin therapy. Niacin has been reported to cause skin lesions similar in appearance to acanthosis nigricans, but not to actually cause this premalignant condition. Niacin may reactivate healed peptic ulcers or increase serum uric acid levels. IV niacin may cause vasodilation and hypotension.
Niacinamide does not cause flushing although it may also elevate liver enzymes. It does not cause the other side effects of niacin. Sustained-release niacinamide appears to be less hepatotoxic than sustained-release niacin. Thus, niacinamide is indicated for all conditions except for lipid lowering effects, vasodilation and dysmenorrhea. Inositol hexanicotinate does not cause a skin flush and has not been reported to cause hepatotoxicity in the doses used. It is generally well tolerated, however additional studies with larger groups of patients are needed to confirm the safety of this compound. Dosage and Administration: RDA: 13-18 mg qd. Doses range 50-500 mg. Alternate forms of niacin include niacinamide and inositol hexa-nicotinate, a compound which is hydrolyzed to form six molecules of niacin and one molecule of inositol. Stabilized NADH is available
Pantothenic Acid Biochemical Functions: formation of acetyl-CoA, which is used in the metabolism of amino acids, carbohydrates and lipids. Used in Acetylation and Acylation Nutrient Interaction: heme synthesis w/ Fe, B6; acylation of AA Food Sources: many foods Deficiency Signs: Because of its ubiquitous presence, deficiency generally is unheard of. Toxicity Signs: Doses as high as 10,000 mg/day have been used without apparent toxic effects, although more research needs to be done on higher doses. No significant toxicity has been reported with pantethine. Dosage and Administration: No established RDA, estimated requirement of 4-7 mg. The alcohol form is d-panthenol which is available form compounding pharmacies (Professional Arts Pharmacy 800-832-9285). Pantethine is a metabolite of pantothenic acid and also a precursor of acetyl-CoA.
Vitamin B6: Pyridoxal (PL), Pyridoxal 5 Phosphate (PLP), Pyridoxine (PN) Over 60 enzyme systems are dependent of B6 Biochemical Functions: energy metabolism nervous system function immune function homocysteine metabolism transamination Trp niacin pathway : 3-H dynurenine3OH anthranilate coenzyme for -aminolevulinate synthase: heme synthesis PLP coenzyme for cystathione synthase lysl oxidase cofactor with Cu2+ for collagen formation Factors that decrease absorption: Compounds that reduce available B6: oral contraceptives, alcohol, coffee, estrogen, tobacco other nutrients in a multiple may inactivate vitamin B6; therefore use a separate vitamin B6 product for therapeutic applications zinc Nutrient interactions: Required for niacin synthesis PN oxidase requires riboflavin PLP kinase requires Zn PL chelates Fe Fe uptake estrogen sulfate competes for DOPA carboxylase Food Sources: whole grains, navy beans, walnuts, potato, chicken, fish, liver, egg yolk, pork, kidney, soybeans, peanuts, walnuts Deficiency Signs Pigmentation, Angular stomatitis, Cheilosis, Atrophic lingual papillae Night blindness Heart failure, Macrocytic anemia Peripheral neuropathy, Ataxia, Dementia, Decreased tendon reflexes Green urine (If vitamin B 6 is deficient, xanthurenic acid is produced from tryptophan. Xanthurenic acid is excreted in the urine.) Deficiency will result in increased levels of Homocysteine (with folic acid) 60% of chemical sensitivity pts. at the Environmental Health Center-Dallas have been found to be deficient whether they are taking oral supplements or not. Low B6 can lead to low taurine; when taurine is low extreme sensitivities to chlorine, chlorite (bleach), aldehydes, alcohols,
solvents, and ammonia can develop. B6 deficiency also results in poor ability to conjugate epinephrine and serotonin. Toxicity Signs: At 500 mg/day or more for extended periods of time may cause sensory neuropathy in a stocking glove distribution which resides after discontinued use but may take up to a year to do so. Lower doses may cause insomnia, anxiety or bed-wetting which may be prevented by co-administration of magnesium. Doses of 120-600 mg/day have been reported to suppress lactation. Dosage Range: RDA: 2.0 mg. Therapeutic doses are 10-500 (rarely that high) mg/day. In regard to forms, most all research has used pyridoxine. The absorption of pyridoxine is near 100%. Theoretically, PLP may be more effective if the ability to convert pyridoxine is impaired, but PLP absorption may be poor required doses > 200 mg. Disease process that increase the need for vitamin B6 include: hyperthyroidism liver disease kidney disease chronic stress
