Beruflich Dokumente
Kultur Dokumente
ThyroidCancer Brochure
Hochgeladen von
Dedy Sambeta0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
110 Ansichten2 SeitenCancer of the thyroid is the most common endocrine-related cancer. Thyroid cancer is easily curable with surgery and rarely causes pain or disability. Papillary thyroid cancer makes up about 70% to 80% of all thyroid cancers.
Originalbeschreibung:
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCancer of the thyroid is the most common endocrine-related cancer. Thyroid cancer is easily curable with surgery and rarely causes pain or disability. Papillary thyroid cancer makes up about 70% to 80% of all thyroid cancers.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
110 Ansichten2 SeitenThyroidCancer Brochure
Hochgeladen von
Dedy SambetaCancer of the thyroid is the most common endocrine-related cancer. Thyroid cancer is easily curable with surgery and rarely causes pain or disability. Papillary thyroid cancer makes up about 70% to 80% of all thyroid cancers.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
Cancer of the Thyroid
Thyroid cancer is the most common endocrine-related cancer; however, it is rare compared to other cancers. In the United States there are only about 20,000 new patients annually. Even though the diagnosis of cancer is terrifying, the outlook for patients with thyroid cancer is usually excellent. First, most thyroid cancer is easily curable with surgery. Second, thyroid cancer rarely causes pain or disability. Third, effective and well-tolerated treatment is available for the most common forms of thyroid cancer.
This page and its contents are Copyright 2005 the American Thyroid Association
ADDITIONAL PATIENT RESOURCES WWW.THYROID.ORG
For further details on this and other thyroid-related topics, please visit the patient resources section on the American Thyroid Association website at www.thyroid.org
SYMPTOMS
DIAGNOSIS
What are the symptoms of thyroid cancer?
The key sign of thyroid cancer is a lump (nodule) in the thyroid, and most thyroid cancers do not cause any symptoms (see Thyroid Nodule brochure). Instead, your doctor may discover the nodule during a routine physical examination or you may notice a lump in your neck while looking in a mirror. A few patients with thyroid cancer complain of pain in the neck, jaw or ear. If the cancer is large enough, it may cause difficulty swallowing or cause a tickle in the throat or shortness of breath if it is pressing on the windpipe. Rarely, hoarseness can be caused if the cancer irritates a nerve to the voice box.
How is thyroid cancer diagnosed?
A diagnosis of thyroid cancer is made on the basis of a biopsy of a thyroid nodule or after the nodule is removed during surgery (see Thyroid Nodule brochure). Although thyroid nodules are very common, less than 1 in 10 harbor a thyroid cancer.
What are the types of thyroid cancer?
Papillary thyroid cancer. Papillary thyroid cancer is the most common type, making up about 70% to 80% of all thyroid cancers. Papillary thyroid cancer can occur at any age. There are only about 12,000 new cases of papillary cancer in the United States each year, but because these patients have such a long life expectancy, we estimate that 1 in a 1000 people in the United States have or have had this form of cancer. Papillary cancer tends to grow slowly and to spread first to lymph glands in the neck. Unlike some other tumors, the generally excellent outlook for papillary cancer is usually not affected by spread of the cancer to the lymph nodes. Follicular thyroid cancer. Follicular thyroid cancer, which makes up about 10% to 15% of all thyroid cancers in the United States, tends to occur in somewhat older patients than does papillary cancer. As with papillary cancer, follicular cancer first can grow into lymph nodes in the neck. Follicular cancer is also more likely than papillary cancer to grow into blood vessels and from there to spread to distant areas, particularly the lungs and bones. Medullary thyroid cancer. Medullary thyroid cancer, which accounts for 5% to 10% of all thyroid cancers, is more likely to run in families and be associated with other endocrine problems. In fact, medullary thyroid cancer is the only thyroid cancer that can be diagnosed by genetic testing of the blood cells. In family members of an affected person, a positive test for the RET proto-oncogene can lead to an early diagnosis of medullary thyroid cancer and, subsequently, curative surgery to remove it. Anaplastic thyroid cancer. Anaplastic thyroid cancer is the most advanced and aggressive thyroid cancer and is the least likely to respond to treatment. Fortunately, anaplastic thyroid cancer is rare and found in less than 5% of patients with thyroid cancer.
