Beruflich Dokumente
Kultur Dokumente
06 Inguinal Hernia Srs
Hochgeladen von
lowhillOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
06 Inguinal Hernia Srs
Hochgeladen von
lowhillCopyright:
Verfügbare Formate
1|Page
A CRITICAL APPRAISAL OF SURGICAL TECHNIQUES IN GROIN HERNIA REPAIR
1. DEFINITION OF HERNIA 2. HISTORY AND EVOLUTION OF TECHNIQUES 3. SURGICAL TECHNIQUES 3.1. TISSUE REPAIR 3.1.1 BASSINI REPAIR 3.1.2 SHOULDICE REPAIR 3.1.3 FEMORAL HERNIA REPAIR 3.1.3.1 FEMORAL APPROACH 3.1.3.2 INGUINAL APPROACH 3.1.3.3 EXTRAPERITONEAL APPROACH
3.2 TENSION FREE (MESH) REPAIR 3.2.1 OPEN REPAIR 3.2.1.1.STOPPA REPAIR 3.2.1.2 LICHTENSTEIN REPAIR (OPEN ANTERIOR) 3.2.1.3 KUGEL PATCH (OPEN POSTERIOR) 3.2.1.4 PERFIX PLUG 3.2.1.5 PROLENE HERNIA REPAIR SYSTEM 3.2.2 LAPAROSCOPIC REPAIR
4.CRITICAL APPRAISAL 5.CONCLUSION 6.BIBLIOGRAPHY
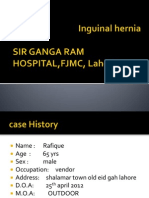
1.DEFINITION(1) Inguinal hernia is defined as protrusion of intrabdominal content or preperitoneal fat through a hernia defect irrespective of whether this is congenital. Recurrent Inguinal Hernia is a swelling due to defect in the inguinal region where a previous operation for hernia was carried out.
2|Page
HISTORY OF HERNIA REPAIR (2) Bassini from Italy is credited with laying the foundation for modern hernia repair. His technique was revisited by Shouldice and incorporated into what became one of the most successful tissue repairs in the history of hernia surgery. Posterior preperitoneal approach by Cheatle and and unilateral pararectal approach by Mc Evdy later popularised by Nyhus were the other remarkable developments in this era. The credit for the introduction of mesh should be attributed to Usher. He initially used polyethylene and later substituted it with polypropylene mesh. Rives, Stopa and Wantz tredded along his path and made significant contributions in this area of surgery. While Newman was first to use mesh for anterior repair but Lichtenstein popularised this approach. Gilbert introduced the Prolene Hernia Repair system based on the inputs from Usher. The later part of 20th century also saw the development of laparoscopic skills being applied to this entity. Laparoscopic surgery for hernia repair was first introduced by Ger and at present it has got a good share of followers. In the year 1979, an enthusiastic French Surgeon Chevrel founded the first hernia society which later developed into the European Hernia Society and later with its American counterpart American Hernia Society brought out the journal HERNIA. Hernia is presently recognised as a systemic collagen illness. Consequently patients should be evaluated from this perspective with an aim to identify other co-existing problems stemming from the same pathology .On the other side antidotes are being looked at to treat this illness. In all it righteousness herniology seems to be destined to be a subspecialty in surgery. 3. SURGICAL APPROACH 3.1.1 BASSINIS OPERATION Bassini of Padua, Italy was the first to understand and develop an anatomical approach this problem. The technique was to enter the preperitoneal space by incising the internal oblique, transversus abdominis and transversalis fascia. This was followed by high ligation of the sac and later mass suturing to the inguinal ligament. In the hands of Bassini the recurrence rate was an impressive 2.7%.(2)However this was not the case with the general experience. 3.1.2 SHOULDICE TECHNIQUE (3) Shouldice technique is actually a modification of the Bassinis repair based on the very same principles of dissection. The two steps that need to be highlighted in this technique are resection of the cremaster, and opening of the posterior wall of the canal. This enables the operator to visualise the existence of any indirect hernia which is a major cause of recurrence. Repair is then carried out in four layers. Originally steel sutures were placed in a continuous manner. Present trend is to use continuous non absorbable sutures with an aim to evenly distribute the tension 3.1.3.FEMORAL HERNIA REPAIR (4)
3|Page
3.1.3.1 FEMORAL APPROACH Socin was the first to describe this method. Gilbert introduced mesh plugs and later Rutkow and Robbins introduced Perfix plug( preshaped mesh plugs) which can be used to repair femoral and inguinal hernias. 3.1.3.2 INGUINAL APPROACH Lotheissen approximated the conjoint tendon to the Coopers ligament. McVays repair was one of the most popular. Chester McVay used a supra inguinal incision to access the preperitoneal space The transversalis fascia is opened and the repair is undertaken by approximating the conjoint tendon to the Coopers ligament. This is often accompanied by placing a relaxing incision on the rectus sheath which tends to avoid tension in the repair. 3.1.3.3EXTRAPERITONEAL APPROACH Nyhus used a transverse incision placed above the pubic symphysis to gain access to the preperitoneal space for exposing the femoral ring. The hernia was reduced and the sac excised. He approximated the iliopubic tract to the Coopers ligament. 