Beruflich Dokumente
Kultur Dokumente
Enzymes Liver Pancreas FC
Hochgeladen von
Lois LipanovichOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Enzymes Liver Pancreas FC
Hochgeladen von
Lois LipanovichCopyright:
Verfügbare Formate
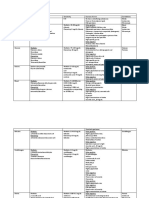
Enzymes Liver Pancreas
Cell destruction Cell Proliferation Increases synthesis oxidoreductases, transferases, hydrolases, lyases, isomerases, ligases Substrate concentration Enzyme concentration pH Temperature Cofactors inhibitors
Elevation of enzyme levels caused by:
Enzyme Classification: 6 classes:
Factors that influence enzymatic reactions 6
Enzyme reactions requires: 4 Zero Order difference in rate? Why?
1.Enzyme 2.Substrate 3.E-S complex 4.End Product the at nearby concentrations of substrate is almost negligible At these concentrations almost all of the enzyme molecules are bound to substrate and the rate is independent of substrate, zero order. At substrate concentrations near point A the rate appears to be directly proportional to substrate concentration At the substrate concentration exactly half the enzyme molecules are in an ES complex at any instant and the rate is exactly one half of Vmax concentration of substrate that gives "halfmaximal activity". if enzyme is elevated that all substrate is consumed early in reaction. Then the rate change is minimal = Errors sudden decrease in reaction rate, may indicate that the patient sample containing a enzyme level requires a dilution or decreased amount. Lipase: Triglyceride substrate Omylase: Starch substrate Elevated in liver and bone disorders Normal elevations in children and during pregnancy. 1
reaction rate - first order
Vmax = Point B
Constant Km =
Fixed Time problem
Kinetic problem Acute pancreatitis enzymes
Alkaline Phosphatase
Enzymes Liver Pancreas
Acid Phosphatase Elevated in prostatic cancer Tested for as confirmation in rape cases if found in vaginal fluid fraction of bilirubin covalently bound to albumin; in conventional methods it is measured as part of conjugated bilirubin. Because of its covalent bond during the recovery phase of hepatocellular jaundice it may persist in the blood for a week or more after urine clears. ALT- alanine transaminase AST - aspartate transaminase GGT - gamma-glutamyltranspeptidase Alkaline phosphatase Aldolase 1.Alk PO4
delta bilirubin
Liver function evaluated with enzyme testing
1.Which is helpful in diagnosing bone disease? 2.Which enzymes are helpful in diagnosis of muscle disorders? 3.Which enzymes tests for hepatic function? 4.Which one enzyme is most sensitive for all types of liver disease? 5.Is AST or ALT more specific for liver disease? 6.Which is sensitive indicator of alcoholism? first organ to encounter nutrients, vitamins, drugs, toxic agents etc. Most common liver injury is due to
2.CK, AST, LD, aldolase
3.ALT,AST, alkaline PO4 4.GGT 5.ALT is primarily found in liver & RBCs
6.GGT Liver viruses (hepatitis). 1. Synthetic and Metabolic 2. Excretory 3. Detoxification and protective 4. Hematology/Coagulation
FUNCTIONS OF LIVER
CATEGORIES of LIVER DISEASE (amyloid, neoplasm) 2
Enzymes Liver Pancreas
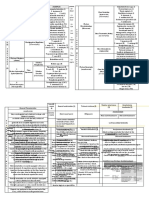
Cirrhosis: Inflammation of the liver: scaring and abnormal architecture of the liver Alcohol is common cause Autoimmune, viral, drugs Tumors: uncommon in US but common in other cultures for unknown reasons. Reyes Syndrome: death from liver destruction following viral infection, associated with aspirin use. Drug Induced: Most common fatty liver (vacuoles of fat) drugs
LIVER DISEASES 4 categories Most Common?
