Beruflich Dokumente
Kultur Dokumente
Cardiac Muscle: - Cardiac Muscle Tissue: Cardiac Myocyte
Hochgeladen von
mcwnotes0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
183 Ansichten4 SeitenCardiac myocytes are surrounded by a basal lamina, similar to skeletal muscle. They are involuntary and have 1-2 nuclei per cell (not 100's) High levels of MB-creatine kinase indicative of a heart attach. Myocytes also have a Few t-tubules, smaller than ventricular myocytes. Myofibrils are barely discernable.
Originalbeschreibung:
Originaltitel
Cardiac Muscle: • Cardiac Muscle Tissue: ○ Cardiac Myocyte
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
DOCX oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCardiac myocytes are surrounded by a basal lamina, similar to skeletal muscle. They are involuntary and have 1-2 nuclei per cell (not 100's) High levels of MB-creatine kinase indicative of a heart attach. Myocytes also have a Few t-tubules, smaller than ventricular myocytes. Myofibrils are barely discernable.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als DOCX herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
183 Ansichten4 SeitenCardiac Muscle: - Cardiac Muscle Tissue: Cardiac Myocyte
Hochgeladen von
mcwnotesCardiac myocytes are surrounded by a basal lamina, similar to skeletal muscle. They are involuntary and have 1-2 nuclei per cell (not 100's) High levels of MB-creatine kinase indicative of a heart attach. Myocytes also have a Few t-tubules, smaller than ventricular myocytes. Myofibrils are barely discernable.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als DOCX herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 4
Cardiac Muscle:
• Cardiac Muscle Tissue:
○ Cardiac Myocyte
○ Endothelia cells
Referred to as endocardium
○ Cardiac fibroblasts
• Cardiac Myocyte:
○ Features similar to Skeletal Muscle:
Each cardiac myocytes is surrounded by a basal lamina
Striated
Similar mechanism of contraction
○ Features different from skeletal muscle:
Involuntary
Smaller (Micrometers, not millimeters)
Nucleus is centrally located
• 1-2 nuclei per cell (not 100’s)
Cardiac cells bifurcate
Highly vascularized
MB-creatine kinase (compared to MM-creatine kinase)
• High levels are indicative of a heart attach
Cross-striations faint
Myofibrils are barely discernable
○ Differences at the electron microscopic level
Highly enriched in glycogen, myoglobin and mitochondria
Triads are replaced with dyads:
• Located at the Z-line (not A-I jxn)
Intercalated discs (know ultrastructure)
• Intercellular attachments cause cardiac myocytes to work
together
• Behaves like a synctium but isn’t
• Transverse part:
○ Transmits force of contraction
○ Half a z band, consists of:
A fascia adherens (does not encircle cell)
Desmosome (macula adherens)
○ Actin filaments butt into half Z bands (reminiscent
of zonaula adherens)
N-cadherins are present
• Lateral Part:
○ Of the intercalated disk fxns in cell-cell signaling:
Via nexuses (gap jxns)
• Maintain rhythmicity of heatbeat
• Made up of connexins
○ Has desmosomes
• Regional differences among cardiac myocytes:
○ Atrium:
Fewer t-tubules, smaller than ventricular myocytes
Atrial Natriuretic Factor
• Membrane-bound granules near nuclei
• Causes kidney to excrete water and sodium
Right Atrium
• SA and AV nodes
○ Nodal myocytes are very small and embedded in
dense CT
○ Few myofibrils and are adapted for impulse
propagation
AV bundle of his
• Large purkinje myocytes
• Few myofibrils
• Copious glycogen
• Inconspicuous intercalated discs
• Development of purkinje fibers
○ Endothelia cells in coronary arteries secrete endothelin
Induces cardiac myocytes to differentiate into purkinje cell fibers
• Endocardium
○ Lining of cardiac endothelial cells
○ Simple squamous epithelium
○ Lines all chambers of the heart
○ Continuous with endothelium lining the vascular system
• Cardiac fibroblasts
○ Most abundant cell type in the heart
• Cardiac Mycocyte Energy Requirements:
○ Triglycerides are major fuel
Stored in membrane bound lipid droplets near nucleus
Cardiac myofibers occupied by mitochondria
• 20X higher than skeletal muscle
Heart continuously operates as an aerobic organ
• High myoglobin, mitochondria and rich vascular supply
enable this.
