Beruflich Dokumente
Kultur Dokumente
Diabetes Pathophysiology
Hochgeladen von
Katelyn CherryCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diabetes Pathophysiology
Hochgeladen von
Katelyn CherryCopyright:
Verfügbare Formate
Diabetes Pathophysiology Paper
Kines 403 March 31st, 2012 Katelyn Cherry
Cherry
Disease Process Today, about 7% of the U.S population suffers from diabetes. Diabetes is a metabolic disorder that has the potential to affect the entire body. (Gulli, et al. 621). This disease arises when the body cannot control glucose levels in the blood. This disease has two different forms, Type I or Type II. Type I diabetes occurs when the body cannot produce insulin. In a recent study, it was found that this type of diabetes is characterized by a genetic predisposition that triggers a response by the bodys immune system. This causes interference within certain insulin producing cells in the pancreas. Type II diabetes occurs when the body is unable to use the insulin that was originally produced. This type of diabetes occurs when the amount of receptor sites for insulin decreases or there is defect within the receptor locations. The Type II form is typically linked to obese individuals (Medi-Info). In both Type I and Type II diabetes, the lack of insulin causes a decrease in the amount of glucose that can be carried across the cell membrane. In turn, the metabolism of lipids, carbohydrates, amino acids and proteins is disrupted, along with the storage of proteins in the muscles and fat in the adipose tissue. Because of these factors, this allows for an overproduction of glucose, thus blood glucose levels rise and hyperglycemia ensues (Medi-Info). Hypoglycemia, or low blood sugar, may also occur in individuals with diabetes. This develops in three different ways. First, when the glucose is taken up very rapidly, second, if glucose is released too slowly and finally, if too much insulin is introduced to the body. This generally occurs when an individual skips meals, takes too much insulin or drinks alcohol. If there is not enough glucose in the blood, glucose levels will fall, which will impair the functioning of the brain. Hypoglycemia is an acute condition that can be treated relatively fast as
Cherry
compared to hyperglycemia where it develops over time and may take hours or even days to treat. (Board). Affected Organ System The main organs that are affected due to diabetes consist primarily of the heart and blood vessels, kidneys, nervous system and eyes. Due to an increase in blood glucose levels, the cardiovascular system is at risk in individuals with diabetes. This is because the high blood sugar levels have a detrimental effect on lipids circulating throughout the bloodstream. This negative effect results in plaque buildup lining the blood vessel walls causing atherosclerosis, which is a precursor to a heart attack or stroke (Lind). The kidneys are also affected in people with diabetes because of the endless filtering of high glucose levels. This may eventually cause the kidneys to leak and may put the person at risk for renal disease (Lind). The nervous system may also be compromised in individuals with this condition. This is because nerve damage may be the product of high blood glucose levels. Automatic diabetic neuropathy is impairment within the bodys nervous system, which leads to loss of sexual functions, incontinence and the inability to produce sweat (Lind). Lastly, high blood sugar may also contribute to eye problems or even blindness. Glaucoma, a nerve disorder in the eye, may develop from high glucose levels. It is possible that this may cause a decrease in the amount of blood that enters the eye, resulting in blindness (Lind). Signs and Symptoms There are many signs and symptoms related to diabetes. Signs can be described as something that is physically seen, while symptoms are observed by the patient. According to the
