Beruflich Dokumente
Kultur Dokumente
Pulmonary Embolus (PE)
Hochgeladen von
Heidi M FischerOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pulmonary Embolus (PE)
Hochgeladen von
Heidi M FischerCopyright:
Verfügbare Formate
Pulmonary Embolism (PE)
Obstruction of the pulmonary arterial bed by a dislodged thrombus, which may be fatal. Complication of venous thromboembolism.
Aetiology DVT and all associated risk factors. Untreated acute proximal DVT causes clinical PE in 33-50% of
patients. Atrial fibrillation Valvular heart disease
Pathophysiology A thrombus arising from DVT dislodges, travels through the bloodstream (large veins & vena cava)
and through the right atrium into the lungs, lodging in the arterial bed of the lungs. After traveling to the lung, large thrombi can lodge at the bifurcation of the main pulmonary artery or the lobar branches and cause hemodynamic compromise. Smaller thrombi typically travel more distally, occluding smaller vessels in the lung periphery. Mechanical obstruction of the pulmonary circulation leads to reflex vasoconstriction due to release of vasoactive agents (ie, serotonin) by platelets. The arterial obstruction increases alveolar dead space and leads to redistribution of blood flow, thus impairing gas exchange due to the creation of low ventilation-perfusion areas within the lung. Obstruction of pulmonary blood flow by an embolus causes reflex bronchoconstriction in the affected area of the lung, augmenting airway resistance and leading to impaired gas exchange and loss of alveolar surfactant. The increased pulmonary vascular resistance causes an increase in right ventricular afterload, and tension rises in the right ventricular wall, which may lead to dilatation, dysfunction, and ischemia of the right ventricle. The result is right heart failure, cardiogenic shock and even death.
Clinical Manifestations
Diagnosis of PE can be difficult because classic signs and symptoms are often absent in patients and it can mimic other diseases, such as pneumonia. The "classic" presentation with abrupt onset of pleuritic chest pain, shortness of breath, and hypoxia is rarely seen. A thorough history and physical examination often provide the first clue for early diagnosis of PE. History: acute onset of shortness of breath; sometimes able to pinpoint the moment of distress. May have signs of deep venous thrombosis, lower extremity swelling and warmth to touch or tenderness. Tachypnea (respiratory rate _ 20 breaths/min) Dyspnea Tachypnea (more than 18 breaths per minute) Tachycardia (heart rate >100 bpm) Pleuritic or central chest pain Cyanosis Hemoptysis Sudden collapse Cough Sweating Pyrexia may be present Patients with massive pulmonary embolism are in shock. They have systemic hypotension, poor perfusion of the extremities, tachycardia, and tachypnea. In addition, patients appear weak, pale, sweaty, and oliguric and develop impaired mentation. Very high fatality rate (About 1/3 of PE cases are fatal) most people dying from PE do so in the first 30 minutes. If a patient is thought to have PE or has documented PE, the absence of tenderness, erythema, edema, or a palpable cord upon examination of the lower extremities does not rule out
thrombophlebitis, nor does it imply a source other than a leg vein. More than two thirds of patients with proven PE lack any clinically evident phlebitis. Nearly one third of patients with proven PE have no identifiable source of DVT, despite a thorough investigation. DVTs can lie undetected within the deep venous system of the lower extremity and pelvis in 90% of cases.
Diagnosis
Imaging studies: Chest radiograph: findings most often are normal. Doppler ultrasonography: can evidence the presence of thrombus within a vein Pulmonary angiography: diagnostic criterion standard, which allows for the visualization of the pulmonary vasculature using contrast material. Evidences a cutoff of a vein and lack of flow to the affected area. Ventilation-perfusion scanning: most common screening technique. Helical (spiral) CT scanning Contrast venography: invasive technique that can provide direct proof of thrombus by demonstrating a filling defect with the aide of contrast medium through the deep venous system Echocardiography can demonstrate signs of right heart strain and can be used to identify signs of impending heart failure. Electrocardiography is of greatest value in ruling out myocardial infarction. Chest computed tomography Laboratory studies: D-dimer test: D-dimers are degradation products of cross-linked fibrin by plasmin and levels may be elevated in any medical condition where clots form (trauma, recent surgery, hemorrhage, cancer, and sepsis). D-dimer test can be used as a rapid screening measure in cases where leg swelling exists in the face of equivocal or negative clinical or radiologic findings. Additional blood work: coagulation studies to evaluate for a hypercoagulable state. ABGs: hypoxemia, hypocapnia, and respiratory alkalosis WBC count: may be normal or elevated (as high as 20,000) Serum troponin levels can be elevated due to acute right ventricular myocardial stretch Patients suspected of having pulmonary embolismbecause of unexplained dyspnea, tachypnea, or chest pain or the presence of risk factors for pulmonary embolismmust undergo diagnostic tests until the diagnosis is ascertained or eliminated or an alternative diagnosis is confirmed.
