Beruflich Dokumente
Kultur Dokumente
Musculoskeletal Trauma
Hochgeladen von
Stephanie TalbotOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Musculoskeletal Trauma
Hochgeladen von
Stephanie TalbotCopyright:
Verfügbare Formate
MUSCULOSKELETAL TRAUMA A. SPRAINS & STRAINS- excessive stretching or twisting of muscle (strain) or tendon (sprain). 1.
Can be 1-3rd degree, s/s edema, pain, contusion, decreased fxn i. Tx: stop activity & rest limb, ice 24-48hrs, apply compression bandage (decrease swelling0, NSAIDS, warm after 24-48hrs & encourage limb use if cast, splint or tape. 2nd-3rd degree require immobilization through cast, splint or bandage 2. Teach stretch & warm-up, strengthening, balance & endurance exercises B. FRACTURES- break in continuity of bone 1. Can be complete or incomplete, open(compound)-bone breaks skin or closed(simple)bone doesnt break skin i. Immobilize limb in position found if suspect fracture Pelvis fracture- handle w/ care as to no damage internal organs, check bowel, urinary & distal neurovascular fxn, turn if D.O, use trapeze for back careNO WEIGHT BEARING TILL HEALED. Long bone- fat embolism huge risk, skeletal traction 8-12wks, encourage ROM unaffected side, D.O for affected side, once bone union, cast or hip spica applied Hip fracture- assoc w/ osteoporosis, bucks traction 72hrs, if femoral neck broken-prosthesis, if extracapsulare fracturepins, nails, plates 2. Phases bone healing: i. Hematoma formation (24-72hrs)granulation hematoma (3dys-2wks)callous formation & ossification- clinical union occurs here(2dys-6wks)bone consolidation & remodelling (up to 1yr) 3. Complications of fractures: i. Infection-require debridement, jet-pulsed irrigation, antibiotics. Most common=Osteomyelitis ii. Compartment syndrome- compromises circulation..EMERGENCY...assess 6 Ps: pain, paresthesia, pallor, pulselessness, paralysis, pressure. TX=fasciotomy.
*DO NOT ELEVATE EXTREMITY ABOVE LEVEL HEART. Give IV fluids, diuretics, low dose dopamine to enhance renal perfusion iii. Hypovolemic shock- if fracture damages blood vessel iv. Venous thrombosis-tx= antiembolism stockings, dorsiflexion/plantar flexion fingers & toes, ROM unaffected side, LMWH v. Fat embolism syndrome- s/s: change LOC, tachycardia, tachypnea, chest pain HTN, *petechiae around neck, axilla, chest wall tx=immobilization, fluid restriction, encourage cough deep bx C. FRACTURE TX: GOALS: re-alignment, immobilization to maintain alignment, restoration fxn 1. In emergency assess respiratory distress, bleeding & head injuryif these not present padres fractureemergency fracture care i. Check fracture, control bleeding, check VS, place pt. Supine, keep warm, immobilize fracture, use sterile gauze for open fracture, check neurovascular status 2. Re-alignment: i. Closed reduction- traction & counter traction applied manually to re-align bone Bucks traction- application Velcro boot w/ weight @ end to decrease muscle spasmscasts, external d=fixation, splints & orthosis (braces) used to immobilize ii. Open reduction- correction bone alignment through surgery, includes internal fixation w/ plates, pins, rods or nailstraction & counter traction used & skin traction used 48-72 hrs until skeletal traction 9weight or pin in bone to align) facilitates early ambulation. *check neurovascular status, complications & groin. 3. NSG INTERVENTIONS TRACTION- maintains balance between traction pull & counter traction force. *need D.O remove weight i. Check skin q8hrs for inflammation ii. Remove belt/boot skin traction q8hrs iii. Inspect pts of entry pins & wires q8 iv. Check traction equipment to ensure working properly q8-12hrs v. Verify weights-replace if not corrects
D. AMPUTATION- removal of body part due to dx or trauma 1. For traumatic amputation, ensure patent airway, put pressure on area & cover w/ dry cloth, evaluate above heart to decrease bleed. 2. For fingers & toescover dry cloth, place sealed plastic bag on ice water 3. Big toe amputation affects push-off walking 4. NSG TX: i. Check tissue perfusionskin flap pin 7 warm, check proximal pulses for strength & compare ii. Manage pain residual & phantom limb Phantompropanolol for dull, burning pain, antiepileptics carbamazepine(Tegretol) or Gabapentin(neurontin0 for knife-like pain, antispasmodics baclofen(lioresal) for muscle spasms iii. Complementary & alternative therapy ex. TENS iv. Prevent infection- broad spectrum antibiotics- initial pressure dressing & drains removed by surgeon 48-72hrs, assess inflammation, change dressing daily until sutures removed v. Promote mobility- teach ROM to prevent infection contraction hip, place trapeze above bed to help strengthen upper extremities vi. Assist pt. Into prone position q3-4hrs for 20-30min, instruct pull residual lib close to other leg & contract gluts, teach those BKA push residual limb down toward bed while supporting it on a pillow, do not elevate residual limb on pillow while supinekeep flat to prevent flexion contractions vii. Prepare for prosthetic- coordinate w/ prosthetis-orthotis, instruct bring sturdy shoes E. HIP ARTHROPLASTY- hip reconstruction or replacement 1. Leg abduction maintained (wedge between legs) while moving in bed, hips cant be lower than knees F. KNEE ARTHROPLASTY- isometric quadriceps sitting begins first day.