Steatosis
HEPATOTOXIC AGENTS many Halothane
Necrosis means neoplasia BILIRUBIN Conjugated (water soluble) bilirubin is excreted from liver into the removes the glucuronide from bilirubin and reduces bilirubin to
premature death of cells in living tissue The formation or presence of a new, abnormal growth of tissue. bile.
urobilinogen.
excreted in
2 ways how?
urine or oxidized to form urobilin and excreted in feces.
turns color which gives feces and urine its color. BILIRUBIN METABOLISM Excreted as: 2 chemicals? Where? stays attached until the albumin molecule is turned over, but measures as conjugated 3
Delta bilirubin
Enzymes Liver Pancreas
Clinical manifestation of hyperbilirubinemia Icterus and mucous membranes Kernicterus: blood brain barrier < 1 mg/dL (hemolytic) unconjugated hyperbilirubinemia; no bilirubin in urine defective conjugation; transport failure; hepatocellular damage or necrosis inability to transport conjugated bilirubin out of liver; obstruction of common bile duct by gall stones, neoplasms, spasms or stricture. HYPERBILIRUBINEMIA jaundice with yellow skin and sclera (2.5 - 5.0 mg/dL). 1. Overproduction 2. Impaired uptake by liver cells 3. Defects in the conjugation reaction 4. Reduced excretion into the bile 5. Obstruction to the flow of bile (1) Overproduction: due to excess RBC destruction, rate of hemolysis exceeds livers ability to clear bilirubin. Almost all unconjugated. (hemolytic anemia, sickle cell disease). (2) Impaired Uptake by Liver Cells: drugs block bilirubin uptake into liver hepatocytes. (3) Defective Conjugation (4) Reduced Excretion: Damage to liver cells, hepatitis, cirrhosis, drug induced. Conjugated bilirubin rises. (5) Obstruction: Mechanical obstruction of bile flow, gallstones in bile duct Mostly conjugated bilirubin rises. decrease of bilirubin transport into hepatocytes deficiency of UDPG- transferase Acquired: drug inhibits the enzyme Neonatal jaundice: the enzyme is not fully developed yet 4
JAUNDICE 2 kinds
total bilirubin = normal Classification of Jaundice Prehepatic Hepatic Jaundice
Posthepatic Jaundice
BILIRUBIN IN BLOOD 2 causes
Defective Conjugation Gilberts syndrome Crigler-Najjar syndrome Defective Conjugation Non-inherited
Enzymes Liver Pancreas
BILIRUBIN TERMINOLOGY Total Bilirubin = All forms of Bilirubin= Direct + Indirect+ Delta water soluble conjugated Bilirubin diglucuronide and delta Bilirubin (albumin bound) not water soluble alcohol soluble requires accelerator unconjugated Bilirubin toxic - 1.0 mg/dL -2 days) 3.4 11.5 -5 days) 1.5 12.0 Direct 0 - 0.2 mg/dL liver disease or bile ducts Decreased secretion into canaliculi hepatitis and/or drugs Decreased drainage stones in gall bladder carcinoma drugs tumors cirrhosis RBC hemolysis Inhibition of transport into hepatocyte by drugs Decreased conjugation Neonatal jaundice Inhibition of enzyme by drugs Gilbert Syndrome UROBILINOGEN metabolism. Bacteria in intestines converts urobilinogen into urobilin, a brown pigment. hemolytic disease and defective liver-cell function (hepatitis)
Direct Bilirubin =
Indirect Bilirubin =
BILIRUBIN REFERENCE INTERVALS -2 days) -5 days) Direct Elevated conjugated implies
Conjugated Elevated (cholestasis) In the liver 2 categories of reasons
Unconjugated Elevated In the liver 3 categories of reasons
Enzymes Liver Pancreas
biliary obstruction. purple color formation with Ehrlichs reagent (pdimethylaminobenzaldehyde). aid absorption of cholesterol and triglycerides Liver Proteins Transthyretin Ceruloplasmin Alpha1 antitrypsin Haptoglobin Beta2 microglobulin Transferrin Alpha fetoprotein (Transports/ binds iron) (Copper carrier) (Acute phase protein) (Transports/ binds free Hb) Bile Acids (Prealbumin:nutritional indicator)
(early liver cancer marker)
ALBUMIN Chronic Hepatitis Acute Hepatitis
hepatocytes as a marker of general liver function. -21 days
INCREASED ALBUMIN In 4?
Albumin Normal Range Transthyretin (prealbumin) RI
3.5 5.5 g/dL 18 - 22 mg/dL 6
Enzymes Liver Pancreas
AST & ALT: OTHER FACTORS Hemolysis Age/ Gender Diurnal Variation Race Exercise Body weight Muscle injury AST Reference Range ALT Reference Range 5-30 U/L
-50 then decreases
> ALT
6-37 U/L
Less than 1:1 viral hepatitis nonalcoholic steatohepatitis Greater than 1:1 (2:1, 3:1) chronic alcohol-induced liver damage (AST rarely more than 8x normal; ALT seldom more than 5x; maybe normal)
AST:ALT ratio
ALT
Male: 10-40 U/L Female: 7-35 U/L
ALKALINE PHOSPHATASE Factors effecting ALP
inhibits enzyme activity -3 X - no effect
ALKALINE PHOSPHATASE REFERENCE INTERVALS
44 to 147 IU/L Bile Duct Obstruction gall stones, surgery, cancer Bile Duct Disease primary biliary cirrhosis Drug-Induced cholestasis Liver Infiltration cancer, fungus, sarcoidosis may give highest values 7
MARKEDLY ELEVATED ALP (Normal or slightly elevated AST ALT)
Enzymes Liver Pancreas
high concentrations of kidney and liver but also pancreas and intestine GGT -Transferase from liver.
