Beruflich Dokumente
Kultur Dokumente
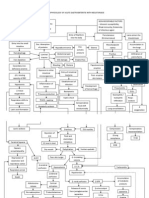
Pathophysiology of Gastritis
Hochgeladen von
Florsean Mae SalaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pathophysiology of Gastritis
Hochgeladen von
Florsean Mae SalaCopyright:
Verfügbare Formate
Pathophysiology Acute gastritis has a number of causes, including certain drugs; alcohol; bile; ischemia; bacterial, viral, and
fungal infections; acute stress (shock); radiation; allergy and food poisoning; and direct trauma. The common mechanism of injury is an imbalance between the aggressive and the defensive factors that maintain the integrity of the gastric lining (mucosa). Acute erosive gastritis can result from the exposure to a variety of agents or factors. This is referred to as reactive gastritis. These agents/factors include nonsteroidal anti-inflammatory medications (NSAIDs), alcohol, cocaine, stress, radiation, bile reflux, and ischemia. The gastric mucosa exhibits hemorrhages, erosions, and ulcers. NSAIDs, such as aspirin, ibuprofen, and naproxen, are the most common agents associated with acute erosive gastritis. This results from oral or systemic administration of these agents either in therapeutic doses or in supratherapeutic doses. Because of gravity, the inciting agents lie on the greater curvature of the stomach. This partly explains the development of acute gastritis distally on or near the greater curvature of the stomach in the case of orally administered NSAIDs. However, the major mechanism of injury is the reduction in prostaglandin synthesis. Prostaglandins are chemicals responsible for maintaining mechanisms that result in the protection of the mucosa from the injurious effects of the gastric acid. Long-term effects of such ingestions can include fibrosis and stricture. Bacterial infection is another cause of acute gastritis. The corkscrew-shaped bacterium called H pylori is the most common cause of gastritis. Complications result from a chronic infection rather than from an acute infection. The prevalence of H pylori in otherwise healthy individuals varies depending on age, socioeconomic class, and country of origin. The infection is usually acquired in childhood. In the Western world, the number of people infected with H pylori increases with age. Evidence of H pylori infection can be found in 20% of individuals younger than 40 years and in 50% of individuals older than 60 years. How the bacterium is transmitted is not entirely clear. Transmission is likely from person to person through the oral-fecal route or through the ingestion of contaminated water or food. This is why the prevalence is higher in lower socioeconomic classes and in developing countries. H pylori is associated with 60% of gastriculcersand80%ofduodenalulcers. H pylori gastritis typically starts as an acute gastritis in the antrum, causing intense inflammation, and over time, it may extend to involve the entire gastric mucosa resulting in chronic gastritis. The acute gastritis encountered with H pylori is usually asymptomatic. The bacterium imbeds itself in the mucous layer, a protective layer that coats the gastric mucosa. It protects itself from the acidity of the stomach through the production of large amounts of urease, an enzyme that catalyzes the breakdown of urea to the alkaline ammonia and carbon dioxide. The alkaline ammonia neutralizes the gastric acid in the immediate vicinity of the bacterium conferring protection. H pylori also has flagella that enable it to move and help it to penetrate the mucous layer so that it comes into contact with gastric epithelial cells. It also has several adhesions that help it to adhere to these cells. It produces inflammation by activating a number of toxins and enzymes that activate IL-8, which eventually attracts polymorphs and monocytes that cause acute gastritis. Antigen-presenting cells activate lymphocytes and other mononuclear cells that lead to chronic superficial gastritis. The infection is established within a few weeks after the primary exposure to H pylori. It produces inflammation via the production of a number of toxins and enzymes. The intense inflammation can result in the loss of gastric glands responsible for the production of acid. This is referred to as atrophic gastritis. Consequently, gastric acid production drops. The virulence genotype of the microbe is an important determinant for the severity of the gastritis and the formation of intestinal metaplasia, the transformation of gastric epithelium. This transformation can lead to gastric cancer. Reactive gastropathy is the second most common diagnosis made on gastric biopsy specimens after H pylori gastritis. This entity is believed to be secondary to bile reflux and was originally reported after partial gastrectomy (Billroth I or II). It is now considered to represent a nonspecific response to a variety of other gastric irritants. Helicobacter heilmanii is a gram-negative, tightly spiraled, helical-shaped organism with 5-7 turns. The prevalence of H heilmanii is extremely low (0.25-1.5%). The source of H heilmanii infection is unclear, but animal contact is thought to be the means of transmission. Tuberculosis is a rare cause of gastritis, but an increasing number of cases have developed because of patients who are immunocompromised. Gastritis caused by tuberculosis is generally associated with pulmonary or disseminated disease.