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Prioritization, DelegationDokument5 SeitenPrioritization, DelegationStephanie Talbot100% (1)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- MCQ Examination For Year 1 Residents in Orthopaedics SurgeryDokument15 SeitenMCQ Examination For Year 1 Residents in Orthopaedics SurgeryTefera Letebo100% (2)
- ORP Handout English External Fixation NlogoDokument9 SeitenORP Handout English External Fixation NlogotripodegrandeNoch keine Bewertungen
- Principles of DelegationDokument16 SeitenPrinciples of DelegationStephanie Talbot100% (1)
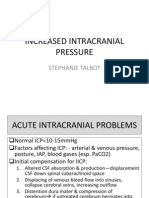
- Increased Intracranial PressureDokument13 SeitenIncreased Intracranial PressureStephanie Talbot100% (1)
- Depressed Fracture: Modul Bedah, July 2021Dokument31 SeitenDepressed Fracture: Modul Bedah, July 2021Muhammad MuhidNoch keine Bewertungen
- Daily OrganizationDokument4 SeitenDaily OrganizationStephanie TalbotNoch keine Bewertungen
- TPN OutlineDokument1 SeiteTPN OutlineStephanie TalbotNoch keine Bewertungen
- Reproductive System For Female OutlineDokument2 SeitenReproductive System For Female OutlineStephanie Talbot100% (1)
- CardiacDokument43 SeitenCardiacStephanie TalbotNoch keine Bewertungen
- Reproductive CancersDokument2 SeitenReproductive CancersStephanie TalbotNoch keine Bewertungen
- BRY's Biology, 1st SemesterDokument93 SeitenBRY's Biology, 1st SemesterStephanie TalbotNoch keine Bewertungen
- Structural Defects Upper GIDokument15 SeitenStructural Defects Upper GIStephanie TalbotNoch keine Bewertungen
- Module 10.3: Children Who Have Alterations in Tissue PerfusionDokument23 SeitenModule 10.3: Children Who Have Alterations in Tissue PerfusionStephanie TalbotNoch keine Bewertungen
- STD'S BacterialDokument2 SeitenSTD'S BacterialStephanie TalbotNoch keine Bewertungen
- Ulcerative Colitis OutlineDokument3 SeitenUlcerative Colitis OutlineStephanie TalbotNoch keine Bewertungen
- OBESITY OutlineDokument2 SeitenOBESITY OutlineStephanie TalbotNoch keine Bewertungen
- PUD OutlineDokument4 SeitenPUD OutlineStephanie TalbotNoch keine Bewertungen
- Module 7.3 Drug ChartDokument1 SeiteModule 7.3 Drug ChartStephanie Talbot100% (1)
- Musculoskeletal System OutlineDokument3 SeitenMusculoskeletal System OutlineStephanie TalbotNoch keine Bewertungen
- Module 7.2 Drug ChartDokument1 SeiteModule 7.2 Drug ChartStephanie TalbotNoch keine Bewertungen
- Neurovascular AssessmentDokument5 SeitenNeurovascular AssessmentStephanie TalbotNoch keine Bewertungen
- Module 7.1 Drug ChartDokument2 SeitenModule 7.1 Drug ChartStephanie TalbotNoch keine Bewertungen
- Laboratory Tests GI SystemDokument1 SeiteLaboratory Tests GI SystemStephanie TalbotNoch keine Bewertungen
- Hepatitis OutlineDokument3 SeitenHepatitis OutlineStephanie TalbotNoch keine Bewertungen
- Intestinal Obstruction OutlineDokument2 SeitenIntestinal Obstruction OutlineStephanie Talbot100% (1)
- Diverticulosis OutlineDokument3 SeitenDiverticulosis OutlineStephanie TalbotNoch keine Bewertungen
- Gynocological ProblemsDokument3 SeitenGynocological ProblemsStephanie TalbotNoch keine Bewertungen
- Cholecystitis Cholelithiasis OutlineDokument2 SeitenCholecystitis Cholelithiasis OutlineStephanie TalbotNoch keine Bewertungen
- Hiatal Hernia OutlineDokument2 SeitenHiatal Hernia OutlineStephanie TalbotNoch keine Bewertungen
- Crohns OutlineDokument4 SeitenCrohns OutlineStephanie TalbotNoch keine Bewertungen
- Cirrhosis OutlineDokument3 SeitenCirrhosis OutlineStephanie TalbotNoch keine Bewertungen
- Portfolio in OrthopedicDokument72 SeitenPortfolio in OrthopedicAlex Delos SantosNoch keine Bewertungen
- Sic Fracture AgainDokument5 SeitenSic Fracture AgainEzra Miguel DarundayNoch keine Bewertungen
