Beruflich Dokumente
Kultur Dokumente
CME Trunk, Abdomen, and Pressure Sore Reconstruction
Hochgeladen von
Veronica TomaselloOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CME Trunk, Abdomen, and Pressure Sore Reconstruction
Hochgeladen von
Veronica TomaselloCopyright:
Verfügbare Formate
CME
Trunk, Abdomen, and Pressure Sore Reconstruction
Salah Rubayi, M.D. Bala S. Chandrasekhar, M.D.
Downey and Los Angeles, Calif.
Learning Objectives: After reading this article, the participant should be able to: 1. Describe the principles of wound closure, torso reconstruction, and pressure sore reconstruction. 2. Outline standard options to treat defects of the chest, abdomen, and back and pressure ulcers in all anatomical areas. 3. Manage and prevent pressure ulcers. Summary: Chest wall reconstruction is indicated following tumor resection, radiation wound breakdown, or intrathoracic sepsis. Principles of wound closure and chest wall stabilization, where indicated, are discussed. Principles of abdominal wall reconstruction continue to evolve with the introduction of newer bioprosthetics and the application of functional concepts for wound closure. The authors illustrate these principles using commonly encountered clinical scenarios and guidelines to achieve predictable results. Pressure ulcers continue to be devastating complications to patients health and a functional hazard when they occur in the bedridden, in patients with spinal cord injuries, and in patients with neuromuscular disease. Management of pressure ulcers is also very expensive. The authors describe standard options to treat defects of the chest, abdomen, and back and pressure ulcers in all anatomical areas. A comprehensive understanding of principles and techniques will allow practitioners to approach difficult issues of torso reconstruction and pressure sores with a rational confidence and an expectation of generally satisfactory outcomes. With pressure ulcers, prevention remains the primary goal. Patient education and compliance coupled with a multidisciplinary team approach can reduce their occurrence significantly. Surgical management includes appropriate patient selection, adequate debridement, soft-tissue coverage, and use of flaps that will not limit future reconstructions if needed. Postoperatively, a strict protocol should be adapted to ensure the success of the flap procedure. Several myocutaneous flaps commonly used for the surgical management of pressure are discussed. Commonly used flaps in chest and abdominal wall reconstruction are discussed and these should be useful for the practicing plastic surgeon. (Plast. Reconstr. Surg. 128: 201e, 2011.)
CHEST WALL RECONSTRUCTION
cquired chest wall defects result from trauma, tumor excision, radiation injury, complication caused by cardiac bypass surgery (Fig. 1), or sepsis from intrathoracic disease, such as bronchopleural fistulas.1 Full-thickness lateral chest wall defects and those involving multiple rib resections may also cause a flail chest.2,3 Reconstructive goals include eradication of infection, airtight pleural cavFrom the Department of Surgery, Rancho Los Amigos National Rehabilitation Center, and the Division of Plastic and Reconstructive Surgery, Keck School of Medicine, University of Southern California. Received for publication November 20, 2009; accepted February 17, 2011. Copyright 2011 by the American Society of Plastic Surgeons DOI: 10.1097/PRS.0b013e31822214c1
ity seal, skeletal stabilization, and wound closure. (See Video 1, which contains case studies that demonstrate principles of chest and abdominal wall reconstruction, available in the Related Videos sec-
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Video content is available for this article. The videos can be found under the Related Videos section of the full-text article, or, for Ovid users, using the URL citations printed in the article.
www.PRSJournal.com
201e
Plastic and Reconstructive Surgery September 2011
Fig. 1. Irradiated chest wall following mastectomy, with underlying chondritis and osteomyelitis.
Video 1. Video 1, which contains case studies that demonstrate principles of chest andabdominal wall reconstruction, is availablein the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A373.
tion of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A373.) Preoperative Evaluation Pulmonary function tests, bronchoscopy, and computed tomographic scans are often indicated to delineate and characterize specific problems. Tumor size and invasion of surrounding structures, presence of intrathoracic infection, and rib cage abnormality are identified. Important comorbidities such as diabetes, history of irradiation, smoking history, and nutritional status are noted and optimized. Angiography is unnecessary unless there is a question about the vascular supply of proposed muscle flaps. Culture-specific antibiotics are used where indicated.
Principles of Reconstruction The primary pathologic findings will often dictate reconstructive goals. Infected and devitalized tissue is excised initially. Irradiated wounds often involve bone and cartilage under the necrotic soft tissue, and a full-thickness chest wall resection may be indicated as a first step in wound closure.1 Once the defect is identified, the goals become clearer. Chest wall stability, if needed, is restored simply with prosthetic mesh or human acellular dermal matrix sutured to the edges of the defect.1 4 The visceral pleura will adhere to and create an airtight seal. Stabilization is indicated in lateral full-thickness wounds, especially if more than six ribs are resected. Smaller defects generally do not need this, as scar formation beneath the soft-tissue cover will provide sufficient rigidity. Sternal and costal cartilage resection for osteomyelitis generally does not need stabilization. Large soft-tissue defects are closed with pectoralis major or latissimus dorsi flaps. Serratus flaps work well for closure of bronchopleural fistulas, as they are small and can be moved into the thorax easily either through a previous thoracotomy incision, creating a window in the intercostal space, or by rib resection and creation of a new passage.2,5 The approach depends on the fistula location and available local muscle flap. Less common are superiorly based transverse rectus abdominis musculocutaneous flaps, pedicled greater omental flaps, and rectus abdominis flaps. The pedicled greater omentum can close extremely large defects well1,6,7 and can be harvested laparoscopically.8 (See Video 1, which contains case studies that demonstrate principles of chest and abdominal wall reconstruction, available in the Related Videos section of the full-text ar-
202e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
ticle on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A373.) The irradiated chest wall wound presents unique problems. The borders of the damaged tissue are indistinct and adequacy of the resection is, at best, an educated guess. This wound is prone to infection, and use of prosthetic mesh is relatively contraindicated. Generous wound debridement including un derlying ribs followed by healthy muscle flap rotation offers the best chance for healing. Sternal osteomyelitis following cardiac surgery is fatal unless managed aggressively (Fig. 2, left). The infection can involve cardiac suture lines, prosthetic valves, and grafts (Fig. 2, right). Wide debridement of all infected bone, cartilage, and soft-tissue and elimination of the mediastinal dead space with vascularized tissue should be considered as soon as the diagnosis is made. Bilateral pectoralis major flaps based on the thoracoacromial pedicle are excellent options for sternal reconstruction.9 A rectus abdominis muscle turnover flap is used for lower sternal coverage if needed. For deep mediastinal wounds, omental flaps may be the best choice.7 ware when possible, and vascularized tissue coverage remain the keys for successful outcomes. Depending on the size and location of the defects, one may use latissimus, trapezius, gluteus maximus, or paraspinal muscle flaps for wound closure. The superior gluteal artery perforator flap is an alternate choice for lower lumbar or sacral defects.
CONGENITAL DEFORMITIES
Pectus Excavatum Pectus excavatum is the most common congenital defect and is thought to be a result of overgrowth of rib cartilages, pushing the sternum toward the spine and causing the typical funnel-shaped chest. Cardiorespiratory dysfunction is common in severe deformities. Mild deformations can be left alone or camouflaged with custom silicone implants placed submuscularly.10 Sternal reconstruction is indicated in children with functional problems such as dyspnea, decreased exercise tolerance, or tachycardia. The Nuss procedure is designed to slip a convex steel bar under the sternum and stabilize it in an anterior position for 2 to 5 years. This procedure is best performed by experienced pediatric thoracic surgeons. Teenagers or older patients will require resection of the diseased costal cartilages, sternal osteotomy, and rigid support.11,12 Meningomyelocele Meningomyelocele is the most common variant of spina bifida, where the neural elements of
POSTERIOR TRUNK DEFECTS
Back wounds are created by trauma, tumor resection, or radiation therapy. Urgent closure is indicated for coverage of exposed hardware used for spinal stabilization. Reconstructive principles of radical wound debridement, removal of hard
Fig. 2. (Left) Sternal osteomyelitis and mediastinitis following aortic arch replacement with a Dacron graft. (Right) Exposed Dacron graft aortic arch replacement after sternal de bridement.
