Beruflich Dokumente
Kultur Dokumente
5asepsis & Infection Control
Hochgeladen von
Nurse DianneOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
5asepsis & Infection Control
Hochgeladen von
Nurse DianneCopyright:
Verfügbare Formate
ASEPSIS & INFECTION CONTROL
TERMINOLOGIES
Sterilization all microorganisms including their spores are destroyed Disinfection not including the spores (surg instruments, thermometers) Antiseptic inhibit only the growth of the pathogens Bactericidal chemical used to destroy microorganism Bacteriostatic prevents only bacterial multiplication STAGES OF INFECTIOUS PROCESS 1. Incubation Period entry of microorganism on the body up to the onset of the signs & symptoms 2. Prodromal Period onset of the appearance of specific or non-specific signs & symptoms 3. Illness Period positive evidence of sign & symptoms 4. Convalescent Period signs & symptoms subside until the client turn into the normal state
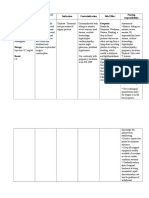
THE CHAIN OF INFECTION
1 Etiologic Agent (microorganism)
2 Reservoir (Source)
6 Susceptible Host (Ill person)
3 Portal of Exit (Sputum, blood, stool)
5 Portal of Entry (Skin GI tract)
4 Modes of Transmission
MODE OF TRANSMISSION
1) Contact Transmission Direct Contact body surface to body surface (bathing, dressing changes, insertion of tubes & catheters) Indirect Contact exposure in a contaminated objects (dressing, needles, surg instruments) 2) Droplet Transmission Exposure of mucous membrane with a distance of 3 feet (coughing, sneezing, talking) 3) Airborne Transmission Microorganism are suspended in air deposited in the skin TYPES OF IMMUNIZATION 1. Active Immunization antibodies produced by own body a. Natural presence of active infection of the body Lifelong immunity Recovery from mumps, chicken pox b. Passive vaccines or toxoids which administer to stimulate antibody reaction for a long time which can be inhaled or
requires booster
TT, OPV
2. Passive Immunization produced by animals a. Natural mother to her baby
breast feeding
b. Passive
immune serum from animals or human
TIGH
BREAKING THE CHAIN OF INFECTION
I. II. III. IV. V.
Handwashing Cleaning, disinfection, sterilization Used of barriers Isolation technique Surgical asepsis
Based handscrub are effective preparations for removing microorganism Before & after client care should wash hands Adequate friction and thoroughness of surfaced cleansed Medical Asepsis - holdings hands lower the elbows Clean under finger nails Closed the faucet by paper towel Wear gloves during client care especially the skin is abraded
I. HANDWASHING
II. CLEANING, DISINFECTION, STERILIZATION
Any item introduced into sterile tissues or vascular tissues such as surgical instruments cardiac & urinary catheters, vaginal speculum, implants, IV fluids & needles must be STERILE
METHODS OF STERILIZATION a. Steam Sterilization Autoclaving using steam under pressure Non toxic, inexpensive, sporicidal, & able to penetrate fabrics rapidly Color indicator strips change in color , indicates sterilization occured b. Gas Sterilization Ethylene Oxide is colorless gas that penetrate plastic & rubber cotton Expensive & requires 2-5 hrs Ethylene Oxide is toxic to humans c. Radiations deeply into the object d. Chemicals effective disinfectant Chlorine is used e. Boiling Least expensive for used in homes 15 mins TYPES OF DISINFECTION 1) Concurrent Disinfection Ongoing practices during the care of the client 2) Terminal Disinfection After the illness is no longer communicable
USE OF BARRIERS
(PERSONAL PROTECTION EQUIPMENT PPE)
Masks Caps & shoe coverings Gloves Private rooms Waterproof disposable bags for linen & trash Labelling & bagging of contaminated equipment & specimen Control of airflow into the sterile areas & out of contaminated areas Goggles or face shield
MASKS Should fit tightly to the face, covering nose and mouth Wet mask considered contaminated 1 micromilimeter small of organism can passed GOWNS
Used it only once When wet changed it CAPS & SHOE COVERINGS It shield body parts from accidental exposure to contaminated body secretion GLOVES Discard between clients & changed when torn & grossly soiled Should not be washed & used PRIVATE ROOMS Clients gowns & dressing should be changed before leaving the room & wear barriers EQUIPMENT & REFUSE HANDLING Linens soiled by any body fluid should be placed in impervious (waterproof) bag before it removes at the client bedsides DOUBLE BAGGING when outside of the bag becomes contaminated, placed another bag in other bag
V.