- Inflammation and RepairDokument34 SeitenInflammation and Repairanshum guptaNoch keine Bewertungen
- Functional Outcome of Surgical Management of Malleolar Fractgures of The Anklejoint Using Baird Jackson Score ScoringDokument5 SeitenFunctional Outcome of Surgical Management of Malleolar Fractgures of The Anklejoint Using Baird Jackson Score ScoringAxell C MtzNoch keine Bewertungen
- Head Injury .Dokument26 SeitenHead Injury .Lenjun100% (4)
- Management of The Floating Knee.Dokument8 SeitenManagement of The Floating Knee.barbara liuva chia policarpoNoch keine Bewertungen
- Is Socrates Dying PDFDokument3 SeitenIs Socrates Dying PDFPraveen KNoch keine Bewertungen
- Skeletal Trauma - Basic Science, Management, and Reconstruction, 2-Volume Set, 5E (Browner) (2015)Dokument2.807 SeitenSkeletal Trauma - Basic Science, Management, and Reconstruction, 2-Volume Set, 5E (Browner) (2015)paula catanaNoch keine Bewertungen
- System Brochure - Foot Plating System PDFDokument8 SeitenSystem Brochure - Foot Plating System PDFAngulo HernandezNoch keine Bewertungen
- Tulipan 2018Dokument7 SeitenTulipan 2018redityoNoch keine Bewertungen
- Arvin Noscal Pediatric FemurDokument84 SeitenArvin Noscal Pediatric FemuranoscalNoch keine Bewertungen
- Fractures of The Humerus in The Neonatal PeriodDokument4 SeitenFractures of The Humerus in The Neonatal PeriodSandroNoch keine Bewertungen
- Fractures and Soft Tissue InjuriesDokument7 SeitenFractures and Soft Tissue InjuriesShirlyn GeorgeNoch keine Bewertungen
- Treatment Priciples in The Management of Open FractureDokument23 SeitenTreatment Priciples in The Management of Open FractureNunks FiryaniNoch keine Bewertungen
- Leibinger Stryker Hand or Foot Set PDFDokument40 SeitenLeibinger Stryker Hand or Foot Set PDFJacob Dougherty100% (1)
- Acumed Case Study EN AP3 Dual Plating For Posterior Pilon Fractures FNA70 08 ADokument4 SeitenAcumed Case Study EN AP3 Dual Plating For Posterior Pilon Fractures FNA70 08 AmayankNoch keine Bewertungen
- Cuz End of Term 3 MCQ Surgery1 Sept 2020Dokument14 SeitenCuz End of Term 3 MCQ Surgery1 Sept 2020MustafaNoch keine Bewertungen
- Pathology Unit Plan on Inflammation, Wounds, and BonesDokument15 SeitenPathology Unit Plan on Inflammation, Wounds, and BonesSumant Sharma VishwakarmavansiNoch keine Bewertungen
- Femoral Shaft Fractures in Children - UpToDateDokument5 SeitenFemoral Shaft Fractures in Children - UpToDatenogarithNoch keine Bewertungen
- "Approwed" On The Meeting of The Department of Surgical Dentistry and Maxillofacial SurgeryDokument10 Seiten"Approwed" On The Meeting of The Department of Surgical Dentistry and Maxillofacial SurgeryMadeline WanhartNoch keine Bewertungen
- A Fracture of The Distal Radius or UlnaDokument3 SeitenA Fracture of The Distal Radius or UlnaSweetie StarNoch keine Bewertungen
- Module Description. Pathology of Musculosceletal SystemDokument52 SeitenModule Description. Pathology of Musculosceletal SystemAlberto MayorgaNoch keine Bewertungen
- Stress Reaction and Fractures - StatPearls - NCBI BookshelfDokument6 SeitenStress Reaction and Fractures - StatPearls - NCBI BookshelfAlejandro OrduzNoch keine Bewertungen
- Indigenous splint fixes cow's tibiaDokument2 SeitenIndigenous splint fixes cow's tibiavetarifNoch keine Bewertungen
- Bone Fracture Grp3Dokument12 SeitenBone Fracture Grp3Marjian BaruaNoch keine Bewertungen
- Comminuted Quadrilateral Plate Fracture Fixation Through The Iliofemoral ApproachDokument8 SeitenComminuted Quadrilateral Plate Fracture Fixation Through The Iliofemoral ApproachdrarunlalNoch keine Bewertungen
- 2024 USFSSTG001V4 US DeLorean STG Rev1aDokument70 Seiten2024 USFSSTG001V4 US DeLorean STG Rev1aNathaly GuevaraNoch keine Bewertungen