Folic Acid Biochemical Functions: DNA metabolism (cellular replication) central nervous system function, immune function homocysteineMuscle energy technique More information from http://www.hscbklyn.edu/SUNY/Biochem/ALCOHOL/alcohol_folate_bkgd.html#folate_overview Food Sources: beer, wheat germ, yeast, liver, kidney, asparagus, Brussels sprouts, green leafies, legumes, seed oils. In foods, folic acid is found as pteroyl polyglutamate, which requires hydrolyzation prior to absorption. Folic acid supplements are single pteroyl glutamate molecule and are absorbed well on an empty stomach. Thus, supplements appear to be better utilized than folic acid from food. Factors that increase absorption: vitamin C, glutamate Zn dependent exopeptidases, glucose Factors that decrease absorption: conjugase inhibitors, zinc, food
Nutrient Interaction: ethanolamine choline niacin NANM required for niacin for conversion to TRP B12 prevents entrapment in methylated form vit C protects folate from oxidation *large doses may promote a deficiency of zinc or vitamin B 12 (as in pernicous anemia). In turn, large doses of zinc, vitamin B6 or B12 may increase the need for folic acid. If treatment requires >5 mg folic acid, administer a multiple vitamin with zinc. *Folate metabolism is the target for two therapeutic groups: folate antagonists (methotrexate) thymidylate synthase inhibitors (5-flyourouracil) Long term use of these medications can lead to folate depletion. In turn, the susceptibility to folate depletion caused by these drugs may be due to single nucleotide polymorphisms in the enzymes involved in folate metabolism. 5-formylmethyltetrahydrofolate may be a form of folic acid that can reduce toxicity of methotrexate as well as improve efficacy. Deficiency Signs: atrophic lingual papillae, glossitis, tachycardia and pallor secondary to macrocytic anemia Toxicity Signs: Large doses may promote seizures in epileptics. Dosage and Administration: RDA: 200 g; pregnancy 400 g; lactation 300 g. In regard to available dosages, 1 mg is the limit for manufacture. However, compounding pharmacies can produce and dose requested. Liquid preparations is another method for achieving higher doses easily.
Biotin Biochemical Functions: coenzyme in oxidation and chain elongation of fatty acids coenzyme in oxidation of carbohydrates Food Sources: Liver, egg yolk, soy flour, cereals, yeast Deficiency Signs: Deficiency is rare, if not unheard of. Deficiency may result from eating raw eggs due to the avidin content of egg whites which binds biotin into an indigestible compound Dosage and Administration: RDA 200 g , up to 8-16 mg Toxicity Signs: Generally well tolerated.
Cobalamins: Vitamin B-12 Biochemical Functions: Involved in DNA synthesis coenzyme for Met synthase: homocysteine Met adenosylcobalamin coenzyme for methylmalonyl CoA mutase: methylmalonyl succinyl CoA synthesis of SAMe involved in normal functioning of the nervous system and immune system. The methylated form, methylcobalamine inhibits the toxic effect of methylmercury on nerve fibers in animals (possibly by increasing phosphatidyl choline synthesis). B 12 and C have been shown to reduce Pb toxicity and CCl4 toxicity. B 12 with choline and inositol reverses Aflatoxin induced fatty liver. Food Sources: Fish, liver and organ meats, meat, poultry, cheese, yogurt, milk, eggs, bivalves Factors that increase absorption: intrinsic factor Factors that decrease absorption: C (>500mg C), Maybe Cu and thiamin (?) From food, not supplements, is inhibited by drugs that interfere with gastric acid secre-tion, antacids, potassium, citrate, chloride, colchicine, some oral hypoglycemic medications Nutrient interactions: prevents folate trap deficient B6 iron increases likelihood of deficient B12 Deficiency Signs: Cobalamin deficiency is more likely to occur in the elderly and may also occur vegans and patients with hypochlorhydria. tachycardia, pallor secondary to macrocytic anemia atrophic lingual papillae paleness, glossitis dementia peripheral neuropathy, ataxia, decreased tendon reflexes (in B 12 deficiency the myelin sheath is malformed. 15% of CS pts at the Environmental Heath Center in Dallas were found to be deficient in B 12. Dosage and Administration: RDA: 3g. Dosage is variable depending on route of administration and condition being treated. For most conditions, IM hydroxocobalamin 1 ml (1,000 g) is recommended. Hydroxocobalamin is longer acting and achieves higher serum levels than cyanocobalamin. Methylcobalamin has been used in some studies. Oral, sublingual or intranasal administration is usually not effective for conditions requiring high serum concentrations. However, large oral doses have been used successfully to treat pernicious anemia.