CAUSES
What causes thyroid cancer?
Thyroid cancer is more common in people who have a history of exposure of the thyroid gland to radiation, have a family history of thyroid cancer, and are older than 40 years of age. However, for most patients, we do not know the specific reason why they develop thyroid cancer. Exposure of the thyroid to radiation causes thyroid cancer in susceptible patients, especially if the exposure occurred as a child. Many years ago (ie, in the 1940s and 1950s), radiation exposure included Xray treatments for acne, inflamed tonsils, adenoids, lymph nodes, or an enlarged thymus gland. X-rays also were used to measure foot sizes in shoe stores. Currently, X-ray exposure is usually limited to treatment of serious cancers such as Hodgkins disease (cancer of the lymph nodes). Routine X-ray exposure (eg, dental X-rays, chest X-rays, mammograms) does not cause thyroid cancer. Thyroid cancer can be caused by absorbing radioactive iodine released during a nuclear power plant emergency, such as the 1986 nuclear accident at the Chernobyl power plant in Russia. Children who were exposed were the most affected, and cancers were seen within a few years of that disaster. You can be protected from developing thyroid cancer due to a nuclear power plant emergency by taking potassium iodide, which blocks your thyroid from absorbing radioactive iodine. The United States government is currently developing guidelines to distribute potassium iodide to people living near nuclear power plants.
Cancer of the Thyroid
4
TREATMENT
What is the treatment for thyroid cancer?
Surgery. The primary therapy for all forms of thyroid cancer is surgery. The generally accepted approach is to remove the entire thyroid gland, or as much of it as can be safely removed. After surgery, patients need to be on thyroid hormone for the rest of their life (see Thyroid Hormone Treatment brochure). Often the thyroid cancer is cured by surgery alone, especially if the cancer is small. If the cancer is large within the thyroid or if it has spread to lymph nodes or if your doctor feels that you are at high risk for recurrent cancer, radioactive iodine can be used as a magic bullet to destroy thyroid cancer cells after removal of the thyroid gland by surgery. Radioactive iodine therapy. A major reason for the usually excellent prognosis for patients with papillary and follicular thyroid cancer is that radioactive iodine can be used as a magic bullet to seek out and destroy thyroid cancer cells with little or no damage to other tissues in the body. Thyroid cells normally concentrate iodine from the bloodstream to use to produce the thyroid hormones. By contrast, thyroid cancer cells usually take up only tiny amounts of iodine. However, high levels of thyroid stimulating hormone (TSH) can arouse thyroid cancer cells to take up significant amounts of iodine. If your doctor recommends radioactive iodine therapy, high levels of TSH will be produced in your body by making you hypothyroid for a short timeeither by not starting thyroid hormone pills after the thyroid gland is removed or by stopping your thyroid hormone pills if you are already on medication. Sometimes, to minimize your symptoms of hypothyroidism, your doctor may prescribe Cytomel (T3) to take while you are becoming hypothyroid. Also, you may be asked to go on a low iodine diet before the treatment to increase the effectiveness of the radioactive iodine. Once the TSH level is high enough, a whole body iodine scan is done by administering a small dose of radioactive iodine to determine if there are remaining thyroid cells that need to be destroyed. If enough cells show up on the whole-body iodine scan, a large dose of radioactive iodine (I131) is given, and then the thyroid pills are re-started. Radioactive iodine therapy has proved to be safe and welltolerated, and it has even been able to cure cases of thyroid cancer that had already spread to the lungs.
This page and its contents are Copyright 2005 the American Thyroid Association
What is the follow-up for patients with thyroid cancer?
