Beruflich Dokumente
Kultur Dokumente
EKGpart II
Hochgeladen von
Sarif CassanovaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
EKGpart II
Hochgeladen von
Sarif CassanovaCopyright:
Verfügbare Formate
Electrocardiography Review Part II Blocks and Injury Patters Ben Lawner, MS-I, NSUCOM
ATRIOVENTRICULAR BLOCK
Heart block simply means that an interruption exists in the pattern of conduction from the atria to the ventricles. Heart block is traditionally categorized in terms of degrees. The degree of heart block specifices the type of conduction abnormality. The review handout features three major types of heart block as seen on the electrocardiogram.
FIRST DEGREE ATRIOVENTRICULAR BLOCK
First degree AV block is simply a prolongation of the P-R interval. Recall that a normal PR interval is 0.12 to 0.20 seconds. Therefore, PR intervals longer than five small horizonal boxes are classified as first degree. First degree heart block can be induced with pharmacological agents or may be indicative of damage to the SA node. In first degree heart block, conduction is still 1:1 (one QRS per P wave.)
SECOND DEGREE AV BLOCK, TYPE ONE
Two types of second degree blocks exist. In type one second degree block (Wenckebach- pronounced WINKYBOK), the PR interval gets progressively longer until a QRS is eventually dropped. Simply put, the impulse from the AV node is eventually not conducted through the ventricular/purkinje system. So, second degree AV block (TYPE ONE) features a progressively lengthening PR interval. Eventually, a dropped beat occurs. The EKG strip below shows a progressive elongation of the PRI in QRS complexes one through three. No QRS occurs after the fourth P wave. This pattern typically repeats.
SECOND DEGREE AV BLOCK, TYPE TWO
Type two block features a mismatch in P:QRS conduction. Some P waves fail to cause ventricular conduction. Lengthening of the PRI typically does not occur. The hallmark of type two second degree block is that it takes successive P waves to stimulate the ventricles. Often, 2:1 or 3:1 conduction occurs in second degree, type II AV block.. The EKG strip below illustrates a 3:1 type II second degree heat block. Notice that the first three P waves show 1 to 1 conduction. One P produces one QRS. The next part of the EKG strip showcases some lonely P waves. Observe that three P waves are required to produce ventricular depolarization. This pattern of 3:1 or 2:1 conduction will often repeat itself. This type of block is especially dangerous because it usually indicates myocardial ischemia or damage. Patients exhibiting type II second degree block can deteriorate into third degree block and eventual sinus arrest.
THIRD DEGREE HEART BLOCK
Third degree heart block occurs when the SA node and the ventricles are having two simultaneous, but different conversations. The atrial pacemakers are firing but do not produce a conducted QRS. The atria are firing at their own intrinsic rate, and the ventricles depolarize independently. Though the P waves occur at regular intervals, they are often randomly dispersed throughout a following QRS complex. Think of third degree heart block as dissociated communication. Third degree is often called, complete heart block because none of the atrial depolarizations are conducted to the ventricles. Note the regular R to R intervals and P to P intervals.
In the tracing below, the first visible P wave occurs before the QRS. The second P wave occurs after the QRS complex. The third P wave is buried in the T wave of the following QRS complex. Though the interval from P wave to P wave is probably regular, the P waves DO NOT cause ventricular depolarization.
MYOCARDIAL INJURY PATTERS AS SEEN ON THE EKG
12 lead EKGs take a more complete heart picture and provide valuable insight into the heart as it sits within the coronal and horizontal planes. Abnormalities of the ST segment and axis deviations convey much about cardiac pathology to the treating physician. The review handout will list the three most significant types of ST segment abnormalities. A) Inverted T waves=ISCHEMIA Flipped, or upside-down T waves are sometimes indicitave of ischemia. Patients who are hypoxic often exhibit changes in ventricular repolarization. T waves are normally upright in all leads except aVR. In symptomatic patients, inverted T waves may herald infarction. T waves can also be changed by hypertrophy, pharmacological agents, and stress. Simply be aware that flipped T waves may indicate abnormalities. Classical ischemic T waves are both SYMMETRICAL and inverted. In limb leads, MINIMAL T wave inversion may be associated with normal ADULT variants. T wave inversion in V (precordial leads) V2-V6 is pathological. B) ST segment depression=INJURY When the ST segment dives below the baseline of the EKG, myocardial ischemia is often present. ST segment depression exists when the entire ST segment sits >1mm (one small box) below the baseline.