ISOLATION TECHNIQUE
Classified as Standard Precautions, Transmission Based Precautions & Protective Isolation STANDARD PRECAUATIONS Prevent transmission of bloodborne & moist body substance Wear clean gloves when touching Any secretions & excretions, any body fluids Mucous membranes Non-intact skin Perform handwashing immediately When there is direct contact with any secretions & excretions, any body fluids After removing gloves Between patient contacts Wear a mask, eye protection & face shield during procedure & patient care Wear a cover gown during procedure & patient care Clean & reprocess all equipment before reused by other clients Discard all single used items immediately Prevent injuries from sharp objects (needles, scalpels) Never remove, recap, bend or break used needles Never point needle toward body parts Used ONE- HANDED SCOOP METHOD on special syringes for enclosing a needle TRANSMISSION BASED PRECAUTIONS Airborne Precautions small particle droplets (TB varicella measles) Client should in a private, negative airflow room Caregivers should wear mask Clients wear mask when transported out of the room
Droplet Precautions larger-particle droplet (influenza, diphtheria, rubella, pneumonia
In private room Wear mask 3 feet away from the client Contact Precautions by hand or skin to skin contact (shigella, impetigo) In private room COHABITATION client who has a roommate with a same disease Before entering the room, wear gloves Remove gloves before leaving the room PROTECTIVE ISOLATION People whose resistance to infection/body defenses are lowered or compromise In private room Handwashing by client, family, & caregivers Restrict visitors Persons who suspected an infection are not allowed to visit the client No fresh fruits, vegetables, raw foods, fresh flowers or potted plants Cooked foods or canned fruits are allowed
V.
SURGICAL ASEPSIS
surgical procedures procedures that invade the blood stream IM injections Insertion of tubes, catheters
PRINCIPLES OF SURGICAL ASEPSIS 1. Moisture causes contamination Prevent splashing of liquids in sterile field Wet objects are placed in sterile basin Microorganisms more easily travel in moist environment 2. Never assume that an object is sterile Ensure that it is labelled as sterile Check the integrity Verify the expiration date Whenever in doubt of the sterility of an object, consider it as unsterile 3. Always face the sterile field Objects that out of the line of vision are considered contaminated 4. Sterile articles may touch only sterile articles or if surface they are to maintain their sterility Objects used in cleaning the skin (swab) must be used once 5. Sterile equipment or areas must be kept above the waist & top of the sterile field Drapes hanging over the edge of the table are contaminated Waist level is the limit of good visual field 6. Prevent unnecessary traffic & air currents around the sterile area Closed doors Unfold drapes or wrappers slowly
Do not reach across sterile fields 7. Open unused sterile articles are no longer sterile after the procedure Once protective wrapping have been removed the articles are contaminated Liquids open during the procedure that remain in their original container are contaminated 8. Person who is considered sterile who becomes contaminated must reestablished sterility 9. Surgical technique is a team effort STERILE CONSCIENCE best to achieved sterile technique To enhance everyones sterile technique, review the procedures & infection control surveillance
Related Nursing Skills: PERFORMING STERILE PROCEDURES
SURGICAL HAND SCRUB PURPOSE: Remove as many microorganism from the hands as possible before the sterile procedure EQUIPMENT: Sink with knee or foot controls (ideally) Antimicrobial soap Surgical scrub brush Plastic nail stick or sterile nail cleaner (ideally) Sterile towel for drying STEPS: 1) 2) 3) 4) Be sure fingernails are short & healthy. Nail polish should be removed Remove rings. Apply surgical shoe covers, cap, face mask & protective eye wear Wash & rinse hands for initial wash Open disposable brush impregnated with antimicrobial soap, adjust water temperature to warm using knee or foot control lever.