3.2.1 TENSION FREE TECHNIQUES 3.2.1.1 STOPPA REPAIR (5) The Stoppa repair uses giant prosthesis for repair of complex or bilateral hernias. The preperitoneal space is entered with a midline subumbilical incision or a low transverse incision.The preperitoneal space is created with blunt dissection. Hernia is reduced and an indirect sac is opened and its contents reduced. A giant mesh of size 24*18 cm is places with the help of clamps.Stoppa prefers not to use tacks. The mesh is held in place by the intraabdominal pressure (Pascals law) 3.2.1.2 LICHTENSTEINS REPAIR (5) Originally invented by Newman, the technique was popularised by Lichtenstein. Lichtensteins repair is an anterior repair and has the advantage of minimum dissection and quicker learning curve. Performed under local anaesthesia a 5 cm incision extending from the pubic tubercle along the langers line is used to open the external oblique aponeurosis. The sac is separated from the cord. A direct sac is simply inverted. An indirect sac is dissected free and inverted or if difficult proximal part is ligated and everted while the distal part is left open. A mesh 8 into 16 cm is placed and the inferior border is fixed using continuous sutures starting medially from the pouparts ligament overriding the pubic tubercle to just lateral to the internal ring. The superiomedial border is fixed to the rectus sheath while the superior part is sutured using interrupted stitches to the conjoint tendon and internal oblique. In the event of the presence of a femoral hernia the inferior border is sutured to the Coopers ligament. In the lateral part of the mesh a slit is made the lower portion of which should be 1/3rd the size of the mesh. The so formed tails should wrap around the cord and they are further suture fixed to the inguinal ligament. When the mesh is finally placed the distal part
4|Page
of the tail will lie beneath the external oblique. Routine division of the cremaster is not proposed. 3.2.1.3 PLUG AND PATCH (5) A cone shaped polypropylene mesh is used to plug the inguinal canal and a mesh is sewn around the spermatic cord. Mesh migration has been reported as a complication. The technique is relatively easy to perform and can be adopted to repair hernias of various sizes. 3.2.1.4 KUGEL REPAIR (3) Is preperitoneal or posterior hernia repair using tension free technique. It boasts a fast recovery and minimum inguinodynia arising from extensive dissection. The technique is useful in all groin hernias. According to Kugel the procedure should be avoided in cases of recurrence after laparoscopic hernia repair and in the younger paediatric population. The operation is preferably undertaken under local anaesthesia and involves using a mesh patch which comes with a choice of two sizes; small 8/12 and medium 11/14. The placement of incision is very important is carry out a smooth dissection as the operation proceeds. An incision is placed just superior to the internal ring and just lateral to the inferior epigastric vessels. After incising through the skin and subcutaneous tissue the external and internal oblique muscles are bluntly opened to identify the transversalis fascia. This can be the most difficult step in the whole dissection for the beginner. After entering the preperitoneal space a small pocket is created just lateral to the inferior epigastric vessels. These vessels serve as the orienting structures throughout the period of dissection. The cord is dissected and the hernia is reduced. If it is a direct hernia the the mesh should be placed directly over the symphysis pubis. A self-expanding patch is introduced and held in place with a single stitch. 3.2.1.2 PROLENE HERNIA REPAIR SYSTEM. (5) Introduced by Gilbert, the inguinal canal is approached through an anterior approach. The sac is dissected and inverted .The posterior layer of the PHS is then placed in the preperitoneal space. The anterior part is placed behind the aponeurosis with a lateral slit to accommodate the spermatic cord. It combines the principles of both anterior and posterior repair. 3.2.2 LAPAROSCOPIC HERNIA REPAIR (3) Still under scrutiny by its critics particularly for its cost effectiveness, laparoscopic hernia repair has been proved to be a safe method of intervention in experienced hands. While the transabdominal preperitoneal approach (TAPP) was soon followed by total extraperitoneal (TEP) approach TAPP continues to enjoy support from a fair number of surgeons. In TAPP the operator uses two 5mm ports placed in the right and left lower quadrants and a 10mm port in the subumbilical area. Once the peritoneum is entered a transverse incision starting from the median umbilical line to the anterior superior iliac spine is placed on the peritoneum which is dissected off from the transversalis fascia. The cord followed by the sac
5|Page
is isolated. The sac is either everted or in case of difficult dissection is dissected with ligation of the proximal part. A large mesh is placed to effectively cover the myopectineal orifice. The mesh is fixed medially to the Coopers ligament and laterally to the iliopubic tract to prevent migration. In TEPP the peritoneum is not penetrated and it is stripped from the transversalis fascia manually or using a balloon dissector. The benefits outlined for TAPP are better initial view, shorter learning curve and an opportunity for the surgeons to evaluate the intraabdominal organs for any other potential pathology. The caveats for this procedure include risk of visceral injury, an increase in operating time by spending on closure of peritoneum .On the other hand TEP is appreciated for its less invasive nature though it comes at the expense of increased operative time and a further increase in the learning