Secondary syphilis of the stomach is a rare cause of gastritis. Phlegmonous gastritis is an uncommon form of gastritis caused by numerous bacterial agents, including streptococci, staphylococci, Proteus species, Clostridium species, and Escherichia coli. Phlegmonous gastritis usually occurs in individuals who are debilitated. It is associated with a recent large intake of alcohol, a concomitant upper respiratory tract infection, and AIDS. Phlegmonous means a diffuse spreading inflammation of or within connective tissue. In the stomach, it implies infection of the deeper layers of the stomach (submucosa and muscularis). As a result, purulent bacterial infection may lead to gangrene. Phlegmonous gastritis is rare. The clinical diagnosis is usually established in the operating room, as these patients present with an acute abdominal emergency requiring immediate surgical exploration. Without appropriate therapy, it progresses to peritonitis and death. Viral infections can cause gastritis. Cytomegalovirus (CMV) is a common viral cause of gastritis. It is usually encountered in individuals who are immunocompromised, including those with cancer, immunosuppression, transplants, and AIDS. Gastric involvement can be localized or diffuse. Fungal infections that cause gastritis include Candida albicans and histoplasmosis. Gastric phycomycosis is another rare lethal fungal infection. The common predisposing factor is immunosuppression. C albicans rarely involves the gastric mucosa. When isolated in the stomach, the most common locations tend to be within a gastric ulcer or an erosion bed. It is generally of little consequence. Disseminated histoplasmosis can involve the stomach. The usual presenting clinical feature is bleeding from gastric ulcers or erosions on giant gastric folds. Parasitic infections are rare causes of gastritis. Anisakidosis is caused by a nematode that embeds itself in the gastric mucosa along the greater curvature. Anisakidosis is acquired by eating contaminated sushi and other types of contaminated raw fish. It often causes severe abdominal pain that subsides within a few days. This nematode infection is associated with gastric fold swelling, erosions, and ulcers. Ulcero-hemorrhagic gastritis is most commonly seen in patients who are critically ill. Ulcero-hemorrhagic gastritis is believed to be secondary to ischemia related to hypotension and shock or to the release of vasoconstrictive substances, but the etiology is often unknown. The gastric mucosa reveals multiple petechiae, mostly in the fundus and body, or exhibits a diffusely hemorrhagic pattern. The gross pathology may resemble that of NSAID- or other ingestion-induced gastritis, except that the location of injury is different. This form of gastritis can be life-threatening if the patient experiences hemorrhaging and may even require emergency gastrectomy. Microscopic evidence of acute gastritis can be seen in patients with Crohn disease, though clinical manifestations are rare (occurring in only about 2-7% of patients with Crohn disease). Focally enhancing gastritis is now recognized as a condition seen in both Crohn disease and ulcerative colitis. Eosinophilic gastritis is often seen in conjunction with eosinophilic gastroenteritis but can be associated with various disorders, including food allergies (eg, cow milk, soy protein), collagen vascular diseases, parasitic infections, gastric cancer, lymphoma, Crohn disease, vasculitis, drug allergies, and H pylori infections. An eosinophilic infiltrate is seen involving the gastric wall or epithelium.