Periodic follow-up examinations are essential for all patients with thyroid cancer because the thyroid cancer can returnsometimes many years after the apparently successful initial treatment. These follow-up visits include a careful history and physical examination, with particular attention to the neck area, as well as blood tests to determine if any changes of your thyroid hormone dose are needed. In particular, blood tests are done to measure the levels of T4 and TSH as well as a thyroid cell protein, thyroglobulin, which serves as a thyroid cancer marker. The thyroid hormone dose is adjusted to lower the TSH level into the low range. If the thyroglobulin level is still detectable despite a TSH in the low range, it means that there still are potential thyroid cancer cells functioning in the body.This finding may lead to additional tests and possible further treatment with radioactive iodine and/or surgery. Unfortunately, in some thyroid cancer patients the presence of interfering antibodies in the blood may prevent accurate thyroglobulin measurement. In addition to routine blood tests, your doctor may want to repeat periodically a whole-body iodine scan to determine if any thyroid cells remain. This can be done after your TSH level is raised, either by stopping your thyroid hormone and your becoming hypothyroid (see above) or by administering Thyrogen (synthetic human TSH) injections.
What is the prognosis of thyroid cancer?
Overall, the prognosis of thyroid cancer is very good. In general, the prognosis is better in younger patients than in those over 40 years of age. Patients with papillary carcinoma who have a primary tumor that is confined to the thyroid gland itself have an excellent outlook: only 1 out of every 100 such patients have died of thyroid cancer by 25 years later. The prognosis is not quite as good in patients over the age of 40, or in patients with tumors larger than 4 centimeters (1 inches) in diameter. Still, even those patients who are unable to be cured of their thyroid cancer are able to live a long time and feel well despite their cancer.
ADDITIONAL PATIENT RESOURCES WWW.THYROID.ORG
For further details on this and other thyroid-related topics, please visit the patient resources section on the American Thyroid Association website at www.thyroid.org
Das könnte Ihnen auch gefallen
- Iodine - The Universal and Holistic Super Mineral - Dr. Gabriel CousensDokument32 SeitenIodine - The Universal and Holistic Super Mineral - Dr. Gabriel CousensJ.J.100% (7)
- Where Hormone Is Produced Hormone Secreted Chemical Class Target Cell Location Hormone FunctionDokument3 SeitenWhere Hormone Is Produced Hormone Secreted Chemical Class Target Cell Location Hormone FunctionRNStudent1100% (1)
- How To Prevent Cancer by David BrownsteinDokument16 SeitenHow To Prevent Cancer by David BrownsteinMisterSharer100% (7)
- Papillary Thyroid CarcinomaDokument17 SeitenPapillary Thyroid CarcinomaEster Sibarani100% (2)
- Prostate Cancer Therapy - What You Must KnowVon EverandProstate Cancer Therapy - What You Must KnowBewertung: 4 von 5 Sternen4/5 (1)
- ThyroidectomyDokument38 SeitenThyroidectomyMaria Paula BungayNoch keine Bewertungen
- Wngtlxkbm3snxfpzvp0qowhm PDFDokument2 SeitenWngtlxkbm3snxfpzvp0qowhm PDFUjjwal0% (1)