curve. CRITICAL APPRAISAL Since the published work of Marcy in 1871 the management of hernia has come a long way. While Bassini is credited with laying the foundation for tissue based repair the present day surgeons focus on tension free repair by deploying various techniques using synthetic mesh. While the initial outlook on a successful repair was to achieve a low rate of recurrence with the emergence of more and more techniques with acceptable recurrence rates other aspects of surgery like avoidance of chronic post operative pain, early return to normal activity and operating time started receiving more attention. Shouldice technique which is a modification of the original Bassini claims a low recurrence rate among open repairs.Scott et al reviewed twenty trials comparing open mesh with non mesh techniques for groin hernia repairs and concluded that mesh repair has less of recurrence with similar rates of complication as non mesh repair.(6) In a prospective randomized trial comparing Lichtenstein technique with four layer Shouldice procedure the author concludes that while both techniques are effective. However the Lichtenstein technique is more favoured because it is easy to master, the recurrence rate is lower, and can be performed under local anaesthesia.(7) In a systematic review by the Cochrane group comparing Shouldice repair with other open mesh and non mesh techniques the authors conclude that Shouldice has got a higher recurrence rate compared to mesh repairs. However they also conclude that Shouldice is the technique with the lowest recurrence rate among all tissue repairs. They didnt notice any major difference with regard to post operative complications, chronic pain or post-operative stay. (8) Many reviews have confirmed that Shouldice is certainly associated with a higher recurrence rate compared to mesh based repair.(2,9,10) Conclusion: Use of mesh results in less recurrence. Shouldice is the best non-mesh repair. (Level 1A evidence ) Mesh decreases the chances of chronic pain. Open mesh hernia repair is more cost effective from the hospital perspective. (Level 1B evidence) In a comparison of Lichtenstein technique with Prolene Hernia Repair system (PHS) and Plug and Patch report from a centre that performed 472 repairs states that the outcomes are similar and PHS and P&P can be performed faster than Lichtensetins.(11) In yet another
6|Page
comparison the authors found that there is no significant difference in the postoperative pain or quality of pain among the three methods(12) Osman et al from turkey compare the Kugel technique with Lichtensteins technique and found that the both the techniques are similar in complication rates. (13) For a surgeon who is proficient in this technique the Kugel repair can indeed prove to be very useful; particularly in the case of recurrent hernias following an open anterior repair. Severe complications like fistulisation with erosion of the mesh into bowel have been reported in the literature.(14) However this might have happened due to a number of reasons like improper technique, failure to appreciate the anatomy fully or technical issues relating to the mesh. In a recent randomized trial comparing pain following Kugels repair and Lichtensteins the authors noticed less pain at three months in the Kugel group.(15) The number of patients reporting pain were also significantly less in the Kugel group. They attribute this to less of neuronal damage in the preperitoneal approach compared to the Lichtensteins. On the contrary the proponents of Lichtensteins argue that the preperitoneal placement of a mesh will make any future operative intervention in this area like radical prostatectomy very difficult.(16) Conclusion: PHS, Plug and Patch, Kugel has comparable outcome in terms of recurrence to Lichtenstein (Level 2B) They can be considered as an alternative treatment for Lichtenstein (Grade B Recommendation) Laparoscopic surgery for cholecystectomy gained widespread acceptance very quickly. The same has not been the case with laparoscopic intervention for hernia. While a lot of comparisons are available in the literature the Veterans affairs Co-operative trial is very often quoted. According to this study the 2 year recurrence rate was significantly higher in the laparoscopic hernia group;10.1% vs 4.9%. (17)The complication rates were also higher with laparoscopic group. Return to activity was almost same in both the groups (39 vs 33.4%) The study was criticised with regard to the experience of the surgeons in laparoscopic Surgery as the reported rate of recurrence for LHR was much higher than other series .In a multicentre randomized trial from Sweden with a follow up of 5 years the authors initially report a recurrence rate of 3.5 % with LHR. With the exclusion of one Surgeon who was responsible for all cases of recurrence in LHR the recurrence rate fell to 2,4% as opposed to 1.2% for Lichtensteins in the same trial.(18) The authors also mention that in the Swedish hernia register the number hernia cases attempted laparoscopically has decreased from 20% in 1990s to 9% in 2006.It is possible that the increased operating time and the long learning curve have prompted surgeons to choose open mesh repair. In a Cochrane review of 41 trials involving more than 7000 patients the author concludes that patients in the laparoscopic arm returned earlier to usual activities and reported less pain. This came at the expense of slightly prolonged operative time and visceral injuries. The review concludes that irrespective of the method it is the use of mesh that reduces the recurrence.(19) In a similar meta-analysis appearing in the American Journal of Surgery the authors state that with the advent of the open mesh posterior technique there has been no significant difference between LHR and OR with regard to post operative recovery and recurrence rate. These authors also hint that it is the presence of the mesh that alters the outcome and not the method in which it is placed. (20) In yet another report from a prospective randomized study from Austria the authors