Cherry
American Academy of Orthopedic Surgeons, the main symptoms of a hyperglycemic crisis include rapid, deep respirations, dehydration, a sweet and fruity odor on the breath, polyuria (excessive urination), polydipsia (excessive thirst), polyphagia (excessive eating) or varying degrees of unresponsiveness (Gulli, et al. 625). Signs and symptoms of a hypoglycemic crisis include the following; shallow respirations, diaphoresis (sweating), altered mental status (aggression, confusion or unusual behavior), hunger, anxiousness, seizure, fainting, weakness on one side of the body or coma (Gulli, et al. 626). Treatment The main treatment that is available to alleviate the symptoms of diabetes associated with hypoglycemia is glucose. Glucose can be administered orally between the cheek and gum-line. One tube contains approximately 15 grams of a gel-like glucose. Diabetic emergencies may sometimes cause altered mental status, which may be mistaken for a drug overdose, poisoning, head injury or seizure. These types of emergencies may also mimic stroke symptoms, therefore, it is important to obtain vitals a SAMPLE history and perform a secondary assessment to determine the cause of the symptoms (PA Protocol, 702). Oral glucose administered by a trained EMT provider is crucial for someone suffering from symptoms related to a diabetic emergency. When arriving on scene, the EMT must follow all standard procedures and then check the patients airway, breathing and circulation to rule out any life threats. The EMT may call ALS (advance life services) at this time in case the patient begins to rapidly deteriorate. After checking airway, breathing and circulation, high-flow oxygen must be administered via a non-rebreathing mask at 15 L/min. If the patient does not tolerate the mask, a nasal cannula may be used with a flow rate of 4-6 L/min. While it is not mandatory, a
Cherry
pulse oximeter may be utilized to monitor oxygen saturation of the blood. The EMT should examine the patient for any evidence that may point to the suspected cause, such as, a medical alert identification tag, needle marks, head trauma, incontinence of urine, stroke or medicine containers. If the patient is still experiencing hypoglycemia induced symptoms, the EMT may administer one tube of oral glucose. (PA Protocol, 702). The EMT must first check the six rights pertaining to the medication. These rights include, the right medication, patient, dose, route, time, documentation and finally that the medication has not expired. Then, the EMT must place a small amount of oral glucose on a tongue depressor and remove the non-rebreathing mask from the patients mouth. The EMT may then deposit the oral glucose between the cheek and gums. Next, the EMT must instruct the patient to not swallow the glucose, but instead let it dissolve and then reapply the oxygen. It is important to remember that the glucose may only be given to patients who are able to swallow (Gulli, et al. 631). The EMT may continue to administer oral glucose until the patient has improved. After the first tube is given, the patient may be transported to the hospital. The EMT must assess vitals en route to the hospital every 15 minutes if the patient is stable or every 5 minutes if patient is unstable (PA Protocol, 702)
Cherry
Bibliography Board, A.D.A.M. Editorial. "Hypoglycemia." Hypoglycemia. U.S. National Library of Medicine. Web. 31 Mar. 2012. <http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001423/>. Gulli, Benjamin, Joseph A. Ciatolla, and Leaugeay Barnes. Emergency Care and Transportation of the Sick and Injured. Sudbury, MA: Jones and Bartlett, 2011. Print. Lind, Melissa. "What Organs Are Affected When Diabetes Occur?"LIVESTRONG.COM. 21 Aug. 2011. Web. 31 Mar. 2012. <http://www.livestrong.com/article/78198-organsaffected-diabetes-occur/>. "Medi-Info.COM." Diabetes Mellitus. Medi-Info. Web. 31 Mar. 2012. <http://www.mediinfo.com/diabetes-mellitus/>. PA DOH BLS Protocol. Protocol #702. Print. 28 Mar. 2012.