- Case Study - Toxic GoiterDokument22 SeitenCase Study - Toxic GoiterJohn Matley Caampued100% (2)
- ThyroidectomyDokument50 SeitenThyroidectomyKyle Jingco100% (2)
- A CASE REPORT: Hyperthyroidism in PregnancyDokument46 SeitenA CASE REPORT: Hyperthyroidism in PregnancyIrma Permata sariNoch keine Bewertungen
- Word ThyroidDokument20 SeitenWord Thyroiderwansyah1990Noch keine Bewertungen
- ThyroidCancer Brochure PDFDokument4 SeitenThyroidCancer Brochure PDFPutri Juita KhairatihNoch keine Bewertungen
- Thyroid Cancer TreatmentDokument3 SeitenThyroid Cancer TreatmentevanNoch keine Bewertungen
- Thyroid Cancer 1 Running Head: Thyroid CancerDokument9 SeitenThyroid Cancer 1 Running Head: Thyroid Cancerapi-280626728Noch keine Bewertungen
- Thyroid CancerDokument10 SeitenThyroid Canceraishaiqbal6789Noch keine Bewertungen
- Thyroid CancerDokument9 SeitenThyroid Cancerapi-346427317Noch keine Bewertungen
- ThyroidcancerDokument20 SeitenThyroidcancerReshma rsrNoch keine Bewertungen
- When To See A DoctorDokument11 SeitenWhen To See A DoctorMellisa Faith Yebes GoNoch keine Bewertungen
- About Thyroid Cancer: Overview and TypesDokument12 SeitenAbout Thyroid Cancer: Overview and TypesRum Afida RasfaNoch keine Bewertungen
- Questions and Answer of Thyroid Nodule: 1. What Are The Most Important Complications of Thyroid Surgery?Dokument4 SeitenQuestions and Answer of Thyroid Nodule: 1. What Are The Most Important Complications of Thyroid Surgery?Ranty Rizky PuspadewiNoch keine Bewertungen
- Diagnosis and Treatment Hot NoduleDokument4 SeitenDiagnosis and Treatment Hot NoduleGame overNoch keine Bewertungen
- Thyroid CancerDokument5 SeitenThyroid CancerJulia Rae Delos SantosNoch keine Bewertungen
- Thyroid Cancer Early Detection, Diagnosis, and StagingDokument24 SeitenThyroid Cancer Early Detection, Diagnosis, and StagingDao Trung HaiNoch keine Bewertungen
- Thyroid Cancer Basic InformationDokument2 SeitenThyroid Cancer Basic Informationberuangmadu777Noch keine Bewertungen
- Thyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e RDokument7 SeitenThyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e REndang Rahayu Fuji LestaryNoch keine Bewertungen
- Anaplastic Thyroid Cancer BrochureDokument3 SeitenAnaplastic Thyroid Cancer Brochurey8cp6nqvn2Noch keine Bewertungen
- Cancer of ThyroidDokument19 SeitenCancer of ThyroidFatima Zafar - BDSNoch keine Bewertungen
- Thyroid Nodule ThesisDokument8 SeitenThyroid Nodule ThesisCustomPaperServiceUK100% (2)
- Thyroid Nodules: What Is The Thyroid Gland?Dokument3 SeitenThyroid Nodules: What Is The Thyroid Gland?sougataNoch keine Bewertungen
- Collated Thyroid PBLDokument13 SeitenCollated Thyroid PBLnik_khadijah_2Noch keine Bewertungen
- What Is Radiation TherapyDokument5 SeitenWhat Is Radiation TherapyKinan Eiad Al-riyahiNoch keine Bewertungen
- Practice Essentials: Signs and SymptomsDokument20 SeitenPractice Essentials: Signs and SymptomsrainbowshopNoch keine Bewertungen
- The Thyroid Nodule: Clinical PracticeDokument8 SeitenThe Thyroid Nodule: Clinical PracticeAkhdan AufaNoch keine Bewertungen
- TP - Kanker Tiroid Diagnosis - Danial Sampepayung - KoreksiDokument7 SeitenTP - Kanker Tiroid Diagnosis - Danial Sampepayung - KoreksiAdhitya WicaksonoNoch keine Bewertungen
- Thyroid NodulesDokument43 SeitenThyroid NodulesRaker AMSANoch keine Bewertungen