Warm water decreases drying of hands 5) Wet hands & arms. Keep hands above the elbows. 6) Use nail stick or cleaner to clean under nails of both hands 7) Wet scrub brush or apply antimicrobial soap if not already impregnated in the brush 8) Anatomic Timed Scrub. Starting with finger tips, scrub each anatomic area (nails, fingers each side & web space, palmar surface, dorsal surface & forearm) for around 5 mins. Scrub vigorously using vertical strokes. repeat with other hand. 9) Counted Brush Stroke Method. Starting with finger, scrub each anatomic area (same as in step no. 8) for the designated number of strokes according to agency policy. Scrub vigorously using vertical strokes 10) Rinse hands thoroughly under warm running water, holding hands upward. These allow water to drain towards the flexed elbows. 11) Keep hands held upward to allow water to drip from the hands to the elbow. Dry hands with sterile towel
APPLYING & REMOVING STERILE GLOVES PURPOSE: Prevent transfer of microorganisms from hands to sterile objects or open wounds. EQUIPMENT: Packaged sterile gloves in correct size Flat working surface STEP: APPLYING GLOVES Wash hands. Peel of outside wrapper as directed by manufacturer (peel sides part) Lay inner package on clean, flat surface about waist level. Open wrapper from the outside, keeping gloves on inside surface Grasp first glove by inside edge of cuff with thumb & first 2 fingers of the dominant hand. Hold hands above waist; insert non-dominant hand into glove. Adjust fingers inside glove after both gloves are on. Slip glove hand ($ fingers with thumb up) underneath second gloved cuff and pull over dominant hand Put gloves on the nondominant hand first, then on the nondominant hand Keeping hands above waist, adjust above glove fit, touching only sterile areas REMOVING GLOVES Wash hands With dominant hand, grasp outer surface of nondominant glove adjust below thumb. Peel off glove inside out without touching exposed wrist Place ungloved hand under thumb side of second cuff & peel of toward the fingers holding first gloved inside second glove. Discard into appropriate receptacle Wash hands DONNING A STERILE GOWN & CLOSED GLOVING Purpose: to apply attire necessary to safely carry out sterile procedures usually in the OR & DR EQUIPMENT: Sterile gown Sterile gloves Mayo stand or flat surface area above waist level STEPS: 1) Wear shoe covers, cap that covers all hair, face mask & protective wear (ideally) & perform the surgical scrub DONNING A STERILE 2) Grasp folded sterile gown at the neckline & step away from the sterile field. Allow gown to gently unfold, being careful that it does not touch the floor. The inside of the gown is toward the user. 3) Holding the arms & shoulder level, grasp the sterile gown just below the neckband near the shoulders A slide arms until the fingers are & the end of the cuffs but not through the cuffs. 4) Have someone to tie back of the gown, taking caret the ties are touched & not the sides or front of the gown.
The front of the gown from shoulder to the table level is sterile & the sleeves are considered sterile from 2 inches above the elbow to the wrist.
CLOSED GLOVING With fingers still within the cuff of the gown, open the inner sterile glove package & pick up the first glove by the cuff, using the nondominant hand. Position the cuff over the cuff of the gown so the fingers are in alignment, & stretch the entire glove over the cuff of the gown, being carefully not to touch its edge. Fingers remain with the cuff of the gown Work finger into the glove & pull the glove up over the wrist with the nondominant hand that still remains within the cuff of the gown Use the sterile gloved hand to pick up the second glove, placing it over the cuff of the gown of the other hand & repeat the glove application Adjust glove for comfort & fit, taking care to keep hands above waist level & all times. DONNING & REMOVING GLOVES, MASK, GOWNS & EYE WEAR For sterile procedures on a general nursing division, the nurse may wear surgical mask and gloves without the cap. Eye wear is ideally worn if there is risk of fluid or blood splashing into the nurses eye. First applies a clean cap, mask eye wear, & shoe cover In removing: gloves, mask, gown, eye wear, cap & shoe cover PREPARING & MAINTAINING A STERILE