Beruflich Dokumente
Kultur Dokumente
Hemodialysis
Hochgeladen von
Ganda SihotangOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Hemodialysis
Hochgeladen von
Ganda SihotangCopyright:
Verfügbare Formate
Ganda Sihotang Blocking A1 Hemodialysis
The objectives of hemodialysis are to extract toxic nitrogenous substances from the blood and to remove excess water. A dialyzer (also referred to as an artificial kidney) serves as a synthetic semipermeable membrane, replacing the renal glomeruli and tubules as the filter for the impaired kidneys. In hemodialysis, the blood, laden with toxins and nitrogenous wastes, is diverted from the patient to a ma- chine, a dialyzer, where toxins are filtered out and removed and the blood is returned to the patient. Hemodialysis is used for patients who are acutely ill and re- quire short-term dialysis (days to weeks) and for patients with advanced CKD and ESRD who require long-term or permanent renal replacement therapy. Hemodialysis pre- vents death but does not cure renal disease and does not compensate for the loss of endocrine or metabolic activities of the kidneys. The preferred method of permanent access is an arteriovenous fistula (AVF) that is created surgically (usually in the forearm) by joining (anastomosing) an artery to a vein, either side to side or end to side Most patients receive intermittent he- modialysis that involves treatments three times a week with the average treatment duration of 3 to 4 hours in an outp aient setting. The patient and a caregiver can also perform hemodialysis at home. With home dialysis, treat- ment time and frequency can be adjusted to meet optimal patient needs. With the initiation of dial- ysis, disturbances of lipid metabolism (hypertriglyceridemia) are accentuated and contribute to cardiovascular complica- tions. Heart failure, coronary heart disease, angina, stroke, and peripheral vascular insufficiency may occur and can in- capacitate the patient.
Adequate dialysis costs from P25,000 to P46,000 per month
Continuous renal replacement therapies
. CRRT provides slow and balanced fluid removal that even unstable patients - those with shock or severe fluid overload - can more easily tolerate. CRRT is indicated in any patient who meets criteria for hemodialysis therapy but cannot tolerate intermittent dialysis due to hemodynamic instability. CRRT is better tolerated by hemodynamically unstable patients because fluid volume, electrolytes and pH are adjusted slowly and steadily over a 24 hour period rather than a 3 4 hour period. There are two options for vascular access for CRRT, venovenous and arteriovenous. Venovenous access is by far the most commonly used in the modern ICU. Suitable for use in hemodynamically unstable patients. Precise volume control, which is immediately adaptable to changing circumstances. Very effective control of uremia, hypophosphatemia and hyperkalemia. Rapid control of metabolic acidosis Improved nutritional support (full protein diet). Available 24 hours a day with minimal training. Expense probably the same as IHD. Anticoagulation to prevent extracorporeal circuit from clotting. Complications of line insertion and sepsis. Risk of line disconnection. Cost the same as HD
Peritoneal Dialysis -The process uses the patient's peritoneum in the abdomen as a membrane across which fluids and dissolved substances (electrolytes, urea, glucose, albumin and other small molecules) are exchanged from the blood. PD may be the treatment of choice for patients with renal failure who are unable or unwilling to undergo hemodialysis or renal transplantation. -The amount of dialysis that occurs depends on the volume of the dwell, the regularity of the exchange and the concentration of the fluid. APD cycles between 3 and 10 dwells per night, while CAPD involves four dwells per day of 2-2.5 litres per dwell, with each remaining in the abdomen for 48 hours -The costs and benefits of hemodialysis and PD are roughly the same
PD equipment is cheaper but the costs associated with peritonitis are higher.[4] Patient's on PD are seen less often in the ER as they are typically more compliant with treatment, and dialysis occurs more frequently and thus not allowing the waste to accumulate in the blood for several days.