Nursing Intervention
ABC O2 therapy via cannula or mask; patient may need ventilation if lungs are severely compromised Monitor ABG levels Monitor coagulation studies and monitor for bleeding when on anti coagulants Analgesia See DVT nursing care for other considerations and patient education
Pharmacology
Immediate full anticoagulation is mandatory for all patients suspected to have DVT. Anticoagulant therapy Heparin is the first line of therapy. It is administered by bolus dosing, followed by a continuous infusion. A short course of heparin is followed by a longer course of oral anticoagulant, warfarin sodium. It should be started only after effective anticoagulation has been achieved, as there can be an increase in coagulability and thrombogenesis during the first few days of oral anticoagulant administration. The goal is to achieve an international normalized ratio (INR) of 2.0-3.0. Thrombolytic therapy Thrombolytic therapy dissolves recent clots promptly by activating a plasma proenzyme, plasminogen, to its active form, plasmin. Plasmin degrades fibrin to soluble peptides. Thrombolytic therapy speeds pulmonary tissue reperfusion and rapidly reverses the right heart failure. It
improves pulmonary capillary blood flow and more rapidly improves hemodynamic parameters. contraindications to thrombolysis include gastrointestinal bleeding within the last 6 months, active or recent internal bleeding, a history of hemorrhagic stroke, intracranial or intraspinal disease, recent cranial surgery or head trauma, and pregnancy. Other: The vena caval filter is designed to trap potentially lethal emboli while maintaining vena caval patency. It is indicated in cases where there is a contraindication to anticoagulation, when there has been a complication of anticoagulation, in the event of failure of anticoagulation, and in the case of pulmonary embolectomy. References: De Palo, V. A. (2010). Thromboembolism. Retrieved from http://emedicine.medscape.com/article/1267714-overview Gaspard, K. J. (2009). Disorders of hemostasis. In C. M. Porth & G. Matfin (Eds.), Pathophysiology: Concepts of altered health states (8th ed., pp. 262-277). Philadelphia, PA: Wolters Kluwer Health, Lippincott Williams & Wilkins. Matfin, G. (2009). Disorders of blood flow in the systemic circulation. In C. M. Porth & G. Matfin (Eds.), Pathophysiology: Concepts of altered health states (8th ed., pp. 477-504). Philadelphia, PA: Wolters Kluwer Health, Lippincott Williams & Wilkins. Morrison, R. (2006). Venous thromboembolism: Scope of the problem and the nurses role in risk assessment and prevention. Journal of Vascular Nursing 24(3), 82-90. doi:10.1016/j.jvn.2006.05.002 Ouelette, D. R. (2011). Pulmonary embolism. Retrieved from http://emedicine.medscape.com/article/300901-overview Patel, K. (2011). Deep venous thrombosis. Retrieved from http://emedicine.medscape.com/article/1911303-overview Pooler, C. (2009). Disorders of ventilation and gas exchange. In C. M. Porth & G. Matfin (Eds.), Pathophysiology: Concepts of altered health states (8th ed., pp. 701-738). Philadelphia, PA: Wolters Kluwer Health, Lippincott Williams & Wilkins.