FIELD PURPOSE: to create an environment that helps ensure the sterility of supplies & equipment & prevent of microorganisms during sterile procedure. EQUIPMENT: Flat work surface Sterile drape Sterile supplies (sterile gauze, sterile basin, solutions, scissors, forceps) Packaged sterile gloves STEPS: SPECIAL CONSIDERATIONS Wash hands Inspect all sterile packages for package integrity, contamination, or moisture. Never turn back on the sterile field or lower hands below the level of the field during the entire procedure. OPENING A STERILE DRAPE Remove the sterile drape from the outer wrapper & place the inner drape in the surface of the work surface, at or above waist level with the outer flap facing away from you. Touching the outside of the flap, reach around (rather than over) the sterile field to open the flap away from you. open the side flaps in the same manner, using the right hand for the right flap & left hand for the left flap Open the innermost flap that faces you, being careful that it does not touch your clothing or any object. ADDING STERILE SUPPLIES TO THE FIELD
1) 2) 3)
4) 5) 6) 7)
8)
open unsealed edge of prepackaged sterile supplies, taking care not to touch the supplies with the hands 9) Hold supplies 10 to 12 inches above the field and allow them to fall to middle of the sterile field. 10) Wrapped sterile supplies are added by holding the sterile objects with one hand and unwrapping the flaps with the flaps with the other hand. Carefully drop the object onto the sterile field. POURING SOLUTIONS TO A STERILE FIELD 11) Check the label and expiration date of the solution. Note any signs of contamination. 12) Remove cap & place it with the inside facing up on a flat surface. do not touch inside of cap or rim of bottle 13) Hold bottle 6 inches above receptacle on the sterile field & pour it slowly to avoid spills 14) Recap the solution bottle, place it outside the sterile field label it with date 7 time of opening if the solution is to be reused 15) Add any additional supplies & don sterile gloves just prior to beginning the procedure helps to ensure sterility. CARE OF THE STERILE PICK-UP FORCEPS PURPOSE: To transfer sterile articles & maintain sterility of these articles & the sterile field. EQUIPMENT: Sterile forceps in sterile bottle with germicidal/disinfectant solution STEPS: 1) The prongs of the sterile forceps should be fully immersed in disinfectant solution 2) Sterile forceps are always held above & in front of the waist, within the vision of the nurse 3) The tips of the forceps are always considered sterile & need to be held down 4) The handles of the forceps are considered contaminated except when they are undergone in sterilization 5) Use the thumb & middle fingers when lifting the forceps from the container. From the tip should not touch the rim or any part of the container not directly in contact with the disinfectant 6) Tap the handle of the forceps with index finger to remove excess from the tip, ouside the sterile field. 7) When removing sterile items from a container, the tips of the forceps and/or the item should be kept away from the edges of the container or disposable wrapper 8) Return the forceps to the container, without touching the tips to the rim or part of the container not immersed in disinfectant.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- ShouldiceDokument16 SeitenShouldiceAbdullah AhmedNoch keine Bewertungen
- OncologyDokument3 SeitenOncologyNurse DianneNoch keine Bewertungen
- Integumentary SystemDokument2 SeitenIntegumentary SystemNurse DianneNoch keine Bewertungen
- Hematology SystemDokument9 SeitenHematology SystemNurse DianneNoch keine Bewertungen
- Neuro SystemDokument22 SeitenNeuro SystemNurse DianneNoch keine Bewertungen
- Gut SystemDokument8 SeitenGut SystemNurse DianneNoch keine Bewertungen
- E. A. D. A.: Gastrointestinal SystemDokument9 SeitenE. A. D. A.: Gastrointestinal SystemDominic ReambonanzaNoch keine Bewertungen
- Endo SystemDokument21 SeitenEndo SystemNurse DianneNoch keine Bewertungen
- 6sterss Adaptation, Homeostasis PHYSIOLOGIC RESPONSESDokument6 Seiten6sterss Adaptation, Homeostasis PHYSIOLOGIC RESPONSESNurse DianneNoch keine Bewertungen
- Circulatory SystemDokument9 SeitenCirculatory SystemNurse DianneNoch keine Bewertungen