disease Reference Ranges ALT AST ALP GTT - 37 U/L female - 30 U/L - 90 U/L age important - 45 U/L male 5 30 U/L Female
AMMONIA (NH3)
Elevated in blood when liver failure levels low in Serum Encephalopathy, or damage to nerves in the brain, may be consequence of high ammonia (up to 5x)
GASTRIN hormones, and enzymes Zollinger-Ellison syndrome : Gastric-producing tumor leading to peptic ulcers, gastric hypersecretion; elevated gastrin Acute Pancreatitis Blockage of pancreatic duct with gallstones Alcohol excess Physical Trauma Chronic Pancreatitis Gall Bladder disease Alcoholism Pancreatic Cancer 4th most frequent form of fatal cancer 5 year survival <5% Pancreatic Insufficiency Cystic Fibrosis Chronic Pancreatitis
Pancreatic diseases
Enzymes Liver Pancreas
AMYLASE particularly acute pancreatitis
AMYLASE: Testing METHODS
formed Amyloclastic: measure decrease in starch substrate from dye-labeled substrate Hydrolyzes triglycerides
LIPASE earlier and persist longer Titrimetric: olive oil substrate; titrate fatty acids using pH indicator Turbidimetric: measure decrease in turbidity due to hydrolysis of substrate coupled with enzymatic reaction
LIPASE: Testing METHODS
Fecal Fat analysis Other pancrease test
mutations in a gene located on chromosome 7. Causes production of thick mucus due to faulty transport of Na and Cl within cells lining lungs and pancreas. Mucus obstructs pancreatic secretions from reaching duodenum Manifestations: intestinal obstruction, pulmonary infections, malabsorption
CYSTIC FIBROSIS
Enzymes Liver Pancreas
Symptoms: salty-tasting sweat; persistent coughing, wheezing or pneumonia; poor weight gain; bulky stools Treatment: vigorous percussion on back and chest; antibiotics; nutritional supplementation; Gene Therapy
CYSTIC FIBROSIS Symptoms Treatment:
CYSTIC FIBROSIS DIAGNOSIS SWEAT CHLORIDE ANALYSIS CONSIDERED MOST RELIABLE SINGLE TEST FOR DIAGNOSIS OF CYSTIC FIBROSIS Elevated sweat sodium and chloride (>60 mmol/L) in cystic fibrosis Iontophoresis, using drug pilocarpine to induce sweat Sweat is collected on preweighed gauze Elevated sweat sodium and chloride (>60 mmol/L) in cystic fibrosis Iontophoresis, using drug pilocarpine to induce sweat Sweat is collected on preweighed gauze Chloride/ Na is measured d-Xylose: pentose sugar not normally in blood Ability to absorb D-xylose helps in diagnosing malabsorption problems in intestine vs pancreatic insufficiency Test Fast, void in AM, drink d-Xylose and water Collect blood at 2 hours, and Urine collected after 5 hours
SWEAT CHLORIDE ANALYSIS
Tests of Intestinal Function D-Xylose Absorption Test
10
Das könnte Ihnen auch gefallen
- CLINICAL CHEMISTRY: Passbooks Study GuideVon EverandCLINICAL CHEMISTRY: Passbooks Study GuideNoch keine Bewertungen
- Liver Function Tests and EnzymesDokument90 SeitenLiver Function Tests and EnzymesNaji Mohamed Alfatih100% (1)
- Liver Function TestDokument5 SeitenLiver Function Testkriss WongNoch keine Bewertungen
- BACTERIOLOGY RecallsDokument6 SeitenBACTERIOLOGY RecallsRachelle AbonalesNoch keine Bewertungen
- Summary of Reagent Strip TestsDokument8 SeitenSummary of Reagent Strip TestsDarla YsavelNoch keine Bewertungen
- Compre - RevieverDokument20 SeitenCompre - RevieverjohnNoch keine Bewertungen
- Liver Function (Clinical Chemistry)Dokument11 SeitenLiver Function (Clinical Chemistry)Patricia PerfectoNoch keine Bewertungen
- Clinical Microbiology QuestionsDokument18 SeitenClinical Microbiology QuestionsArianne Joy C. TamarayNoch keine Bewertungen