Das könnte Ihnen auch gefallen
- Pulmonary EmbolismDokument5 SeitenPulmonary EmbolismKian Justin HidalgoNoch keine Bewertungen
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtVon EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtBewertung: 5 von 5 Sternen5/5 (1)
- Acute Pulmonary ThromboembolismDokument37 SeitenAcute Pulmonary ThromboembolismОльга КоваленкоNoch keine Bewertungen
- Venous Thromboembolic DiseaseDokument27 SeitenVenous Thromboembolic DiseaseAndra BauerNoch keine Bewertungen
- Pulmonary EmbolismDokument48 SeitenPulmonary Embolismganga2424100% (3)
- Lungs 3Dokument60 SeitenLungs 3Surya L KNoch keine Bewertungen
- Pulmonary EmbolismDokument16 SeitenPulmonary EmbolismEhab Mokhtar WehebaNoch keine Bewertungen
- Pulmonary EmbolismDokument96 SeitenPulmonary Embolismsamice5100% (1)
- Pleural EffusionDokument24 SeitenPleural Effusionalyas alyasNoch keine Bewertungen
- HemothoraxDokument27 SeitenHemothoraxShreyasi AnkushNoch keine Bewertungen
- Prepared:: Mardin Mazhar Shanga IsmailDokument34 SeitenPrepared:: Mardin Mazhar Shanga IsmailAhmed HassanNoch keine Bewertungen
- Pulmonary EmbolismDokument47 SeitenPulmonary EmbolismmalathiNoch keine Bewertungen
- Pulmonary ThromboembolismDokument4 SeitenPulmonary ThromboembolismValerrie NgenoNoch keine Bewertungen
- HemoptysisDokument35 SeitenHemoptysisElad MizrahiNoch keine Bewertungen
- Pericardial EffusionDokument26 SeitenPericardial EffusionjsenocNoch keine Bewertungen
- Efusi PleuraDokument9 SeitenEfusi PleuraYoseph Alam NaibahoNoch keine Bewertungen
- Chest InjuryDokument19 SeitenChest InjuryWild GrassNoch keine Bewertungen
- PneumothoraxDokument5 SeitenPneumothoraxSaiful UmamNoch keine Bewertungen
- Pleuraleffusion 160424141916Dokument20 SeitenPleuraleffusion 160424141916Jessa AdenigNoch keine Bewertungen
- Critical Management For Pulmonary EmbolismDokument37 SeitenCritical Management For Pulmonary EmbolismNurse TethaNoch keine Bewertungen
- HemoptysisDokument30 SeitenHemoptysisMarshall ThompsonNoch keine Bewertungen
- HematothoraxDokument15 SeitenHematothoraxmail junkNoch keine Bewertungen
- Oncologic Mechanical Emergencies 2014 Emergency Medicine Clinics of North AmericaDokument14 SeitenOncologic Mechanical Emergencies 2014 Emergency Medicine Clinics of North AmericamarcosjuniormutucaNoch keine Bewertungen
- Cyanotic Heart DiseaseDokument66 SeitenCyanotic Heart DiseasePrasanth SankarNoch keine Bewertungen
- Oncologicmechanical Emergencies: Umar A. Khan,, Carl B. Shanholtz,, Michael T. MccurdyDokument14 SeitenOncologicmechanical Emergencies: Umar A. Khan,, Carl B. Shanholtz,, Michael T. MccurdySandra PargaNoch keine Bewertungen
- Hemoptysis: Bahman Saatian, M.DDokument57 SeitenHemoptysis: Bahman Saatian, M.DRovanNoch keine Bewertungen
- Deep Venous Thrombosis and Pulmonary ThromboembolismDokument19 SeitenDeep Venous Thrombosis and Pulmonary ThromboembolismTaqdees ManzoorNoch keine Bewertungen
- Nursing Acn-IiDokument80 SeitenNursing Acn-IiMunawar100% (6)
- Venous Thromboembolism LumabanDokument17 SeitenVenous Thromboembolism LumabanBEA RADANoch keine Bewertungen
- Pulmonary Thromboembolism: DR Olubunmi Ogunlade Consultant PulmonologistDokument34 SeitenPulmonary Thromboembolism: DR Olubunmi Ogunlade Consultant PulmonologistEmeka Chinedu Precious PetrousNoch keine Bewertungen
- Apasi Yg Ga Buat NisaDokument20 SeitenApasi Yg Ga Buat Nisamuhammad iqbal mahfuzhNoch keine Bewertungen
- Chest Injury and Its TypesDokument14 SeitenChest Injury and Its TypesKoochi PoojithaNoch keine Bewertungen
- Pulmonary ThromboembolismDokument61 SeitenPulmonary ThromboembolismsanjivdasNoch keine Bewertungen
