Beruflich Dokumente
Kultur Dokumente
NCP
Hochgeladen von
Trixie Al MarieCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NCP
Hochgeladen von
Trixie Al MarieCopyright:
Verfügbare Formate
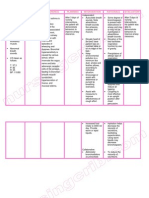
Patient X Chief complaint: Difficulty of breathing Gender: Male Diagnosis: Retained Hemothorax s/p CTT insertion right secondary
to multiple stabbed wound Cues ( Subjective/ Objective) Subjective: Nakukurian gad ako pag ginhawa. as verbalized by the patient. Objective: - respiratory rate of 26 cycles per minute - dyspnea - alteration in depth of breathing - nasal flaring - pursed lip breathing Nursing Diagnosis Ineffective breathing pattern related to decreased lung expansion Rationale The lung contains gas, blood, thin alveolar walls and support structures. The alveolar wall contains elastic and collagen fibers; these form a threedimensional basketlike structure that allows the lung to inflate in all directions. These fibers are capable of stretching when a pulling force is exerted on them from outside of the body or when they inflate from within. The elastic recoil helps return the lungs to their resting volume. If air or increased amounts of serous fluid, blood, or pus accumulate in the thoracic space, it may hinder adequate lung expansion and causes the pleural membranes (essential for diffusion of gases) to compress thus respiratory Goal of Care
Age: 42 years old
Nursing Intervention Independent:
Rationale
Evaluation
After 1 hour of nursing interventions, the client will: 1. Establish a normal and effective breathing pattern within clients normal range.
GOAL MET. 1. Identify etiology or precipitating factors. Understanding the cause is necessary for choice of therapeutic measures. Monitoring the vital signs is necessary to evaluate the degree of compromise. Respiratory rate less than 12 or more than 24 or use of accessory muscles indicate distress. Diminished lung sounds indicate possible poor air movement and impaired gas exchange. Respiratory distress and changes in vital signs occur as a result of physiologic stress and pain, or may indicate development of shock due to hypoxia or hemorrhage. Within 1 hour of nursing care, the patient stated acceptable dyspnea. Mas nakakaginhawa na ako hin maupay kesa kanina. In addition, the patient participated in treatment regimen. Vital signs are within normal range.
2. Monitor vital signs.
3. Assess lung sounds, respiratory rate and effort and the use of accessory muscles.
4. Evaluate respiratory function, noting rapid or shallow respirations, dyspnea, reports of air hunger, and changes in vital signs.
difficulties follow. Sources: Medical-Surgical Nursing 8th Edition by Black and Hawks Understanding Medical-Surgical Nursing 3rd Edition by William, L. Hopper 6. Encourage adequate rest and limit activities within clients level of tolerance. Promote a calm and restful environment. Dependent: 1. Administer supplemental oxygen as ordered by the physician. 2. Administer medications as prescribed by the physician. Supplemental oxygen decreases hypoxia. 5. Observe skin and mucous membranes for signs of cyanosis. Cyanosis indicates poor oxygenation. Oral mucous membrane cyanosis indicates serious hypoxia. Helps limit oxygen needs and consumption.
To treat underlying conditions.
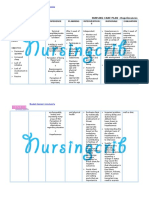
Patient X Chief complaint: Difficulty of breathing Gender: Male Diagnosis: Retained Hemothorax s/p CTT insertion right secondary to multiple stabbed wound Cues ( Subjective/ Objective) Subjective: Na kirot an didi may tungod ha ak tubo. as verbalized by the patient. Objective: - guarding behavior, protective gestures, positioning to avoid pain - facial mask of pain - narrowed focus Nursing Diagnosis Acute pain related to presence of tubes and drains Rationale The effect of anesthesia can be diminished after the patient has been fully awakened and conscious. The hole made by incision and insertion of the tube can be painful as movements often cause tension and pull to the tube thus the perceived pain. Source: Understanding Medical-Surgical Nursing 3rd Edition by William, L. Hopper Goal of Care
Age: 42 years old
Nursing Intervention Independent: 1. Assess pain every four hours and as needed.
Rationale
Evaluation GOALS MET.