203e
Plastic and Reconstructive Surgery September 2011
the spinal cord or cauda equina are exposed in the newborn baby. Neurologic deficits include weakness in the lower extremities, bowel and bladder dysfunction, and hydrocephalus. Latex allergies are also common in these infants. Urgent coverage of the wound is indicated. The neurosurgeon closes the dural defect and seals the cerebrospinal fluid leak. En bloc bilateral latissimus dorsi and gluteus myocutaneous flap advancement are good choices but place the wound closure scar directly over the defect.13 Bilobed flaps of skin and subcutaneous tissue avoid this problem.14 Smaller defects can be simply closed by direct soft-tissue mobilization and advancement.
ABDOMINAL WALL RECONSTRUCTION
Complex abdominal wall defects result from tumor resection, trauma, radiation injury, failed ventral hernioplasties, or following the open technique to prevent abdominal compartment syndrome (Fig. 3). These wounds can be complicated by the presence of infected prosthetic mesh, enteral fistulas (Fig. 4), colostomies, or protruding bowel, with the loss of abdominal domain. Partial losses of abdominal layers, and small and lateral defects are easier to reconstruct than large, midline, full-thickness losses. (See Video 1, which contains case studies that demonstrate principles of chest and abdominal wall reconstruction, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A373.)
Fig. 4. Central abdominal defect with multiple enterocutaneous fistulas after wound dehiscence.
Goals of Treatment Wound closure needs to provide durable and stable protection of the viscera and prevention of recurrent herniation, using the fewest procedures possible, to decrease morbidity.15 Preoperative Assessment Assessment and optimization of comorbidities such as diabetes, smoking, and cardiovascular and nutritional problems is routinely performed. Computed tomographic scans will help to accurately assess the extent of myofascial loss, location of the rectus muscles, and intraabdominal abscesses. Pulmonary function tests are indicated when there is a history of chronic obstructive pulmonary disease and for reducing huge ventral hernias. Surgery There are several algorithms available with which to classify and provide direction as to the best approach to these difficult problems.15,16 Preoperative evaluation will define the size, location, and nature of the defects and other considerations such as fistulas or continued intraabdominal sepsis or bleeding. Immediate reconstruction is deferred until the intraabdominal catastrophe is resolved. Soft-tissue cover is usually not an issue, but relative or absolute fascial deficits need to be addressed correctly. Partial Defects Defects with just loss of skin and subcutaneous fat with intact myofascial integrity can be closed either by local tissue mobilization and advancement, or with skin grafts. Small fascial defects alone can be reconstructed with prosthetic mesh, fascia lata, or
Fig. 3. Delayed skin grafting over the bowel following abdominal compartment syndrome with loss of domain and lateral retraction of the abdominal musculature.
204e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
human acellular dermal matrix, placed in the preperitoneal layer whenever this is possible, as an inlay. Midline abdominal defects that cannot be closed by direct approximation with minimal tension may warrant component separation17 with or without the addition of a mesh or bioprosthetic to accomplish the closure.18,19 Release up to 18 cm can be obtained using this technique (at the level of the umbilicus). Bioprosthetic materials such as human acellular dermal matrix have distinct advantages over synthetic mesh in abdominal wall reconstruction. These materials are readily available and do not create donorsite concerns. Human acellular dermal matrix can be used successfully in contaminated wounds, as it heals by regeneration and is ultimately replaced with native tissue.4 There are also fewer adhesions to underlying bowel.20 Exposure of human acellular dermal matrix because of loss of soft-tissue cover does not necessitate removal. Human acellular dermal matrix is expensive and has a tendency to stretch over time.21,22 Other bioprosthetic materials are available in larger sizes,23 but long-term outcome studies delineating their role in complex abdominal reconstruction are not available. (See Video 1, which contains case studies that demonstrate principles of chest and abdominal wall reconstruction, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http:// links.lww.com/PRS/A373.) Full-Thickness Defects The principles of fascial closure are similar to those indicated above. Frequently, the integument can be closed by soft-tissue elevation and advancement. Absolute loss of soft tissue may preclude this type of closure, and additional tissue flaps are indicated.24 26 The tensor fasciae latae myocutaneous flap and the rectus femoris are useful for closing defects in the lower abdomen. The latissimus is useful for upper lateral defects. Occasionally, free flaps such as anterolateral thigh flaps are used for large defects where regional flaps, because of their limited size and arc of rotation, are inadequate. The laparotomy wound that is deliberately left open for repeated debridements or prevention of compartment syndrome is a special challenge. Bowel edema, continued sepsis, and lateral abdominal wall retraction prevent easy fascial closure. Temporary use of a negative-pressure wound therapy device over a polyethylene sheet that wraps around the viscera allows for control of sepsis and prevention of adhesions between bowel and the inner surface of the abdominal wall.27 The device keeps medial tension on the edges of the abdominal defect and gives better control of enteral fistulas. At the time of definitive wound closure, this lack of lateral retraction allows easier component separation and secure abdominal fascial closure. Complications Postoperative complications are common, especially after massive repairs. Wound dehiscence, enterocutaneous fistula, and recurrent ventral hernia are dreaded problems. Aggressive wound debridement and control of fistulas and sepsis are the first steps in managing the patient. Except in unusual cases, the infected prosthetic mesh is removed. Rupture of the wound repair is commonly caused by excessive tension. Malnutrition, sepsis, uncontrolled diabetes, and smoking contribute to poor wound healing and need to be addressed before secondary reconstruction is attempted. Seromas are common following the use of bioprosthetic materials. Repeated aspiration or ultrasound-guided drainage may be necessary.