C) ST segment elevation=INFARCT ST segment elevation above the baseline is often indicative of myocardial injury. Significant ST elevation occurs when the entire segment is elevated > 1 mm above the baseline. Pathological ST elevation occurs when the elevation is present in two or more CONTIGUOUS leads. Always correlate EKG findings with patient presentation. Indeed, physicians have varying standards as to the degree of ST elevation that is considered pathognomonic for myocardial infarction. Some doctors have suggested that any ST elevation of 1mm or greater is abnormal. Others postulate that elevation of 2mm or more is problematic. Simply put, always investigate ST elevation that is present in two or more contiguous leads. Interestingly enough, the leads of the EKG correspond to areas of the heart injured from ischemia. That is to say, the finding of ST elevation in specific leads helps the physician to localize myocardial injury. ST elevation is often the earliest sign of a heart attack. ST elevation >1mm that is present in contiguous leads should be vigorously worked up. The patters of injury are not important for the cardiovascular physiology examination, but they might be good for impressing IGC mentors. They are provided for your information only. Often, the clinician will observe reciprocal changes in the EKG leads that are roughly opposite to the ones displaying abnormal findings. Simply put, changes in one section of the myocardium often affect adjacent locations. Anterior wall injuries produce changes in the inferior wall, and lateral wall injury might cause changes in the posterior myocardium. For your information only: LOCATION OF INJURY Anterior Septal Inferior Anterio-lateral Lateral Posterior INDICATIVE CHANGES (ST ELEVATION/DEPRESSION) I and aVL, V1-V6 V1, V2 II, III, aVF I and aVL, V5-V6 I and aVL, V5-V6 V1-V3 **often ST depression ARTERY OFTEN AFFECTED Left anterior descending Right coronary artery Circumflex (similar to anterior MI pattern) Right coronary artery
The EKG below has ST elevation in leads I and AVL. Massive ST elevation is seen in leads V1 through V4. This patient is having massive anterior-septal wall MI with some lateral wall involvement. This is often a lethal MI pattern due to occlusion of the big guy, the left anterior descending. Axis, anyone??
The EKG below demonstrates a classic inferior wall injury pattern. There is massive, obvious ST elevation in leads II, III, and AVF. Unfortunately, this patient is also experiencing a massive right ventricular wall infarction. Notice the EKG reads, right side chest leads. Instead of placing V1-V6 on the LEFT patients chest, the electrodes are placed on the RIGHT side of the patients chest. Physicians often order a right side chest lead EKG to rule out simultaneous right ventricular wall infarction. This patients ability to handle decreases in preload is severely compromised and is at risk for bradycardia and hypotension. USE EXTREME CAUTION in administering NTG to patients with RV infarction. They will quickly decompensate.
The following patient has EKG changes in many leads. ST depression exists in leads one and aVL, which is consistent with ST elevation in II, III, and aVF. ST elevation in II, III, and aVF is most consistent with an inferior wall infarction. It might be a good idea to check right sided chest leads in this patient.
Das könnte Ihnen auch gefallen
- NIH Public Access: Author ManuscriptDokument20 SeitenNIH Public Access: Author ManuscriptSarif CassanovaNoch keine Bewertungen
- BouhnikDokument9 SeitenBouhnikSarif CassanovaNoch keine Bewertungen
- Rekap Anggota DPD Ipai Sulawesi Selatan Dan Barat: Tana TorajaDokument3 SeitenRekap Anggota DPD Ipai Sulawesi Selatan Dan Barat: Tana TorajaSarif CassanovaNoch keine Bewertungen
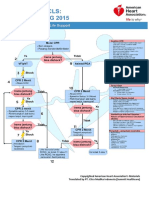
- Algoritma ACLS Bhs IndonesiaDokument6 SeitenAlgoritma ACLS Bhs IndonesiaSarif CassanovaNoch keine Bewertungen