Within 8 hours of nursing interventions, the client will:
Good assessment must guide treatment. Changes in these vital signs often indicate acute pain and discomfort. Note: Some clients may have a slightly lowered BP, which returns to normal range after pain relief is achieved. Discomfort can be caused or aggravated by presence of nonpatent indwelling catheters, parenteral lines (bladder pain, gastric fluid and gas accumulation, and infiltration of IV fluids or medications). Understanding the cause of the discomfort provides emotional reassurance.
1. Report pain relieved or controlled. (State that the pain is relieved 2. Assess vital signs from the scale of 3-5 noting tachycardia, out of 10 in pain scale.) hypertension and increased respirations, 2. Verbalize at least 2 even if client denies non-pharmacologic pain. methods that provide relief. 3. Appears relaxed, able to rest or sleep and 3. Assess causes of participate in activities possible discomfort appropriately. other than operative procedure.
The patients pain was relieved as evidenced by pain scale of 4 out of 10. The patient verbalized method that provided relief such as the pain medication given, distraction techniques by constantly talking to significant others.
4. Provide information about transitory nature of discomfort, as appropriate.
5. Reposition as indicated. (Example: semi-Fowler; lateral Sims)
May relieved pain and enhance circulation. semi-Fowlers position relieves abdominal muscle tension and arthritic back muscle tension, whereas lateral Sims will relieve dorsal pressure. Improves circulation, reduces muscle tension and anxiety associated with pain. Enhances sense of well-being. Relieves muscle and emotional tension; enhances sense of control and may improve coping abilities.
6. Provide additional comfort measures; e.g., backrub, heat or cold application. 7. Encourage use of relaxation techniques; e.g., deep breathing exercises, guided imagery, visualization, music. Dependent: 1. Administer analgesics as ordered by the physician.
The patient who is pain free will be better able to participate in care and take measures to prevent complications.
Patient X Chief complaint: Difficulty of breathing Gender: Male Diagnosis: Retained Hemothorax s/p CTT insertion right secondary to multiple stabbed wound Cues ( Subjective/ Objective) Objective: Post op status: Chest tube attached to the patient. Nursing Diagnosis Risk for infection related to invasive procedure Rationale Infections occur when an organism (e.g., bacterium, virus, fungus, or other parasite) invades a susceptible host. Breaks in the integument, the bodys first line of defense, and/or the mucous membranes allow invasion by pathogens. If the hosts (patients) immune system cannot combat the invading organism adequately, an infection occurs. Open wounds, traumatic or surgical, can be sites for infection; soft tissues (cells, fat, muscle) and organs (kidneys, lungs) can also be sites for infection either after trauma, invasive procedures, or by invasion of pathogens carried through the bloodstream or lymphatic system. Goal of Care
Age: 42 years old
Nursing Intervention Independent: 1. Note risk factors for occurrence of infection.
Rationale
Evaluation GOALS MET.
After 24 hours of nursing interventions the client will: 1. Verbalize understanding of individual causative or risk factors. 2. Identify at least two interventions to prevent or reduce risk of infection. 3. Demonstrate at least two techniques to promote safe environment. 4. Be free of infection as evidenced by temperature, blood pressure within normal limits and absence of complications (such as redness and swelling at incision site)
Intubation, prolonged mechanical ventilation, trauma, general debilitation, malnutrition, age, and invasive procedures are factors that potentiate clients risk of acquiring infection and prolonging recovery. Hand washing may be the simplest but the most important key to prevent hospitalacquired infections. Maximizes lung expansion and mobilization of secretions to prevent or reduce atelectasis and accumulation of sticky, thick secretions. Early recognition and treatment of infection enhances outcomes.
2. Reduce nosocomial risk factors via proper hand washing or alcohol-based hand rubs by all caregivers and patient as well. 3. Encourage deep breathing, coughing with frequent position changes.
After 24 hours of nursing care, patient verbalized understanding of the possible factors which may contribute to infection. In addition, patients vital signs are within normal range and no sign of infection was noted.
4. Monitor and report signs and symptoms of infection: fever,
Source: www.Scribd.com www.MedicineNet.com
increased respiratory rate. 5. Check all tubing for kinds, breaks or broken connections. Verify that all connections are securely taped. Microorganisms may infiltrate if there is any breaks in the connection.