PRESSURE SORE RECONSTRUCTION
Pressure Ulcer Management Plastic surgeons in training or in practice may deal with pressure ulcers on a frequent basis. This article discusses current knowledge concerning pressure ulcers from the point of view of cause, pathology, preoperative patient selection, preparation for surgery, and postoperative management. Pressure ulcer development is devastating to the patient, the health care provider, and society. Pressure ulcers can develop in the insensate and sensate patient when certain factors coexist. Here, we cover important issues of which every plastic surgeon should be aware concerning pressure ulcers. Medicolegal and reimbursement issues from the health insurance providers to the surgeon and hospital are common, and therefore detailed documentation is essential. Details of operative surgery can be found in textbooks of plastic surgery and the accompanying video. The plastic surgeon should be the leader of the team responsible for the management of the pressure ulcer. Goals for Treatment and Advantages and Disadvantages of the Methods Advantages of early aggressive wound treatment include reduced spread of infection, improved quality of life, and decreased mortality rates. In patients who develop pressure ulcers following acute injury or illness, it is strongly recom-
205e
Plastic and Reconstructive Surgery September 2011
mended that surgical intervention be performed before the start of the rehabilitation program. Proper wound closure will allow for the patient to participate more actively in rehabilitation without the burden of constant wound care and will help restore quality of life. Despite the benefits of muscle flap closure of pressure ulcers, for some patients, surgery may not be an option because they are medically compromised. For the nonsurgical candidate with a stage IV pressure ulcer, standard wound treatment options include use of air fluidized pressure-relieving beds, nutritional support, control of bacterial wound colonization through use of antibiotics, and local wound care. Given all of these conservative measures, it is often observed in clinical practice that stage IV pressure ulcers do not heal properly. If wound healing does take place, it usually requires more than 8 weeks to occur and results in an unstable scar highly vulnerable to wound recurrence. Flap surgery provides excellent quality of soft-tissue coverage to the underlying defect and bone and offers long-term durability to the affected area. Preoperative and Postoperative Management Pressure ulcer surgery is elective, but a patient that acquires a pressure ulcer always has medical problems that need to be optimized preoperatively. General laboratory tests are important, especially if there is infection or anemia. Prealbumin, albumin, and radiographs of the pelvis and hips are very important and may uncover pathologic conditions such as scoliosis, hip joint dislocation, fracture or subluxation, and heterotopic ossification. Magnetic resonance imaging scans are indicated for suspected osteomyelitis. Bone scans are not very helpful in pressure sores, as they are all positive. All abnormal laboratory test results should be corrected before surgery. Deep wound culture and sensitivity should be performed before surgery, and appropriate preoperative antibiotic coverage is started at least 1 day before surgery and continued postoperatively, depending on the severity of the ulcer. If results of deep bone culture and sensitivity and histopathology are positive for acute osteomyelitis, antibiotics are administered for 4 to 6 weeks after flap surgery.28 Muscle spasms should be dealt with before surgery, as they interfere with flap healing, resulting in wound dehiscence, seroma, or bursa formation. Common medications for spasms are baclofen, diazepam, and dantrolene. Phenol nerve injections or botulinum toxin may also be used effectively. Bowel diversion by colostomy before flap surgery may be indicated if the ulcer or multiple ulcers are in close proximity to the anus or less than 6 cm from the ulcer excision margin. When an ulcer involves the perineal urethra in men, temporary or permanent urinary diversion should be performed. A patient with spinal cord injury may manifest psychosocial conditions, and a psychosocial evaluation and treatment of any abnormality should be considered preoperatively. Rehabilitation after surgery consists of physical therapy and occupational therapy and addresses the long period of immobilization of patients. The type of rehabilitation program depends on the primary diagnosis. The sitting program is performed in a gradual fashion after flap surgery, as it is very important to build skin tolerance to pressure along with improved tensile strength of the wound. Our sitting program29 starts at 6 weeks after flap surgery with 30 minutes on the first day, and increasing by 30 minutes each subsequent day. When the sitting program reaches 6 hours per day, the patient can be discharged to home, provided that there is no skin breakdown. This protocol can be modified according to (1) the primary patient diagnosis, (2) the type and healing of the flap, (3) the extent of the operation, and (4) the appearance of the wound clinically. The sitting program may start at 4 or 5 weeks after surgery when wound healing is uncomplicated and the tensile strength of the wound is approximately 40 to 50 percent of normal. At 6 weeks after flap surgery, the tensile strength is approximately 80 to 90 percent of normal.30,31 Basic Surgical Procedure for the Ulcer The unhealthy skin edge of the ulcer is marked for excision, Methylene blue dye is used to color all the undermining and ulcer extension and helps to visually confirm complete ulcer excision. After excision of the ulcer, the prominent underlying bone is shaved to the healthy bleeding level. If osteomyelitis is suspected, a biopsy specimen from the deep bone should be sent for histopathologic evaluation and culture and sensitivity to establish diagnosis of osteomyelitis.28 Then, an available flap is designed according to the anatomical area of the ulcer for reconstruction of the defect.
SACRAL COCCYGEAL ULCER
Flap Selection and Choice The main flap used is the gluteus maximus muscle. It can be designed as a rotation flap,32,33 advancement island flap,34 42 or split flap.43 The choice depends on the size of the ulcer and
206e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
whether the ulcer is primary. A first-time ulcer may need a simple flap, whereas a recurrent ulcer usually requires a large and complex flap. In an ambulatory patient, complete detachment of the gluteus maximus inferiorly should be avoided to prevent a functional deficit, and the muscle is used only after exhausting other options. The other gluteus muscles (medius and minimus) will compensate for the function of the used gluteus maximus muscle, and this can be identified by muscle testing. Fasciocutaneous flaps such as the superior gluteal artery perforator flap are useful especially in the ambulatory patient. Gluteus Maximus as a Myocutaneous Rotation Flap Advantages of the gluteus maximus as a myocutaneous rotation flap include the fact that it is good for covering large defects in nonambulatory patients32,33 (Fig. 5). Disadvantages include extensive dissection, blood loss, and the part of the flap that covers the defect is fasciocutaneous. This flap is not indicated in ambulatory patients. In a recurrent or larger size ulcer, a bilateral gluteus maximus muscle is used to cover the defect. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http:// links.lww.com/PRS/A374.) Gluteus Maximus Sliding Island Flap Advantages of the gluteus maximus sliding island flap include the fact that it is excellent for small and medium defects. Also, it involves less extensive dissection and less blood loss and is ideal for ambulatory, sensory patients. The muscle bulk will cover exposed bone34 41 (Fig. 6). Disadvantages are that in larger defect it requires a bilateral flap. (See Video 2, which dem-
Video 2. Video 2, which demonstrates comprehensive management of pressure ulcers, is available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.
Fig. 6. The design for the gluteus maximus sliding island flap.
Fig. 5. The design for the gluteus maximus rotation flap.
onstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) Gluteus Maximus Splitting Flap Advantages of the gluteus maximus splitting flap are that it is a good flap for coccygeal ulcer, has less dissection and less blood loss, has the muscular bulk to cover the coccygeal bone, and is a good flap for the ambulatory patient43 (Fig. 7). The disadvantage is that it is not suitable for a larger defect. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.)
207e
Plastic and Reconstructive Surgery September 2011
using a vascular Doppler over a triangular area between the iliac crest, the greater trochanter, and posterior superior iliac spine. The flap can be advanced at least 2 to 3 cm in any direction to close sacral or lumbar ulcers. Advantages include the fact that it is useful for closing small defects and is indicated in ambulatory patients. Disadvantages are that the flap requires meticulous dissection and cannot be revised in cases of wound complications or recurrent ulceration. Recurrent Extensive Sacral Ulceration. When the gluteus maximus has been previously used and cannot be mobilized or readvanced, the following surgical options are used:
Fig. 7. The design for the gluteus maximus splitting flap.
Superior Gluteal Artery Perforator Flap This fasciocutaneous flap has excellent vascularity and is usually used for microsurgical breast reconstruction.44 It is also described as a flap for sacral and lumbar defects.45 47 The axis of the skin paddle can be placed in many directions to cover the adjacent defect. The perforators are located by
Distant fasciocutaneous flap. Posterior thigh flap or extended tensor fasciae latae flap. Vastus lateralis muscle transfer. It can be tunneled under the skin to the defect, and the muscle surface is covered with skin graft (Fig. 8). Otherwise, an island of skin may be carried with the muscle and tunneled to the defect. Disarticulation and total thigh flap. With complete loss of both gluteus maximus muscles and ex-
Fig. 8. Surgical photographs showing the use of vastus lateralis muscle tunneled to the sacral area.