- Advances in Management of Thyroid CancerDokument49 SeitenAdvances in Management of Thyroid Cancerazuresea01Noch keine Bewertungen
- Testicular Cancer Is A Disease in Which Cells Become Malignant (Cancerous) inDokument5 SeitenTesticular Cancer Is A Disease in Which Cells Become Malignant (Cancerous) inAngel CastroNoch keine Bewertungen
- Thyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e RDokument7 SeitenThyroid Cancer: Burden of Illness and Management of Disease: J o U R N A L o F C A N C e RRum Afida RasfaNoch keine Bewertungen
- Thyroid CancerDokument2 SeitenThyroid CancerReza SaraswatiNoch keine Bewertungen
- CA ThyroidDokument6 SeitenCA ThyroidBastiaanNoch keine Bewertungen
- Thyroid Cancer TreatmentDokument5 SeitenThyroid Cancer TreatmentMarielaTessyGonzalesParedesNoch keine Bewertungen
- Different Kinds of CancerDokument4 SeitenDifferent Kinds of CancerMaría Felix Ovalle Beitia (MaryFe)Noch keine Bewertungen
- Thyroid Cancer: ANATOMY AND PHYSIOLOGY: The Thyroid Is A Butterfly-Shaped Gland That Sits Low OnDokument9 SeitenThyroid Cancer: ANATOMY AND PHYSIOLOGY: The Thyroid Is A Butterfly-Shaped Gland That Sits Low OnRitika RanaNoch keine Bewertungen
- Workupandmanagementof Thyroidnodules: Derek A. Escalante,, Kelly G. AndersonDokument23 SeitenWorkupandmanagementof Thyroidnodules: Derek A. Escalante,, Kelly G. AndersonLauraNoch keine Bewertungen
- WileycancerDokument11 SeitenWileycancerapi-310375757Noch keine Bewertungen
- Thyroid Cancer Causes, Risk Factors, and PreventionDokument10 SeitenThyroid Cancer Causes, Risk Factors, and PreventionDavid RefuncionNoch keine Bewertungen
- Is Lic Ensed Unde R: CCB Y-NcDokument31 SeitenIs Lic Ensed Unde R: CCB Y-NcBinita ShresthaNoch keine Bewertungen
- Project CancerDokument4 SeitenProject CancerShinu BathamNoch keine Bewertungen
- Lung CancerDokument14 SeitenLung Cancerabhiram.08112006Noch keine Bewertungen
- Thyroid Carcinoma: Abhishek Thakur 1610050Dokument24 SeitenThyroid Carcinoma: Abhishek Thakur 1610050Abhishek ThakurNoch keine Bewertungen
- Goiter: Signs and Symptoms of GoitersDokument15 SeitenGoiter: Signs and Symptoms of GoitersGraceLanaNoch keine Bewertungen
- Ca Tiroid 2 PDFDokument11 SeitenCa Tiroid 2 PDFAlfindyNoch keine Bewertungen
- Lung CancerDokument4 SeitenLung Cancerapi-286974345Noch keine Bewertungen
- Thyroid Nodule PDFDokument21 SeitenThyroid Nodule PDFrima oktariniNoch keine Bewertungen
- Thyroid CancerDokument19 SeitenThyroid CancerPowell TabogocNoch keine Bewertungen
- Thyroid Surgery: Questions and ConsiderationsDokument2 SeitenThyroid Surgery: Questions and Considerationshoneysutton8Noch keine Bewertungen
- Cancer Risk FactorsDokument44 SeitenCancer Risk FactorsSalomo Galih NugrohoNoch keine Bewertungen
- AhmedDokument6 SeitenAhmedAbubaker sikyNoch keine Bewertungen
- Guideline ThyroidDokument21 SeitenGuideline ThyroidDesti EryaniNoch keine Bewertungen
- CancerDokument4 SeitenCancerUmer RafiqNoch keine Bewertungen
- Benign Liver Tumors: HemangiomaDokument6 SeitenBenign Liver Tumors: HemangiomaEnricoSetiawanNoch keine Bewertungen
- Cancer Screening: Dr. Waqar MunirDokument26 SeitenCancer Screening: Dr. Waqar MunirWaqar MunirNoch keine Bewertungen
- Safari - 29 Sep 2019 at 21:52Dokument1 SeiteSafari - 29 Sep 2019 at 21:52micaNoch keine Bewertungen
- CancerDokument3 SeitenCancershreya thakurNoch keine Bewertungen