6. Verify that the This allows proper drainage system is drainage of pleural below level of patients fluid. chest at all times. 7. Instruct client / significant others to protect the integrity of skin/insertion sites. Dependent: 1. Administer antibiotics as needed. Administering antibiotics helps treat microorganisms that are suspected to cause infection and/or complications to the patient. Protecting the integrity of the skin helps prevent infection at the incision site.
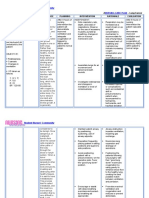
Patient X Chief complaint: Difficulty of breathing Gender: Male Diagnosis: Retained Hemothorax s/p CTT insertion right secondary to multiple stabbed wound Cues ( Subjective/ Objective) Subjective: Diri ak nakakakiwa hin maupay kay nahadlok ak bangin matangal an tubo. as verbalized by the patient. Objective: Source: - inability to move or change position when lying in bed - needs assistance when sitting down - demonstrates guarding behavior at surgical site Understanding Medical-Surgical Nursing 3rd Edition by William, L. Hopper Nursing Diagnosis Impaired physical mobility related to discomfort at surgical site Rationale The incision site after chest tube insertion is not closed for the tube to be detached. This might cause friction between the surface of the skin and the tube which might cause discomfort and restrict movement. Goal of Care
Age: 42 years old
Nursing Intervention Independent 1. Determine degree of mobility. 2. Observe movement when client is unaware of observation. 3. Support affected body part. 4. Perform range of motion exercises, passively at first then actively when the patient is able. 5. Assist patient to ambulate as tolerated on first day as needed. Dependent: 1. Administer medications prior to activity as needed.
Rationale
Evaluation GOALS PARTIALLY MET.
After 2 days of nursing interventions, the client will: 1. Verbalize understanding of situation or risk factors and individual treatment regimen and safety measures. 2. Demonstrate techniques that enable resumption of activities. 3. Maintain skin integrity as evidenced by absence of swelling, redness and pus formation at the surgical site.
To assess functional ability.
After 2 days of nursing intervention, the patient verbalized To note any understanding of the incongruencies with situation and risk reports of abilities. factors and also individual treatment. However, patient still To maintain position of demonstrated limited function. activity and remains in bed. This helps prevent contracture of the arm and the shoulder on the affected site. Ambulation helps maintain mobility and prevents post operative complications.
To permit maximal effort and involvement in activity.
Patient X Chief complaint: Difficulty of breathing Gender: Male Diagnosis: Retained Hemothorax s/p CTT insertion right secondary to multiple stabbed wound Cues ( Subjective/ Objective) Objective: Post op status: Chest tube attached to the patient. Nursing Diagnosis Risk for impaired skin integrity related to physical immobilization Rationale Immobility, which leads to pressure, shear, and friction, is the factor most likely to put an individual at risk for skin integrity. Advanced age; the normal loss of elasticity; inadequate nutrition; environmental moisture, especially from incontinence; and vascular insufficiency potentiate the effects of pressure and hasten the development of skin breakdown. Source: www. Scribd.com Goal of Care
Age: 42 years old
Nursing Intervention
Rationale
Evaluation
Within 3 hours of nursing Independent: interventions, the client will: 1. Assess skin. Note color, turgor, circulation, and 1. Verbalize sensation. understanding of condition and causative factors. 2. Maintain or instruct good skin hygiene. 2. Identify at least 2 interventions appropriate for specific condition. 3. Promote adequate fluid intake. 3. Demonstrate behaviors/lifestyle changes to promote 4. Practice aseptic technique healing and prevent for complications/recurrence. cleansing/dressing/medicating lesions. 4. Display progressive improvement in 5. Change position frequently wound/lesion healing. in bed and chair.
GOALS MET Establishes comparative baseline providing opportunity for timely intervention. Maintaining clean, dry skin provides a barrier of infection. Helps maintain good circulating volume for tissue perfusion. Reduce risk for crosscontaminations. After 3 hours of nursing interventions, the client was able to verbalize understanding of conditions, identified appropriate interventions, demonstrated and displayed behaviors to promote wound healing.
Improve circulation, muscle tone and promotes client participation. Avoids friction/abrasion injury of skin.
