Beruflich Dokumente
Kultur Dokumente
Effects of Cis-Resveratrol On Inflammatory Murine Macrophages Antioxidant Activity and Down-Regulation of Inflammatory Genes PDF
Hochgeladen von
Sava1988Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Effects of Cis-Resveratrol On Inflammatory Murine Macrophages Antioxidant Activity and Down-Regulation of Inflammatory Genes PDF
Hochgeladen von
Sava1988Copyright:
Verfügbare Formate
Effects of cis-resveratrol on inammatory murine macrophages: antioxidant activity and down-regulation of inammatory genes
Jose Leiro,* Ezequiel Alvarez, Juan A. Arranz,* Reyes Laguna, Eugenio Uriarte, and Francisco Orallo,1 Departamentos de *Microbiologa y Parasitologa, Farmacologa, y Qumica Organica, Facultad de Farmacia, Universidad de Santiago de Compostela, Spain
Abstract: This study investigated for the rst time the effects of the cis isomer of resveratrol (c-RESV) on the responses of inammatory murine peritoneal macrophages, namely on the production of reactive oxygen species (ROS) and reactive nitrogen species (RNS) during the respiratory burst; on the biosynthesis of other mediators of inammation such prostaglandins; and on the expression of inammatory genes such as inducible nitric oxide synthase (NOS)-2 and inducible cyclooxygenase (COX)-2. Treatment with 1100 M c-RESV signicantly inhibited intracellular and extracellular ROS production, and c-RESV at 10 100 M signicantly reduced RNS production. c-RESV at 1100 M was ineffective for scavenging superoxide radicals (O2 ), generated enzymatically by a hypoxanthine (HX)/xanthine oxidase (XO) system and/or for inhibiting XO activity. However, c-RESV at 10 100 M decreased nicotinamide adenine dinucleotide/nicotinamide adenine dinucleotide phosphate (NADH/NADPH) oxidase activity in macrophage homogenates. c-RESV at 100 M decreased NOS-2 and COX-2 mRNA levels in lipopolysaccharide (LPS) interferon gamma (IFN- )-treated macrophages. At 10 100 M, c-RESV also signicantly inhibited NOS-2 and COX-2 protein synthesis and decreased prostaglandin E2 (PGE2) production. These results indicate that c-RESV at micromolar concentrations signicantly attenuates several components of the macrophage response to proinammatory stimuli (notably, production of O2 and of the proinammatory mediators NO and PGE2). J. Leukoc. Biol. 75: 1156 1165; 2004.
Key Words: NADH/NADPH oxidase xanthine oxidase nitric oxide inducible nitric oxide synthase cyclooxygenase-2 prostaglandin E2
despite a high-fat diet, little exercise, and widespread smoking, is associated with a very low incidence of cardiovascular diseases, mainly coronary heart disease (the so-called French paradox) [1]. The cardioprotective effects of red wine appear to be independent of alcohol content, and over the last few years, numerous studies have been performed with the aim of identifying the components responsible. Although these compounds have yet to be conclusively identied, the principal candidates are a number of polyphenolic compounds such as stilbenes and avonoids (for review, see, e.g., ref. [2]). Resveratrol [3,4 ,5-trihydroxystilbene (RESV)] is a natural phytoalexin (phytoestrogen) synthesized in response to injury or fungal attack, found in grape skin, and notably, in red wine in its two isomers, trans and cis (ref. [3]; see Fig. 1). A wide range of RESV concentrations in the different wines analyzed (depending on a number of factors) has been reported. In some wines, the cis isomer is in higher concentrations than the trans isomer, whereas in other wines, the predominant form is the trans-resveratrol (t-RESV; see, e.g., refs. [4, 5]). To date, the majority of studies of pharmacological effects have considered t-RESV, which has been proposed as one of the principal candidates involved in the cardioprotective effects of red wine (see, e.g., ref. [6]). This isomer of RESV displays in the in vitro, ex vivo, and/or in vivo experiments a number of pharmacological effects including modulatory lipoprotein metabolism, antiinammatory, platelet antiaggregatory, anticarcinogenic, and vasodilatory properties, as has been reviewed previously (see, e.g., refs. [3, 7]). Some of these pharmacological effects seem to be implicated in the cardiovascular protection attributed to t-RESV and red wine [7]. In contrast, much less is known about the pharmacological activity of the cis isomer (c-RESV), possibly as a result of the fact that c-RESV (unlike the trans isomer) is not available commercially. A few studies have demonstrated only quantitative differences in the activity of the two forms; for example, the cis isomer induces a greater decrease in collagen-induced platelet aggregation than the trans
INTRODUCTION
A number of large-scale epidemiological studies have suggested that a prolonged and moderate consumption of red wine by the Southern French and other Mediterranean populations,
1156 Journal of Leukocyte Biology Volume 75, June 2004
Correspondence: Departamento de Farmacologa, Facultad de Farmacia, Universidad de Santiago de Compostela, Campus Universitario Sur, E-15782 Santiago de Compostela (La Coruna), Spain. E-mail: fforallo@usc.es Received November 13, 2003; revised January 8, 2004; accepted January 15, 2004; doi: 10.1189/jlb.1103561.
1
http://www.jleukbio.org
isomer [8], and in the cyclooxygenase (COX)-1 assay, t-RESV appears to be more active than c-RESV [9]. During phagocytosis or stimulation with any of a wide variety of agents, macrophages activate various cell processes including the respiratory burst, in which an increase in oxygen uptake results in the production of reactive oxygen species (ROS), critical for successful defense against invading organisms [10]. ROS production occurs through two main mechanisms. One is activation of a multicomponent nicotinamide adenine dinucleotide/nicotinamide adenine dinucleotide phosphate (NADH/NADPH) oxidase, which is assembled at the plasma membrane and cytosolic protein components and catalyzes the vectorial synthesis of superoxide radicals (O2 ) from oxygen and cellular NADPH (the preferred substrate in phagocytic cells), supplied by the hexose monophosphate shunt (see, e.g., ref. [11]). The second is stimulation of the enzyme xanthine oxidase (XO), which catalyzes the oxidative hydroxylation of purine substrates (e.g., xanthine or hypoxanthine) at the molybdenum center (the reductive half-reaction) with production of uric acid and the subsequent reduction of O2 at the avin center with generation of O2 or H2O2 (the oxidative half-reaction) [12, 13]. Increased ROS production by activated macrophages is also involved in immune diseases, and ROS excess (oxidant/antioxidant imbalance) may play an important role in the (patho)physiology associated with the progression of various chronic inammatory disorders, such as atherosclerosis, rheumatoid arthritis, osteoarthritis, lung diseases, and neurodegenerative diseases [14 18]. In addition, during the respiratory burst, macrophages also produce nitric oxide (NO), a major radical nitrogen species (RNS), which reacts with superoxide to form peroxynitrite, a potent microbicidal agent [19]. NO and prostaglandin E2 (PGE2), produced by inducible NO synthase type 2 (NOS-2) from the amino acid L-arginine and inducible COX-2, respectively, are also important mediators in inammation processes [20]. In this context, a possible role of macrophage activation in different steps of coronary heart disease has been shown by several studies (see, e.g., refs. [2123]). Because of its effects on activated macrophages and on other cell types, t-RESV has been proposed in a number of previous studies as one of the components present in red wine that may confer specic protection against ischemic heart disease [7, 24]. To date, however, there have been no studies of the effects of c-RESV on macrophage respiratory burst responses or on production of inammatory mediators. In the present study, we investigated the in vitro effects of c-RESV on ROS and RNS generation during the respiratory burst of murine thyoglicollate-elicited macrophages. Specically, we investigated effects of c-RESV on the activities of the O2 -generating enzymes NADH/NADPH oxidase and XO; whether c-RESV is able to scavenge O2 ; and whether c-RESV modulates NOS-2/ COX-2 gene or protein expression and PGE2 production in inammatory peritoneal macrophages stimulated with lipopolysaccharide (LPS) and interferon- (IFN- ).