7|Page
mention no significant difference in complications or recurrence at the end of three years between LHR and various forms of open repair.(21) While some element of controversy mars the laparoscopic hernia repair, there seems to be general agreement in the use of laparoscopic surgery for recurrent hernias. A randomized prospective trial from Finland comparing TEP and Lichtensteins repair for recurrent inguinal hernias showed better results for LHR.(22) There was early return to work, less of post operative pain (27.7% vs 8.2%) and no recurrence rate (6.4% vs 0.0%) with LHR. In the case of bilateral inguinal hernia the recurrence rates are very similar between anterior mesh repair and LHR. TAPP has been compared with TEP in many studies. TAPP is technically more simple but essentially enters the peritoneal cavity. TEP has the benefit of staying out of the peritoneal cavity and therefore less damage to viscera. There has been no significant difference between the two with regard to postoperative pain, length of stay or return to normal activity.(23) Conclusion Laparoscopic Surgery claims less of wound infection, haematoma and early return to work or activity (Level 1A evidence) There is less of chronic pain. There is less of postoperative pain and faster convalescence in recurrent hernia. From socio economic perspective laparoscopic hernia is more beneficial (particularly in the case of bilateral hernias) Level 1 B evidence Chronic Groin Pain (24) With less and less of recurrence noticed with mesh and laparoscopic repair the focus has shifted to a complication that was previously not well recognized, namely inguinodynia or chronic groin pain. This is defined as persistence of groin pain following inguinal hernia surgery for a period of more than 3 months after complete healing has taken place. Inguinodynia is reported to be present in about 30% of the patients in the form of mild discomfort and in 6% as high intensity pain to the limit that it interfere with the day to day activities of the individual. Avoiding extensive dissections of nerves, the cremaster and the tissues, along with proper identification of nerves will help prevent the incidence of this complication. When present conservative measures are tried as first line including oral analgesics and regional nerve blocks. When the pain is severe and disabling operative intervention should be undertaken. The choice of procedure is triple neurectomy involving division of ilioinguinal,iliohypogastric and genital branch of genitofemoral nerve with reported resolution of symptoms in upto 80% of the patients.. CONCLUSION Hernia surgery will continue to put a significant burden on health resources in the developed and developing countries. Although a number of surgical options have surfaced in the last few decades a consensus has not been reached as to the best possible option. For a successful outcome the surgeon should be proficient in his technique and also in his understanding of anatomy of the inguinal area. This is reflected in the fact that almost all the techniques have shown admirable results in the hands of specialists surgeons in respective areas. In the light
8|Page
of present evidence mesh repair has superior results to tissue repair with regard to recurrence. However mesh repair cant be attempted where gangrenous bowel is present. Hence mastering a tissue based repair is essential for the surgeon. Laparoscopic surgery needs considerable experience in the part of the operating surgeon to achieve similar results as that of open mesh repair.
BIBLIOGRAPHY 1. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients Hernia (2009) 13:343403 2. Herniology Past, Present and Future R C Read Hernia (2009) 13:577580 3. Mastery of Surgery 4. Femoral Hernia Repair T Hachisuka Surgical Clinics of North America 83 (2003) 1189-1205 5. Open Repair of Inguinal Hernia:An Evidence-Based Review Surg Clin N Am 88 (2008) 139155 6. Cochrane Database Syst Rev. 2002;(4):CD002197. Open mesh versus non-mesh for repair of femoral and inguinal hernia.Scott NW et al,Department of Public Health, University of Aberdeen, UK 7. Prospective Randomized comparison of the Shouldice and Lichtenstein Hernia Repair Procedures J E McGuillicuddy Arch Surg Vol 133, Sep 1998, page 974 8. Shouldice technique versus other open techniques for inguinal hernia repair (Review) Amato B, Moja L, Panico S, Persico G, Rispoli C, Rocco N, Moschetti 9. Recurrence Rates for Shouldice Repair versus Tension-free techniques in Inguinal Hernia repair: A Meta-Analysis. GERHARDUS A, PERLETH M Annu Meet Int Soc Technol Assess Health Care Int Soc Technol Assess Health Care Meet. 2001; 17: abstract no. 92.