208e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
posure of the entire sacral bone and pelvic floor, there may be no other flap option available. This is an end-stage procedure. This is seen typically in insensate and nonambulatory patients. can be under tension even with the back cut when it is rotated medially, and this may lead to skin breakdown in the postoperative period. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) V-Y Hamstring Muscle Advancement Flap The vascularity of the skin island of this myocutaneous flap is based on the hamstring muscle perforators. This flap can be used for recurrent ischial ulceration or primary ulcer. Advantages of this flap are that it requires less dissection and entails less blood loss than other options, it can be revised for recurrent ulceration, and it is quite robust49 52 (Fig. 10). Disadvantages are that it is not indicated in ambulatory patients, as transection of the hamstring tendons distally will leave a functional deficit. The proximal part of the flap is fasciocutaneous, and the gracilis muscle is used to fill the defect. If the gracilis muscle is not available, deepithelialization of the proximal part of the ham-
ISCHIAL ULCER
This ulcer is common in the insensate spinal injury patient. The main cause is prolonged sitting without pressure relief or without a proper wheelchair cushion. Gluteus Maximus Myocutaneous Rotation Flap The gluteus maximus myocutaneous rotation flap is one flap used to close the ulcer48 (Fig. 9). An advantage of this flap is that it is indicated when the ulcer is undermined. On occasions, this flap alone is sufficient to cover the defect, but deeper wounds may need another layer of muscle to cover the bone in addition to the gluteus maximus as a final cover. This flap can be revised and readvanced with recurrent ulceration. A disadvantage is that it is not indicated in an ambulatory patient because of the functional deficit. Occasionally, the gluteus maximus flap
Fig. 9. The design for the gluteus maximus flap for ischial ulcers.
209e
Plastic and Reconstructive Surgery September 2011
Fig. 10. The design for the hamstring muscle advancement flap for ischial ulcers.
string flap is performed and advanced into the defect. If the ulcer is too proximal in the gluteal area, this flap cannot be advanced to cover the defect without tension. Combined Flaps of Gracilis Muscle Transfer to Cover the Ischium and the Medial Thigh Rotation Fasciocutaneous Flap We prefer a combination of these flaps as a first choice for ambulatory patients and in recurrent ulcerations where other options have been used before5356 (Fig. 11). A disadvantage is that it is difficult to reuse or revise this flap. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) Tunneled Gracilis Muscle Transfer to Cover the Ischium with Direct Closure of the Skin and Subcutaneous Layer over the Muscle Advantages are that it involves less dissection, is ideal for the ambulatory patient, and reserves the other flaps for future use in patients with spinal cord injury. Also, it is an ideal option for smaller ulcers. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) Inferior Gluteal Artery Perforator Flap This is a fasciocutaneous flap has a skin paddle island over the gluteal crease and lateral to the ischium. The flap was described for free tissue breast reconstruction but can be used to close
Fig. 11. Surgical photographs showing the use of the gracilis muscle and medial thigh rotation fasciocutaneous flap to close an ischial ulcer.
ischial or perineal ulcers. The vascularity of this flap is based on the branches from the inferior gluteal artery and vein. The flap can be advanced medially to close an ischial defect.57
210e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
An advantage is that it is a small flap, ideal for mobile patients, as it leaves no functional deficit. Disadvantages are that it is difficult to revise or reuse this flap in recurrent ulceration and it does need meticulous dissection to isolate the perforators. Posterior Thigh Fasciocutaneous Flap as a Rotation Flap This flap is available if there is no prior ulceration or scarring in the posterior thigh with deep and extensive ulceration; the posterior thigh fasciocutaneous flap may not be sufficient to eliminate the dead space58 (Fig. 12). The gracilis muscle is transferred under the proximal fasciocutaneous part of the flap to cover the bone, and the posterior thigh fasciocutaneous flap is rotated to close the skin defect. Extensive Recurrent Ischioperineal Ulcer Seen in Patients with Spinal Cord Injury As a last option, the vastus lateralis muscle may be used as a transposition flap from the vertical anatomical position to a horizontal position to cover the defect. The vastus lateralis is an excellent muscle because of its size and blood supply. It can cover bilateral ischial defects. The surface of the muscle can be covered by skin graft or a fasciocutaneous flap such as the extended tensor fasciae latae flap. associated with extension into the anatomical trochanteric bursa. Extension into the hip joint can cause infection and destruction of this joint. Options for Repair The most common flap used to close the ulcer is the tensor fasciae latae,59 63 which is used in both ambulatory and nonambulatory patients without any significant functional deficit. Tensor Fasciae Latae as a V-Y Advancement Flap The indication for the use of this flap is for ulcers that are small to medium in size and located over the greater trochanter62,63 (Fig. 13). The flap can be revised and advanced in the event of recurrent ulceration. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) Tensor Fasciae Latae as a Rotation Flap The use of tensor fasciae latae in this form is indicated for larger ulcers and when the greater trochanter is rotated posteriorly, secondary to hip subluxation. This posterior trochanteric ulcer is seen frequently in patients with spinal cord injury and severe muscle spasticity. Anterior Lateral Thigh Flap This flap is perfused by descending branches of the lateral circumflex femoral artery. It is an island flap but can be used as a rotation flap to close small trochanteric ulcers. Distal Gluteus Maximus Myocutaneous Rotation Flap This flap may be used when the trochanteric ulcer is small and posteriorly rotated. Rectus Femoris Muscle Flap This muscle has application for a deep extensive trochanteric ulcer with wide exposure of the greater trochanter. This muscle is used as the first layer of repair over the bone and is then covered by the tensor fasciae latae flap in any form (e.g., rotation or V-Y). Hip Joint Infection The hip joint is vulnerable to secondary infection when ulceration is close to the joint and may result in joint destruction. The most common ulcers that can cause septic arthritis are trochanteric and ischial ulcers. Hematogenous hip infection is rare. The principles of management of septic hip arthritis are through debridement and wound closure with healthy tissues.
TROCHANTERIC ULCER
This ulcer is less common than ischial and sacral ulcers. It can develop in insensate and sensate patients because of direct pressure from a prominent greater trochanter. Skin ulceration is
Fig. 12. The design of the posterior thigh fasciocutaneous flap to close an ischial ulcer.
211e
Plastic and Reconstructive Surgery September 2011
Fig. 13. The design of the tensor fasciae latae flap in V-Y fashion and rotation to close a trochanteric ulcer.
The first step is the Girdlestone procedure64 68 and debridement of all of the infected bone and heterotopic calcification. In the next step, the defect is closed with a muscle flap.65 68 The common muscle used is the vastus lateralis muscle (Fig. 14)
with direct skin closure over muscle. In a large wound, a tensor fasciae latae flap is designed as a rotation flap to close the defect over the vastus lateralis muscle. Both procedures can be performed in one stage or two stages, depending on the severity of the infection. If the hip cavity after debridement is small, the rectus femoris can be used to fill the defect, preserving the vastus lateralis muscle for future use in the patient with spinal cord injury. (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) End-Stage Disease Sometimes, a patient presents with extensive recurrent ulceration around the pelvis and a history of bilateral Girdlestone procedures and multiple flaps having been performed previously; also, the patient may have a urinary diversion and colostomy. The only option available is disarticulation and a total thigh flap.69 72 The amputation level is either above or below the knee
Fig. 14. Surgical photograph showing the use of a vastus lateralis muscle flap to fill a hip defect following the Girdlestone procedure.
212e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
Fig. 15. Surgical photographs showing disarticulation and removal of the entire femur and amputation at the knee level to use the total thigh flap for coverage of extensive ulceration.
to use the calf muscles to cover the sacral ulcer (Fig. 15). (See Video 2, which demonstrates comprehensive management of pressure ulcers, available in the Related Videos section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/A374.) Closure of Multiple Ulcers by Multiple Flaps as a Single-Stage Procedure It is very common to see multiple ulceration in patients with spinal cord injury. We recommend closing these ulcers as a one-stage procedure.7274 It has the advantages of removing all septic foci and expedient wound closure, improving the health and quality of life of the patient. The disadvantages are the need for an operating team, significant blood loss, and increased anesthesia and operative time. Complications The predisposing factors are the premorbid medical conditions of patient age, primary diagnosis, flap selection, preexisting skin condition, and the available reserve of muscles. Common complications are wound dehiscence, skin necrosis and hematoma under the flap, seroma, and bursa formation. The initial management is local wound care and debridement of necrotic tissue and negative-pressure wound therapy. If the wound shows no healing with all of these local measures, a flap revision or new flap is performed.