• Clinically relevant differences between cardiac and skeletal myocytes:
○ MB-CK, high serum levels of this enzyme is diagnostic of a myocardial
infarction
Located in M line
○ Skeletal muscles have mm-ck (diagnostic of skeletal dystrophy
Located in M line
○ Troponin-I has diagnostic value for cardiac muscle
• Cardiac Myocyte Innervation
○ Vagus and autonomic nerves modulate heart rate
○ Heart will beat without nervous stimulation
• Chronology of heart attack:
○ Myocyte death begins immediately, apoptosis/necrosis begin
○ Inflammation occurs 12-16 hours lateractivates cytokine release
○ Wound healing begins after 48-72 hours
Collagen III then collagen I is secreted and deposited
○ Angiogenesis begins within 48096 hours
○ Scar formation ensues
Mediated by lysyl oxidase
• Inhibiting this would prevent scarring
• Management of cardiac-insufficient patient:
○ Re-muscularized via transplantation of patient matched pluripotent
cells and multipotent resident adult stem cells
○ Re-musculariztion via proliferation of healthy resident cardio myocytes:
g0prolifertionre-muscularzation.
○ Cardiac myocyte regernation
Hypertrophy
• Bad type: stress induced by chemical insult or high blood
pressure
○ Pathological hypertrophy—re-expression of
embryonic cardiac genes.
• Good: seen in athletes
Ischemic Injury
• Interruption of blood supply that results in myocyte death
• Possible sources of myocyte replacement:
○ Cardiac fibroblasts—heal the wound of infarction
Creates non-contractile scar
Researchers speculate that fibroblasts serve as a reservoir of
myocyte stem cells
Not a likely source of myocyte replacement
○ Stem Cells
Embryonic
• Requires transplantation
Adult
• May or may not require transplantation
• May originate from bone marrow or heart
• Whether or not they can differentiate into functional
cardiomyocytes is controversial
• Transplanted hearts accumulate cardiac myocytes while in
hosts.
○ Myocytes come from hosts bone marrow
○ Evidence that stem cells can differentiate into
cardiac myocyte
○ Animal studies refute these findings
Embryonic Stem Cells (ESC):
• Pluripotent
• Derived from inner cell mass of blastocyst
• Pluuripotent cells can differentiate into functional
cardiomyocytes
○ Not debated
○ But it is not known whether or not this can be with
high efficiency.
• In embryo:
○ Precardic endoderm induces adjacent cells in the
precardiac mesodermbecome cardiac myocytes
○ If precardiac endoderm is cultivated with ESC,
ESC’s become myocytes
• Can surviving adult cardiomyocytes be induced to proliferate and regenerate
after myocardial infarction?
○ Prevailing dogma: we have received all our cardiomyocytes by the end
of the neonatal stage of development.
b/c cardiomyocytes cannot divide and because there are no
stem cells in the myocardium, we can’t make more
cardiomyocytes.
Dogma is being disproven with emerging stem cell evidence.
Evidence is emerging that G0 cardiomyocytes can be induced to
proliferate.
• See notes
Das könnte Ihnen auch gefallen
- Humerus Arm Anatomical Neck ArmDokument41 SeitenHumerus Arm Anatomical Neck ArmmcwnotesNoch keine Bewertungen
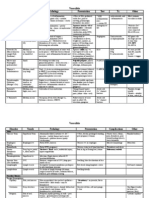
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDokument3 SeitenVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNoch keine Bewertungen
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDokument3 SeitenVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNoch keine Bewertungen
- Cytokines: Cytokine Source Target/Effect OtherDokument1 SeiteCytokines: Cytokine Source Target/Effect OthermcwnotesNoch keine Bewertungen
- Cytokines: Cytokine Source Target/Effect OtherDokument1 SeiteCytokines: Cytokine Source Target/Effect OthermcwnotesNoch keine Bewertungen
- Antibodies: Type Response Action Other Hypersensitivity TypeDokument2 SeitenAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNoch keine Bewertungen
- Antibodies: Type Response Action Other Hypersensitivity TypeDokument2 SeitenAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNoch keine Bewertungen
- Lab 2: Contractility of Visceral and Vascular (Aorta) SmoothDokument3 SeitenLab 2: Contractility of Visceral and Vascular (Aorta) SmoothmcwnotesNoch keine Bewertungen
- Hypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesDokument1 SeiteHypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesmcwnotesNoch keine Bewertungen
- Surface Molecules: Molecule Location Ligand Action OtherDokument1 SeiteSurface Molecules: Molecule Location Ligand Action OthermcwnotesNoch keine Bewertungen