MATERIALS AND METHODS Animals
The animals used throughout this study [Wistar rats (age 8 10 weeks; IffaCredo, LArbresle, Lyon, France), purchased from Criffa (Barcelona, Spain), and BALB/c mouse obtained from Harlan OLAC Ltd. (Oxon, UK)] were housed, cared for, and acclimatized (before the experiments) as previously indicated [6].
Ethical approval
All experiments were performed in accordance with European regulations (Directive 86/609), the Spanish Real Decreto 223/1988 and Orden Ministerial October/13/1989 on animal protection (Directive 86/609), and/or the Guide for the Care and Use of Laboratory Animals, as adopted and promulgated by the U.S. National Institutes of Health (Bethesda, MD; NIH Publication No. 85-23, revised 1996). In addition, all experimental protocols were approved by the Institutional Animal Care and Use Committee of the University of Santiago de Compostela (Spain) and were conducted humanely.
Isolation of murine peritoneal-exudate macrophages
For induction of inammatory responses, animals were injected intraperitoneally (i.p.) with 1 ml (rats) or 0.5 ml (mouse) 3% (w/v in water) thioglycollate broth, and peritoneal exudate was extracted 5 days later. Rat and mouse inammatory peritoneal macrophages were obtained from animals killed by cervical dislocation in a laminar ow chamber to ensure sterile conditions, as described previously by Leiro et al. [25, 26]. More than 97% of the adherent cells showed nonspecic esterase activity, determined as per Strober [27], indicating that they were macrophages.
Assay of ROS generation
The extracellular and intracellular production of ROS during the respiratory burst response of rat thioglycollate-elicited macrophages (i.e., macrophages from rats that had received thioglycollate broth i.p. 5 days previously) was evaluated with OxyBURST Green probes (Molecular Probes, Leiden, The Netherlands) using the OxyBURST Green dihydro-2 ,4,5,6,7,7 -hexauorouorescein/bovine serum albumin (BSA) reagent for quantication of extracellular release of ROS induced by phorbol 12-myristate 13-acetate (PMA) and the amine-reactive OxyBURST Green succinimidyl ester of 2,7-dichlorodihydrouorescein (H2DCF) diacetate reagent conjugated to Kluyveromyces lactis yeast cells for quantitation of intracellular production of ROS as described previously [25, 26].
Generation of O2 by use of the enzymatic hypoxanthine oxidase (HX)XO system
The O2 was generated enzymatically in an HXXO system and quantied by spectrophotometric measurement of the product of the reduction of nitroblue tetrazolium (NBT; Sigma, Alcobendas, Spain), essentially following the procedure described previously [6, 26].
Determination of NADH/NADPH oxidase activity
Rat peritoneal macrophages that had been prestimulated in vivo with thioglycollate were obtained and counted as described previously [25, 26], washed once by centrifugation at 1000 g for 10 min at 4C, and resuspended in 1 ml Hanks balanced salt solution (HBSS) to an approximate concentration of 30 40 106 cells/ml. These cells, maintained on ice, were immediately lysed by sonication at 60 W for 1 min (two pulses of 30 s) to give the macrophage extract. Lysis was conrmed by light microscopy. O2 production was measured in this extract by lucigenin enhanced chemiluminescence (ECL) as described by Orallo et al. [6] and Leiro et al. [26], using 100 M NADPH (tetrasodium salt, Sigma; freshly diluted in HBSS) as substrate for NADH/NADPH oxidase.
Determination of XO activity by use of the xanthineXO system
The potential effects of c-RESV on XO activity were tested by measuring its effects on uric acid formation from xanthine following the general method indicated in Orallo et al. [6].
Leiro et al. Effects of cis-resveratrol on murine macrophages
1157
Determination of XO activity by lucigeninECL assay
This assay was the same as the NADH/NADPH oxidase assay (see above) except that the NADH/NADPH oxidase substrate NADPH was replaced with the XO substrate xanthine (100 M). The chemiluminescence signal emitted in these assays was approximately half that emitted with NADPH as substrate.
Assay of nitrite production
NO production was estimated on the basis of nitrite production in rat macrophage culture supernatants, measured by the Griess reaction, as described elsewhere [25, 28].
Determination of PGE2 in culture supernatants
Aliquots (100 l) of the rat macrophage suspension (106 peritoneal macrophages per ml, obtained after prestimulation with thioglycollate as indicated above) were incubated for 3 h with LPS [100 ng/ml in Dulbeccos modied Eagle medium (DMEM); Sigma] plus IFN- (10 units/ml in DMEM); c-RESV at various concentrations (1, 10, or 100 M in DMEM) or indomethacin (a known, nonselective inhibitor of COX expression and COX enzymatic activity; ref. [29]) at 30 M; or without c-RESV or indomethacin (controls) in 96-well microculture plates at 37C under 5% CO2 in a humidied incubator. The plates were centrifuged at 400 g for 5 min, and PGE2 levels were determined in the supernatant by using a competitive binding immunoassay (R & D Systems, Minneapolis, MN) following the manufacturers instructions.
Determination of NOS-2 and COX-2 mRNA levels by reverse transcriptase-polymerase chain reaction (RT-PCR)
Aliquots (1 ml) of 107 inammatory rat peritoneal macrophages prestimulated in vivo 5 days previously with thioglycollate were incubated for 2 h at 37C in DMEM containing 10 units/ml IFN- , 100 ng/ml LPS, and c-RESV (1, 10, or 100 M) or without c-RESV (controls). Total RNA was isolated from macrophage samples using a monophasic solution of phenol and guanidine thiocyanate (Tripure isolation reagent, Roche, Basel, Switzerland) following the manufacturers instructions. The resulting RNA was dried and then dissolved in diethylpyrocarbonate-treated RNase-free water at 1 g/ml (Sigma). cDNA synthesis was accomplished as described previously [26]. The resulting cDNA (100 ng) was amplied by the PCR using a specic murine NOS-2 forward/ reverse primer pair, 5 -TGGAAGCCGTAACAAAGGAAA-3 /5 -ACCACTCGTACTTGGGATGCT-3 [selected from the complete sequence of NOS-2 mRNA; GenBank of the National Center for Biotechnology Information (NCBI), accession number U03699], and a specic COX-2 forward/reverse primer pair, 5 -TGATCGAAGACTACGTGCAAC-3 /5 -TCATCTCTCTGCTCTGGTCAA-3 (NCBI, accession number NM_011198). Amplication of glyceraldehyde 3-phosphate dehydrogenase (GAPDH) with the forward/reverse primer pair, 5 -ACCGCATCTTCTTGTGCAGT-3 /5 - GCCAAAGTTGTCATGGATGA-3 (NCBI, accession number AF106860), was performed as a control of gene expression. Thermal cycling conditions were as follows: initial denaturing at 94C for 5 min; then, 35 cycles at 94C for 30 s, 55C (NOS-2 and COX-2) or 53C (GAPDH) for 45 s, and 72C for 1 min; and nally, a 7-min extension phase at 72C. In all experiments, we performed RT-PCR controls without RNA or without RT; in no case were amplication products obtained. PCR products (20 l aliquots) were separated on a 2% (w/v) agarose gel in Tris-boric acidEDTA buffer, stained with 0.5 g/ml ethidium bromide, and photographed with a digital camera under Spectroline 312 variable-intensity UV transilluminator (Spectroline, New York, NY). Bands were quantied in tagged image le format (TIFF) using densitometry analysis software (ImageMaster Total Laboratory, ver. 2.00, Amersham Biosciences Europe GmbH, Barcelona, Spain).