Closing a wound, especially in a functional part of the body, is very rewarding, as it improves the patients quality of life. Unfortunately, in the insensate group of patients, the phenomenon of recurrent ulceration places the reconstructive surgeon in a moral and ethical dilemma as to how long to continue with repeated surgery. Education of all health care providers on prevention of pressure ulcers in a hospital or nursing home environment is important and is mandated and legislated by federal and state laws. Collaboration between health care providers and at-risk patients in preventive measures is warranted to reduce the chances of developing this unfortunate problem in the first place.
Salah Rubayi, M.D. Rancho Los Amigos National Rehabilitation Center 7601 East Imperial Highway Downey, Calif. 90242 srubayi@dhs.lacounty.gov
REFERENCES
1. Arnold PG, Pairolero PC. Chest wall reconstructions: An account of 500 consecutive cases. Plast Reconstr Surg. 1996; 98:804810. 2. Losken A, Thourani VH, Carlson GW, et al. A reconstructive algorithm for plastic surgery following extensive chest wall resection. Br J Plast Surg. 2004;57:295302. 3. Chang RR, Mehrara BJ, Hu Q, Disa JJ, Cordeiro PG. Reconstruction of complex oncologic chest wall defects: A 10 year experience. Ann Plast Surg. 2004;52:471479; discussion 479.
213e
Plastic and Reconstructive Surgery September 2011
4. Butler CE, Langstein HN, Kronowitz SJ. Pelvic, abdominal and chest wall reconstruction with AlloDerm in patients with increased risk for mesh related complications. Plast Reconstr Surg. 2005;116:12631275; discussion 12761277. 5. Michaels BM, Orgill DP, Decamp MM, Pribaz JJ, Eriksson E, Swanson S. Flap closure of postpneumonectomy empyema. Plast Reconstr Surg. 1997;99:437442. 6. Hultman CS, Culbertson JH, Jones JE, et al. Thoracic reconstruction with the omentum: Indications, complications and results. Ann Plast Surg. 2001;46:242249. 7. Ferron G, Garrido I, Martel P, et al. Combined laparoscopically harvested omental flap with meshed skin graft and vacuum assisted closure for reconstruction of complex chest wall defects. Ann Plast Surg. 2007;58:150155. 8. Pairolero PC, Arnold PG, Harris JB. Long term results of pectoralis major muscle transposition for infected sternotomy wounds. Ann Surg. 1991;213:583589; discussion 589 590. 9. Eifert S, Kronschnabl S, Kaczmarek I, Reichart B, Vicol C. Omental flap for recurrent deep sternal wound infection and mediastinitis after cardiac surgery. Thorac Cardiovasc Surg. 2007;55:371374. 10. Snel BJ, Spronk CA, Werker PM, van der Lei B. Pectus excavatum reconstruction with silicone implants: Long-term results and a review of the English language literature. Ann Plast Surg. 2009;62:205209. 11. Fonkalsrud EW. 912 open pectus excavatum repairs: Changing trends, lessons learned. One surgeons experience. World J Surg. 2009;33:180190. 12. Fonkalsrud EW. Current management of pectus excavatum. World J Surg. 2003;27:502508. 13. Ramasastry SS, Cohen M. Soft tissue closure and plastic surgery aspects of large open meningomyeloceles. Neurosurg Clin North Am. 1995;6:279291. 14. Lapid O, Rosenberg L, Cohen A. Meningomyelocele reconstruction with bilobed flaps. Br J Plast Surg. 2001;54:570572. 15. Lowe JB III. Updated algorithm for abdominal wall reconstruction. Clin Plast Surg. 2006;33:225240. 16. Rodriguez ED, Bluebond-Langner R, Silverman RP, et al. Abdominal wall reconstruction following severe loss of domain: The R Adams Cowley Shock Trauma Center algorithm. Plast Reconstr Surg. 2007;120:669680. 17. Ramirez OM, Ruas E, Dellon A. Component separation method for closure of abdominal wall defects: An anatomical and clinical study. Plast Reconstr Surg. 1990;86:519526. 18. Buinewicz B, Rosen B. Acellular cadaveric dermis (AlloDerm): A new alternative for abdominal hernia repair. Ann Plast Surg. 2004;52:188194. 19. Kolker AR, Brown DJ, Redstone JS, Scarpinato VM, Wallack MK. Multilayer reconstruction of abdominal wall defects with acellular dermal allograft (AlloDerm) and component separation. Ann Plast Surg. 2005;55:3641; discussion 4142. 20. Butler CE, Prieto VG. Reduction of adhesions with composite AlloDerm/polypropylene mesh implants for abdominal wall reconstruction. Plast Reconstr Surg. 2004;114:464473. 21. Bluebond-Langner R, Keifa ES, Mithani S, Bochicchio GV, Scalea T, Rodriguez ED. Recurrent abdominal laxity following interpositional human acellular dermal matrix. Ann Plast Surg. 2008;60:7680. 22. deMoya MA, Dunham N, Inaba K, et al. Long term outcome of acellular dermal matrix when used for large traumatic open abdomen. J Trauma 2008;65:349353. 23. Pomahac B, Aflaki P. Use of noncrosslinked porcine dermal scaffold in abdominal wall reconstruction. Am J Surg. 2010; 199:2227. 24. Gruen RL, Morrison WA, Vellar ID. The tensor fasciae latae myocutaneous flap closure of major chest and abdominal wall defects. Aust N Z J Surg . 1998;68:666669. 25. Brown DM, Sicard GA, Flye MW, Khouri RK. Closure of complex abdominal wall defects with bilateral rectus femoris flaps with fascial extensions. Surgery 1993;114:112116. 26. Wong CH, Lin CH, Fu B, Fang JF. Reconstruction of complex abdominal wall defects with free flaps: Indications and clinical outcomes. Plast Reconstr Surg. 2009:124:500509. 27. DeFranzo AJ, Pitzer K, Molnar JA, et al. Vacuum assisted closure for defects of the abdominal wall. Plast Reconstr Surg. 2008;121:832839. 28. Marriott R, Rubayi S. Successful truncated osteomyelitis treatment for chronic osteomyelitis secondary to pressure ulcers in spinal cord injury patients. Ann Plast Surg. 2008; 61:425429. 29. Rubayi S, Cousins S, Valentine WA. Myocutaneous flaps: Surgical treatment of severe pressure ulcers. AORN J. 1990; 52:4047, 50, 5255. 30. Madden JW, Peackock EE Jr. Studies on the biology of collagen during wound healing: I. Rate of collagen synthesis and deposition in cutaneous wounds of the rat. Surgery 1968;64: 288294. 31. Levenson SM, Geever EF, Crowley LV, Oates JF III, Berard CW, Rosen H. The healing of rat skin wounds. Ann Surg. 1965;161:293308. 32. Parkash S, Banerjee S. The total gluteus maximus rotation and other gluteus maximus musculocutaneous flaps in the treatment of pressure ulcers. Br J Plast Surg. 1986;39:6671. 33. Ramirez OM, Hurvitz DJ, Futrell JW. The expansive gluteus maximus flap. Plast Reconstr Surg. 1984;74:757770. 34. Ramirez OM, Orlando JC, Hurvitz DJ. The sliding gluteus maximus myocutaneous flap: Its relevance in ambulatory patients. Plast Reconstr Surg. 1984;74:6875. 