- NutritionDokument1 SeiteNutritionNurse DianneNoch keine Bewertungen
- 4concepts of Health and IllnessDokument2 Seiten4concepts of Health and IllnessNurse DianneNoch keine Bewertungen
- 3concepts of Man & His Basic Human NeedsDokument2 Seiten3concepts of Man & His Basic Human NeedsNurse DianneNoch keine Bewertungen
- 2nursing Leaders in The PhilippinesDokument1 Seite2nursing Leaders in The PhilippinesNurse DianneNoch keine Bewertungen
- 1nursing Basic TheoriesDokument3 Seiten1nursing Basic TheoriesNurse DianneNoch keine Bewertungen
- Hepatobiliary DisorderDokument19 SeitenHepatobiliary DisorderNurse DianneNoch keine Bewertungen
- Respiratory DiseaseDokument27 SeitenRespiratory Diseaseعبدالسلام الأسمرNoch keine Bewertungen
- Women S Health MidtermDokument30 SeitenWomen S Health MidtermKatarzyna CiesielskaNoch keine Bewertungen
- Disentri AmubaDokument8 SeitenDisentri AmubaVivi DeviyanaNoch keine Bewertungen
- Difference Between Serum and PlasmaDokument2 SeitenDifference Between Serum and PlasmaCynthia Adeline SNoch keine Bewertungen
- Maternal and Child HealthDokument60 SeitenMaternal and Child HealthStar AcademyNoch keine Bewertungen
- Test Bank For Physical Examination and Health Assessment 1st Canadian Edition by JarvisDokument10 SeitenTest Bank For Physical Examination and Health Assessment 1st Canadian Edition by JarvisThomas White100% (22)
- Australian and New Zealand College of Veterinary Scientists: Fellowship ExaminationDokument11 SeitenAustralian and New Zealand College of Veterinary Scientists: Fellowship Examinationabazanhasan6705Noch keine Bewertungen
- 2) Megaloblastic AnemiaDokument17 Seiten2) Megaloblastic AnemiaAndrea Aprilia100% (1)
- Medical Image Analysis - Overview - NewDokument11 SeitenMedical Image Analysis - Overview - Newedi pNoch keine Bewertungen
- Abiraterone Acetate Plus Prednisone Versus Placebo Abiratetone LancetDokument9 SeitenAbiraterone Acetate Plus Prednisone Versus Placebo Abiratetone LancetMahesh TamhaneNoch keine Bewertungen
- IsoketDokument2 SeitenIsoketJaessa FelicianoNoch keine Bewertungen
- Gastric GavageDokument3 SeitenGastric GavageRico Delgado of WorldbexNoch keine Bewertungen
- D Dimer Test in VTEDokument35 SeitenD Dimer Test in VTEscribmedNoch keine Bewertungen
- Managing Multiple Comorbidities - UpToDateDokument15 SeitenManaging Multiple Comorbidities - UpToDateGaby GarcésNoch keine Bewertungen
- Interstitial Lung Diseases Radiology 22222Dokument26 SeitenInterstitial Lung Diseases Radiology 22222Daniel AshooriNoch keine Bewertungen
- HEPA Filter Inthe Covid 19 Era-Function and EficacyDokument3 SeitenHEPA Filter Inthe Covid 19 Era-Function and EficacynoeNoch keine Bewertungen
- Hospital Infections PDFDokument794 SeitenHospital Infections PDFJOSEPH APPIAHNoch keine Bewertungen
- ENDO Buku Ekatalog Disposable Fix PDFDokument12 SeitenENDO Buku Ekatalog Disposable Fix PDFHanggar PutraNoch keine Bewertungen
- Vasofix SafetyDokument6 SeitenVasofix Safetydex99Noch keine Bewertungen
- Drug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaiseDokument3 SeitenDrug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaisekristel_nicole18yahoNoch keine Bewertungen
- WHO - HQ - Reports G2 PROD EXT TBCountryProfileDokument1 SeiteWHO - HQ - Reports G2 PROD EXT TBCountryProfileAngelo Santos EstrellaNoch keine Bewertungen
- Karya - KTI - Poltekkes Kemenkes SurakartaDokument11 SeitenKarya - KTI - Poltekkes Kemenkes Surakartasheenazz •Noch keine Bewertungen
- Case Study UrtiDokument9 SeitenCase Study UrtiRonica GonzagaNoch keine Bewertungen
- Makalah Leigh Disease by Boys KDokument6 SeitenMakalah Leigh Disease by Boys KAzizul HakimNoch keine Bewertungen
- Case Presentation: - Vuppu BhavaniDokument53 SeitenCase Presentation: - Vuppu BhavaniLohith Kumar MenchuNoch keine Bewertungen
- Burn Management by Tajuu Seid: Surgical WardDokument33 SeitenBurn Management by Tajuu Seid: Surgical Wardelias adugnaNoch keine Bewertungen
- The Prevention and Cure Effects of Aspirin Eugenol Ester On Hyperlipidemia and Its MetabonomicsDokument108 SeitenThe Prevention and Cure Effects of Aspirin Eugenol Ester On Hyperlipidemia and Its MetabonomicsKavisa GhoshNoch keine Bewertungen
- Shock RosenDokument10 SeitenShock RosenJuan GallegoNoch keine Bewertungen
- Clinical EnzymologyDokument23 SeitenClinical EnzymologyKishore KaranNoch keine Bewertungen