-PD is less efficient at removing wastes from the body than hemodialysis, and the only drawback is the presence of the tube presents a risk of peritonitis due to the potential to introduce bacteria to the abdomen;[3] peritonitis is best treated through the direct infusion of antibiotics into the peritoneum with no advantage for other frequently used treatments such as routine peritoneal lavage or use of urokinase[9] The tube site can also become infected NURSING MANAGEMENT
Promoting Pharmacologic Therapy
Patients undergoing hemodialysis who require medica- tions (eg, cardiac glycosides, antibiotic agents, antiarrhyth- mic medications, antihypertensive agents) are monitored closely to ensure that blood and tissue levels of these med- ications are maintained without toxic accumulation. Promoting Nutritional and Fluid Therapy Diet is important for patients on hemodialysis because of the effects of uremia. Goals of nutritional therapy are to minimize uremic symptoms and fluid and electrolyte imbalances; to maintain good nutritional status through adequate protein, calorie, vitamin, and mineral intake; and to enable the patient to eat a palatable and enjoyable diet. Meeting Psychosocial Need Patients requiring long-term hemodialysis are often concerned about the unpredictability of the illness and the disruption of their lives. Calculate Dosage The standard HD prescription targets fluid removal to a clinically derived estimate of dry weight. Dry weight is currently defined as the lowest weight a patient can tolerate without the development of symptoms or hypotension. So based on the dry weight and the clients weight during the start of the procedure we can come up with the ultrafiltration rate.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Freelance Contract AgreementDokument10 SeitenFreelance Contract AgreementGayathri Prajit100% (1)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- We Are An OfferingDokument1 SeiteWe Are An OfferingGanda Sihotang100% (3)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- I Can Trust JesusDokument6 SeitenI Can Trust JesusGanda SihotangNoch keine Bewertungen
- FM Solved ProblemsDokument28 SeitenFM Solved ProblemsElisten DabreoNoch keine Bewertungen
- Starbucks Delivering Customer Service Case Solution PDFDokument2 SeitenStarbucks Delivering Customer Service Case Solution PDFRavia SharmaNoch keine Bewertungen
- Basic Services and Facilities Matrix - Local Gov''tDokument2 SeitenBasic Services and Facilities Matrix - Local Gov''tMishi Liao100% (2)
- Gmu Unofficial TranscriptDokument3 SeitenGmu Unofficial Transcriptapi-491861804Noch keine Bewertungen
- First God OutlineDokument4 SeitenFirst God OutlineGanda SihotangNoch keine Bewertungen
- Analytical and Critical Thinking SkillsDokument2 SeitenAnalytical and Critical Thinking SkillsGanda SihotangNoch keine Bewertungen
- The LiverDokument15 SeitenThe LiverGanda SihotangNoch keine Bewertungen
- Insurance Companies IndoDokument3 SeitenInsurance Companies IndoGanda SihotangNoch keine Bewertungen
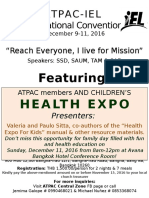
- Atpac Iel PosterDokument1 SeiteAtpac Iel PosterGanda SihotangNoch keine Bewertungen
- Favourite Medical Tourism DestinationsDokument2 SeitenFavourite Medical Tourism DestinationsGanda SihotangNoch keine Bewertungen
- Bic Army of Faith ObjectivesDokument1 SeiteBic Army of Faith ObjectivesGanda SihotangNoch keine Bewertungen
- His Hands Sheet Music PDFDokument6 SeitenHis Hands Sheet Music PDFGanda SihotangNoch keine Bewertungen
- Immuniation Schedule Hs 472Dokument2 SeitenImmuniation Schedule Hs 472api-272755914Noch keine Bewertungen
- Passion FruitDokument22 SeitenPassion FruitGanda SihotangNoch keine Bewertungen
- Song ServiceDokument23 SeitenSong ServiceGanda SihotangNoch keine Bewertungen
- CmeDokument1 SeiteCmeGanda SihotangNoch keine Bewertungen
- Singapore Losing Medical Tourist To NeighborsDokument2 SeitenSingapore Losing Medical Tourist To NeighborsGanda SihotangNoch keine Bewertungen
- Passion FruitDokument22 SeitenPassion FruitGanda SihotangNoch keine Bewertungen
- AXA Company Profile 2015 (Eng) - LowresDokument8 SeitenAXA Company Profile 2015 (Eng) - LowresGanda SihotangNoch keine Bewertungen
- Passion FruitDokument22 SeitenPassion FruitGanda SihotangNoch keine Bewertungen
- Premium Table (English) - LowresDokument2 SeitenPremium Table (English) - LowresGanda SihotangNoch keine Bewertungen