- Micro para OSCE For YL6 BacteriaDokument2 SeitenMicro para OSCE For YL6 Bacteriagzldiwa100% (1)
- Final DX ResultsDokument9 SeitenFinal DX ResultszysheaiNoch keine Bewertungen
- Clinical CaseDokument17 SeitenClinical CaseDev ROYNoch keine Bewertungen
- Alkaline PH Acid PH N Amorphous Phosphate Uric AcidDokument3 SeitenAlkaline PH Acid PH N Amorphous Phosphate Uric AcidSurriya NawazNoch keine Bewertungen
- AnemiaDokument9 SeitenAnemiaMila Canoza HerreraNoch keine Bewertungen
- Food and Waterborne Diseases Prevention and Control ProgramDokument3 SeitenFood and Waterborne Diseases Prevention and Control ProgramJake PitosNoch keine Bewertungen
- Chapter 4 Physical Examination PDFDokument4 SeitenChapter 4 Physical Examination PDFJulie Anne Soro ValdezNoch keine Bewertungen
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Dokument6 Seiten(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerNoch keine Bewertungen
- Clinical Chemistry 2 Lecture Notes in Trace ElementsDokument6 SeitenClinical Chemistry 2 Lecture Notes in Trace ElementsMoira Pauline LibroraniaNoch keine Bewertungen
- Chapter 2 Introduction To Urinalysis PDFDokument4 SeitenChapter 2 Introduction To Urinalysis PDFJulie Anne Soro ValdezNoch keine Bewertungen
- HematologyDokument4 SeitenHematologyliesel_12Noch keine Bewertungen
- Common Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Dokument2 SeitenCommon Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Elizabeth Enjambre HernaniNoch keine Bewertungen
- Lab ValuesDokument5 SeitenLab Valuespragya_devkotaNoch keine Bewertungen
- Student Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentDokument5 SeitenStudent Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentMelody PardilloNoch keine Bewertungen
- A. Neisseria Gonorrhoeae B. Moraxella Catarrhalis C. Neisseria Meningitidis D. Neisseria LactamicaDokument7 SeitenA. Neisseria Gonorrhoeae B. Moraxella Catarrhalis C. Neisseria Meningitidis D. Neisseria LactamicaWynlor AbarcaNoch keine Bewertungen
- Peptic UlcerDokument4 SeitenPeptic UlcerEris Abdul AzizNoch keine Bewertungen
- NEMATODES NotesDokument34 SeitenNEMATODES NotesbebibobuNoch keine Bewertungen
- EndocrinologyDokument12 SeitenEndocrinologyNathaniel Derige AndesNoch keine Bewertungen
- CC Bishop QuestionsDokument3 SeitenCC Bishop QuestionsJohanna Kate DiestroNoch keine Bewertungen
- Vii. Urine Screening For Metabolic DisordersDokument4 SeitenVii. Urine Screening For Metabolic DisordersDee GeeNoch keine Bewertungen
- Tables VirusesDokument9 SeitenTables VirusesOmphile DansonNoch keine Bewertungen
- Hematology ReviewerDokument4 SeitenHematology ReviewerAbigail Puno100% (1)
- AmoebaDokument5 SeitenAmoebasarguss14Noch keine Bewertungen
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDokument12 SeitenRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Urine and Other Body FluidsDokument248 SeitenUrine and Other Body FluidsGennelyn Ross Delos Reyes0% (1)
- Staphylococci: Streptococcus PyogenesDokument20 SeitenStaphylococci: Streptococcus PyogenesPharmacy2015100% (2)
- Unit 3 Flash Cards - Clinical Chemistry - Diabetes and Other Carbohydrate Disease Lab TestsDokument10 SeitenUnit 3 Flash Cards - Clinical Chemistry - Diabetes and Other Carbohydrate Disease Lab TestsLois Lipanovich100% (1)
- Harrisons: Introduction To Infectious DiseasesDokument3 SeitenHarrisons: Introduction To Infectious Diseasesapi-3704562Noch keine Bewertungen
- Bacte TestDokument10 SeitenBacte TestRiondalionNoch keine Bewertungen
- UrinalysisDokument5 SeitenUrinalysisRaidis PangilinanNoch keine Bewertungen