- Management of Foreskin ConditionsDokument26 SeitenManagement of Foreskin ConditionsSarif CassanovaNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Case Study 5.6.1 JOHNSON AND JOHNSONDokument2 SeitenCase Study 5.6.1 JOHNSON AND JOHNSONnaman0% (1)
- DPN Icu PDFDokument1 SeiteDPN Icu PDFharoonNoch keine Bewertungen
- Florida Physician Database - Areas Includes Gainesville, Orlando and JacksonvilleDokument20 SeitenFlorida Physician Database - Areas Includes Gainesville, Orlando and JacksonvilleBhuvana RajendranNoch keine Bewertungen
- MLT Student NotesDokument5 SeitenMLT Student NotesClaire GonzalesNoch keine Bewertungen
- Tramadol, Paracetamol, Calmoseptine, B12Dokument5 SeitenTramadol, Paracetamol, Calmoseptine, B12Denise EspinosaNoch keine Bewertungen
- Sekilas Info: CardiomyopathyDokument15 SeitenSekilas Info: CardiomyopathyZukmianty SuaibNoch keine Bewertungen
- Alexandra Mcfall - Annotated BibliographyDokument6 SeitenAlexandra Mcfall - Annotated Bibliographyapi-549246948Noch keine Bewertungen
- JuRnal 6 PDFDokument8 SeitenJuRnal 6 PDFNurhajar AzzahraNoch keine Bewertungen
- DisabilityDokument450 SeitenDisabilityTony Kelbrat100% (1)
- GH 13 600Dokument9 SeitenGH 13 600Gar BettaNoch keine Bewertungen
- Rituximab Tullus Kjeil 2021Dokument9 SeitenRituximab Tullus Kjeil 2021Carmen MunteanNoch keine Bewertungen
- 4th Week Health ModulesDokument13 Seiten4th Week Health ModulesYza VelleNoch keine Bewertungen
- Patel 2013Dokument8 SeitenPatel 2013joantyy 1Noch keine Bewertungen
- 4788 ID Faktor Risiko Lingkungan Kejadian Leptospirosis Di Jawa Tengah Studi Kasus Di Ko PDFDokument8 Seiten4788 ID Faktor Risiko Lingkungan Kejadian Leptospirosis Di Jawa Tengah Studi Kasus Di Ko PDFbintang nurzakiahNoch keine Bewertungen
- CONFUSION TextoDokument15 SeitenCONFUSION TextoBarbara SolangeNoch keine Bewertungen
- Sean Benesh Resume 10-1-23Dokument2 SeitenSean Benesh Resume 10-1-23api-708800698Noch keine Bewertungen
- Respiratory MCQDokument24 SeitenRespiratory MCQfrabziNoch keine Bewertungen
- Pathophysiology of Septic ShockDokument19 SeitenPathophysiology of Septic ShockRoberto López MataNoch keine Bewertungen
- Role of Presepsin in Determining The Incidence of Septic Shock and Mortality in Patients With SepsisDokument8 SeitenRole of Presepsin in Determining The Incidence of Septic Shock and Mortality in Patients With Sepsisfaraz.mirza1Noch keine Bewertungen
- Hospital Payment Systems Based On DiagnosisDokument16 SeitenHospital Payment Systems Based On DiagnosisErma HandayaniNoch keine Bewertungen
- The Prevalence of Severe Malaria in Children Below Five Years of Age at Hoima Regional Referral Hospital, Hoima CityDokument9 SeitenThe Prevalence of Severe Malaria in Children Below Five Years of Age at Hoima Regional Referral Hospital, Hoima CityKIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- Homeopathy and Placebo - Synonym, Similar or Different?: Frank Zimmermann-Viehoff Karin MeissnerDokument2 SeitenHomeopathy and Placebo - Synonym, Similar or Different?: Frank Zimmermann-Viehoff Karin MeissnerSaim ShahNoch keine Bewertungen
- Community - Based NursingDokument16 SeitenCommunity - Based NursingManu CvNoch keine Bewertungen
- Developmental Endocrine Reproductive Toxicologist in NJ NY Resume Edward FrizellDokument7 SeitenDevelopmental Endocrine Reproductive Toxicologist in NJ NY Resume Edward FrizellEdwardFrizellNoch keine Bewertungen
- Vibrio Cholerae PosterDokument1 SeiteVibrio Cholerae PosterStela MonkNoch keine Bewertungen
- The Icd - 10 DictionaryDokument10 SeitenThe Icd - 10 DictionarySeraphin MulambaNoch keine Bewertungen
- PCOL Notes 001 IntroDokument1 SeitePCOL Notes 001 IntroCansNoch keine Bewertungen
- Or NCP (Risk For Infection)Dokument1 SeiteOr NCP (Risk For Infection)Nikki M. Arapol100% (1)
- Stroke Mimics: Clinical and Radiological Evaluation: Poster No.: Congress: Type: Authors: KeywordsDokument20 SeitenStroke Mimics: Clinical and Radiological Evaluation: Poster No.: Congress: Type: Authors: KeywordsOrlin ZlatarskiNoch keine Bewertungen
- BHW Reference Manual and Playbook - TagalogDokument136 SeitenBHW Reference Manual and Playbook - TagalogCarlen Mae L. YacapinNoch keine Bewertungen