Das könnte Ihnen auch gefallen
- Secondary Hyperparathyroidism in CKDDokument52 SeitenSecondary Hyperparathyroidism in CKDLee Zhi Yong100% (3)
- Science Form 2 Chapter 5.5 - Acid and Alkali NoteDokument20 SeitenScience Form 2 Chapter 5.5 - Acid and Alkali NoteMiNH Hayat90% (21)
- Crosslinking Reagents Handbook PDFDokument56 SeitenCrosslinking Reagents Handbook PDFAlexandraPatricheNoch keine Bewertungen
- Water Soluble VitaminsDokument83 SeitenWater Soluble VitaminsSourabh KumarNoch keine Bewertungen
- Vitamin 20 JulyDokument33 SeitenVitamin 20 JulySafura IjazNoch keine Bewertungen
- Biochemistry FADokument48 SeitenBiochemistry FAJaankiNoch keine Bewertungen
- Vitamins and MineralsDokument91 SeitenVitamins and MineralsPyaesone AungNoch keine Bewertungen
- Water Soluble VitaminsDokument87 SeitenWater Soluble VitaminsSwosti ShresthaNoch keine Bewertungen
- Lipid Lowering AngentDokument22 SeitenLipid Lowering AngentDave BraveNoch keine Bewertungen
- Water Soluble Vitamins Lecture For 1st Year MBBS by DR Sadia HaroonDokument67 SeitenWater Soluble Vitamins Lecture For 1st Year MBBS by DR Sadia HaroonIMDCBiochem100% (2)
- 32 LN Water Soluble Vitamins II BLGDokument45 Seiten32 LN Water Soluble Vitamins II BLGDakshitha DharmakeerthiNoch keine Bewertungen
- 2 - Vitamin B ComplexDokument57 Seiten2 - Vitamin B ComplexPaulinNoch keine Bewertungen
- Vit B1,2,3 (Autosaved)Dokument23 SeitenVit B1,2,3 (Autosaved)lovi bahunNoch keine Bewertungen
- Drugs For HyperlipidemiaDokument29 SeitenDrugs For Hyperlipidemiasultan khabeebNoch keine Bewertungen
- VitaminsDokument96 SeitenVitaminskiedd_0480% (5)
- Vitamin B5: (Pantothenic Acid)Dokument53 SeitenVitamin B5: (Pantothenic Acid)Sagar BadnakheNoch keine Bewertungen
- Dr. Drg. Nur Permatasari, MS. Dr. Dian Nugrahenny, M.BiomedDokument24 SeitenDr. Drg. Nur Permatasari, MS. Dr. Dian Nugrahenny, M.BiomedTutde SedanaNoch keine Bewertungen
- Vitamin b52c b62cb72cb9b12 Final 1Dokument53 SeitenVitamin b52c b62cb72cb9b12 Final 1Anonymous zJcGQRnQCNoch keine Bewertungen
- Calcium Metabolism and RegulationDokument39 SeitenCalcium Metabolism and RegulationSanchita SahaNoch keine Bewertungen
- Metabolitos Azealaic AcidDokument4 SeitenMetabolitos Azealaic AcidGuillermo GonzalezNoch keine Bewertungen
- Sandomigran PiDokument6 SeitenSandomigran PiNexi anessaNoch keine Bewertungen
- Drugs Used in Gastrointestinal Diseases FinalDokument30 SeitenDrugs Used in Gastrointestinal Diseases FinalFaridah Yuwono 28Noch keine Bewertungen
- Intravenous Nutrient SolutionsDokument28 SeitenIntravenous Nutrient SolutionsElsayed AhmedNoch keine Bewertungen
- Diuretics: Generic Name: FUROSEMIDEDokument12 SeitenDiuretics: Generic Name: FUROSEMIDEJR BetonioNoch keine Bewertungen
- Nucleotide and CHO Metabolism ActivityDokument3 SeitenNucleotide and CHO Metabolism ActivityJanson SarmientoNoch keine Bewertungen
- Git Pepticulcer 150106043824 Conversion Gate01Dokument43 SeitenGit Pepticulcer 150106043824 Conversion Gate01NomanNoch keine Bewertungen
- Acute Poisoning Guidelines.Dokument7 SeitenAcute Poisoning Guidelines.Manoj KumarNoch keine Bewertungen
- B ComplexDokument25 SeitenB ComplexBimalKrishnaNoch keine Bewertungen
- 26 Pharmacology Anti-HyperlipidemiaDokument41 Seiten26 Pharmacology Anti-Hyperlipidemianisaauliasafitri03Noch keine Bewertungen
- Nutrition and Metabolism: Vitamins Presented Dr. Alhaji GblaDokument23 SeitenNutrition and Metabolism: Vitamins Presented Dr. Alhaji GblaAlhaji GblaNoch keine Bewertungen