Tris-buffered saline (TBS: 50 mM Tris, 0.15 M NaCl, pH 7.4) and resuspended in 0.4 ml TBS and 0.1 ml protease inhibitor cocktail (Sigma) containing 104 mM 4-(2-amino-ethyl)-benzenesulfonyl uoride, 80 M aprotinin, 2 mM leupeptin, 4 mM bestatin, 1.5 mM pepstatin A, and 1.4 mM E-64 [N-(transepoxysuccinyl)-L-leucine-4-guanidinobutylamine]. Thereafter, the mouse peritoneal macrophages (maintained in ice) were sonicated at 60 W for 15 s and centrifuged for 5 min at 13,000 g, and the protein concentration in the supernatant was measured by the Bradford method [30] using BSA as standard. Equal amounts of total protein (60 g in 100 l) were transferred to a hydrophobic polyvinylidene diuoride membrane (Hybond-P, Amersham Biosciences) using a slot-blot ltration manifold (Amersham Biosciences). Membranes were subsequently blocked with 5% (w/v) nonfat milk powder in TBS containing 0.2% (w/v) Tween 20 for 1 h, and COX-2 and NOS-2 were immunodetected by incubation for 1 h at room temperature with a rabbit polyclonal antiserum against murine COX-2 (Cayman Chemical Co., Ann Arbor, MI) and NOS-2 (Alpha Diagnostic International, San Antonio, TX) diluted 1:1000 in dilution buffer [TBS containing 0.05% (w/v) Tween 20 and 1% (w/v) nonfat dry milk]. After incubation with primary antibody, the membranes were washed ve times with washing buffer [TBS containing 0.05% (v/v) Tween 20], incubated for 1 h at room temperature with the secondary antibody (horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin, Amersham Biosciences) at 1:3000 in dilution buffer, and washed ve times with washing buffer. Finally, antibody binding was visualized by ECL detection (Amersham Biosciences) following the instructions from the supplier, using autoradiography lm (Hyperlm ECL, Amersham Biosciences). Bands in lms were then scanned, stored as TIFF images, and analyzed by means of a densitometry analysis software (ImageMaster Total Laboratory, ver. 2.00, Amersham Biosciences). To convert relative light units (RLU; pixel intensity) into ng/mg protein, ovine COX-2 (Cayman Chemical Co.) and mouse NOS-2 peptide (a 19-amino acid peptide sequence designated INOS22-P; control peptide; 11251144 amino acids, Alpha Diagnostic International) were used as standards.
Stimuli, drugs, and chemicals
K. lactis (strain NRRL-41140) yeast cells were cultured on yeast extract peptone dextrose medium (Sigma) at 30C at a growth rate of 0.07/h, then washed with distilled water, and nally freeze-dried. Stock solution of LPS from Escherichia coli serotype 0111:B4 (Sigma) was made up at 10 mg/ml in phenol-red-free DMEM (Sigma) containing 0.584 g/l glutamine (Sigma) and stored at 20C until use. Thioglycollate broth (Merck, Darmstadt, Germany) was prepared to a concentration of 3% (w/v) in phosphate-buffered saline (PBS), autoclaved at 121C for 10 min, and stored at room temperature until use. Recombinant murine IFN- was purchased from Genzyme (Cambridge, MA). Stock solution (100 mM) of PMA (Sigma) was dissolved in dimethyl sulfoxide (DMSO) and stored in the dark at 80C until use. For preparation of c-RESV (Fig. 1), a solution of 500 mg t-RESV (Sigma) in 300 ml methanol was irradiated ( 254 nm) for 8 h. The solvent was then evaporated under reduced pressure, and the residue was puried by highpressure liquid chromatography in a reverse-phase column (Cyclobond I2000 RSP, Astec, Whippany, NJ) using 1:1 methanolwater as eluent to give an oil, c-RESV (390 mg), and a white solid, t-RESV (100 mg). Retention times (ux of 1 ml/min in column of 500 9.2 mm): c-RESV, 10.4 min; t-RESV, 27.2 min. 1 H nuclear magnetic resonance (MeOD) characterization of the c-RESV fraction: 6.11 (t, 1H, J 2.1 Hz, H-4), 6.21 (d, 2H, J 2.1 Hz, H-2 and H-6), 6.31 (d, 1H, J 12.2 Hz, H-7), 6.41 (d, 1H, J 12.2 Hz, H-8), 6.62 (d, 2H, J 8.5 Hz, H-3 and H-5 ), and 7.09 (d, 2H, J 8.5 Hz, H-2' and H-6') ppm. Infrared characterization of the c-RESV fraction: 3330, 1592, 1511, 1438, 1239, 1152, 1002, 835 cm1. Stock solutions (100 mM) of c-RESV and indomethacin (Sigma) were prepared in DMSO and stored in the dark at 80C until use. Stock solutions of the arginine analog N-monomethyl-L-arginine monoacetate (L-NMMA, Calbiochem, San Diego, CA) and L( ) ascorbic acid (Merck) were made up at 100 mM in DMEM and stored until use at 20C in the dark. HX, sodium azide, xanthine, superoxide dismutase (SOD; from bovine erythrocytes), diphenyleneiodonium chloride (DPI), allopurinol, XO (from buttermilk), sulfanilamide, and naphthylenediamine hydrochloride were all purchased from Sigma. Appropriate dilutions of the above drugs were prepared every day immediately before use in PBS (XO assays), in HBSS (NADPH oxidase assays), and/or in deionized water (for the other experiments) from the following concentrated stock solutions kept at 20C: SOD (20 kunits/ml) in deionized water, HX and xanthine (10 mM) in a 0.1% w/v aqueous KOH
Slot-blot assay
The levels of the enzymes COX-2 and NOS-2 were determined by slot-blot assay in soluble extracts. Cultures of inammatory mouse peritoneal macrophages (107 cells/ml) stimulated in vitro for 6 h in DMEM containing 10 units/ml IFN- , 100 ng/ml LPS, and c-RESV at various concentrations (1, 10, and 100 M) or without drug (controls) were incubated at 37C in a humidied 5% CO2 atmosphere. After this incubation period, cells were washed with
1158
Journal of Leukocyte Biology Volume 75, June 2004
http://www.jleukbio.org
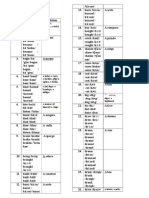
Fig. 1. Generation of c-RESV after the irradiation of t-RESV with UV light (h ).
solution; all other compounds (100 mM) in deionized water. Xanthine oxidase was dissolved daily before the experiments in PBS. Deionized water and the appropriate dilutions of the different vehicles used had no signicant, pharmacological effects in any of the tests performed in the present study. In addition, unlike t-RESV, c-RESV is a stable compound and never isomerized to the trans isomer during storage or throughout the period in which the different experiments were performed. The specic chemicals and materials used in the different tests were purchased from suppliers indicated in the corresponding references provided in Materials and Methods. All other chemicals, including the reagents used in the preparation of different buffers and physiological solutions, were of the best quality commercially available.
phages were investigated using OxyBURST Green probes, and the results are shown in Figure 2. Extracellular and intracellular ROS production in control inammatory rat macrophages were, respectively, 81 5 and 35 2 arbitrary uorescence units per min. c-RESV at concentrations of 1 M or higher signicantly inhibited PMA-induced extracellular ROS release, with an IC50 of 99 8 M (n 5; Fig. 2A). Likewise, c-RESV at concentrations of 1 M or higher signicantly inhibited K. lactis-induced intracellular ROS production, with an IC50 of 14 1.3 M (n 5; Fig. 2B).