- Pleura Effusion Bahan Kuliah PakarDokument27 SeitenPleura Effusion Bahan Kuliah PakarAfifah NaurahNoch keine Bewertungen
- Pleura Effusion Bahan Kuliah PakarDokument27 SeitenPleura Effusion Bahan Kuliah PakarRudy LusmiandaNoch keine Bewertungen
- Pulmonary Embolism: by Odinaka EdebeatuDokument25 SeitenPulmonary Embolism: by Odinaka EdebeatudidiNoch keine Bewertungen
- Pulmonary EmbolismDokument9 SeitenPulmonary EmbolismcbnhvpqpgrNoch keine Bewertungen
- Acute Pulmonary EmbolismDokument82 SeitenAcute Pulmonary Embolismincredible Prages100% (1)
- Interpretation of Chest Imaging1Dokument91 SeitenInterpretation of Chest Imaging1Brooke TurnerNoch keine Bewertungen
- Cardio-Respiratory Conditions: by DR Priscus MushiDokument73 SeitenCardio-Respiratory Conditions: by DR Priscus MushiMusaNoch keine Bewertungen
- Cardiac Tamponade (Suryani)Dokument72 SeitenCardiac Tamponade (Suryani)Hamdani UsmanNoch keine Bewertungen
- Cor Pulmonale IkaDokument19 SeitenCor Pulmonale IkaIka Lukita SariNoch keine Bewertungen
- Pe in HospitalDokument5 SeitenPe in HospitalAbdiaziz WalhadNoch keine Bewertungen
- Pulmonary EmbolismDokument23 SeitenPulmonary EmbolismBianca Dizon0% (1)
- Pericarditis AbDokument39 SeitenPericarditis AbAbnet WondimuNoch keine Bewertungen
- Practice Essentials of Pulmonary ThromboembolismDokument39 SeitenPractice Essentials of Pulmonary ThromboembolismEzzat Abdelhafeez SalemNoch keine Bewertungen
- Pulmonary EmbolismDokument5 SeitenPulmonary EmbolismNica Duco100% (2)
- Lung PathologyDokument101 SeitenLung Pathologyhm3398Noch keine Bewertungen
- Care of Patient With Pulmonary EmbolismDokument19 SeitenCare of Patient With Pulmonary Embolismtankmp100% (1)
- Pleural EffusionsDokument41 SeitenPleural Effusionssanjivdas100% (1)
- 16 - Venous ThromboembolismDokument2 Seiten16 - Venous ThromboembolismLenard BangugNoch keine Bewertungen
- Cardiac TemponadeDokument18 SeitenCardiac TemponadeDIVYA GANGWAR100% (1)
- Massive Hemoptysis: Resident Grand RoundsDokument7 SeitenMassive Hemoptysis: Resident Grand RoundsEko CahyonoNoch keine Bewertungen
- Pleural EffusionsDokument49 SeitenPleural Effusionsdale 99Noch keine Bewertungen
- Pleural Effusion 23-24Dokument21 SeitenPleural Effusion 23-24bazyan3aNoch keine Bewertungen
- Pleural Effusion: DR - Md.Toufiqur RahmanDokument22 SeitenPleural Effusion: DR - Md.Toufiqur RahmanBitu JaaNoch keine Bewertungen
- Pulmonary Hypertension: Saurabh Biswas PGT, Dept. of Chest Medicine, CNMCHDokument59 SeitenPulmonary Hypertension: Saurabh Biswas PGT, Dept. of Chest Medicine, CNMCHbsaurabh20Noch keine Bewertungen
- Pulmonaryembolism 150329161109 Conversion Gate01Dokument60 SeitenPulmonaryembolism 150329161109 Conversion Gate01Rafika RaraNoch keine Bewertungen
- Cardiac TamponadeDokument43 SeitenCardiac TamponadeMădălina GreereNoch keine Bewertungen
- Nadi Pariksha or Pulse DiagnosisDokument2 SeitenNadi Pariksha or Pulse Diagnosisshenali nadeeshaNoch keine Bewertungen
- Dermatology For The Small Animal Practitioner (Made Easy Series)Dokument163 SeitenDermatology For The Small Animal Practitioner (Made Easy Series)Nela Frade0% (1)
- Dance TherapyDokument17 SeitenDance TherapySaheli Mukherjee100% (3)
- 1236-Article Text-3136-1-10-20190909Dokument5 Seiten1236-Article Text-3136-1-10-20190909asmita sainiNoch keine Bewertungen
- PILEX001.DOC: Pilex - Clinical Reports Index Sl. No - File Name Title & Authors Detail Jour., Vol., (No.), PP YearDokument8 SeitenPILEX001.DOC: Pilex - Clinical Reports Index Sl. No - File Name Title & Authors Detail Jour., Vol., (No.), PP YearAbdul Rehman KhanNoch keine Bewertungen