- Git PharmacologyDokument73 SeitenGit PharmacologyShehu Baba AbdullahiNoch keine Bewertungen
- Generic Name: Brand Name: Drug Class: Chemical Structure:: Atorvastatin Lipitor StatinsDokument3 SeitenGeneric Name: Brand Name: Drug Class: Chemical Structure:: Atorvastatin Lipitor StatinsnivraeNoch keine Bewertungen
- Degradation of Purine PDFDokument36 SeitenDegradation of Purine PDFShrey SundriyalNoch keine Bewertungen
- Degradation of PurineDokument36 SeitenDegradation of PurineShrey SundriyalNoch keine Bewertungen
- PoisoningDokument23 SeitenPoisoningseed1876Noch keine Bewertungen
- Liver DiseaseDokument17 SeitenLiver DiseaseGANESH KUMAR JELLANoch keine Bewertungen
- VitaminsDokument20 SeitenVitaminssoumyajitchakraborty0238Noch keine Bewertungen
- Vitamin B2 - B6Dokument19 SeitenVitamin B2 - B6Biruk GeremewNoch keine Bewertungen
- Hypothalamic AgentsDokument9 SeitenHypothalamic Agentskeziah caraigNoch keine Bewertungen
- Drugs Trade Mechanism Indications Kinetics Ci/Ae Hypothalamic-Anterior Pituitary AxisDokument7 SeitenDrugs Trade Mechanism Indications Kinetics Ci/Ae Hypothalamic-Anterior Pituitary Axisrmiller8456161Noch keine Bewertungen
- NCMA216.PHARMA Drugs Acting On The Endocrine SystemDokument71 SeitenNCMA216.PHARMA Drugs Acting On The Endocrine SystemKhams TolentinoNoch keine Bewertungen
- M3 - Lesson 1bDokument20 SeitenM3 - Lesson 1bLhara MañoNoch keine Bewertungen
- CKD Case StudyDokument8 SeitenCKD Case StudyEspiridionNoch keine Bewertungen
- 12 Antilipemics UpdDokument46 Seiten12 Antilipemics Updone_nd_onlyuNoch keine Bewertungen
- Drug Study Case PresentationDokument5 SeitenDrug Study Case PresentationRobert MedinaNoch keine Bewertungen
- Gastrointestinal and Gastrointestinal and Antiemetic Drugs Antiemetic DrugsDokument34 SeitenGastrointestinal and Gastrointestinal and Antiemetic Drugs Antiemetic DrugsZakir UllahNoch keine Bewertungen
- Agents Used in HyperlipidemiaDokument37 SeitenAgents Used in HyperlipidemiacreativejoburgNoch keine Bewertungen
- Disorders of Purine and Pyrimidine MetabolismDokument17 SeitenDisorders of Purine and Pyrimidine MetabolismUbaid AhmedNoch keine Bewertungen
- Dyslipidemia 1Dokument57 SeitenDyslipidemia 1DR. MUSICNoch keine Bewertungen
- MigraineDokument16 SeitenMigraineTNoch keine Bewertungen
- Antidyslipidemic Drugs (Geppetti)Dokument32 SeitenAntidyslipidemic Drugs (Geppetti)Ariel OlshevskyNoch keine Bewertungen
- Peptic Ulcer Therapy - Antiemetics - Laxatives - Antidiarrheal DrugsDokument18 SeitenPeptic Ulcer Therapy - Antiemetics - Laxatives - Antidiarrheal Drugsmanik_ghadlingeNoch keine Bewertungen
- HyperlipidemiaDokument11 SeitenHyperlipidemiabil-bilNoch keine Bewertungen
- Purine MetabolismDokument30 SeitenPurine MetabolismSamarTharwatNoch keine Bewertungen
- Naturopathic Nutrition: Amino AcidsDokument28 SeitenNaturopathic Nutrition: Amino Acidsglenn johnston100% (1)
- Role of Vitamins As Coenzymes: Riboflavin Pantothenic Acid Pyridoxine Folic AcidDokument34 SeitenRole of Vitamins As Coenzymes: Riboflavin Pantothenic Acid Pyridoxine Folic AcidNeethu JohnNoch keine Bewertungen
- Hypolipidemic AgentsDokument15 SeitenHypolipidemic Agentsapi-3725624100% (1)
- Module 1 Part 5B. Parathyroid AgentsDokument21 SeitenModule 1 Part 5B. Parathyroid AgentsBSN2G- SABLA-ON LORRAINE ANNENoch keine Bewertungen