Cherry
Das könnte Ihnen auch gefallen
- Diabetis MellitusDokument25 SeitenDiabetis Mellituscdamasco18Noch keine Bewertungen
- NCP - Poststreptococcal GlomerulonephritisDokument12 SeitenNCP - Poststreptococcal GlomerulonephritisAya BolinasNoch keine Bewertungen
- Family health nursing and malnutritionDokument5 SeitenFamily health nursing and malnutritionLea TanNoch keine Bewertungen
- Risk For Bleeding - Cirrhosis NCPDokument2 SeitenRisk For Bleeding - Cirrhosis NCPPaula AbadNoch keine Bewertungen
- Colon Cancer Case Study - 64yo Male Diagnosed After Rectal BleedingDokument2 SeitenColon Cancer Case Study - 64yo Male Diagnosed After Rectal BleedingDragan Djordjevic100% (4)
- Pathophysiology of Diabetes Mellitus Type 2Dokument1 SeitePathophysiology of Diabetes Mellitus Type 2faula rocamora100% (3)
- NCP Ineffective Tissue PerfusionDokument7 SeitenNCP Ineffective Tissue Perfusionapi-283753722100% (3)
- Pathophysiology of Diabetes Mellitus Type 1Dokument3 SeitenPathophysiology of Diabetes Mellitus Type 1CajRofuli100% (2)
- Decreased Cardiac Output RM 7Dokument9 SeitenDecreased Cardiac Output RM 7api-283470660Noch keine Bewertungen
- Cardiology Case 1Dokument2 SeitenCardiology Case 1vil62650% (2)
- Nursing Concept Map for Diabetes Patient ManagementDokument1 SeiteNursing Concept Map for Diabetes Patient ManagementSev Kuzmenko0% (1)
- Physical Assessment For Patient With DM Type1Dokument4 SeitenPhysical Assessment For Patient With DM Type1Mae AzoresNoch keine Bewertungen
- ABC: Sickle-Cell Anemia, Shock, PoisoningDokument46 SeitenABC: Sickle-Cell Anemia, Shock, Poisoningroneln100% (1)
- Lymphocytic LeukemiaDokument6 SeitenLymphocytic Leukemiaル シリ100% (1)
- Impaired Tissue Integrity - CellulitisDokument3 SeitenImpaired Tissue Integrity - CellulitisKelvin Kurt B. AgwilangNoch keine Bewertungen
- DM NCPDokument2 SeitenDM NCPVirgilio Reyes ManuelNoch keine Bewertungen
- Leukemias: Care SettingDokument11 SeitenLeukemias: Care SettingTinNoch keine Bewertungen
- Mcdonald Case StudyDokument12 SeitenMcdonald Case StudyJohn WickNoch keine Bewertungen
- Case Study DM TYPE IIDokument16 SeitenCase Study DM TYPE IIrose_avy200975% (4)
- Diverticular DiseaseDokument8 SeitenDiverticular Diseasenurse_enzo100% (1)
- Case Study 18 CKDDokument7 SeitenCase Study 18 CKDapi-301049551Noch keine Bewertungen
- GordonsDokument83 SeitenGordonsAlex SilvanoNoch keine Bewertungen
- DMDokument76 SeitenDMrose ann ayala100% (1)
- Diabetes Mellitus Type 2 Schematic DiagramDokument1 SeiteDiabetes Mellitus Type 2 Schematic DiagramChristelle GarciaNoch keine Bewertungen
- University of Northern PhilippinesDokument1 SeiteUniversity of Northern PhilippinesCezanne CruzNoch keine Bewertungen
- DM Case StudyDokument4 SeitenDM Case Studyapi-273276737100% (3)
- NCP 3Dokument3 SeitenNCP 3Grae TaclobNoch keine Bewertungen
- Case Study PresentationDokument21 SeitenCase Study Presentationapi-302058960100% (2)
- Deficient Fluid VolumeDokument1 SeiteDeficient Fluid VolumeSheila ErpeloNoch keine Bewertungen
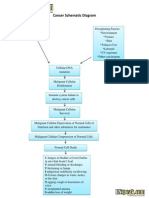
- Cancer Schematic DiagramDokument1 SeiteCancer Schematic DiagramCyrus De Asis100% (4)
- GoutDokument12 SeitenGoutEarle Jimenez Niervo RN100% (1)
- DM Case StudyDokument4 SeitenDM Case Studylspearman100% (7)
- Nursing Care Plan For Type1 DiabetesDokument1 SeiteNursing Care Plan For Type1 DiabetesBushra AlkhdourNoch keine Bewertungen
- Asthma Nanda Diagnoses Goals InterventionsDokument4 SeitenAsthma Nanda Diagnoses Goals InterventionsZinya RobinsonNoch keine Bewertungen
- ER equipments & drugsDokument3 SeitenER equipments & drugsApple LlanesNoch keine Bewertungen
- Dka Patho DiagramDokument1 SeiteDka Patho DiagramGrae TaclobNoch keine Bewertungen