Das könnte Ihnen auch gefallen
- Mockery Breed Murder Birds PDFDokument12 SeitenMockery Breed Murder Birds PDFLautaro BojanichNoch keine Bewertungen
- CheckList For Checking of Drawings-R1Dokument4 SeitenCheckList For Checking of Drawings-R1jatin kalraNoch keine Bewertungen
- Flow Chart - QCDokument2 SeitenFlow Chart - QCKarthikeyan Shanmugavel100% (1)
- Case Study GastritisDokument6 SeitenCase Study Gastritisapi-37524814078% (9)
- Calculous CholecystitisDokument137 SeitenCalculous Cholecystitisrremonde100% (5)
- Chronic Gastritis Case StudyDokument16 SeitenChronic Gastritis Case Studyavtooril91% (11)
- GROSS Mystery of UFOs A PreludeDokument309 SeitenGROSS Mystery of UFOs A PreludeTommaso MonteleoneNoch keine Bewertungen
- Acute GastritisDokument28 SeitenAcute GastritisSarah Repin50% (2)
- Acute Glomrulonephritis PathophysiologyDokument2 SeitenAcute Glomrulonephritis PathophysiologyJai - HoNoch keine Bewertungen
- A Case PresentationDokument50 SeitenA Case PresentationAnaleah MalayaoNoch keine Bewertungen
- NCP Gastritis NewDokument3 SeitenNCP Gastritis NewNova Triska Purnama Sari0% (1)
- Acute GastritisDokument42 SeitenAcute GastritisKaloy Kamao88% (8)
- CROHNSDokument2 SeitenCROHNSAlvin Germo Pasuquin100% (1)
- NCP Crohn'sDokument2 SeitenNCP Crohn'sJanice Marco100% (1)
- CP - Acute GastritisDokument25 SeitenCP - Acute GastritisRichard John Casquejo BroaNoch keine Bewertungen
- Chronic Gastritis Case StudyDokument17 SeitenChronic Gastritis Case StudyKaren Evangelista50% (4)
- Pathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsDokument4 SeitenPathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsYuyu Tulawie100% (1)
- Pathophysiology of NephrosclerosisDokument2 SeitenPathophysiology of NephrosclerosisJessica Damasen Caballero0% (1)
- Stomach - GastritisDokument22 SeitenStomach - GastritisaimanNoch keine Bewertungen
- Pathophysiology Acute GastritisDokument4 SeitenPathophysiology Acute GastritisKaloy Kamao100% (2)
- CHOLECYSTITISDokument13 SeitenCHOLECYSTITISdolly joy100% (1)
- Acute GlomerulonephritisDokument57 SeitenAcute Glomerulonephritisynadelcastillo100% (7)
- Pancreatitis: (Alterations in Metabolic and Endocrine Functions)Dokument7 SeitenPancreatitis: (Alterations in Metabolic and Endocrine Functions)Jorie Roco0% (1)
- Acute Glomerulonephritis Case StudyDokument12 SeitenAcute Glomerulonephritis Case Study19lyon92100% (6)
- Pathophysiology of AGEDokument1 SeitePathophysiology of AGEtinatin9890% (1)
- Acute GlomerulonephritisDokument17 SeitenAcute GlomerulonephritisBayanSecond WardNoch keine Bewertungen
- CHOLECYSTITIS CASE STUDY Version 2.0Dokument57 SeitenCHOLECYSTITIS CASE STUDY Version 2.0Gabriel Arch100% (1)
- Age With Moderate Dehydration New 1Dokument74 SeitenAge With Moderate Dehydration New 1Jhade Relleta100% (1)
- Cholecystitis Case PresDokument103 SeitenCholecystitis Case PresAnton LaurencianaNoch keine Bewertungen
- Better - Homes.and - Gardens.usa - TruePDF December.2018Dokument136 SeitenBetter - Homes.and - Gardens.usa - TruePDF December.2018MadaMadutsaNoch keine Bewertungen
- Chronic Gastritis Case StudyDokument17 SeitenChronic Gastritis Case StudyErmawati ErmaNoch keine Bewertungen
- Acute Gastroenteritis For PediatricsDokument12 SeitenAcute Gastroenteritis For PediatricsJamila B. MohammadNoch keine Bewertungen
- Inferring The Speaker's Tone, ModeDokument31 SeitenInferring The Speaker's Tone, Modeblessilda.delaramaNoch keine Bewertungen
- By: Leila Floresca Esteban BSNIII-BDokument38 SeitenBy: Leila Floresca Esteban BSNIII-BMonica Morales100% (2)
- NCP Liver CirrhosisDokument7 SeitenNCP Liver CirrhosisIris Jimenez-BuanNoch keine Bewertungen