9|Page
10. Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs M. Butters 1, J. Redecke 1, J. Kninger 1British Journal of SurgeryVolume 94 Issue 5, Pages 562 565 11. Prolene Hernia System, Lichtenstein mesh and plug-and-patch for primary inguinal hernia repair: 3-year outcome of a prospective randomised controlled trial. TheBOOP study: bi-layer and connector, on-lay, and on-lay with plug for inguinalhernia repair. alenbck J, Andersson C, Anesten B, Bjrck S, Eklund S, Magnusson O, Rimbck G, Stenquist B, Wedel N. Hernia. 2009 Apr;13(2):121-9; discussion 231. Epub 2008 Nov 13. 12. Randomized trial comparing the Prolene Hernia System, mesh plug repair and Lichtenstein method for open inguinal hernia repair. Nienhuijs SW, van Oort I, Keemers-Gels ME, Strobbe LJ, Rosman C. Br J Surg. 2005 Jan;92(1):33-8. 13. Systemic inflammatory response after Kugel versus laparoscopic groin hernia repair: a prospective randomized trial 14. Colovesical Wstula following an open preperitonealKugel mesh repair of an inguinal hernia S. G. Barreto D. Schoemaker M. Siddins D. Wattchow Hernia (2009) 13:647649 15. Pain after Open Preperitoneal Repair versus Lichtenstein Repair: A Randomized Trial Simon Nienhuijs Erik Staal Mariel Keemers-Gels Camiel Rosman Luc StrobbeWorld J Surg (2007) 31:17511757 16. Groin Hernia Repair: Open Techniques Parviz K Amid World J. Surg. 29, 1046 1051 (2005) 17. Open Mesh versus laparoscopic repair of Inguinal Hernia Neumayer et al NEJM, 2004 April 29 Vol 350 No 18 18. Low recurrence rate after laparoscopic and open inguinal hernia repair Eklund et al Ann Surg 2009, 249, 33-38 19. Laparoscopic techniques versus open techniques for inguinal hernia repair (Review) McCormack K, Scott N, Go PM, Ross SJ, Grant A, Collaboration the EU Hernia Trialists 20. Meta-analysis of laparoscopic inguinal hernia trials favors open hernia repair with preperitoneal mesh prosthesis C. Randle Voyles, Brian J. Hamilton, William D. Johnson. The American Journal of Surgery 184 (2002) 610 21. Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized H. Pokorny A. Klingler T. Schmid R. Fortelny C. Hollinsky R. Kawji E. Steiner H. Pernthaler Hernia (2008) 12:385389 22. Lichtenstein Hernioplasty Versus Totally Extraperitoneal Laparoscopic Hernioplasty in Treatment of Recurrent Inguinal HerniaA Prospective Randomized Trial Sanna T. H. Kouhia et al Annals of Surgery Volume 249,
Number 3, March 2009
23. Laparoscopic versus Open Inguinal Hernia Repair Jon Gould, MD, FACS Surg Clin N Am 88 (2008) 10731081
10 | P a g e
24. Postherniorrhaphy groin pain and how to avoid it G S Ferzli surgical Clinics of North America 88 (2008) 203-216
Das könnte Ihnen auch gefallen
- Treatment: Bassini RepairDokument5 SeitenTreatment: Bassini RepairziehonkNoch keine Bewertungen
- Hernia - Hernioplasty With Bilayer Polypropylene Mesh PDFDokument4 SeitenHernia - Hernioplasty With Bilayer Polypropylene Mesh PDFAnonymous YLmmme4XX0Noch keine Bewertungen
- Incisional Hernia RepairDokument6 SeitenIncisional Hernia RepairLouis FortunatoNoch keine Bewertungen
- Incisional HerniaDokument13 SeitenIncisional HerniaMaya Dewi permatasariNoch keine Bewertungen
- Femoral Hernia. The SAGES Manual of Hernia Repair.Dokument12 SeitenFemoral Hernia. The SAGES Manual of Hernia Repair.Eri ContrerasNoch keine Bewertungen
- Synchronous Open Hernioplasty of Primary Bilateral Inguinal HerniaDokument6 SeitenSynchronous Open Hernioplasty of Primary Bilateral Inguinal HerniaKhaled MonazeaNoch keine Bewertungen
- HernioplastyDokument58 SeitenHernioplastyFobin VargheseNoch keine Bewertungen
- Hernia PathophysiologyDokument1 SeiteHernia PathophysiologyIvan Louise Fajardo Maniquiz83% (6)
- Open Inguinal Hernia RepairDokument6 SeitenOpen Inguinal Hernia RepairKris TejereroNoch keine Bewertungen