- (Microbio) Staphyloccocus and Streptococcus-Dr. Salandanan (BHND)Dokument16 Seiten(Microbio) Staphyloccocus and Streptococcus-Dr. Salandanan (BHND)Lee Delos Santos100% (1)
- Review in Clinical MicrosDokument103 SeitenReview in Clinical MicrosSyvelmarie Tinte100% (1)
- Hematology 2 TEST QUESTIONSDokument4 SeitenHematology 2 TEST QUESTIONSa a r o n b a u t i s t aNoch keine Bewertungen
- Urinalysis and Body Fluids2020Dokument47 SeitenUrinalysis and Body Fluids2020MONFOLA100% (1)
- Chapter 24 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Non Immune CausesDokument5 SeitenChapter 24 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Non Immune CausesNathaniel SimNoch keine Bewertungen
- CPC NephrolithiasisDokument81 SeitenCPC NephrolithiasisOmar Zaman KhanNoch keine Bewertungen
- Lesson 1: History of Immunohematology and Blood Transfusion Practice and Future TrendsDokument129 SeitenLesson 1: History of Immunohematology and Blood Transfusion Practice and Future TrendsNicole CutieNoch keine Bewertungen
- Microbiology FlashcardsDokument36 SeitenMicrobiology FlashcardsKrisha Bernadette TillamanNoch keine Bewertungen
- Liver Function TestDokument50 SeitenLiver Function TestJhannNoch keine Bewertungen
- Coagulation CascadeDokument4 SeitenCoagulation CascadezainabNoch keine Bewertungen
- Hematology Ii Lectures Introduction To HemostasisDokument28 SeitenHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Fasciolopsis Buski: F Hepatica F. BuskiDokument4 SeitenFasciolopsis Buski: F Hepatica F. BuskiGela ReyesNoch keine Bewertungen
- Clinical Chemistry KeyNotes For Board ExaminationDokument12 SeitenClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- Protein Case SummaryDokument2 SeitenProtein Case SummaryGlydenne Glaire Poncardas Gayam100% (2)
- Bacte Day 2Dokument24 SeitenBacte Day 2Jadey InfanteNoch keine Bewertungen
- Hema Lec CompiledDokument68 SeitenHema Lec Compiledchris andrieNoch keine Bewertungen
- Pediatrics SamplexDokument6 SeitenPediatrics SamplexThea SansonNoch keine Bewertungen
- Gram Positive CocciDokument6 SeitenGram Positive Coccitamiqua1Noch keine Bewertungen
- Clin Path Trans 3.05 Urinalysis (2b)Dokument6 SeitenClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezNoch keine Bewertungen
- Practical Microbiology Exam Revision: Slide Spots CollectionDokument40 SeitenPractical Microbiology Exam Revision: Slide Spots Collectionعلي الكوافيNoch keine Bewertungen
- Diseases of The Immune SystemDokument9 SeitenDiseases of The Immune SystemVenzNoch keine Bewertungen
- Clinical Chemistry Review 1-110Dokument6 SeitenClinical Chemistry Review 1-110Lois Lipanovich89% (9)
- Enzyme Flash CardsDokument2 SeitenEnzyme Flash CardsLois LipanovichNoch keine Bewertungen
- Lab QC FlashcardsDokument7 SeitenLab QC FlashcardsLois LipanovichNoch keine Bewertungen
- Unit 3 Flash Cards - Clinical Chemistry - Diabetes and Other Carbohydrate Disease Lab TestsDokument10 SeitenUnit 3 Flash Cards - Clinical Chemistry - Diabetes and Other Carbohydrate Disease Lab TestsLois Lipanovich100% (1)
- Unit 6 Flash Cards Hematology CoagulationDokument13 SeitenUnit 6 Flash Cards Hematology CoagulationLois LipanovichNoch keine Bewertungen
- 3 - PancreaseDokument12 Seiten3 - PancreasemyarjddbzNoch keine Bewertungen
- Operation Atlas of Hepato Pancreato Biliary Surgery Collected CaseDokument339 SeitenOperation Atlas of Hepato Pancreato Biliary Surgery Collected Caseمحمد ورفليNoch keine Bewertungen
- Pathology of The Exocrine PancreasDokument5 SeitenPathology of The Exocrine PancreassatriayanuwardaniNoch keine Bewertungen