6. Keep sheets and bedclothes clean, dry and free from wrinkles, crumbs and other irritating materials.
Dependent: 1. Administer nutritional supplements and vitamins as indicated. Aids in healing/cellular regeneration.
Patient X Chief complaint: Difficulty of breathing Gender: Male Diagnosis: Retained Hemothorax s/p CTT insertion right secondary to multiple stabbed wound Cues ( Subjective/ Objective) Subjective: Nayakan hi doc nga meada pa tubig ha ak baga. Asya nakukurian ako pag ginhawa. Objective: - difficulty of breathing - nasal flaring - ineffective cough Nursing Diagnosis Ineffective airway clearance related to retained secretions Rationale Normally the lungs are free from secretions. Due to the trauma that has occurred on the ribs, an intense inflammatory response occurred. Exudation of plasma, leukocytes, and infiltration of most cells, growth factors and inflammatory leukocytes occurs in effect. These fluid and exudates crosses the permeable membrane of the pleurae causing it to accumulate in the membranous space. Source: www. Scribd.com Goal of Care
Age: 42 years old
Nursing Intervention
Rationale
Evaluation
Within 8 hours of nursing Independent: interventions, the client will: 1. Assess/monitor respiratory rate. 1. Maintain airway patency. 2. Verbalize understanding of cause and therapeutic regimen. 3. Demonstrate at least 2 behaviors to improve or maintain clear airway. 2. Note presence/degree of dyspnea. Use 0-10 scale to rate breathing difficulty.
GOAL MET. Tachypnea is usually present to some degree and maybe pronounced during stress/concurrent acute infection. Respirations may be shallow and rapid with prolonged expiration in comparison to inspiration. Respiratory dysfunction is variable depending on the underlying process. Using a 0-10 scale to rate dyspnea aids in quantifying and tacking respiratory distress. Elevation of the head of the bed facilitates respiratory function by use of gravity; however, client in severe distress will seek the position that Within 8 hours of nursing interventions, patient was able to verbalized understanding of regimen and demonstrated effective exercise. Airway patency is maintained.
3. Assist client to assume position of comfort; e.g. elevate head of bed, have client lean on overbed table or sit on edge of bed.
most eases breathing. Supporting arms/legs with table, pillows, and so on helps reduce muscle fatigue and can aid chest expansion. 4. Encourage/assist with abdominal or pursed lip breathing exercises. Provides client with some means to cope with/control dyspnea and reduce airtrapping. Hydration helps decrease the viscosity of secretions, facilitating expectoration.
5. Encourage to increase fluid intake. Provide warm/tepid liquids. Recommend intake of fluids between instead of during meals.
Das könnte Ihnen auch gefallen
- Nursing Care PlanDokument13 SeitenNursing Care PlanCris Solis33% (3)
- NURSING CARE PLAN Problem Body Weakness Nursing Diagnosis Impaired PhysicalDokument1 SeiteNURSING CARE PLAN Problem Body Weakness Nursing Diagnosis Impaired Physicalmitchie riveraNoch keine Bewertungen
- Cues Nursing Diagnosis Scientific Rationale Goals Nursing Interventions Rationale EvaluationDokument3 SeitenCues Nursing Diagnosis Scientific Rationale Goals Nursing Interventions Rationale EvaluationIngrid Nicolas100% (1)
- NCP Impaired Gas Exhange CHEST INJURYDokument4 SeitenNCP Impaired Gas Exhange CHEST INJURYMa. Elaine Carla Tating100% (2)
- Nursing Care Plan For A Patient With Pleural EffusionDokument4 SeitenNursing Care Plan For A Patient With Pleural EffusionTrixie Anne GamotinNoch keine Bewertungen