35. Maruyama Y, Nakajima H, Wada M, Imai T, Fujino T. A gluteus maximus myocutaneous island flap for the repair of a sacral decubitus ulcer. Br J Plast Surg. 1980;33:150155. 36. Rees RS, Reilley AF, Nanney LB, Lynch JB. Sacral pressure sores: Treatment with island gluteus maximus musculocutaneous flaps. South Med J. 1985;78:11471151. 37. Scheflan M, Nahai F, Bostwick J III. Gluteus maximus island musculocutaneous flap for closure of sacral and ischial ulcers. Plast Reconstr Surg. 1981;68:533538. 38. Stevenson TR, Pollack RA, Rohrich RJ, VanderKolk CA. The gluteus maximus musculocutaneous island flap: Refinements in design and application. Plast Reconstr Surg. 1987; 79:761768. 39. Ramirez OM, Swartz WM, Futrell JW. The gluteus maximus muscle: Experimental and clinical considerations relevant to reconstruction in ambulatory patients. Br J Plast Surg. 1987; 40:110. 40. Heywood AJ, Quaba AA. Modified gluteus maximus V-Y advancement flaps. Br J Plast Surg. 1989;42:263265. 41. Park C, Park BY. Fasciocutaneous V-Y advancement flap for repair of sacral defects. Ann Plast Surg. 1988;21:2326. 42. Parry SW, Mathes SJ. Bilateral gluteus maximus myocutaneous advancement flaps: Sacral coverage for ambulatory patients. Ann Plast Surg. 1982;8:443445. 43. Rubayi S, Doyle BS. The gluteus maximus muscle splitting myocutaneous flap for treatment of sacral and coccygeal pressure ulcer. Plast Reconstr Surg. 1995;96:13661371. 44. Allen RJ, Tucker C Jr. Superior gluteal artery perforator free flap for breast reconstruction. Plast Reconstr Surg. 1995;95: 12071212. 45. Verpaele AM, Blondeel PN, Van Landuyt K, et al. The superior gluteal artery perforator flap: An additional tool in the
214e
Volume 128, Number 3 Torso and Pressure Sore Reconstruction
treatment of sacral pressure sores. Br J Plast Surg. 1999;52: 385391. Koshima I, Moriguchi T, Soeda S, Kawada S, Ohta S, Ikeda A. The gluteal perforator-based flap for repair of sacral pressure sores. Plast Reconstr Surg. 1993;91:678683. Ao M, Mae O, Namba Y, Asagoe K. Perforator-based flap for coverage of lumbosacral defects. Plast Reconstr Surg. 1998; 101:987991. Mills RL. Gluteus maximus musculocutaneous flap. In: Strauch B, Vasconez LO, Hall-Findlay EJ, eds. Grabbs Encyclopedia of Flaps. Vol. 3. Boston: Little, Brown; 1990:16871688. Baker DC, Barton FE Jr, Converse JM. A combined biceps and semitendinosus muscle flap in the repair of ischial sores. Br J Plast Surg. 1978;31:2628. Conway H, Griffith BH. Plastic surgery for closure of decubitus patients with paraplegia: Based on experience with 1,000 cases. Am J Surg. 1956;91:946975. James JH, Moir IH. The biceps femoris musculocutaneous flap in the repair of pressure sores around the hip. Plast Reconstr Surg. 1980;66:736739. Tobin GR, Sanders BP, Mann D, Weiner LJ. The biceps femoris myocutaneous advancement flap: A useful modification for ischial pressure ulcer reconstruction. Am Plast Surg. 1981;6:396401. Mathes SJ, Nahai F, eds. A systematic approach to flap selection. In: Clinical Applications for Muscle and Musculocutaneous Flaps. St. Louis: Mosby; 1982:438439. Wingate GB, Friedland JA. Repair of ischial pressure ulcers with gracilis myocutaneous island flaps. Plast Reconstr Surg. 1978;62:245248. Labandter HP. The gracilis muscle flap and musculocutaneous flap in the repair of perineal and ischial defects. Br J Plast Surg. 1980;33:9598. Homma K, Murakami G, Fujioka H, Fujita T, Imai A, Ezoe K. Treatment of ischial pressure ulcers with a posteromedial thigh fasciocutaneous flap. Plast Reconstr Surg. 2001;108: 19901996; discussion 1997. Rosen JM, Mo ST, Lui A. Experience with the island inferior gluteal thigh flap compared with other local flaps for the reconstruction of the pelvic area. Ann Plast Surg. 1990;24: 498509. Hurwitz DJ, Swartz WM, Mathes SJ. The gluteal thigh flap: A reliable sensate flap for the closure of buttock and perineal wounds. Plast Reconstr Surg. 1981;68:521532. 59. Nahai F, Silverton JS, Hill HL, Vasconez LO. The tensor fascia lata musculocutaneous flap. Ann Plast Surg. 1978;1: 372379. 60. Nahai F, Hill HL, Hester TR. Experiences with tensor fasciae latae flap. Plast Reconstr Surg. 1979;63:788799. 61. Nahai F. The tensor fasciae latae flap. Clin Plast Surg. 1980; 7:5156. 62. Lewis VL Jr, Cunningham BL, Hugo NE. The tensor fasciae latae V-Y retroposition flap. Ann Plast Surg. 1981;6:3437. 63. Siddiqui A, Wiedrich T, Lewis VL Jr. Tensor fasciae latae V-Y retroposition myocutaneous flap: Clinical experience. Ann Plast Surg. 1993;31:313317. 64. The classic. Acute pyogenic arthritis of the hip: An operation giving free access and effective drainage. G. R. Girdlestone, 1943. Clin Orthop Relat Res. 1982;170:37. 65. Arnold PG, Witzke DJ. Management of failed total hip arthroplasty with muscle flaps. Ann Plast Surg. 1983;11: 474478. 66. Eltorai I. The Girdlestone procedure in spinal cord injury patients: A ten-year old experience. J Am Paraplegia Soc. 1983; 6:8586. 67. Klein NE, Luster S, Green S, Moore T, Capen D. Closure of defects from pressure sores requiring proximal femoral resection. Ann Plast Surg. 1988;21:246250. 68. Rubayi S, Pompan D, Garland D. Proximal femoral resection and myocutaneous flap for treatment of pressure ulcers in spinal injury patients. Ann Plast Surg. 1991;27:132138. 69. Georgiade N, Pickrell K, Maguire C. Total thigh flaps for extensive decubitus ulcers. Plast Reconstr Surg (1946) 1956; 17:220225. 70. Berkas EM, Chesler MD, Sako Y. Multiple decubitus ulcer treatment by hip disarticulation and soft-tissue flaps from the lower limbs. Plast Reconstr Surg. 1961;27:618619. 71. Capen DA, Nelson RW, Zigler J, et al. Staged total thigh rotation flap for coverage of chronic recurrent pressure sores. Contemp Orthop. 1988;16:2330. 72. Tizian C, Brenner P, Berger A. The one-stage surgical treatment of multilocated pressure sores using various myocutaneous island flaps. Scand J Plast Reconstr Surg Hand Surg. 1988;22:8387. 73. Lari AR, Rajacic N. One-stage repair of multiple bed sores. Br J Plast Surg. 1992;45:540543. 74. Rubayi S, Burnett CC. The efficacy of single-stage surgical management of multiple pressure sores in spinal cord-injured patients. Ann Plast Surg. 1999;42:533539.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
215e
Das könnte Ihnen auch gefallen