Data presentation and statistical analysis
In gures, data are expressed as means SEM. Statistical comparisons ( 0.05) were performed by one-way ANOVA followed by the Tukey-Kramer test for multiple comparisons. The details of the expression of results are specically described in the references provided in the different Materials and Method sections. The inhibitory effects of c-RESV and some of the reference drugs are expressed (where appropriate) as IC50 (concentrations that produce a 50% inhibition), calculated by least-squares linear regression using a tting program (OriginTM 5.0, Microcal Software, Inc., Northampton, MA) of log molar concentration of the tested compound on percent of maximal pharmacological response obtained with each concentration.
O2 -scavenging capacity of c-RESV
We next investigated the ability of c-RESV to scavenge O2 generated by an enzymatic system (HXXO; Fig. 3). c-RESV itself was unable to directly reduce NBT. Control activity was 0.04 0.003 A560 units/min (n 5). This value was unaffected by c-RESV (1100 M), and consequently, it had no effect as a selective scavenger of O2 (Fig. 3). SOD (0.110 units/ml), however, was capable of removing O2 generated by the enzymatic HXXO system (Fig. 3). The IC50 value was 0.99 0.08 units/ml (n 5).
RESULTS Effects of c-RESV on ROS production by inammatory rat macrophages
The effects of c-RESV on extra- and intracellular ROS production by thioglycollate-prestimulated rat peritoneal macro-
Effects of c-RESV on XO activity
The effects of c-RESV on XO activity were investigated by measuring its effects on the production of uric acid from xanthine (assays using commercial XO; Fig. 4A) or on O2 production from xanthine as quantied by lucigeninECL (assays using rat macrophage homogenates as a source of XO; Fig.
Fig. 2. Effects of c-RESV (1100 M) on the extracellular production of ROS induced by PMA (100 ng/ml; A) and on the intracellular production of ROS induced by K. lactis cells/OxyBURST Green H2DCF complex (B) in thioglycollate-elicited rat peritoneal macrophages. L( ) ascorbic acid (0.1 mM; A) or sodium azide (1 mM; B) was used as an inhibitory reference drug. Each column represents the mean value SEM (indicated by vertical bars) for ve experiments. Asterisks indicate signicant differences (*, P 0.05, and **, P 0.01) with respect to control.
Leiro et al. Effects of cis-resveratrol on murine macrophages
1159
4B). c-RESV (1100 M) did not inhibit XO activity in either assay. By contrast, the reference XO inhibitor allopurinol at 10 M signicantly inhibited XO activity in both assays (Fig. 4).
Effects of c-RESV on NADH/NADPH oxidase activity in inammatory rat macrophage homogenates
c-RESV itself was unable to reduce lucigenin directly. NADH/ NADPH oxidase activity in control inammatory rat macrophage homogenates was 5483 411 RLU (n 5). c-RESV (10 100 M) and DPI (1100 M), a know inhibitor of NADH/NADPH oxidase, decreased NADH/NADPH oxidase activity in a concentration-dependent manner, with IC50 values of 34 3 and 28 2 M, respectively (n 5; Fig. 5).
Fig. 3. O2 scavenging activity of c-RESV (1100 M) and the reference scavenger SOD (0.110 units/ml) in assays in which O2 was generated by the enzymatic HX/XO system. Values shown are means SEM (n 5). *, P 0.01, with respect to control values. A560nm, Absorbance at 560 nm.
Effects of c-RESV on RNS production by inammatory rat macrophages stimulated with LPS and IFNRat peritoneal macrophages elicited in vivo with thioglycollate and stimulated in vitro for 48 h with LPS and IFN- were incubated in the presence or absence of c-RESV (1100 M). L-NMMA at 250 M was used as reference inhibitor of NO production. Cultures incubated with 10 or 100 M c-RESV showed delayed and signicantly reduced nitrite production, with an IC50 of 39 3 M (n 5; Fig. 6).
Effects of c-RESV on PGE2 production by inammatory rat macrophages stimulated with LPS and IFNWe next investigated whether c-RESV inhibits the induction by LPS and IFN- of PGE2 production in rat peritoneal macrophages. The synthesis of this active product of the COX pathway was inhibited by c-RESV (10 100 M) and by the nonselective inhibitor of COX expression and COX enzymatic activity indomethacin at 30 M (Fig. 7).
Fig. 4. Effects of c-RESV (1100 M) and the XO inhibitor allopurinol (10 M) on production of uric acid by XO in the presence of 100 M xanthine (A) or on O2 production from xanthine as quantied by lucigeninECL (B). Assays (A) were performed in vitro with commercial XO; assays (B) with an inammatory rat macrophage homogenate as a source of XO. Values shown are mean SEM (n 5). *, P 0.01, with respect to control.
Fig. 5. Effects of c-RESV (1100 M) and DPI (1100 M) NADH/NADPH oxidase activity (using NADPH 100 M as substrate) in thioglycollate-elicited rat peritoneal macrophage homogenates as quantied by lucigeninECL. Values shown are mean SEM (n 5). *, P 0.01, with respect to control values.
1160
Journal of Leukocyte Biology Volume 75, June 2004
http://www.jleukbio.org
Fig. 6. In vitro effects of c-RESV (1100 M) and the NOS-2 inhibitor L-NMMA (250 M) on NO levels in supernatants of 48 h cultures of inammatory rat peritoneal macrophages stimulated with 100 ng/ml LPS and 10 units/ml IFN- . Values shown are means SEM (n 5). *, P 0.01, with respect to control.
Effects of c-RESV on NOS-2 and COX-2 mRNA levels
To determine whether the above effects on NO and PGE2 production are related to inhibitory effects in NOS-2 and COX-2 mRNA synthesis, we used a semiquantitative RT-PCR assay applied to RNA extracted from inammatory rat peritoneal macrophages stimulated with LPS and IFN- . Treatment with c-RESV (100 M) signicantly reduced levels of NOS-2 and COX-2 mRNA in the macrophage extracts (Fig. 8).
Effects of c-RESV on synthesis of NOS-2 and COX-2
To determine the effect of c-RESV on NOS-2 and COX-2 protein levels in inammatory peritoneal macrophages, a slotblot analysis was used. As the corresponding rat antibodies are not commercially available (as far as we know) in these experiments, we used mouse peritoneal macrophages in place of rat macrophages. Treatment of LPS/IFN- -stimulated, inammatory macrophages with c-RESV (10 100 M) signicantly reduced the levels of NOS-2 (Fig. 9A) and COX-2 (Fig. 9B).