- NCP LocDokument2 SeitenNCP LocMel RodolfoNoch keine Bewertungen
- Nursing Care PlanDokument11 SeitenNursing Care Planaycee0316100% (1)
- Nursing Care PlanDokument4 SeitenNursing Care PlanAdreanah Martin RañisesNoch keine Bewertungen
- TB, Ineffectivbe Breathing PatternsDokument1 SeiteTB, Ineffectivbe Breathing PatternsnikkilyceeNoch keine Bewertungen
- NCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsDokument3 SeitenNCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsSarah Ann Jamilla FaciolanNoch keine Bewertungen
- Nursing Care PlanDokument4 SeitenNursing Care PlanJoy Callo100% (2)
- Nursing Care Plan Bronchial AsthmaDokument2 SeitenNursing Care Plan Bronchial AsthmaSummer Ilu100% (1)
- NCP Inffective Tissue PerfusionDokument3 SeitenNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- Ineffective Breathing PatternDokument5 SeitenIneffective Breathing PatternruguNoch keine Bewertungen
- ANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationDokument2 SeitenANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationEdrianne Tui100% (2)
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDokument2 SeitenNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- Nursing Care PlanDokument4 SeitenNursing Care Planapi-309251523Noch keine Bewertungen
- Fdar UTIDokument2 SeitenFdar UTINickaela CalalangNoch keine Bewertungen
- NCP For SVTDokument6 SeitenNCP For SVTRen VillenaNoch keine Bewertungen
- Nursing Care Plan For "HEMOTHORAX PNEUMOTHORAX"Dokument8 SeitenNursing Care Plan For "HEMOTHORAX PNEUMOTHORAX"jhonroks78% (9)
- NCP (Deficient Fluid VolumeDokument3 SeitenNCP (Deficient Fluid VolumeNica RespondoNoch keine Bewertungen
- NCP Ineffective Breathing GunshotDokument3 SeitenNCP Ineffective Breathing GunshotMikko Enoc100% (1)
- NCP - Ineffective Airway ClearanceDokument2 SeitenNCP - Ineffective Airway ClearanceKhat100% (1)
- Nursing Care Plan Infection)Dokument4 SeitenNursing Care Plan Infection)Kez Domine100% (1)
- NCP HemothoraxDokument3 SeitenNCP HemothoraxMichael John F. NatividadNoch keine Bewertungen
- Final NCP Ineffective Airway ClearanceDokument8 SeitenFinal NCP Ineffective Airway ClearanceHazel EndayaNoch keine Bewertungen
- Nursing Measures To Maintain Normal Respiratory Function and OxygenationDokument2 SeitenNursing Measures To Maintain Normal Respiratory Function and Oxygenationlodeth100% (2)
- Impaired Gas Exchange-Sample NCPDokument1 SeiteImpaired Gas Exchange-Sample NCPKaycee BinanNoch keine Bewertungen
- Assessment Diagnosis Planning Intervention EvaluationDokument2 SeitenAssessment Diagnosis Planning Intervention EvaluationCharissa Magistrado De LeonNoch keine Bewertungen
- Prioritized Nursing Problem For Pneumothorax Nursing Diagnosis Nursing Intervention RationaleDokument3 SeitenPrioritized Nursing Problem For Pneumothorax Nursing Diagnosis Nursing Intervention RationaleJoshua VillarbaNoch keine Bewertungen
- Care Plan ExampleDokument2 SeitenCare Plan Exampleincess27100% (1)
- Ncp-Ineffective Airway ClearanceDokument3 SeitenNcp-Ineffective Airway Clearancelouanne0550% (2)
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDokument2 SeitenNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Assessment Diagnosis Planning Implementation Rationale EvaluationDokument3 SeitenAssessment Diagnosis Planning Implementation Rationale Evaluationria_soriano_2Noch keine Bewertungen
- NCP - Ineffective Airway ClearanceDokument4 SeitenNCP - Ineffective Airway ClearanceKim Gabrielle Exene LeeNoch keine Bewertungen
- NCP For OxygenationDokument6 SeitenNCP For OxygenationChriz LechNoch keine Bewertungen