- The Guide to Breast Reconstruction: Step-By-Step from Mastectomy Through ReconstructionVon EverandThe Guide to Breast Reconstruction: Step-By-Step from Mastectomy Through ReconstructionBewertung: 4 von 5 Sternen4/5 (1)
- Atlas of Gastrointestinal Endoscopy and Related PathologyDokument2 SeitenAtlas of Gastrointestinal Endoscopy and Related PathologyMaria PatituNoch keine Bewertungen
- Postcholecystectomy SyndromeDokument27 SeitenPostcholecystectomy SyndromeMonica TurnerNoch keine Bewertungen
- Conservative Management of Perforated Peptic UlcerDokument4 SeitenConservative Management of Perforated Peptic UlcerAfiani JannahNoch keine Bewertungen
- Surgical Management of ObesityDokument13 SeitenSurgical Management of Obesityمحمد حميدانNoch keine Bewertungen
- Simple MastectomyDokument3 SeitenSimple MastectomyCindy DayocNoch keine Bewertungen
- Management of Anastomotic Complications of Colorectal SurgeryDokument13 SeitenManagement of Anastomotic Complications of Colorectal Surgerydadupipa100% (1)
- Phyllodes Tumors of The Breast UpToDateDokument22 SeitenPhyllodes Tumors of The Breast UpToDateSean SialanaNoch keine Bewertungen
- Causes of Upper Gastrointestinal Bleeding in Adults - UpToDateDokument37 SeitenCauses of Upper Gastrointestinal Bleeding in Adults - UpToDateAline MoraisNoch keine Bewertungen
- Management of Acute Appendicitis in Adults - UpToDateDokument28 SeitenManagement of Acute Appendicitis in Adults - UpToDateaulia rachman100% (1)
- Abdominal Wall IncisionDokument42 SeitenAbdominal Wall IncisionURo KkuNoch keine Bewertungen
- Surgical Safety ChecklistDokument2 SeitenSurgical Safety ChecklistLian CatindigNoch keine Bewertungen
- Perioperative Management of Patients Receiving Anticoagulants - UpToDateDokument65 SeitenPerioperative Management of Patients Receiving Anticoagulants - UpToDatejames lxNoch keine Bewertungen
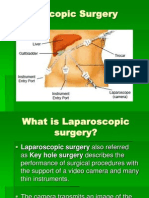
- Laparoscopic SurgeryDokument10 SeitenLaparoscopic Surgerynainacurthberrt50% (2)
- Baltarowich ABD pt1 Hepatobiliary US PDFDokument22 SeitenBaltarowich ABD pt1 Hepatobiliary US PDFEka KusumaningatiNoch keine Bewertungen
- Diagnosis and Acute Management of Suspected Nephrolithiasis in Adults - UpToDateDokument44 SeitenDiagnosis and Acute Management of Suspected Nephrolithiasis in Adults - UpToDateManu Luciano100% (1)
- PreOp Evaluation in CKD Patients Up To DateDokument14 SeitenPreOp Evaluation in CKD Patients Up To DateMaría Fernanda RíosNoch keine Bewertungen
- General SurgeryDokument18 SeitenGeneral SurgeryYogesh KharcheNoch keine Bewertungen
- Principles of Abdominal Wall Closure - UpToDateDokument32 SeitenPrinciples of Abdominal Wall Closure - UpToDatesteve inga pomaNoch keine Bewertungen
- Postoperative Peritoneal Adhesions in Adults and Their Prevention - UpToDateDokument17 SeitenPostoperative Peritoneal Adhesions in Adults and Their Prevention - UpToDateDesak PramestiNoch keine Bewertungen
- Schwartz Hour - BurnDokument62 SeitenSchwartz Hour - BurnM3 SURGERY100% (1)
- Topical Hemostatic Agents in Surgery PDFDokument10 SeitenTopical Hemostatic Agents in Surgery PDFFernanda SouzaNoch keine Bewertungen
- Acute Colonic Diverticulitis: Medical Management - UpToDateDokument20 SeitenAcute Colonic Diverticulitis: Medical Management - UpToDateFelipe Orellana MuñozNoch keine Bewertungen
- Liver Function TestDokument40 SeitenLiver Function TestanojNoch keine Bewertungen
- Antimicrobial Prophylaxis For Prevention of Surgical Site Infection in AdultsDokument59 SeitenAntimicrobial Prophylaxis For Prevention of Surgical Site Infection in Adultsbolohan biatriceNoch keine Bewertungen
- (HLMN 5-19) Evaluation of The Adult With Abdominal Pain - UpToDateDokument21 Seiten(HLMN 5-19) Evaluation of The Adult With Abdominal Pain - UpToDateandylumanNoch keine Bewertungen
- Management of Acute Pancreatitis - UpToDateDokument33 SeitenManagement of Acute Pancreatitis - UpToDateCesar Luna RamirezNoch keine Bewertungen
- Initial Management of Trauma in Adults - UpToDateDokument37 SeitenInitial Management of Trauma in Adults - UpToDateAlberto Kenyo Riofrio PalaciosNoch keine Bewertungen
- Circumcision in Baby BoysDokument6 SeitenCircumcision in Baby BoysJbl2328Noch keine Bewertungen
- Surgical Management of Acute CholecystitisDokument17 SeitenSurgical Management of Acute Cholecystitisgrayburn_1Noch keine Bewertungen
- ComponentsDokument5 SeitenComponentsprakashmathewNoch keine Bewertungen
- Laparoscopic Inguinal and Femoral Hernia Repair in Adults - UpToDateDokument22 SeitenLaparoscopic Inguinal and Femoral Hernia Repair in Adults - UpToDategdi3Noch keine Bewertungen
- Use of Blood Products in The Critically Ill - UpToDateDokument13 SeitenUse of Blood Products in The Critically Ill - UpToDateOscar F RojasNoch keine Bewertungen
- Have Half-Lives in The Range 2 - 6 H. Lovenox Is 4.5 Hours. The Anticoagulant Effect ofDokument37 SeitenHave Half-Lives in The Range 2 - 6 H. Lovenox Is 4.5 Hours. The Anticoagulant Effect ofkellixgNoch keine Bewertungen
- Fibromialgia - UptodateDokument21 SeitenFibromialgia - UptodateaeadaNoch keine Bewertungen
- Gallstones in Pregnancy - UpToDateDokument51 SeitenGallstones in Pregnancy - UpToDateLeira BarbosaNoch keine Bewertungen
- Laparoscopic Abdominoperineal ResectionDokument19 SeitenLaparoscopic Abdominoperineal ResectionJohnson Mallibago100% (2)
- Anorectal Surgery PDFDokument33 SeitenAnorectal Surgery PDFLuminitaDumitriuNoch keine Bewertungen
- Perforated Peptic Ulcer DiseaseDokument2 SeitenPerforated Peptic Ulcer DiseaseRene John FranciscoNoch keine Bewertungen
- Surgical Treatment of Hemorrhoidal Disease - UpToDateDokument27 SeitenSurgical Treatment of Hemorrhoidal Disease - UpToDateJune DoNoch keine Bewertungen
- An Updated Review of Cystic Hepatic LesionsDokument8 SeitenAn Updated Review of Cystic Hepatic LesionsMayerlin CalvacheNoch keine Bewertungen
- Surgery II - Pancreas 2014Dokument20 SeitenSurgery II - Pancreas 2014Medisina101Noch keine Bewertungen
- GERD SchwartzDokument10 SeitenGERD SchwartzMina Tharwat AzerNoch keine Bewertungen
- Bile Duct InjuryDokument62 SeitenBile Duct InjuryShashidhara Puttaraj100% (1)
- Approach To The Adult Patient With Anemia - UpToDateDokument23 SeitenApproach To The Adult Patient With Anemia - UpToDateNicole SierraNoch keine Bewertungen
- Basic Principles of Wound Healing - UpToDateDokument8 SeitenBasic Principles of Wound Healing - UpToDateNguyễn TrangtrangNoch keine Bewertungen
- Perforated Peptic UlcerDokument68 SeitenPerforated Peptic UlcerSaibo BoldsaikhanNoch keine Bewertungen