concentration-dependently inhibited extracellular and intracellular ROS production by inammatory peritoneal macrophages at concentrations as low as 1 M (i.e., it exhibited a typical antioxidant activity). Within the same range of concentrations (110 M), t-RESV also inhibits ROS production by inammatory rat peritoneal macrophages [28]. The above results may be attributable to effects on enzyme activities (XO and/or NADH/NADPH oxidase) or to direct scavenging of O2 by c-RESV. We therefore rst evaluated the O2 -scavenging capacity of c-RESV, using the enzymatic HXXO system. O2 produced in this system reduces NBT to produce the colored compound formazan, which can be quantied spectrophotometrically as a measure of O2 level [6]; in this assay system, c-RESV, like t-RESV [6], did not scavenge O2 . In view of these negative results, we investigated the possible effects of c-RESV on XO and/or NADH/NADPH oxidase enzymatic activity. Like t-RESV (see ref. [6]), c-RESV did not modify the production of uric acid from xanthine (assays using commercial XO). In addition, c-RESV had no effects on O2 generation from xanthine, as specically quantied in the present study by lucigeninECL (assays using rat macrophage homogenates as source of XO). These data demonstrate that c-RESV does not affect XO activity. By contrast, c-RESV inhibited NADH/NADPH oxidase enzymatic activity, i.e., the specic chemiluminescence signal emitted by the reaction between lucigenin and O2 generated from NADPH, in inammated rat macrophage extracts. These results indicate that the decrease of this enzymatic activity may be responsible, at least in part, for the inhibitory effects of c-RESV on ROS production. Similar effects on NADH/NADPH oxidase have been described previously for t-RESV in rat aortic homogenates [6]. Stimulation of murine macrophages with bacterial wall components (LPS) and IFN- induces them to express large
DISCUSSION
In this study, we have investigated for the rst time the effects of c-RESV on inammatory murine macrophage function. During respiratory burst, macrophages produce and release large amounts of ROS and RNS, which play a role in the destruction of infectious agents; however, current evidence strongly indicates that activated macrophages are also involved in different steps of coronary heart disease (see Introduction) as well as in many inammatory processes. K. lactis and PMA rapidly stimulate macrophages to produce ROS [28, 31, 32] through stimulation of NADH/NADPH oxidase and/or XO enzymatic activity (see Introduction). c-RESV
Fig. 7. Effects of c-RESV (1100 M) and indomethacin (30 M, a known, nonselective inhibitor of COX expression and COX enzymatic activity) on PGE2 production by inammatory rat peritoneal macrophages stimulated with 100 ng/ml LPS and 10 units/ml IFN- for 3 h. Values shown are means SEM (n 5). *, P 0.05, and **, P 0.01, with respect to untreated control cells.
Leiro et al. Effects of cis-resveratrol on murine macrophages
1161
Fig. 8. Effects of c-RESV (10 100 M) on NOS-2 and COX-2 mRNA levels in inammatory rat peritoneal macrophages, as determined by semiquantitative RT-PCR. Macrophages were stimulated in vitro with LPS (100 ng/ml) and IFN- (10 units/ml). (A) Agarose analysis (2%) of RT-PCR products using primers for NOS-2 (519 bp), COX-2 (345 bp), or the housekeeping gene GADPH (544 bp). (B) Densitometric quantication of normalized RT-PCR products of NOS-2 and COX-2 [optical density (OD) of enzyme band/OD of corresponding band in analysis using primer for GADPH]. Values are means SEM (n 5). *, P 0.01, with respect to control values. Mw, Molecular weight markers (100 bp ladder).
amounts of NOS-2, which leads to a strong, endogenous NO production [33, 34]. This NO production is abrogated by 10 100 M c-RESV (present results). Over the same concentration range, t-RESV likewise inhibits the production of nitrogen intermediates by inammatory rat macrophages stimulated with LPS and IFN- [28]. Activation of murine macrophages with LPS and IFNinduces COX-2 expression and markedly increases PGE2 production [35], which is a potent mediator of inammation and cell proliferation [36]. In the present study, treatment of LPS/IFN- -stimulated inammatory peritoneal macrophages with c-RESV inhibited PGE2 production, although only at concentrations of 10 M or more. Similar results have been reported previously for t-RESV in mouse macrophages [37] and murine 3T6 broblast [38], which may explain, at least in part, the inhibition of the 3T6 broblast growth produced by this RESV isomer [38]. To investigate whether the above inhibitory effect of c-RESV on RNS and PGE2 production may be related (at least in part) to an action on NOS-2/COX-2 gene or protein expression, we also studied the potential effects of c-RESV on NOS-2/COX-2 mRNA and protein levels. Our results show that c-RESV at 100 M inhibits NOS-2 and COX-2 mRNA production (determined by semiquantitative RT-PCR) in inammatory rat peritoneal macrophages, and c-RESV at 10 100 M inhibits NOS-2 and COX-2 protein synthesis (determined by slot-blot
1162 Journal of Leukocyte Biology Volume 75, June 2004
assay) in inammatory mouse peritoneal macrophages treated with LPS and IFN- . This apparent difference in effective inhibitory concentrations may be a result of the different animal models used (for justication of the choice of mouse macrophages in place of rat macrophages for the determination of NOS-2/COX-2 protein synthesis, see Results). Similar inhibitory effects have been described previously for t-RESV on NOS-2 mRNA levels [39, 40] and on COX-2 enzyme expression [37] in mouse macrophages. Taking into account that several studies have proposed a positive modulatory role of PGE2 (see, e.g., ref. [41]) and ROS [37, 42] on NOS-2 induction in murine macrophages, the inhibitory effects of c-RESV on NOS-2 mRNA and protein levels could be related, at least in part, to the ability of this RESV isomer for decreasing the production of ROS and PGE2. Furthermore, as previous studies have shown that NO is necessary for maintaining prolonged COX-2 gene expression (see, e.g., ref. [35]), the action of c-RESV on RNS production observed in the present study could be responsible, at least in part, for the effects of this natural compound on COX-2 mRNA and enzyme levels. Moreover, in the same way as t-RESV in mice [39, 43, 44] or in humans (see, e.g., ref. [45]), the action of the c-RESV on NOS/COX-2 gene and protein expression described above could be mediated by an inhibition of the nuclear factor- B (NF- B) activation, mainly as a result of the inhibition of the
http://www.jleukbio.org
Fig. 9. Effects of c-RESV (1100 M) on NOS-2 and COX-2 protein expression in inammatory mouse peritoneal macrophages stimulated with LPS (100 ng/ml) and IFN- (10 units/ml). Levels of NOS-2 (A) and COX-2 (B) were determined after 6 h of incubation by slot-blot assay; the gure shows a representative blot. Values shown are means SEM (n 5), expressed as ng enzyme per mg protein in the macrophage extract. *P 0.01 with respect to control.
degradation of inhibitor of B (I B ). The precise effects of c-RESV on the NF- B signaling pathway are currently being evaluated in our laboratory, basically using a DNA hybridization array containing 96 NF- B-related genes. The preliminary results obtained in these experiments (data not shown) indicate that c-RESV produces an increase of the I B gene expression and a down-regulation of two genes of the NF- B family, NF- B1 and NF- B2. In summary, our data indicate that c-RESV at micromolar concentrations signicantly attenuates several components of the macrophage response to proinammatory stimuli. Specically, c-RESV blocks O2 production by inammatory macrophages (by inhibition of NADPH/NADPH oxidase activity) and inhibits the production of the proinammatory mediators NO and PGE2 (at least in part by inhibition of NOS-2 and COX-2 gene and protein expression). These inhibitory effects on the inammatory response are qualitatively similar to those previously observed for t-RESV. Therefore, the different spatial conformation of c-RESV (vs. that of the trans isomer, see Fig. 1) does not seem to modify markedly its interaction with the potential cellular targets. As noted in Introduction, because of its effects on macrophage function and on other cell types, t-RESV has been implicated in the protection induced by the prolonged consumption of moderate amounts of wine, especially of red wine, against the incidence of cardiovascular diseases (mainly cor-
onary heart disease). In this context, it has been described previously that the t-RESV concentrations reached in plasma and tissues after the oral administration of this natural compound to rats and humans seem to approach the in vitro active concentrations; an average drinker of wine can, particularly in the long term, absorb a sufcient amount of RESV to explain the benecial effect of red wine on health (see, e.g., refs. [46, 47]). In addition, it is interesting to point out (see also Introduction) that an increased macrophage activation (e.g., through, among others, overproduction of ROS and RNS, abnormally high NADH/NADPH oxidase, NOS-2, and/or COX-2 activities) has been observed in different steps of coronary heart disease and in a number of inammatory processes (including atherosclerosis). Bearing in mind the above considerations and assuming that c-RESV shows a similar behavior in humans, our results suggest that the benecial cardioprotective effects of consumption of foods and beverages containing RESV (notably red wine) may thus be a result of the combined effects of the two isomers. Finally, taking into account the pharmacological properties described for c-RESV in the present study, it can also be concluded that this natural polyphenol may have value as a structural model for the design and subsequent development of new drugs useful for improving the pharmacological treatment
1163
Leiro et al. Effects of cis-resveratrol on murine macrophages
of inammatory diseases involving hyper-responsiveness of phagocytic cells.