- Abdominoperineal Resection MilesDokument17 SeitenAbdominoperineal Resection MilesHugoNoch keine Bewertungen
- HerniaDokument41 SeitenHerniashobharamkrishna67% (3)
- 002 Hernia InghinalaDokument120 Seiten002 Hernia InghinalaAdina Paula Găburoi100% (1)
- Abdominal Wall ReconstructionDokument32 SeitenAbdominal Wall ReconstructionRahab SaeedNoch keine Bewertungen
- Laparoscopic Total Extra Peritoneal Inguinal Hernia RepairDokument11 SeitenLaparoscopic Total Extra Peritoneal Inguinal Hernia Repairmarquete72100% (1)
- Laparoscopic Trans Abdominal Pre Peritoneal Inguinal Hernia ReDokument7 SeitenLaparoscopic Trans Abdominal Pre Peritoneal Inguinal Hernia Remarquete72100% (1)
- Laparoscopic Repair of Supra Pubic Ventral HerniasDokument17 SeitenLaparoscopic Repair of Supra Pubic Ventral Herniasmarquete72100% (1)
- Img 0044Dokument1 SeiteImg 0044O'jays NavarroNoch keine Bewertungen
- The 3rd Edition: Prevention & Management: Complications of Laparoscopic Inguinal Hernia RepairDokument5 SeitenThe 3rd Edition: Prevention & Management: Complications of Laparoscopic Inguinal Hernia RepairVishnu KumarNoch keine Bewertungen
- Bulbar Urethroplasty Using The Dorsal Approach: Current TechniquesDokument7 SeitenBulbar Urethroplasty Using The Dorsal Approach: Current TechniquesFitrah TulijalrezyaNoch keine Bewertungen
- Inguinal Hernia Surgery OverviewDokument15 SeitenInguinal Hernia Surgery OverviewWarda BajwaNoch keine Bewertungen
- Laparoscopic Repair of Inguinal HerniaDokument12 SeitenLaparoscopic Repair of Inguinal Herniawadhe omara100% (1)
- Incisional Hernia Open ProceduresDokument25 SeitenIncisional Hernia Open ProceduresElias Emmanuel JaimeNoch keine Bewertungen
- TAPP - Stuttgart Technique and Result of A Large Single Center SeriesDokument5 SeitenTAPP - Stuttgart Technique and Result of A Large Single Center SeriessravikanthNoch keine Bewertungen
- Laparoscopic Appendectomy: Samir DelibegovićDokument7 SeitenLaparoscopic Appendectomy: Samir DelibegovićKamran AfzalNoch keine Bewertungen
- (Theo) M. Zuvela, Management of Epigastric, Umbilical, Spigelian AnDokument7 Seiten(Theo) M. Zuvela, Management of Epigastric, Umbilical, Spigelian AnTheo Rezende CamargoNoch keine Bewertungen
- Pediatric Laparoscopic Inguinal Hernia Repair - A Review of Techniques - A SAGES Wiki ArticleDokument30 SeitenPediatric Laparoscopic Inguinal Hernia Repair - A Review of Techniques - A SAGES Wiki ArticleAndri Feisal NasutionNoch keine Bewertungen
- Appendectomy Case PresentationDokument23 SeitenAppendectomy Case PresentationMarie Nelle Escriba LimpocoNoch keine Bewertungen
- Stoppa Forgotten SurgeryDokument4 SeitenStoppa Forgotten SurgeryGuilherme Kazuo OgawaNoch keine Bewertungen
- Richter's Sacrospinous FixationDokument13 SeitenRichter's Sacrospinous FixationChopin SripramodyaNoch keine Bewertungen
- Closure in Lap PDFDokument10 SeitenClosure in Lap PDFpritiNoch keine Bewertungen
- Surgical Techniques in Primary Inguinal Hernia RepairDokument7 SeitenSurgical Techniques in Primary Inguinal Hernia RepairNuno AzenhaNoch keine Bewertungen
- Ciencia e Technica Omentum Overlay PDFDokument10 SeitenCiencia e Technica Omentum Overlay PDFAlin MihetiuNoch keine Bewertungen
- Print Test Page556Dokument5 SeitenPrint Test Page556andhikaaji4980Noch keine Bewertungen
- Appendiktomi Translate BookDokument19 SeitenAppendiktomi Translate Bookalyntya melatiNoch keine Bewertungen
- Types of Abdominal IncisionsDokument3 SeitenTypes of Abdominal Incisionsjhuzt4_facebook_343onlyNoch keine Bewertungen
- AppendectomyDokument6 SeitenAppendectomyMarie Nelle Escriba LimpocoNoch keine Bewertungen
- Anterior Abdominal Wall HerniaDokument8 SeitenAnterior Abdominal Wall HerniaOttofianus Hewick KalangiNoch keine Bewertungen