- Lab 1: Electrical and Mechanical Properties of Skeletal MuscleDokument3 SeitenLab 1: Electrical and Mechanical Properties of Skeletal MusclemcwnotesNoch keine Bewertungen
- Lab 1: Electrical and Mechanical Properties of Skeletal MuscleDokument3 SeitenLab 1: Electrical and Mechanical Properties of Skeletal MusclemcwnotesNoch keine Bewertungen
- Lab 10 Digestive System: Salivary Glands, Tongue, Esophagus, StomachDokument3 SeitenLab 10 Digestive System: Salivary Glands, Tongue, Esophagus, StomachmcwnotesNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Palmitic Acid Induced Lipotoxicity Is Associated With Altered Lipid Metabolism, Enhanced CYP450 2E1 and Intracellular Calcium Mediated ER Stress in Human Hepatoma CellsDokument15 SeitenPalmitic Acid Induced Lipotoxicity Is Associated With Altered Lipid Metabolism, Enhanced CYP450 2E1 and Intracellular Calcium Mediated ER Stress in Human Hepatoma CellssouradiptaNoch keine Bewertungen
- Class: 8 Science Chapter - 8 Cell - Structure and FunctionsDokument10 SeitenClass: 8 Science Chapter - 8 Cell - Structure and FunctionsAmiteshwar SinghNoch keine Bewertungen
- Pancreatic Juice SecretionDokument3 SeitenPancreatic Juice SecretionBilal SaidNoch keine Bewertungen
- Lab 1 AnatomyDokument5 SeitenLab 1 AnatomyNimra Shahnaz Khadim HussainNoch keine Bewertungen
- Students Will Be Called Randomly.Dokument5 SeitenStudents Will Be Called Randomly.Naisy Magalona100% (1)
- 10 1038@nrdp20156Dokument17 Seiten10 1038@nrdp20156Desi DwiNoch keine Bewertungen
- Protein Functia Localizarea Sinteza MaturizareaDokument1 SeiteProtein Functia Localizarea Sinteza MaturizareaAnisoaraNoch keine Bewertungen
- 19 - Lipid MetabolismDokument35 Seiten19 - Lipid MetabolismcheckmateNoch keine Bewertungen
- Protein Kinase C Activation and The Development of Diabetic ComplicationsDokument8 SeitenProtein Kinase C Activation and The Development of Diabetic ComplicationsAna LevcencoNoch keine Bewertungen
- Biochemistry Ebook - Class 11Dokument249 SeitenBiochemistry Ebook - Class 11polluNoch keine Bewertungen
- Astragalus in BrucelozaDokument8 SeitenAstragalus in BrucelozaEmilia PopaNoch keine Bewertungen
- UWorld Biochem ReviewDokument1 SeiteUWorld Biochem ReviewvsalardaNoch keine Bewertungen
- Meiosis & Mitosis Ms As EdxDokument12 SeitenMeiosis & Mitosis Ms As EdxmlkNoch keine Bewertungen
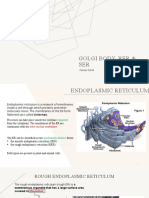
- Golgi Body, Rer & SerDokument8 SeitenGolgi Body, Rer & SerZainab ZahidNoch keine Bewertungen
- Unit 6 & 7 Cell EnergyDokument17 SeitenUnit 6 & 7 Cell EnergyRut ChristineNoch keine Bewertungen
- Nutrition and Gene Expression (PDFDrive)Dokument592 SeitenNutrition and Gene Expression (PDFDrive)Arooj EhsanNoch keine Bewertungen
- Regents Biology Homework Packet Unit 5: Energy in A Cell Photosynthesis & Cellular RespirationDokument15 SeitenRegents Biology Homework Packet Unit 5: Energy in A Cell Photosynthesis & Cellular RespirationHakan Alkan0% (1)
- Botany ReviewerDokument10 SeitenBotany ReviewerJARISSA DIZON GALLAZANoch keine Bewertungen
- 1 Exam Style Answers 1 Asal Biology CBDokument4 Seiten1 Exam Style Answers 1 Asal Biology CBvadixa6007100% (2)
- 2019 Book TauBiology PDFDokument405 Seiten2019 Book TauBiology PDFElisa L BNoch keine Bewertungen
- Vitamin CDokument1 SeiteVitamin CJ-eliNoch keine Bewertungen
- Life Science KsetDokument16 SeitenLife Science KsetRaghunathNoch keine Bewertungen
- Control Over GenesDokument125 SeitenControl Over GenesSwati GautamNoch keine Bewertungen
- Department of Education: Republic of The PhilippinesDokument4 SeitenDepartment of Education: Republic of The PhilippinesROCHELLE MAGBUONoch keine Bewertungen
- PathoGenesis of Periodontal DiseaseDokument20 SeitenPathoGenesis of Periodontal Diseaseneji_murni100% (4)
- Biology - Knee Jerk SPMDokument4 SeitenBiology - Knee Jerk SPMKumar AyavooNoch keine Bewertungen
- On Human Nature by E.O. WilsonDokument138 SeitenOn Human Nature by E.O. Wilsonjayg76100% (5)
- Genomic Analysis of MAP Kinase Cascades In: Arabidopsis Defense ResponsesDokument13 SeitenGenomic Analysis of MAP Kinase Cascades In: Arabidopsis Defense ResponsesMelvin PrasadNoch keine Bewertungen
- Gr12 PAPER 2 Bio TERMSDokument13 SeitenGr12 PAPER 2 Bio TERMSMmabatho VilakaziNoch keine Bewertungen
- QUARTER 4 Summative Test Week 2 3Dokument6 SeitenQUARTER 4 Summative Test Week 2 3marvene paladoNoch keine Bewertungen