- Stroke Nursing Care PlanDokument1 SeiteStroke Nursing Care PlanTracy PearlNoch keine Bewertungen
- NCP PneumothoraxDokument3 SeitenNCP Pneumothorax'Harold Mark Borja100% (2)
- Nursing Care Plan For Hopelessness NCPDokument5 SeitenNursing Care Plan For Hopelessness NCPRammiel Saylo CarlosNoch keine Bewertungen
- Nursing Care PlanDokument5 SeitenNursing Care PlanAnju Luchmun100% (2)
- NCP For Ineffective Breathing Pattern - RMC CasepressDokument2 SeitenNCP For Ineffective Breathing Pattern - RMC Casepressmissyuri08Noch keine Bewertungen
- Ineffective Breathing PatternDokument2 SeitenIneffective Breathing PatternEna Katherine CanonoNoch keine Bewertungen
- NCP - Ineffective Airway ClearanceDokument4 SeitenNCP - Ineffective Airway ClearanceJet BautistaNoch keine Bewertungen
- 6 Pleural Effusion Nursing Care PlansDokument7 Seiten6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNoch keine Bewertungen
- Lung Cancer (Nursing Care)Dokument5 SeitenLung Cancer (Nursing Care)heiyuNoch keine Bewertungen
- Nursing Care Plan For A Patient With Pleural EffusionDokument5 SeitenNursing Care Plan For A Patient With Pleural Effusionmac042250% (4)
- Nursing Care PlanDokument9 SeitenNursing Care PlanJam AbantaoNoch keine Bewertungen
- NCP (Case Pres)Dokument1 SeiteNCP (Case Pres)Flauros Ryu JabienNoch keine Bewertungen
- NURSING-CARE-PLAN-Lung-Cancerxxx 2Dokument3 SeitenNURSING-CARE-PLAN-Lung-Cancerxxx 2Caroline ChaNoch keine Bewertungen
- NURSING-CARE-PLAN-Lung-Cancerxxx 1Dokument3 SeitenNURSING-CARE-PLAN-Lung-Cancerxxx 1Caroline ChaNoch keine Bewertungen
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDokument10 SeitenAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle Acena100% (2)
- NCPDokument7 SeitenNCPRuth MontebonNoch keine Bewertungen
- NCP Difficulties in BreathingDokument4 SeitenNCP Difficulties in BreathingKingJayson Pacman06Noch keine Bewertungen
- NURSING CARE PLAN - Lung CancerDokument3 SeitenNURSING CARE PLAN - Lung Cancerderic80% (15)
- NCPDokument3 SeitenNCPDyanne BautistaNoch keine Bewertungen
- CopdDokument6 SeitenCopdapi-3717941100% (2)
- NCP-Drug Study 2Dokument4 SeitenNCP-Drug Study 2hsiriaNoch keine Bewertungen
- NCP For CAP TB.Dokument5 SeitenNCP For CAP TB.Cherry Ann BalagotNoch keine Bewertungen
- IPPA SampleDokument28 SeitenIPPA Samplekimglaidyl bontuyanNoch keine Bewertungen
- Assessment Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale EvaluationDokument3 SeitenAssessment Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale EvaluationMel Izhra N. MargateNoch keine Bewertungen
- Drug Study (Clindamycin)Dokument1 SeiteDrug Study (Clindamycin)roseonabreeze100% (7)
- NCP HemothoraxDokument3 SeitenNCP Hemothoraxroseonabreeze0% (2)
- Journal ReadingDokument3 SeitenJournal ReadingroseonabreezeNoch keine Bewertungen
- Pregnancy DisordersDokument3 SeitenPregnancy DisordersroseonabreezeNoch keine Bewertungen
- Diaphragm Plication For Eventration or Paralysis (A Review of The Literature)Dokument5 SeitenDiaphragm Plication For Eventration or Paralysis (A Review of The Literature)TommyNoch keine Bewertungen
- COPD GuideDokument69 SeitenCOPD GuideEster Elisabeth WoworNoch keine Bewertungen
- CJ C J CJ CJ Cî CJ CJ C C ! "! Cî C Ë # C Ë # CJ$ C C 0 "% C C & C C C Ë Î C "' (C Ëj "ËjDokument105 SeitenCJ C J CJ CJ Cî CJ CJ C C ! "! Cî C Ë # C Ë # CJ$ C C 0 "% C C & C C C Ë Î C "' (C Ëj "ËjShirin Forbes Aquino100% (2)
- SOAP Note Template 3rd Version (Shorter) 2Dokument3 SeitenSOAP Note Template 3rd Version (Shorter) 2phoenix180Noch keine Bewertungen