- Endemic and Sporadic GoiterDokument13 SeitenEndemic and Sporadic GoiterBtwo SoelNoch keine Bewertungen
- Subclinical Hyperthyroidism Case ReportDokument26 SeitenSubclinical Hyperthyroidism Case ReportkapanjddokterNoch keine Bewertungen
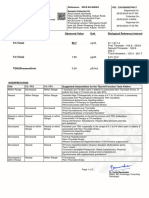
- Kumar Verma: Lab NoDokument3 SeitenKumar Verma: Lab NoSamar SinghNoch keine Bewertungen
- Frequency Rate of Thyroid DiseaseDokument118 SeitenFrequency Rate of Thyroid DiseaseMustafa KhandgawiNoch keine Bewertungen
- Review Sheet Laprak EndokrinDokument4 SeitenReview Sheet Laprak EndokrinrhismaNoch keine Bewertungen
- Kuretase Case Report 2Dokument3 SeitenKuretase Case Report 2Lydia AmaliaNoch keine Bewertungen
- Case StudyDokument4 SeitenCase Studyllyryc100% (1)
- Approach To Diagnosis and Management of Thyroid NoduleDokument11 SeitenApproach To Diagnosis and Management of Thyroid NoduleailegnacantikNoch keine Bewertungen
- Report-230109505074917 MRUNMAYEEMISHAL CUS10634 29feb2024 163753Dokument2 SeitenReport-230109505074917 MRUNMAYEEMISHAL CUS10634 29feb2024 163753mrunmayeemishal.neonarrativesNoch keine Bewertungen
- 2018 Dec Hypothyroidism IJCMASDokument5 Seiten2018 Dec Hypothyroidism IJCMASrociobendana2410Noch keine Bewertungen
- Lecture 26 TextDokument14 SeitenLecture 26 Textvarsha CRNoch keine Bewertungen
- Drugs Acting ON THE Endocrine SystemDokument81 SeitenDrugs Acting ON THE Endocrine SystemLuis WashingtonNoch keine Bewertungen
- Chapter 12 Coordination and Response (Repaired)Dokument18 SeitenChapter 12 Coordination and Response (Repaired)yokekeannNoch keine Bewertungen
- Goiter: What Is The Thyroid Gland?Dokument2 SeitenGoiter: What Is The Thyroid Gland?Julio LeviNoch keine Bewertungen
- EndoquestionssolvedDokument14 SeitenEndoquestionssolvedPuteri Nursyamimi Mohd SabilanNoch keine Bewertungen
- Psychoimmunology Essay by DR Romesh Senewiratne-Alagaratnam (MD)Dokument32 SeitenPsychoimmunology Essay by DR Romesh Senewiratne-Alagaratnam (MD)Dr Romesh Arya Chakravarti100% (2)
- Pathology Lab V Diffuse and Multinodular Goiter.Dokument18 SeitenPathology Lab V Diffuse and Multinodular Goiter.Jeffry Chandra TjahayadiNoch keine Bewertungen
- Laboratory Report: Immunology Thyroid Function TestDokument1 SeiteLaboratory Report: Immunology Thyroid Function Testudesh LuitelNoch keine Bewertungen
- Thyroid Hormones: K.Ramachandran M.Sc. Medical Biochemistry SRM Medical CollegeDokument31 SeitenThyroid Hormones: K.Ramachandran M.Sc. Medical Biochemistry SRM Medical CollegeKuzhandai VeluNoch keine Bewertungen
- Herbal Drugs For Thyroid - PDF: International Journal of Pharmacy and Biological Sciences May 2016Dokument10 SeitenHerbal Drugs For Thyroid - PDF: International Journal of Pharmacy and Biological Sciences May 2016Sanju TkNoch keine Bewertungen
- The Metabolic Solution Ebook PDFDokument26 SeitenThe Metabolic Solution Ebook PDFCynthia WiikNoch keine Bewertungen
- 162 - 4187 - Hermina Novida - GalleyDokument5 Seiten162 - 4187 - Hermina Novida - Galleyaulia fikriNoch keine Bewertungen
- 1678816971346634Dokument47 Seiten1678816971346634SophiyaNoch keine Bewertungen
- Assessment of Serum Minerals and Electrolytes in TDokument5 SeitenAssessment of Serum Minerals and Electrolytes in THasni M MarsaolyNoch keine Bewertungen
- GoiterDokument14 SeitenGoiterMiracle ShopNoch keine Bewertungen