- Type 1 Diabetes Case Study: 15-Year-Old Asian American GirlDokument62 SeitenType 1 Diabetes Case Study: 15-Year-Old Asian American GirlHananErekat100% (2)
- Our Lady of Fatima University - Valenzuela Campus College of NursingDokument27 SeitenOur Lady of Fatima University - Valenzuela Campus College of NursingKHRISTINE MAE ROQUENoch keine Bewertungen
- HTN Urgency Case StudyDokument4 SeitenHTN Urgency Case StudyJavin TNoch keine Bewertungen
- Case Study Heart Attack PDFDokument30 SeitenCase Study Heart Attack PDFtkgoon634950% (2)
- Case Report - Deep Vein ThrombosisDokument12 SeitenCase Report - Deep Vein ThrombosisAndi Meidin AnugerahNoch keine Bewertungen
- Gerontologic Health Promotion ActivityDokument3 SeitenGerontologic Health Promotion ActivityCorinne50% (2)
- Case Liver CirrhosisDokument73 SeitenCase Liver CirrhosisJesus Orita-Delima100% (1)
- Diabetes Mellitus NCP MandoDokument7 SeitenDiabetes Mellitus NCP MandoJan Mar BueraNoch keine Bewertungen
- Mae LNMDokument9 SeitenMae LNMCristina L. Jayson33% (3)
- Endocrine - PathophysiologyDokument66 SeitenEndocrine - Pathophysiologyskeebs23100% (2)
- Activity IntoleranceDokument6 SeitenActivity IntoleranceRaidis PangilinanNoch keine Bewertungen
- PathophysiologyDokument4 SeitenPathophysiologyAngelou Joefred Congreso100% (1)
- Pathophysiology of DiabetesDokument2 SeitenPathophysiology of DiabetesCyrus De Asis100% (4)
- CVD Case StudyDokument9 SeitenCVD Case Studyapi-346620455100% (3)
- Assignment For Oxy. Online BasedDokument5 SeitenAssignment For Oxy. Online BasedNurhassem Nor AkangNoch keine Bewertungen
- Narrative PathophysiologyDokument18 SeitenNarrative PathophysiologyNica Georgelle Maniego SamonteNoch keine Bewertungen
- NCS-DM Type 2 For Case PresentationDokument49 SeitenNCS-DM Type 2 For Case Presentationadnelg0771% (7)
- Gouty Arthritissss PathophyDokument2 SeitenGouty Arthritissss Pathophybilliam123Noch keine Bewertungen
- Pathophysiology of Diabetes Mellitus: Predisposing and Precipitating FactorsDokument2 SeitenPathophysiology of Diabetes Mellitus: Predisposing and Precipitating FactorsJerene67% (3)
- DMDokument24 SeitenDMJudeLaxNoch keine Bewertungen
- CHF Case Study on Congestive Heart FailureDokument40 SeitenCHF Case Study on Congestive Heart Failurelyndzy100% (1)
- Case Study, Chapter 16, Assessing EyesDokument1 SeiteCase Study, Chapter 16, Assessing Eyesclyde i am50% (2)
- Diabetes Mellitus Concept MapDokument2 SeitenDiabetes Mellitus Concept MapIzhra Margate100% (5)
- Case Study in DMDokument34 SeitenCase Study in DMKathrina Marie B. BinaraoNoch keine Bewertungen
- CPR Instruction SetDokument6 SeitenCPR Instruction SetKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument6 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument8 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument8 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument8 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument8 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument7 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Respiratory PathophysiologyDokument6 SeitenRespiratory PathophysiologyKatelyn CherryNoch keine Bewertungen
- Anaphylactic ShockDokument8 SeitenAnaphylactic ShockKatelyn CherryNoch keine Bewertungen
- Kines 403 CardiapathopaperDokument6 SeitenKines 403 CardiapathopaperKatelyn CherryNoch keine Bewertungen
- Kines 403 CardiapathopaperDokument6 SeitenKines 403 CardiapathopaperKatelyn CherryNoch keine Bewertungen
- Kines 403 CardiapathopaperDokument6 SeitenKines 403 CardiapathopaperKatelyn CherryNoch keine Bewertungen
- Measurement of Glucose Homeostasis in VivoDokument10 SeitenMeasurement of Glucose Homeostasis in Vivo19400668Noch keine Bewertungen
- What Is Diabetes? What Causes Diabetes?: Fast Facts On DiabetesDokument6 SeitenWhat Is Diabetes? What Causes Diabetes?: Fast Facts On DiabetesAlfred Melvin SolivaNoch keine Bewertungen