ACKNOWLEDGMENTS
This work was supported in part by grants from the Comision Interministerial de Ciencia y Tecnologa (CICYT; Spain; SAF2000-0137 and SAF2002-02645), the Consellera de Edu cacion e Ordenacion Universitaria, Xunta de Galicia (Spain; PGIDIT02BTF20301PR and PGIDIT02PXIC20305PN), and Almirall Prodesfarma Laboratories (Spain). In addition, this study was awarded with the 2003 prize of the Spanish Pharmacological Society and Almirall Prodesfarma Laboratories.
REFERENCES
1. Renaud, S., de Lorgeril, M. (1992) Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 339, 15231526. 2. Duffy, S. J., Vita, J. A. (2003) Effects of phenolics on vascular endothelial function. Curr. Opin. Lipidol. 14, 2127. 3. Soleas, G. J., Diamandis, E. P., Goldberg, D. M. (2001) The world of resveratrol. Adv. Exp. Med. Biol. 492, 159 182. 4. Soleas, G. J., Diamandis, E. P., Goldberg, D. M. (1997) Resveratrol: a molecule whose time has come? And gone? Clin. Biochem. 30, 91113. 5. Burns, J., Gardner, P.T., ONeil, J., Craeford, S., Morecroft, I., Mcphail, D. B., Lister, C., Matthews, D., Mclean, M. R., Lean, M. E. J., Duthie, G. G., Crozier, A. (2000) Relationship among antioxidant activity, vasodilatation capacity, and phenolic content of red wines. J. Agric. Food Chem. 48, 220 230. 6. Orallo, F., Alvarez, E., Camina, M., Leiro, J. M., Gomez, E., Fernandez, P. (2002) The possible implication of trans-resveratrol in the cardioprotective effects of long-term moderate wine consumption. Mol. Pharmacol. 61, 294 302. 7. Wu, J. M., Wang, Z. R., Hsieh, T. C., Bruder, J. L., Zou, J. G., Huang, Y. Z. (2001) Mechanism of cardioprotection by resveratrol, a phenolic antioxidant present in red wine. Int. J. Mol. Med. 8, 317. 8. Bertelli, A. A., Giovannini, L., Bernini, W., Migliori, M., Fregoni, M., Bavaresco, L., Bertelli, A. (1996) Antiplatelet activity of cis-resveratrol. Drugs Exp. Clin. Res. 22, 61 63. 9. Waffo-Teguo, P., Hawthorne, M. E., Cuendet, M., Merillon, J. M., Kinghorn, A. D., Pezzuto, J. M., Mehta, R. G. (2001) Potential cancerchemopreventive activities of wine stilbenoids and avans extracted from grape (Vitis vinifera) cell cultures. Nutr. Cancer 40, 173179. 10. Shepherd, V. L. (1986) The role of the respiratory burst of phagocytes in host defense. Semin. Respir. Infect. 1, 99 106. 11. Forman, H. J., Torres, M. (2002) Reactive oxygen species and cell signaling: respiratory burst in macrophage signaling. Am. J. Respir. Crit. Care Med. 166, S4 S8. 12. Rinaldo, J. E., Clark, M., Parinello, J., Shepherd, V. L. (1994) Nitric oxide inactivates xanthine dehydrogenase and xanthine oxidase in interferon- stimulated macrophages. Am. J. Respir. Cell Mol. Biol. 11, 625 630. 13. Cos, P., Ying, L., Calomme, M., Hu, J. P., Cimanga, K., Van Poel, B., Pieters, L., Vlietinck, A. J., Berghe, D. V. (1998) Structure-activity relationship and classication of avonoids as inhibitors of xanthine oxidase and superoxide scavengers. J. Nat. Prod. 61, 7176. 14. Dusting, G. J., Fennessy, P., Yin, Z. L., Gurevich, V. (1998) Nitric oxide in atherosclerosis: vascular protector or villain? Clin. Exp. Pharmacol. Physiol. Suppl. 25, S34 S41. 15. Floyd, R. A. (1999) Antioxidants, oxidative stress, and degenerative neurological disorders. Proc. Soc. Exp. Biol. Med. 222, 236 245. 16. Agostini, M., Di Marco, B., Nocentini, G., Delno, D. V. (2002) Oxidative stress and apoptosis in immune diseases. Int. J. Immunopathol. Pharmacol. 15, 157164. 17. Chernajovsky, Y., Winyard, P. G., Kabouridis, P. S. (2002) Advances in understanding the genetic basis of rheumatoid arthritis and osteoarthritis: implications for therapy. Am. J. Pharmacogenomics 2, 223234. 18. Comhair, S. A., Erzurum, S. C. (2002) Antioxidant responses to oxidantmediated lung diseases. Am. J. Physiol. Lung Cell. Mol. Physiol. 283, L246 L255.