- Use of Anticoagulants During Pregnancy and Postpartum - UpToDateDokument38 SeitenUse of Anticoagulants During Pregnancy and Postpartum - UpToDateCristinaCaprosNoch keine Bewertungen
- Endoscopic SurgeryDokument152 SeitenEndoscopic SurgeryiciNoch keine Bewertungen
- Laparoscopic AppendectomyDokument1 SeiteLaparoscopic AppendectomyNANDAN RAINoch keine Bewertungen
- Current Trends in Management of CholedocholithiasisDokument35 SeitenCurrent Trends in Management of Choledocholithiasisrajan kumar100% (6)
- Matary Swellings 01Dokument23 SeitenMatary Swellings 01toolsdesk1Noch keine Bewertungen
- Management of The Pancreatic Remnant During Whipple OperationDokument4 SeitenManagement of The Pancreatic Remnant During Whipple OperationYacine Tarik Aizel100% (1)
- Periphral Vascular Disease 2Dokument44 SeitenPeriphral Vascular Disease 2Sohil ElfarNoch keine Bewertungen
- Total GastrectomyDokument12 SeitenTotal GastrectomyDarlene PiperNoch keine Bewertungen
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDokument28 SeitenOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreabctutorNoch keine Bewertungen
- Anal ProblemsDokument35 SeitenAnal ProblemsSandip VaghelaNoch keine Bewertungen
- Development of MesentryDokument28 SeitenDevelopment of MesentryimmmiNoch keine Bewertungen
- Mesh MaterialsDokument21 SeitenMesh MaterialsbogdanotiNoch keine Bewertungen
- NUFLO Low Power Pre-Amplifier: SpecificationsDokument2 SeitenNUFLO Low Power Pre-Amplifier: SpecificationsJorge ParraNoch keine Bewertungen
- (Essential Skills For Nurses Series) Philippa Sully - Joan Dallas-Essential Communication Skills For Nursing and Midwifery-Mosby - Elsevier (2010) PDFDokument250 Seiten(Essential Skills For Nurses Series) Philippa Sully - Joan Dallas-Essential Communication Skills For Nursing and Midwifery-Mosby - Elsevier (2010) PDFRetno SumaraNoch keine Bewertungen
- Handbook - European Choral AssociationDokument24 SeitenHandbook - European Choral AssociationMonica SaenzNoch keine Bewertungen
- Gel Electrophoresis Worksheet Teacher AnswersDokument3 SeitenGel Electrophoresis Worksheet Teacher AnswersChris FalokunNoch keine Bewertungen
- 1.6 FSI Inlet Manifold Removal Guide - Audi A2 Owners' ClubDokument3 Seiten1.6 FSI Inlet Manifold Removal Guide - Audi A2 Owners' Clubdusan jovanovicNoch keine Bewertungen
- Lahainaluna High School Cafeteria: Lahaina, Maui, HawaiiDokument42 SeitenLahainaluna High School Cafeteria: Lahaina, Maui, HawaiiKeerthy MoniNoch keine Bewertungen
- Fall 20122Dokument98 SeitenFall 20122DobarCovek67% (3)
- Luyện nghe Tiếng Anh có đáp án: I/ Listen and complete the textDokument3 SeitenLuyện nghe Tiếng Anh có đáp án: I/ Listen and complete the textVN LenaNoch keine Bewertungen
- Tyler & Wheeler Curriculum ModelDokument8 SeitenTyler & Wheeler Curriculum Modelliliyayanono100% (1)
- Ken Holt 06 The Secret of Hangman's InnDokument216 SeitenKen Holt 06 The Secret of Hangman's InnPastPresentFuture100% (2)
- Et200sp Im 155 6 PN ST Manual en-US en-USDokument47 SeitenEt200sp Im 155 6 PN ST Manual en-US en-USayaz officeNoch keine Bewertungen
- Family School Project Lesson Plan AstrologyDokument3 SeitenFamily School Project Lesson Plan Astrologyapi-529488210Noch keine Bewertungen
- Part 1. Question 1-7. Complete The Notes Below. Write NO MORE THAN THREE WORDS AND/OR A NUMBER For Each AnswerDokument13 SeitenPart 1. Question 1-7. Complete The Notes Below. Write NO MORE THAN THREE WORDS AND/OR A NUMBER For Each Answerahmad amdaNoch keine Bewertungen
- Day 1 Training Material FlowDokument200 SeitenDay 1 Training Material FlowGhazouani AymenNoch keine Bewertungen
- Police Cranston School Committee Member Stole PTO FundsDokument1 SeitePolice Cranston School Committee Member Stole PTO FundsashaydelineNoch keine Bewertungen
- Combat Storm - Shipping ContainerDokument6 SeitenCombat Storm - Shipping ContainermoiNoch keine Bewertungen
- T10 - PointersDokument3 SeitenT10 - PointersGlory of Billy's Empire Jorton KnightNoch keine Bewertungen
- Tip Sheet March 2017Dokument2 SeitenTip Sheet March 2017hoangvubui4632Noch keine Bewertungen
- KPI's Troubleshooting GuideDokument27 SeitenKPI's Troubleshooting GuideMohamed SayedNoch keine Bewertungen
- Business EthicsDokument10 SeitenBusiness EthicsTeguh HardiNoch keine Bewertungen
- Titus Selection of DiffuserDokument14 SeitenTitus Selection of DiffuserhanyassawyNoch keine Bewertungen
- Chapter 3 Mine Ventialtion ProblemDokument3 SeitenChapter 3 Mine Ventialtion ProblemfahimNoch keine Bewertungen
- Statement of Cash Flows AnswerDokument3 SeitenStatement of Cash Flows Answeranber mohammadNoch keine Bewertungen
- Massey Ferguson MF7600 Technician Workshop ManualDokument798 SeitenMassey Ferguson MF7600 Technician Workshop Manualgavcin100% (5)
- Auburn Bsci ThesisDokument5 SeitenAuburn Bsci Thesisafksaplhfowdff100% (1)
- Norma Geral Astm Bronze Alumínio - b150b150m.19198Dokument7 SeitenNorma Geral Astm Bronze Alumínio - b150b150m.19198EduardoNoch keine Bewertungen
- José Guadalupe PosadaDokument19 SeitenJosé Guadalupe PosadaJudy Baca100% (1)
- Letter of Intent Date: 18-Feb-2019 Mr. Ravi Mishra,: For Multiplier Brand Solutions PVT LTDDokument2 SeitenLetter of Intent Date: 18-Feb-2019 Mr. Ravi Mishra,: For Multiplier Brand Solutions PVT LTDRavi MishraNoch keine Bewertungen
- Program Logic FormulationDokument69 SeitenProgram Logic FormulationIan OffemariaNoch keine Bewertungen
- Caterpillar Sis (01.2014) MultilanguageDokument10 SeitenCaterpillar Sis (01.2014) MultilanguageTemmy Candra Wijaya100% (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (24)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNoch keine Bewertungen
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (5)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningVon EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningBewertung: 4 von 5 Sternen4/5 (3)
- Gut: the new and revised Sunday Times bestsellerVon EverandGut: the new and revised Sunday Times bestsellerBewertung: 4 von 5 Sternen4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 3.5 von 5 Sternen3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyVon EverandAn Autobiography of Trauma: A Healing JourneyBewertung: 5 von 5 Sternen5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisVon EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosVon Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosBewertung: 4.5 von 5 Sternen4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (253)