- Medical TerminologyDokument4 SeitenMedical TerminologyGanda SihotangNoch keine Bewertungen
- Brotherly KindnessDokument2 SeitenBrotherly KindnessGanda SihotangNoch keine Bewertungen
- AYA VolleyballScoreSheet FINALDokument1 SeiteAYA VolleyballScoreSheet FINALGanda SihotangNoch keine Bewertungen
- HemodialysisDokument2 SeitenHemodialysisGanda SihotangNoch keine Bewertungen
- HemodialysisDokument2 SeitenHemodialysisGanda SihotangNoch keine Bewertungen
- Cancer PathophysiologyDokument1 SeiteCancer PathophysiologyGanda Sihotang100% (1)
- VII. in Christ We Are All Free and United by IDENTITY (Salvation) & Purpose (Service), So Therefore We Are Saved To Serve!Dokument1 SeiteVII. in Christ We Are All Free and United by IDENTITY (Salvation) & Purpose (Service), So Therefore We Are Saved To Serve!Ganda SihotangNoch keine Bewertungen
- Health Care DocumentDokument44 SeitenHealth Care DocumentGanda SihotangNoch keine Bewertungen
- Adoesence 2Dokument2 SeitenAdoesence 2Ganda SihotangNoch keine Bewertungen
- Lumbar Puncture: Gelvi Brylle Pelpinosas" &" Ganda Boy Sihotang" A5"Dokument10 SeitenLumbar Puncture: Gelvi Brylle Pelpinosas" &" Ganda Boy Sihotang" A5"Ganda SihotangNoch keine Bewertungen
- Internship ReportDokument2 SeitenInternship ReportFoxyNoch keine Bewertungen
- Tia-Eia-Is 801-1 - 2001Dokument148 SeitenTia-Eia-Is 801-1 - 2001John UrdanetaNoch keine Bewertungen
- XC3000 Series Motion Control System of Laser Cutting Commissioning Manual TextDokument138 SeitenXC3000 Series Motion Control System of Laser Cutting Commissioning Manual Textgerardo.reynosoNoch keine Bewertungen
- How To Create The Approval Transaction Type For AMEDokument5 SeitenHow To Create The Approval Transaction Type For AMERehmat RehmatNoch keine Bewertungen
- KACE SeDokument63 SeitenKACE SeAbdul RahimNoch keine Bewertungen
- Polymer AbbreviationsDokument9 SeitenPolymer AbbreviationsFernando GuerreroNoch keine Bewertungen
- FDI and FIIDokument17 SeitenFDI and FIIsharathNoch keine Bewertungen
- Queen Elizabeth Olympic Park, Stratford City and Adjacent AreasDokument48 SeitenQueen Elizabeth Olympic Park, Stratford City and Adjacent AreasRavi WoodsNoch keine Bewertungen
- Policy 0000000001523360 PDFDokument15 SeitenPolicy 0000000001523360 PDFunique infraNoch keine Bewertungen
- 0 - Resume - Preity Thadani PDFDokument3 Seiten0 - Resume - Preity Thadani PDFClash ClashhNoch keine Bewertungen
- Refill Brand Guidelines 2Dokument23 SeitenRefill Brand Guidelines 2Catalin MihailescuNoch keine Bewertungen
- Q1 LAS 4 FABM2 12 Week 2 3Dokument7 SeitenQ1 LAS 4 FABM2 12 Week 2 3Flare ColterizoNoch keine Bewertungen
- Airbus Settles Fettling Dust With Clean Air SolutionDokument1 SeiteAirbus Settles Fettling Dust With Clean Air SolutionstephendixNoch keine Bewertungen
- Lesson 12: Parallel Transformers and Autotransformers: Learning ObjectivesDokument13 SeitenLesson 12: Parallel Transformers and Autotransformers: Learning ObjectivesRookie Thursday OrquiaNoch keine Bewertungen
- Types of IndexDokument4 SeitenTypes of IndexKantha EnduriNoch keine Bewertungen
- Toyota PDFDokument3 SeitenToyota PDFPushp ToshniwalNoch keine Bewertungen
- Materials Science and Engineering ADokument10 SeitenMaterials Science and Engineering Akhudhayer1970Noch keine Bewertungen
- Montgomery vs. Daly - The Banking SwindleDokument11 SeitenMontgomery vs. Daly - The Banking SwindlequarantinedNoch keine Bewertungen
- Manual of Infection Prevention and Control (PDFDrive)Dokument399 SeitenManual of Infection Prevention and Control (PDFDrive)அந்தோணி சாமி100% (1)
- Thousands of Relocation Jobs Await You Anytime, Anywhere!: About UsDokument3 SeitenThousands of Relocation Jobs Await You Anytime, Anywhere!: About UsWeackson Guerrier100% (1)
- Makalah MGR Promot - Clma Gravity - p2pd TmminDokument27 SeitenMakalah MGR Promot - Clma Gravity - p2pd TmminSandi SaputraNoch keine Bewertungen
- Yosys+Nextpnr: An Open Source Framework From Verilog To Bitstream For Commercial FpgasDokument4 SeitenYosys+Nextpnr: An Open Source Framework From Verilog To Bitstream For Commercial FpgasFutsal AlcoletgeNoch keine Bewertungen
- QuickTransit SSLI Release Notes 1.1Dokument12 SeitenQuickTransit SSLI Release Notes 1.1subhrajitm47Noch keine Bewertungen
- HPDokument71 SeitenHPRazvan OracelNoch keine Bewertungen
- Antenna MCQsDokument38 SeitenAntenna MCQsAishwarya BalamuruganNoch keine Bewertungen