19. Knight, J. A. (2000) Review: free radicals, antioxidants, and the immune system. Ann. Clin. Lab. Sci. 30, 145158. 20. Weinberg, J. B. (2000) Nitric oxide synthase 2 and cyclooxygenase 2 interactions in inammation. Immunol. Res. 22, 319 341. 21. Mazzone, A., De Servi, S., Ricevuti, G., Mazzucchelli, I., Fossati, G., Pasotti, D., Bramucci, E., Angoli, L., Marsico, F., Specchia, G., Notario, A. (1993) Increased expression of neutrophil and monocyte adhesion molecules in unstable coronary artery disease. Circulation 88, 358 363. 22. Auer, J., Berent, R., Labetanig, E., Eber, B. (2001) Serum neopterin and activity of coronary artery disease. Heart Dis. 3, 297301. 23. Ikeda, U., Matsui, K., Murakami, Y., Shimada, K. (2002) Monocyte chemoattractant protein-1 and coronary artery disease. Clin. Cardiol. 25, 143147. 24. Wallerath, T., Deckert, G., Ternes, T., Anderson, H., Li, H., Witte, K., Forstermann, U. (2002) Resveratrol, a polyphenolic phytoalexin present in red wine, enhances expression and activity of endothelial nitric oxide synthase. Circulation 106, 16521658. 25. Leiro, J., Iglesias, R., Parama, A., Sanmartn, M. L., Ubeira, F. M. (2001) Respiratory burst responses of rat macrophages to microsporidian spores. Exp. Parasitol. 98, 19. 26. Leiro, J. M., Alvarez, E., Arranz, J. A., Siso, I. G., Orallo, F. (2003) In vitro effects of mangiferin on superoxide concentrations and expression of the inducible nitric oxide synthase, tumour necrosis factor- and transforming growth factor- genes. Biochem. Pharmacol. 65, 1361 1371. 27. Strober, W. (1997) Wright-Giemsa and nonspecic esterase staining of cells. In Current Protocols in Immunology, vol. 3 (J. E. Coligan, A. M. Kruissbeek, D. H. Margulies, E. M. Shevach, W. Strober, eds.), New York, NY, John Wiley & Sons, A.3C.1A.3C.2. 28. Leiro, J., Alvarez, E., Garca, D., Orallo, F. (2002) Resveratrol modulates rat macrophage functions. Int. Immunopharmacol. 2, 767774. 29. Kato, M., Nishida, S., Kitasato, H., Sakata, N., Kawai, S. (2001) Cyclooxygenase-1 and cyclooxygenase-2 selectivity of non-steroidal anti-inammatory drugs: investigation using human peripheral monocytes. J. Pharm. Pharmacol. 53, 1679 1685. 30. Bradford, M. M. (1976) A rapid and sensitive method for the quantication of microgram quantitites of protein using the principle of protein-dye binding. Anal. Biochem. 72, 248 254. 31. Alvarez, E., Leiro, J., Orallo, F. (2002) Effect of ()-epigallocatechin-3gallate on respiratory burst of rat macrophages. Int. Immunopharmacol. 2, 849 855. 32. Garca, D., Delgado, R., Ubeira, F. M., Leiro, J. (2002) Modulation of rat macrophage function by the Mangifera indica L. extracts Vimang and mangiferin. Int. Immunopharmacol. 2, 797 806. 33. Virgili, F., Kobuchi, H., Packer, L. (1998) Procyanidins extracted from Pinus maritima (pycnogenol): scavengers of free radical species and modulators of nitrogen monoxide metabolism in activated murine RAW 264.7 macrophages. Free Radic. Biol. Med. 24, 1120 1129. 34. Ferret, P. J., Soum, E., Negre, O., Fradelizi, D. (2002) Auto-protective redox buffering systems in stimulated macrophages. BMC Immunol. 3, 3. 35. Perkins, D. J., Kniss, D. A. (1999) Blockade of nitric oxide formation down-regulates cyclooxygenase-2 and decreases PGE2 biosynthesis in macrophages. J. Leukoc. Biol. 65, 792799. 36. Bagga, D., Wang, L., Farias-Eisner, R., Glaspy, J. A., Reddy, S. T. (2003) Differential effects of prostaglandin derived from -6 and -3 polyunsaturated fatty acids on COX-2 expression and IL-6 secretion. Proc. Natl. Acad. Sci. USA 100, 17511756. 37. Martnez, J., Moreno, J. J. (2000) Effect of resveratrol, a natural polyphe nolic compound, on reactive oxygen species and prostaglandin production. Biochem. Pharmacol. 59, 865 870. 38. Moreno, J. J. (2000) Resveratrol modulates arachidonic acid release, prostaglandin synthesis, and 3T6 broblast growth. J. Pharmacol. Exp. Ther. 294, 333338. 39. Tsai, S. H., Lin-Shiau, S. Y., Lin, J. K. (1999) Suppression of nitric oxide synthase and the down-regulation of the activation of NF B in macrophages by resveratrol. Br. J. Pharmacol. 126, 673 680. 40. Chan, M. M., Mattiacci, J. A., Hwang, H. S., Shah, A., Fong, D. (2000) Synergy between ethanol and grape polyphenols, quercetin, and resveratrol, in the inhibition of the inducible nitric oxide synthase pathway. Biochem. Pharmacol. 60, 1539 1548. 41. Chen, B. C., Lin, W. W. (2000) Pyrimidinoceptor potentiation of macrophage PGE2 release involved in the induction of nitric oxide synthase. Br. J. Pharmacol. 130, 777786.
1164
Journal of Leukocyte Biology Volume 75, June 2004
http://www.jleukbio.org
42. Martnez, J., Sanchez, T., Moreno, J. J. (2000) Regulation of prostaglandin E2 production by the superoxide radical and nitric oxide in mouse peritoneal macrophages. Free Radic. Res. 32, 303311. 43. Wadsworth, T. L., Koop, D. R. (1999) Effects of the wine polyphenolics quercetin and resveratrol on pro-inammatory cytokine expression in RAW 264.7 macrophages. Biochem. Pharmacol. 57, 941949. 44. Murakami, A., Matsumoto, K., Koshimizu, K., Ohigashi, H. (2003) Effects of selected food factors with chemopreventive properties on combined lipopolysaccharide- and interferon- -induced I B degradation in RAW264.7 macrophages. Cancer Lett. 195, 1725.
45. Adhami, V. M., Afaq, F., Ahmad, N. (2003) Suppression of ultraviolet B exposure-mediated activation of NF- B in normal human keratinocytes by resveratrol. Neoplasia 5, 74 82. 46. Bertelli, A., Bertelli, A. A. E., Gozzini, A., Giovannini, L. (1998) Plasma and tissue resveratrol concentrations and pharmacological activity. Drugs Exp. Clin. Res. 24, 133138. 47. Soleas, G. J., Yan, J., Goldberg, D. M. (2001) Ultrasensitive assay for three polyphenols (catechin, quercetin and resveratrol) and their conjugates in biological uids utilizing gas chromatography with mass selective detection. J. Chromatogr. B Biomed. Sci. Appl. 757, 161172.
Leiro et al. Effects of cis-resveratrol on murine macrophages
1165
Das könnte Ihnen auch gefallen
- 83Dokument7 Seiten83Sava1988Noch keine Bewertungen
- NinhydrinDokument26 SeitenNinhydrinSava1988Noch keine Bewertungen
- RW A Review On 13 Thiazolidin 4 OnesDokument10 SeitenRW A Review On 13 Thiazolidin 4 OnesSava1988Noch keine Bewertungen
- Molecular Properties Impact Oral Drug AbsorptionDokument21 SeitenMolecular Properties Impact Oral Drug AbsorptionSava1988100% (1)
- Dissolution Testing (Kel 3)Dokument28 SeitenDissolution Testing (Kel 3)Anonymous QEVAyPMNoch keine Bewertungen
- A Convenient and Efficeint Synthesis of Thiazolidin 4 Ones Via Ciclization of Substituted HidrazinecarbathioamidesDokument6 SeitenA Convenient and Efficeint Synthesis of Thiazolidin 4 Ones Via Ciclization of Substituted HidrazinecarbathioamidesSava1988Noch keine Bewertungen
- NinhydrinDokument26 SeitenNinhydrinSava1988Noch keine Bewertungen
- A Bate, A Măcina, A Strivi: Vt/viDokument5 SeitenA Bate, A Măcina, A Strivi: Vt/viElisaveta VicleanuNoch keine Bewertungen
- IndometacinDokument47 SeitenIndometacinSava1988Noch keine Bewertungen
- Design, Synthesis and Evalutation of Novel Indomethacin Antioxidant CodrugsDokument10 SeitenDesign, Synthesis and Evalutation of Novel Indomethacin Antioxidant CodrugsSava1988Noch keine Bewertungen