- GlibenclamideDokument13 SeitenGlibenclamiderotuaserevinaNoch keine Bewertungen
- Kay's Final FRCA NotesDokument10 SeitenKay's Final FRCA Notesmyat2567% (6)
- Concise Review: Importance of Probiotics Yogurt For Human Health ImprovementDokument6 SeitenConcise Review: Importance of Probiotics Yogurt For Human Health ImprovementIOSRjournalNoch keine Bewertungen
- Novorapid® Flexpen®: What Is in This Leaflet What Novorapid® Is Used ForDokument9 SeitenNovorapid® Flexpen®: What Is in This Leaflet What Novorapid® Is Used ForjessyNoch keine Bewertungen
- Estimation of Salivary GlucoseDokument10 SeitenEstimation of Salivary GlucoseSuganya MurugaiahNoch keine Bewertungen
- Diabetes Mellitus: DefinitionDokument54 SeitenDiabetes Mellitus: DefinitionislamnourNoch keine Bewertungen
- Dec Vaspen NewsletterDokument7 SeitenDec Vaspen Newsletterapi-287472804Noch keine Bewertungen
- Managing Your DiabetesDokument34 SeitenManaging Your DiabetesDeresse KebedeNoch keine Bewertungen
- Leaflet DiabetesDokument3 SeitenLeaflet DiabetesWiratama JrsNoch keine Bewertungen
- Presentation Diagnosis of Diabetes Mellitus: Presented by Kanwal AmjadDokument29 SeitenPresentation Diagnosis of Diabetes Mellitus: Presented by Kanwal AmjadSpencerNoch keine Bewertungen
- HypoglycaemiaDokument36 SeitenHypoglycaemiaAwatef AbushhiwaNoch keine Bewertungen
- Diabetic Foot Care Education LackingDokument5 SeitenDiabetic Foot Care Education LackingSarah EddiahNoch keine Bewertungen
- Aloe Vera-A Wonder Plant Its History, Cultivation and Medicinal Uses PDFDokument4 SeitenAloe Vera-A Wonder Plant Its History, Cultivation and Medicinal Uses PDFveronyk28Noch keine Bewertungen
- Case History and Data Interpretation in Medical Practice, 3e (January 31, 2015) - (9351523756) - (Jaypee Brothers Medical Pub)Dokument492 SeitenCase History and Data Interpretation in Medical Practice, 3e (January 31, 2015) - (9351523756) - (Jaypee Brothers Medical Pub)Khan100% (3)
- November 2012 Question Paper 32 PDFDokument20 SeitenNovember 2012 Question Paper 32 PDFSamson YauNoch keine Bewertungen
- Canada Board Mcqs Qualifing ExamDokument26 SeitenCanada Board Mcqs Qualifing Examdr47Noch keine Bewertungen
- South Asian Carbohydrate CountingDokument19 SeitenSouth Asian Carbohydrate CountingavicennaxNoch keine Bewertungen
- Nursing Care Plan For Type1 DiabetesDokument1 SeiteNursing Care Plan For Type1 DiabetesBushra AlkhdourNoch keine Bewertungen
- Garlic (Allium Sativum) As An Anti-Diabetic Agent (Allicin)Dokument13 SeitenGarlic (Allium Sativum) As An Anti-Diabetic Agent (Allicin)Muhammad Arsalan100% (1)
- New Gcse: Foundation Tier Biology 1Dokument15 SeitenNew Gcse: Foundation Tier Biology 1dao5264Noch keine Bewertungen
- Cinnamomum Zeylanicum and Cinnamomum Aromaticum Monograph (Marybeth Missenda) 2013Dokument30 SeitenCinnamomum Zeylanicum and Cinnamomum Aromaticum Monograph (Marybeth Missenda) 2013Marybeth MissendaNoch keine Bewertungen
- Type 2 Diabetes MellitusDokument29 SeitenType 2 Diabetes MellitusHuong NguyenNoch keine Bewertungen
- 10-Comparative Study of The Hypoglycemic Effects of Coconut Water Extract of Picralima Nitida Seeds and Daonil in Alloxan-Induced Diabetic RatsDokument3 Seiten10-Comparative Study of The Hypoglycemic Effects of Coconut Water Extract of Picralima Nitida Seeds and Daonil in Alloxan-Induced Diabetic RatsAditya Praja'schNoch keine Bewertungen
- Healthmedicinet I 2017 1Dokument676 SeitenHealthmedicinet I 2017 1tuni santeNoch keine Bewertungen
- Introduction To DiabetesDokument9 SeitenIntroduction To DiabetesSameer Saurabh100% (1)
- Clincal Practice Guidelines For Diabetes in The PhilippinesDokument40 SeitenClincal Practice Guidelines For Diabetes in The PhilippinesRans NosceNoch keine Bewertungen
- DiabetesMellitus enDokument2 SeitenDiabetesMellitus enRajesh KumarNoch keine Bewertungen