- Theories of Counselling 5033: EducationDokument10 SeitenTheories of Counselling 5033: EducationheymuraliusNoch keine Bewertungen
- 10 1111@pan 13517Dokument9 Seiten10 1111@pan 13517MudrikaNoch keine Bewertungen
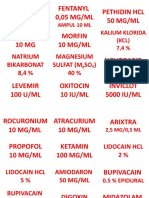
- Label ObatDokument31 SeitenLabel ObatAndiTenriBayangNoch keine Bewertungen
- Voice Therapy ExercisesDokument2 SeitenVoice Therapy ExercisesYudhi EkaputraNoch keine Bewertungen
- MASS102714Dokument29 SeitenMASS102714Pro PaletteNoch keine Bewertungen
- Course: B.Pharm Class: 3 Year Subject: Medicinal Chemistry-I Chapter-1: Basic Principles of Medicinal ChemistryDokument9 SeitenCourse: B.Pharm Class: 3 Year Subject: Medicinal Chemistry-I Chapter-1: Basic Principles of Medicinal ChemistryAnanda VijayasarathyNoch keine Bewertungen
- Hospital Follow Up Progress Note MedicalTemplateDokument1 SeiteHospital Follow Up Progress Note MedicalTemplatee-MedTools100% (18)
- Neurologija SkripticaDokument26 SeitenNeurologija SkripticaLazar VučetićNoch keine Bewertungen
- Price Controls and EntryDokument33 SeitenPrice Controls and EntryplatinumadNoch keine Bewertungen
- Masteral PeplauDokument20 SeitenMasteral PeplauGinger Enireht HTaibNoch keine Bewertungen
- National Mental Health ProgramDokument18 SeitenNational Mental Health ProgramDIYA DINDANoch keine Bewertungen
- Comparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile Seizures PDFDokument5 SeitenComparison of The Effects of Clobazam and Diazepam in Prevention of Recurrent Febrile Seizures PDFCharina Geofhany DeboraNoch keine Bewertungen
- Case Based Pediatrics For Medical Students and ResidentsDokument6 SeitenCase Based Pediatrics For Medical Students and Residentssantosaerwin6591100% (1)
- Guidance ServicesDokument7 SeitenGuidance ServicesJosephine Princess Ibanez SantosNoch keine Bewertungen
- What Doctors Dont Tell You - Good Sight Guide PDFDokument90 SeitenWhat Doctors Dont Tell You - Good Sight Guide PDFMircea OpreaNoch keine Bewertungen
- Ethical DilemmasDokument6 SeitenEthical DilemmasNada Al AyoubiNoch keine Bewertungen
- Selvini - Hypothesizing-Circularity-Neutrality - Three Guidelines For The Conductor of The Session PDFDokument7 SeitenSelvini - Hypothesizing-Circularity-Neutrality - Three Guidelines For The Conductor of The Session PDFAlejandro Arquillos Álvarez100% (1)
- Ulcerative ColitisDokument9 SeitenUlcerative ColitisBheru LalNoch keine Bewertungen
- Bereavement: Coping With A DeathDokument28 SeitenBereavement: Coping With A DeathTheresa SuleNoch keine Bewertungen
- What Is Coaching PDFDokument3 SeitenWhat Is Coaching PDFnicoletagr2744Noch keine Bewertungen
- JWC EWMA Supplement NPWT Jan 2018 AppendixDokument155 SeitenJWC EWMA Supplement NPWT Jan 2018 AppendixirwanchemNoch keine Bewertungen
- BuscogastDokument1 SeiteBuscogastSubrahmanyam KarnaNoch keine Bewertungen
- Kimberli Case StudyDokument4 SeitenKimberli Case StudyLLLJJJ100% (3)
- Treatment Approaches in Management of StutteringDokument46 SeitenTreatment Approaches in Management of StutteringKUNNAMPALLIL GEJO JOHN100% (1)
- Dr. Smith's ECG Blog - "Shark Fin" - A Deadly ECG Sign That You Must Know! PDFDokument7 SeitenDr. Smith's ECG Blog - "Shark Fin" - A Deadly ECG Sign That You Must Know! PDFZACHARIAH MANKIRNoch keine Bewertungen
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisVon EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisBewertung: 5 von 5 Sternen5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainVon EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainBewertung: 4 von 5 Sternen4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedBewertung: 4 von 5 Sternen4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (45)