- Case Report: Laparoscopic Repair of Postoperative Perineal HerniaDokument3 SeitenCase Report: Laparoscopic Repair of Postoperative Perineal HerniacleybismarNoch keine Bewertungen
- Mayo 1901Dokument9 SeitenMayo 1901Martin BergerNoch keine Bewertungen
- Voie Pararectus +++Dokument12 SeitenVoie Pararectus +++amineNoch keine Bewertungen
- Probe Laminotomy: A Simple Technique For Precise Lateral Gutter Placement in Cervical Expansive LaminoplastyDokument5 SeitenProbe Laminotomy: A Simple Technique For Precise Lateral Gutter Placement in Cervical Expansive Laminoplasty阮威勝Noch keine Bewertungen
- Final Hernioplasty Compilation RevisedDokument58 SeitenFinal Hernioplasty Compilation RevisedRaidis PangilinanNoch keine Bewertungen
- Retromuscular Repairs For Ventral HerniaDokument76 SeitenRetromuscular Repairs For Ventral HerniaROUNAK MEHROTRANoch keine Bewertungen
- Laparoscopic Flank Hernia RepairDokument10 SeitenLaparoscopic Flank Hernia Repairmarquete72100% (3)
- Use Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenDokument4 SeitenUse Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenYelisa PatandiananNoch keine Bewertungen
- Procedeul Lichtenstein "Tension-Free" În Tratamentul Herniei InghinaleDokument3 SeitenProcedeul Lichtenstein "Tension-Free" În Tratamentul Herniei InghinaleSpecialNameNoch keine Bewertungen
- FESSDokument5 SeitenFESSMarco Antonio FigueroaNoch keine Bewertungen
- The Lumbar MicrodiscectomyDokument5 SeitenThe Lumbar Microdiscectomyokta fianNoch keine Bewertungen
- Baker 1950Dokument15 SeitenBaker 1950Cotaga IgorNoch keine Bewertungen
- LaparoscopeDokument9 SeitenLaparoscopedharmaNoch keine Bewertungen
- Strangulated Groin Hernia Repair: A New Approach For All: Abst TDokument4 SeitenStrangulated Groin Hernia Repair: A New Approach For All: Abst TAzizah Azhmi AuliaNoch keine Bewertungen
- Gibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryDokument7 SeitenGibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryjuanguapoNoch keine Bewertungen
- Hernia CurrentDokument5 SeitenHernia CurrentSheikha KhadijahNoch keine Bewertungen
- Appendectomy: Surgical TechniqueDokument7 SeitenAppendectomy: Surgical TechniqueEugene LimNoch keine Bewertungen
- Omentum OverlayDokument10 SeitenOmentum OverlayAlin MihetiuNoch keine Bewertungen
- Laparoscopic Umbilical Hernia Repair Technique PapDokument6 SeitenLaparoscopic Umbilical Hernia Repair Technique PapEremeev SpiridonNoch keine Bewertungen
- Double Mandibular Osteotomy With Coronoidectomy For Tumours in The Parapharyngeal SpaceDokument5 SeitenDouble Mandibular Osteotomy With Coronoidectomy For Tumours in The Parapharyngeal SpaceSree BanNoch keine Bewertungen
- Abdominal Anatomy and Surgical IncisionsDokument31 SeitenAbdominal Anatomy and Surgical Incisionsjuan santosNoch keine Bewertungen
- Umbilicalherniarepair: Overview of Approaches and Review of LiteratureDokument16 SeitenUmbilicalherniarepair: Overview of Approaches and Review of LiteratureVictor Matias BarriosNoch keine Bewertungen
- Novel Technique For Safe Primary Trocar InsertionDokument5 SeitenNovel Technique For Safe Primary Trocar InsertionPrameita Rahmawati MITNoch keine Bewertungen
- Jurnal HisprungDokument2 SeitenJurnal HisprungOpi RahmaNoch keine Bewertungen
- Inguinal Hernia - Surgical ManagementDokument2 SeitenInguinal Hernia - Surgical ManagementSubhasree RajagopalanNoch keine Bewertungen
- Tensioned Reverse Abdominoplasty: BackgroundDokument8 SeitenTensioned Reverse Abdominoplasty: BackgroundlarissaNoch keine Bewertungen
- A Manual of the Operations of Surgery: For the Use of Senior Students, House Surgeons, and Junior PractitionersVon EverandA Manual of the Operations of Surgery: For the Use of Senior Students, House Surgeons, and Junior PractitionersNoch keine Bewertungen