- Japanese Clinical Practice Guidelines For Pancreaticobiliary MaljunctionDokument29 SeitenJapanese Clinical Practice Guidelines For Pancreaticobiliary MaljunctionadrianiNoch keine Bewertungen
- Investigation and Treatment of Surgical JaundiceDokument38 SeitenInvestigation and Treatment of Surgical JaundiceUjas PatelNoch keine Bewertungen
- The SGOT/SGPT Ratio - An Indicator of Alcoholic Liver DiseaseDokument4 SeitenThe SGOT/SGPT Ratio - An Indicator of Alcoholic Liver DiseaseSahara MaindokaNoch keine Bewertungen
- Colilithiasis 2Dokument53 SeitenColilithiasis 2Worku KifleNoch keine Bewertungen
- Laporan - Pemeriksaan LaboratoriumDokument36 SeitenLaporan - Pemeriksaan Laboratoriumamalia fitri audinaNoch keine Bewertungen
- Acu Meridians AtlasDokument28 SeitenAcu Meridians AtlasGeeta SajjanNoch keine Bewertungen
- OET Practice Writing TestDokument2 SeitenOET Practice Writing TestyazzNoch keine Bewertungen
- Annular Pancreas Divisumtreated With Whipple Procedure: A Case Reportand Update of Arare ConditionDokument5 SeitenAnnular Pancreas Divisumtreated With Whipple Procedure: A Case Reportand Update of Arare ConditionIJAR JOURNALNoch keine Bewertungen
- Daftar Pustaka 1Dokument7 SeitenDaftar Pustaka 1Teddy Agung SaputraNoch keine Bewertungen
- Open Common Bile Duct ExplorationDokument51 SeitenOpen Common Bile Duct Explorationmathisync100% (4)
- Liver CirrhosisDokument50 SeitenLiver CirrhosisMK CameraNoch keine Bewertungen
- PancreasDokument6 SeitenPancreasSimran Radhika JasujaNoch keine Bewertungen
- Benign Prostatic Hyperplasia (BPH)Dokument3 SeitenBenign Prostatic Hyperplasia (BPH)Shahmeer KhanNoch keine Bewertungen
- Sonnykalangi,+1 +OK+Iriana+T+Seralurin+1-5Dokument5 SeitenSonnykalangi,+1 +OK+Iriana+T+Seralurin+1-5Lineplay HelperNoch keine Bewertungen
- Liver Transplant Workup: IntroductionDokument9 SeitenLiver Transplant Workup: IntroductionKay BristolNoch keine Bewertungen
- LECTURES Liver PathophysiologyDokument118 SeitenLECTURES Liver PathophysiologyTarik100% (1)
- Choledocholithiasis - Clinical Manifestations, Diagnosis, and Management - UpToDateDokument19 SeitenCholedocholithiasis - Clinical Manifestations, Diagnosis, and Management - UpToDateFeer VillarrealNoch keine Bewertungen
- Jaundice: DR Monika PathaniaDokument27 SeitenJaundice: DR Monika PathaniaMuhammed al-jumailyNoch keine Bewertungen
- Liver Complications - SLEDokument5 SeitenLiver Complications - SLEFanny PritaningrumNoch keine Bewertungen
- JaundiceDokument3 SeitenJaundiceNyaoNyao MarcellanaNoch keine Bewertungen
- Anatomy and Physiology GallbladerDokument5 SeitenAnatomy and Physiology GallbladerJanna FavilaNoch keine Bewertungen
- Subtotal Cholecystectomy-''Fenestrating'' Vs ''Reconstituting'' Subtypes and The Prevention of Bile Duct Injury - Definition of The Optimal Procedure In  Difficult Operative ConditionsDokument8 SeitenSubtotal Cholecystectomy-''Fenestrating'' Vs ''Reconstituting'' Subtypes and The Prevention of Bile Duct Injury - Definition of The Optimal Procedure In  Difficult Operative ConditionsBolivar Isea100% (1)
- Cancers 02 02001Dokument10 SeitenCancers 02 02001Madalina CordonasuNoch keine Bewertungen
- Acg 8 207Dokument5 SeitenAcg 8 207Hung DoNoch keine Bewertungen
- Management of Cirrhosis of The LiverDokument48 SeitenManagement of Cirrhosis of The LiverksofianaNoch keine Bewertungen
- Progressive Familial Intrahepatic Cholestasis in ChildrenDokument3 SeitenProgressive Familial Intrahepatic Cholestasis in ChildrenPaul HartingNoch keine Bewertungen