- Acute Glomerulonephritis PathophysiologyDokument4 SeitenAcute Glomerulonephritis PathophysiologyChester NicoleNoch keine Bewertungen
- Case Study of Acute GastritisDokument12 SeitenCase Study of Acute Gastritisstudent_01960% (5)
- Pathophysiology of Hepatitis BDokument9 SeitenPathophysiology of Hepatitis BDianne G Ignacio100% (4)
- Peptic Ulcer Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandPeptic Ulcer Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBewertung: 5 von 5 Sternen5/5 (10)
- Case Presentation (Age) NG Grp. A2 FinalDokument43 SeitenCase Presentation (Age) NG Grp. A2 Finaljean therese83% (6)
- Acute PyelonephritisDokument59 SeitenAcute PyelonephritisKylie Golindang100% (1)
- Stomach CancerDokument7 SeitenStomach CancerSyazmin KhairuddinNoch keine Bewertungen
- Case Study CholelithiasisDokument14 SeitenCase Study Cholelithiasisb_faye20Noch keine Bewertungen
- Pathophysiology of Acute GastroenteritisDokument1 SeitePathophysiology of Acute GastroenteritisAiza Yee Bacani83% (6)
- Diverticular DiseaseDokument8 SeitenDiverticular Diseasenurse_enzo100% (1)
- Pathophysiology of Gastroenteritis, Dehydration, and NecatoriasisDokument3 SeitenPathophysiology of Gastroenteritis, Dehydration, and NecatoriasisRalph Delos Santos100% (2)
- Liver CancerDokument1 SeiteLiver CancerTarantado67% (3)
- CholelithiasisDokument3 SeitenCholelithiasisMIlanSagittarius0% (1)
- 3 Acute GastritisDokument2 Seiten3 Acute GastritisSuresh ThanneruNoch keine Bewertungen
- Amoebiasis PathophysiologyDokument3 SeitenAmoebiasis PathophysiologyApril CornejoNoch keine Bewertungen
- Pathophysiology of CholelithiasisDokument2 SeitenPathophysiology of CholelithiasisSherilNoch keine Bewertungen
- AGE PathophysiologyDokument2 SeitenAGE Pathophysiologyjosephcanlas67% (3)
- Case Study 18Dokument4 SeitenCase Study 18api-271284613Noch keine Bewertungen
- Pathophysiology of Acute GastroenteritisDokument5 SeitenPathophysiology of Acute Gastroenteritisheron_bayanin_15Noch keine Bewertungen
- Individual Case Study Acute GlomerulonephritisDokument26 SeitenIndividual Case Study Acute GlomerulonephritisBatrisyia HalimsNoch keine Bewertungen
- Case Study ReportDokument23 SeitenCase Study Reportapi-290866384Noch keine Bewertungen
- Dyspepsia (Gastritis) Case StudiesDokument9 SeitenDyspepsia (Gastritis) Case StudiesJessica Nurin Graman100% (1)
- Acute Lymphoblastic Leukemia (All)Dokument35 SeitenAcute Lymphoblastic Leukemia (All)Mohamed RehanNoch keine Bewertungen
- Pathophysiology of DiverticulitisDokument1 SeitePathophysiology of Diverticulitisjordan aguilar100% (1)
- Acute Glomerulonephritis PathophysioDokument4 SeitenAcute Glomerulonephritis Pathophysioshaider1190% (1)
- AldazideDokument2 SeitenAldazideianecunarNoch keine Bewertungen
- Case Study Ugib Lower MBDokument65 SeitenCase Study Ugib Lower MBQuolette Constante100% (1)
- Pathophysiology AGEDokument2 SeitenPathophysiology AGEMareeze Hatta100% (1)
- Acute Gastritis - Emedicine - 12 Jan 2011Dokument8 SeitenAcute Gastritis - Emedicine - 12 Jan 2011Melissa KanggrianiNoch keine Bewertungen
- Background: View Media GalleryDokument6 SeitenBackground: View Media Galleryprayitno tabraniNoch keine Bewertungen
- Stomach - GastritisDokument22 SeitenStomach - GastritisBîndar CristianNoch keine Bewertungen
- FDA Drug Safety Bill Passes in The U.S. Senate Health Freedom Advocates Outraged at Betrayal of American ConsumersDokument12 SeitenFDA Drug Safety Bill Passes in The U.S. Senate Health Freedom Advocates Outraged at Betrayal of American ConsumersFlorsean Mae SalaNoch keine Bewertungen