- Tumor Volume To Fetal Weight Ratio As An Early Prognostic Classification For Fetal Sacrococcygeal TeratomaDokument4 SeitenTumor Volume To Fetal Weight Ratio As An Early Prognostic Classification For Fetal Sacrococcygeal TeratomaBembie PurwonoNoch keine Bewertungen
- PancreatitisDokument36 SeitenPancreatitislowhillNoch keine Bewertungen
- Apache ScoreDokument10 SeitenApache ScorelowhillNoch keine Bewertungen
- Paediatrica Indonesiana: Priyanti Kisworini, Amalia Setyati, SutaryoDokument5 SeitenPaediatrica Indonesiana: Priyanti Kisworini, Amalia Setyati, SutaryolowhillNoch keine Bewertungen
- Labiaplasty - Revision of The Large Labia MinoraDokument7 SeitenLabiaplasty - Revision of The Large Labia Minoraufirst rejuvenationNoch keine Bewertungen
- Overview of Treatment For Inguinal and Femoral Hernia in AdultsDokument20 SeitenOverview of Treatment For Inguinal and Femoral Hernia in AdultsjimdioNoch keine Bewertungen
- Grynfeltt-Lesshaft Lumbar Hernia: Sebuah Kasus Wanita 57 Tahun Dengan Benjolan Di Sisi Kanan AbdomenDokument11 SeitenGrynfeltt-Lesshaft Lumbar Hernia: Sebuah Kasus Wanita 57 Tahun Dengan Benjolan Di Sisi Kanan AbdomendewiswahyuNoch keine Bewertungen
- An Inguinal HerniaDokument4 SeitenAn Inguinal HerniaAddy Rayner RobertNoch keine Bewertungen
- New ListDokument39 SeitenNew ListKamal GpNoch keine Bewertungen
- BibliographyDokument10 SeitenBibliographySourav Kumar PatraNoch keine Bewertungen
- Incisional Hernia ThesisDokument5 SeitenIncisional Hernia Thesisgbwy79ja100% (1)
- HerniaDokument61 SeitenHerniaAhmed HassanNoch keine Bewertungen
- Presentation1 HerniaDokument12 SeitenPresentation1 Herniatiwwiyeni16Noch keine Bewertungen
- Hernia InguinalDokument14 SeitenHernia InguinalSisty AdeaNty SNoch keine Bewertungen
- Karakteristik Hernia Inguinalis Di Rumah Sakit Umum Daerah Dr. Pirngadi Medan Tahun 2016Dokument4 SeitenKarakteristik Hernia Inguinalis Di Rumah Sakit Umum Daerah Dr. Pirngadi Medan Tahun 2016Anonymous o7y9x3lGNoch keine Bewertungen
- Clinical Preview About Hernia: It's Types, Clinical Presentation, Diagnosis and RepairDokument10 SeitenClinical Preview About Hernia: It's Types, Clinical Presentation, Diagnosis and RepairAfnan AdelNoch keine Bewertungen
- Current Options in Umbilical Hernia Repair in Adult PatientsDokument5 SeitenCurrent Options in Umbilical Hernia Repair in Adult PatientsSisca Dwi AgustinaNoch keine Bewertungen
- A Study To Assess The Prevalence and Risk Factors of Inguinal HerniaDokument3 SeitenA Study To Assess The Prevalence and Risk Factors of Inguinal Herniamelon segerNoch keine Bewertungen
- Lo 5Dokument13 SeitenLo 5Mutiara Prima DianaNoch keine Bewertungen
- 06 Inguinal Hernia SrsDokument10 Seiten06 Inguinal Hernia SrslowhillNoch keine Bewertungen
- Kuliah 6 - Abdoiminal HerniaDokument30 SeitenKuliah 6 - Abdoiminal HerniamochagilNoch keine Bewertungen
- Abdominal HerniaDokument3 SeitenAbdominal HerniaShenyel Hey'tsmeNoch keine Bewertungen
- HERNIIDokument4 SeitenHERNIISeceleanu MarianNoch keine Bewertungen
- A R Are Case of Amyands Hernia With Mucocele AppendixDokument2 SeitenA R Are Case of Amyands Hernia With Mucocele AppendixRajeev ThilakNoch keine Bewertungen
- Hernia World Conference Program PDFDokument112 SeitenHernia World Conference Program PDFMohamed Irsha0% (1)
- Overview of Treatment For Inguinal and Femoral Hernia in Adults - UpToDateDokument30 SeitenOverview of Treatment For Inguinal and Femoral Hernia in Adults - UpToDatehgz1 colimaNoch keine Bewertungen
- Hernia PDFDokument5 SeitenHernia PDFAngelica SanabriaNoch keine Bewertungen
- Horse HerniaDokument2 SeitenHorse HerniaHadi Putra RihansyahNoch keine Bewertungen
- Abdomen-Clinicals - PDF Version 1Dokument11 SeitenAbdomen-Clinicals - PDF Version 1hamzabhayatNoch keine Bewertungen
- Pemeriksaan Penunjang Hernia InguinalisDokument5 SeitenPemeriksaan Penunjang Hernia InguinalisGalihNoch keine Bewertungen