- Drug StudyDokument5 SeitenDrug Studyjanelle123 toribioNoch keine Bewertungen
- Biologically Important PeptidesDokument12 SeitenBiologically Important PeptidesRoopa RanganathanNoch keine Bewertungen
- Mcat Aamc Practice FLDokument7 SeitenMcat Aamc Practice FLDSNoch keine Bewertungen
- Soil Amendments and Fertilizers 2Dokument8 SeitenSoil Amendments and Fertilizers 2FxNoch keine Bewertungen
- CR Lab ReportDokument6 SeitenCR Lab ReportslowteeNoch keine Bewertungen
- Tego Sto 85 V 0712 en 2000 IfDokument2 SeitenTego Sto 85 V 0712 en 2000 Ifyuncyd100% (1)
- Acid Dissociation ConstantDokument4 SeitenAcid Dissociation ConstantJair RangelNoch keine Bewertungen
- Dna and Rna DLLDokument2 SeitenDna and Rna DLLHeidie BalabboNoch keine Bewertungen
- J.M. Cowie, Polymers SynthesisDokument25 SeitenJ.M. Cowie, Polymers SynthesisKoNi ChiWaNoch keine Bewertungen
- Gene Xpert FinalDokument10 SeitenGene Xpert FinalQaiser ZamanNoch keine Bewertungen
- Stereochemistry Sem 1 2013Dokument82 SeitenStereochemistry Sem 1 2013Vaibhav RanaNoch keine Bewertungen
- Rate OF Hydration Propylene: Ss INSTDokument71 SeitenRate OF Hydration Propylene: Ss INSTMateo VanegasNoch keine Bewertungen
- Hydrogenation of AromaticDokument6 SeitenHydrogenation of AromatickyucheolpaikNoch keine Bewertungen
- PC 20166Dokument10 SeitenPC 20166chopin.wlive.cnNoch keine Bewertungen
- Student Copy True Lipids TrueDokument113 SeitenStudent Copy True Lipids TrueSree Balaji Srinivas KatakamNoch keine Bewertungen
- Photosynthesis in Higher PlantsDokument22 SeitenPhotosynthesis in Higher PlantsHappy PalNoch keine Bewertungen
- Baze de Supozitor PDFDokument6 SeitenBaze de Supozitor PDFLucescu GiuliaNoch keine Bewertungen
- Future Pipe InfoDokument29 SeitenFuture Pipe Infomekag94Noch keine Bewertungen
- Effect of Sugarcane Pressmud Biocompost On Dry Matter Yield and Nutrient Uptake in MaizeDokument6 SeitenEffect of Sugarcane Pressmud Biocompost On Dry Matter Yield and Nutrient Uptake in MaizeNeneng May PutriNoch keine Bewertungen
- Chap. 5 Molecular Genetic Techniques: TopicsDokument28 SeitenChap. 5 Molecular Genetic Techniques: TopicsanushkaNoch keine Bewertungen
- The Chemistry of Benzene: A Guide For A Level StudentsDokument23 SeitenThe Chemistry of Benzene: A Guide For A Level Studentsjules blancoNoch keine Bewertungen
- Types of CoagulantsDokument3 SeitenTypes of CoagulantsBurhanNoch keine Bewertungen
- Lesson-16 Procedures For DNA RAN and Mitochondria DemonstrationDokument6 SeitenLesson-16 Procedures For DNA RAN and Mitochondria DemonstrationSasa AbassNoch keine Bewertungen
- Whole Foods ComplaintDokument13 SeitenWhole Foods ComplaintLaw&CrimeNoch keine Bewertungen
- TestDokument19 SeitenTestCikgu AnitaNoch keine Bewertungen
- Problem Sheet BIOL1XX7 Module1 2021Dokument5 SeitenProblem Sheet BIOL1XX7 Module1 2021Jui-Chi ChenNoch keine Bewertungen
- Oxidation of Fatty AcidsDokument15 SeitenOxidation of Fatty AcidsMomena SafdarNoch keine Bewertungen
- Literature Reviewof Poly Lactic AcidDokument23 SeitenLiterature Reviewof Poly Lactic AcidSamirisNoch keine Bewertungen
- Robert M. Strongin, Jiries Meehan-Atrash, Monica Vialpando - Recent Advances in The Science of Cannabis-CRC Press (2021)Dokument293 SeitenRobert M. Strongin, Jiries Meehan-Atrash, Monica Vialpando - Recent Advances in The Science of Cannabis-CRC Press (2021)Régis ChiconNoch keine Bewertungen
- PyridineDokument16 SeitenPyridineMuhammad AliAliNoch keine Bewertungen