- More Details Emerge in Obama's Secret Dealings With Big Pharma During Health Care OverhaulDokument2 SeitenMore Details Emerge in Obama's Secret Dealings With Big Pharma During Health Care OverhaulFlorsean Mae SalaNoch keine Bewertungen
- Ancestors of Jose RizalDokument4 SeitenAncestors of Jose RizalFlorsean Mae SalaNoch keine Bewertungen
- Advantages of Octupos WiringDokument2 SeitenAdvantages of Octupos WiringFlorsean Mae SalaNoch keine Bewertungen
- A Brief History of The ComputerDokument3 SeitenA Brief History of The ComputerFlorsean Mae SalaNoch keine Bewertungen
- World's Standard Model G6A!: Low Signal RelayDokument9 SeitenWorld's Standard Model G6A!: Low Signal RelayEgiNoch keine Bewertungen
- Module 1 Notes The White Bird Reading The Image Painting Analysis PDFDokument4 SeitenModule 1 Notes The White Bird Reading The Image Painting Analysis PDFMelbely Rose Apigo BaduaNoch keine Bewertungen
- Design and Development of Automatic Pneumatic Jack in Four Wheeler Ijariie5374Dokument5 SeitenDesign and Development of Automatic Pneumatic Jack in Four Wheeler Ijariie5374Saravanan ViswakarmaNoch keine Bewertungen
- Assessment Questions: 1: Wash - Rinse and SanitizeDokument3 SeitenAssessment Questions: 1: Wash - Rinse and SanitizeAna Margarita AycochoNoch keine Bewertungen
- Assignment 2 Mat435Dokument2 SeitenAssignment 2 Mat435Arsene LupinNoch keine Bewertungen
- AssessmentDokument9 SeitenAssessmentJuan Miguel Sapad AlpañoNoch keine Bewertungen
- 4 Force & ExtensionDokument13 Seiten4 Force & ExtensionSelwah Hj AkipNoch keine Bewertungen
- Updated Factory Profile of Aleya Apparels LTDDokument25 SeitenUpdated Factory Profile of Aleya Apparels LTDJahangir Hosen0% (1)
- Week 1 - NATURE AND SCOPE OF ETHICSDokument12 SeitenWeek 1 - NATURE AND SCOPE OF ETHICSRegielyn CapitaniaNoch keine Bewertungen
- Assignment 1Dokument3 SeitenAssignment 1farhang_tNoch keine Bewertungen
- Seminar On Solar Mobile Charger: Submitted To: Submitted byDokument16 SeitenSeminar On Solar Mobile Charger: Submitted To: Submitted byAkhila GottemukkulaNoch keine Bewertungen
- Nissan Copper LTDDokument11 SeitenNissan Copper LTDankit_shahNoch keine Bewertungen
- EPCC Hydrocarbon Downstream L&T 09.01.2014Dokument49 SeitenEPCC Hydrocarbon Downstream L&T 09.01.2014shyaminannnaNoch keine Bewertungen
- Crouse Hinds XPL Led BrochureDokument12 SeitenCrouse Hinds XPL Led BrochureBrayan Galaz BelmarNoch keine Bewertungen
- Someone Who Believes in YouDokument1 SeiteSomeone Who Believes in YouMANOLO C. LUCENECIONoch keine Bewertungen
- Ali Erdemir: Professional ExperienceDokument3 SeitenAli Erdemir: Professional ExperienceDunkMeNoch keine Bewertungen
- Douluo Dalu Volume 05 - Star Dou Forest PDFDokument141 SeitenDouluo Dalu Volume 05 - Star Dou Forest PDFRay Joseph LealNoch keine Bewertungen
- Assignment 2 Unit 20 Fully Completed - ReviewedDokument5 SeitenAssignment 2 Unit 20 Fully Completed - Reviewedchris.orisawayiNoch keine Bewertungen
- Ad149 Manual RDokument69 SeitenAd149 Manual RCharityNoch keine Bewertungen
- 9 5 - 358 362 PDFDokument5 Seiten9 5 - 358 362 PDFمالك مناصرةNoch keine Bewertungen
- Shandong Baoshida Cable Co, LTD.: Technical ParameterDokument3 SeitenShandong Baoshida Cable Co, LTD.: Technical ParameterkmiqdNoch keine Bewertungen
- Syllabus Unit Iv Unit Commitment and Economic DispatchDokument23 SeitenSyllabus Unit Iv Unit Commitment and Economic DispatchBALAKRISHNANNoch keine Bewertungen
- Socialized HousingDokument48 SeitenSocialized HousingJessieReiVicedoNoch keine Bewertungen
- GP1 Q1 Week-1Dokument18 SeitenGP1 Q1 Week-1kickyknacksNoch keine Bewertungen