- Chapter 01. Introduction To Biopharmaceutics and Its Role in Drug DevelopmentDokument25 SeitenChapter 01. Introduction To Biopharmaceutics and Its Role in Drug DevelopmentSava19880% (1)
- Structure-Activity Relationship of Indomethacin Analogues ForDokument10 SeitenStructure-Activity Relationship of Indomethacin Analogues ForSava1988Noch keine Bewertungen
- Designing Safer NSAIDs: Synthesis of Indomethacin-Flavonoid ConjugatesDokument8 SeitenDesigning Safer NSAIDs: Synthesis of Indomethacin-Flavonoid ConjugatesSava1988Noch keine Bewertungen
- Evalutation of Glycolamide Esters of Indomethacin As Potentioal COX2Dokument14 SeitenEvalutation of Glycolamide Esters of Indomethacin As Potentioal COX2Sava1988Noch keine Bewertungen
- Conversion of Tryptophab To Indole 3 Acetic AcidDokument7 SeitenConversion of Tryptophab To Indole 3 Acetic AcidSava1988Noch keine Bewertungen
- Akt 1Dokument11 SeitenAkt 1Sava1988Noch keine Bewertungen
- Analysis of Recent Pharmaceutical Regulatory Documents On Analytical Method ValidationDokument16 SeitenAnalysis of Recent Pharmaceutical Regulatory Documents On Analytical Method ValidationSava1988Noch keine Bewertungen
- Sinteza IndometacinDokument18 SeitenSinteza IndometacinSava1988Noch keine Bewertungen
- 101 Full PDFDokument9 Seiten101 Full PDFSava1988Noch keine Bewertungen
- Emodin Negatively Affects The Phosphoinositide 3-kinase/AKT Signalling Pathway: A Study On Its Mechanism of ActionDokument11 SeitenEmodin Negatively Affects The Phosphoinositide 3-kinase/AKT Signalling Pathway: A Study On Its Mechanism of ActionSava1988Noch keine Bewertungen
- Alfa TomatinaDokument11 SeitenAlfa TomatinaSava1988Noch keine Bewertungen
- Flavonoide Si Sist ImunDokument14 SeitenFlavonoide Si Sist ImunSava1988Noch keine Bewertungen
- Ejaculare PrecoceDokument6 SeitenEjaculare PrecoceSava1988Noch keine Bewertungen
- Pi 3 KDokument8 SeitenPi 3 KSava1988Noch keine Bewertungen
- Mechanism of Actions Ofcarbamazepine and DerivatesDokument10 SeitenMechanism of Actions Ofcarbamazepine and DerivatesSava1988Noch keine Bewertungen
- DesloratadinaDokument3 SeitenDesloratadinaSava1988Noch keine Bewertungen
- 101 Full PDFDokument9 Seiten101 Full PDFSava1988Noch keine Bewertungen
- Oral Analgesics For Chronic Low Back PainDokument7 SeitenOral Analgesics For Chronic Low Back PainSava1988Noch keine Bewertungen
- 101 Full PDFDokument9 Seiten101 Full PDFSava1988Noch keine Bewertungen
- MisoprostolDokument7 SeitenMisoprostolSava1988Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Methyl Paraben Potentiates UV Damage 2Dokument13 SeitenMethyl Paraben Potentiates UV Damage 2Trevor SteynNoch keine Bewertungen
- Protective Effect of Captopril Against Cisplatin-Induced Nephrotoxicity in RatsDokument7 SeitenProtective Effect of Captopril Against Cisplatin-Induced Nephrotoxicity in RatsMad MadNoch keine Bewertungen
- Preparation, Characterization, and Antioxidant Properties of GallicDokument6 SeitenPreparation, Characterization, and Antioxidant Properties of GallicAnonymous xGc8MRRysNoch keine Bewertungen
- Stress Responses in PlantsDokument293 SeitenStress Responses in PlantsIonela RădulescuNoch keine Bewertungen
- Dec 2020Dokument16 SeitenDec 2020Saurabh AgarwalNoch keine Bewertungen
- Anticancer Effect of Alkaline Reduced WaterDokument4 SeitenAnticancer Effect of Alkaline Reduced WatersarasNoch keine Bewertungen
- EXCLUSIV Medecine Univ - Blogspot.com Berek and Novak S GynecologyDokument11 SeitenEXCLUSIV Medecine Univ - Blogspot.com Berek and Novak S GynecologyIan Ervan SimanungkalitNoch keine Bewertungen
- Mechanisms of Drug-Induced HepatotoxicityDokument20 SeitenMechanisms of Drug-Induced Hepatotoxicityfebri kusuma arfiskaNoch keine Bewertungen
- Micronutrients Limiting Pasture Production in Australia: Crop and Pasture Science December 2019Dokument13 SeitenMicronutrients Limiting Pasture Production in Australia: Crop and Pasture Science December 2019RAJ KUMARNoch keine Bewertungen
- The Mechanisms and Application of Cryoprotectants in Aquatic Products, An OverviewDokument10 SeitenThe Mechanisms and Application of Cryoprotectants in Aquatic Products, An Overview브리엘Noch keine Bewertungen
- Diabet Zaharat-Adriana Ciobanu 0753590863Dokument8 SeitenDiabet Zaharat-Adriana Ciobanu 0753590863Adriana CiobanuNoch keine Bewertungen
- A Review of Hydrogen As A New Medical TherapyDokument8 SeitenA Review of Hydrogen As A New Medical TherapyfooykokNoch keine Bewertungen
- Wbi15-01-Jan-2023 Scientific ArticleDokument4 SeitenWbi15-01-Jan-2023 Scientific ArticleCindy TsumaNoch keine Bewertungen
- Ajinomoto - Leaflet An Historic Perspective On Tannin Use - v1.0 - 2010 - CópiaDokument7 SeitenAjinomoto - Leaflet An Historic Perspective On Tannin Use - v1.0 - 2010 - CópiaMiguelNoch keine Bewertungen
- Ccid 8 239Dokument10 SeitenCcid 8 239Marfatul ArifahNoch keine Bewertungen
- Redox and Cancer BookDokument183 SeitenRedox and Cancer BookGabriel ParejoNoch keine Bewertungen
- Accepted Manuscript: Carica PapayaDokument26 SeitenAccepted Manuscript: Carica PapayaAl Bukhari SubulussalamNoch keine Bewertungen
- Mechanisms of salt tolerance in banana revealed by gene expressionDokument8 SeitenMechanisms of salt tolerance in banana revealed by gene expressionJavier Cobos MoraNoch keine Bewertungen
- Drug Induced Liver Injury: An UpdateDokument27 SeitenDrug Induced Liver Injury: An UpdateMari QcNoch keine Bewertungen
- Cancer Simplified Lighter VersionDokument33 SeitenCancer Simplified Lighter VersionRama KrisnaNoch keine Bewertungen
- Dopamine D3 Receptor - A Neglected Participant in Parkinson Disease Pathogenesis and Treatment?Dokument45 SeitenDopamine D3 Receptor - A Neglected Participant in Parkinson Disease Pathogenesis and Treatment?Daniel TorresNoch keine Bewertungen
- Ivermectin Potential Anticancer DrugDokument11 SeitenIvermectin Potential Anticancer DrugJesus Bueno MorenoNoch keine Bewertungen
- Materials 14 04135 v2Dokument54 SeitenMaterials 14 04135 v2Kareem AldalyNoch keine Bewertungen
- Capitulo SupercriticoDokument27 SeitenCapitulo SupercriticoJavier Andres Davila RinconNoch keine Bewertungen
- Structures of Astaxanthin and Their Consequences For Therapeutic ApplicationDokument16 SeitenStructures of Astaxanthin and Their Consequences For Therapeutic ApplicationHelenaNoch keine Bewertungen
- Potent Half-Sandwich Iridium (III) and Ruthenium (II) Anticancer Complexes Containing A P O-Chelated LigandDokument10 SeitenPotent Half-Sandwich Iridium (III) and Ruthenium (II) Anticancer Complexes Containing A P O-Chelated LigandFernandaIbarraVázquezNoch keine Bewertungen
- Biochemical Energy ProductionDokument58 SeitenBiochemical Energy ProductionAlyana GabiniNoch keine Bewertungen
- The Nine Hallmarks of AgingDokument47 SeitenThe Nine Hallmarks of AgingNatalia Macarena López López100% (1)
- Malunggay MonographDokument9 SeitenMalunggay Monographkiara4decenaNoch keine Bewertungen
- (Advances in Parasitology 82) D. Rollinson (Eds.) - Academic Press, Elsevier (2013)Dokument358 Seiten(Advances in Parasitology 82) D. Rollinson (Eds.) - Academic Press, Elsevier (2013)Stoian GoranovNoch keine Bewertungen