- Epidemiological and Clinical Features of Pediatric COVID-19: Researcharticle Open AccessDokument7 SeitenEpidemiological and Clinical Features of Pediatric COVID-19: Researcharticle Open AccessAditha Fitrina AndianiNoch keine Bewertungen
- Seminar - Heart FailuerDokument19 SeitenSeminar - Heart Failuermustafalotfy01Noch keine Bewertungen
- Nursing Intervention : Been Experiencing Chest Pains)Dokument3 SeitenNursing Intervention : Been Experiencing Chest Pains)Czynna Dela CruzNoch keine Bewertungen
- Overview of Neonatal Respiratory Distress - Disorders of TransitionDokument14 SeitenOverview of Neonatal Respiratory Distress - Disorders of TransitionAlfredo Junior Delgado PeláezNoch keine Bewertungen
- Heart Failure NCPDokument9 SeitenHeart Failure NCPMiriam EstradaNoch keine Bewertungen
- DR - Shetty Advices For Heart CareDokument19 SeitenDR - Shetty Advices For Heart CarekintelboyNoch keine Bewertungen
- Neonatal Air Leak Syndrome and The Role Of.3Dokument9 SeitenNeonatal Air Leak Syndrome and The Role Of.3Claudia KosztelnikNoch keine Bewertungen
- NURSING CARE PLAN - Lung CancerDokument3 SeitenNURSING CARE PLAN - Lung Cancerderic80% (15)
- Pulmonary Tuberculosis As A Differential Diagnosis of PneumoniaDokument18 SeitenPulmonary Tuberculosis As A Differential Diagnosis of PneumoniaKadek AyuNoch keine Bewertungen
- Care of Adults 25 Cardiovascular ManagementDokument39 SeitenCare of Adults 25 Cardiovascular ManagementGaras AnnaBerniceNoch keine Bewertungen
- Respiratory Assessment and Monitoring 28 Feb 2012 Final PDFDokument85 SeitenRespiratory Assessment and Monitoring 28 Feb 2012 Final PDFRahiman Abd RahimNoch keine Bewertungen
- 3 MAIN B February 23Dokument13 Seiten3 MAIN B February 23Student Access SLMC-IMNoch keine Bewertungen
- Nursing Care Plan - Thoracic EmpyemaDokument4 SeitenNursing Care Plan - Thoracic EmpyemaKasiban MuniandyNoch keine Bewertungen
- Pioneer Nursing College Vadodara: Subject: Child Health Nursing Topic: Observation Report (Nicu)Dokument13 SeitenPioneer Nursing College Vadodara: Subject: Child Health Nursing Topic: Observation Report (Nicu)Kinjal Vasava100% (1)
- Heart Failure by IvsDokument66 SeitenHeart Failure by IvsArianne LasamNoch keine Bewertungen
- Endorsement February 13-14Dokument148 SeitenEndorsement February 13-14denishashery7Noch keine Bewertungen
- Test Bank For Pathophysiology Concepts of Human Disease 1st Edition Matthew Sorenson Lauretta Quinn Diane KleinDokument36 SeitenTest Bank For Pathophysiology Concepts of Human Disease 1st Edition Matthew Sorenson Lauretta Quinn Diane Kleinknobbyettinjn4u4f100% (40)
- TB Nursing CareplanDokument14 SeitenTB Nursing CareplanEstherThompson100% (1)
- Heart FaliurDokument18 SeitenHeart Faliurdp2711Noch keine Bewertungen
- Endobronchial Ultrasound: Dr. Deepak Talwar India's Best PulmonologistDokument3 SeitenEndobronchial Ultrasound: Dr. Deepak Talwar India's Best PulmonologistMetro HospitalNoch keine Bewertungen
- 2021JULYDokument25 Seiten2021JULYNicole VinnikNoch keine Bewertungen
- Nigel Fong's Approaches To Symptoms of Disease v2.1Dokument123 SeitenNigel Fong's Approaches To Symptoms of Disease v2.1Amrit BajwaNoch keine Bewertungen
- Etat Module Kenya For Distance LearnersDokument242 SeitenEtat Module Kenya For Distance Learnersokwadha simion100% (1)
- HAAD ReviewerDokument27 SeitenHAAD Reviewerkimberly timbalNoch keine Bewertungen
- 1 Topic 1 - Differential Diagnosis of Pneumonia in Children. Complications of Pneumonia ... (PDFDrive)Dokument164 Seiten1 Topic 1 - Differential Diagnosis of Pneumonia in Children. Complications of Pneumonia ... (PDFDrive)Dara PitraNoch keine Bewertungen
- Passable 350 Q&aDokument76 SeitenPassable 350 Q&aDavid Yousef100% (1)