Beruflich Dokumente
Kultur Dokumente
Burns Key Pts Chapter - 025
Hochgeladen von
Ba LitOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Burns Key Pts Chapter - 025
Hochgeladen von
Ba LitCopyright:
Verfügbare Formate
Lewis et al: Medical-Surgical Nursing: Assessment and Management of Clinical Problems, 7th edition Key Points Chapter 25:
Nursing Management: Burns
Burns are body tissue injuries due to heat, cold, chemicals, electrical current, or radiation. Smoke and inhalation injuries result from inhalation of hot air or noxious chemicals.
The resulting effect of burns is influenced by the temperature of the burning agent, the duration of contact time, and the tissue type injured.
Burn prevention programs focus on child-resistant lighters; nonflammable childrens clothing; stricter building codes; smoke detectors/alarms; and fire sprinklers. Nurses need to advocate for scald- and fire riskreduction strategies in the home. Occupational health nurses need to educate workers to reduce scald, chemical, electrical, and thermal injuries in the work setting. Burn treatment is related to injury severity determined by depth. The extent is calculated by the percent of the total body surface area (TBSA), location, and patient risk factors. Burns are defined by degrees: first degree (same as sunburn), second degree, and third degree. A more precise definition of second- and third-degree burns includes the depth of skin destruction: partial-thickness and full-thickness. Second- and third-degree burn extent can be determined using total body surface area based on two guides: Lund-Browder chart and Rule of Nines. Burn extent is often revised after edema subsides and demarcation of injury zones occurs. Face, neck, and circumferential burns to the chest/back area may inhibit respiratory function with mechanical obstruction secondary to edema or leathery, devitalized tissue (eschar) formation. These injuries may cause inhalation injury and respiratory mucosal damage. Hands, feet, and eye burns may make self-care difficult and jeopardize future function. Buttocks or genitalia burns are susceptible to infection. Circumferential burns to extremities can cause circulatory compromise distal to the burn. Burn management is organized chronologically into three phases: emergent (resuscitative), acute (wound healing), and rehabilitation (restorative). Overlaps in care
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc.
Key Points exist from one phase to another.
25-2
EMERGENT PHASE Period of time required to resolve immediate, life-threatening problems. Phase may last from time of burn to 3 or more days, but it usually lasts 24 to 48 hours.
A primary concern is the onset of hypovolemic shock and edema formation. Toward the end of the phase, if fluid replacement is adequate, the capillary membrane permeability is restored. Fluid loss and edema formation cease. The interstitial fluid gradually returns to the vascular space. Diuresis occurs with low urine specific gravities. Manifestations include shock from the pain and hypovolemia. Areas of full-thickness and deep partial-thickness burns are initially anesthetic because the nerve endings are destroyed. Superficial to moderate partial-thickness burns are painful. Shivering occurs as a result of chilling, and most patients are alert. Unconsciousness or altered mental status is usually a result of hypoxia associated with smoke inhalation, head trauma, or excessive sedation or pain medication. Complications: o Cardiovascular system: dysrhythmias and hypovolemic shock o Respiratory system: vulnerable to upper airway injury causing edema formation and obstruction of airway, and inhalation injury o Renal system: if patient is hypovolemic, kidney blood flow may decrease, causing renal ischemia. If it continues, acute renal failure may develop. With fullthickness and electrical burns, myoglobin and hemoglobin are released into the bloodstream and occlude the renal tubules. Management includes a rapid and thorough assessment and intervention of airway management, fluid therapy, and wound care. Analgesics are ordered to promote patient comfort. Early in the postburn period, IV pain medications are given. Early and aggressive nutritional support decreases mortality and complications, optimizes healing of burn, and minimizes negative effects of hypermetabolism and catabolism.
ACUTE PHASE Begins with the mobilization of extracellular fluid and subsequent diuresis. Phase concludes when burned area is completely covered by skin grafts or when wounds are healed. This may take weeks or many months.
Manifestations include eschar from partial-thickness wounds. Once removed, reepithelialization appears as red or pink scar tissue. Margins of full-thickness eschar take longer to separate. As a result, they require surgical debridement and skin grafting for healing.
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc.
Key Points
25-3
Because the body is trying to reestablish fluid and electrolyte homeostasis, it is important for the nurse to follow the patients serum electrolyte levels closely (hypo- or hypernatremia, hypo- or hyperkalemia). Complications include wound infection progressing to transient bacteremia as result of manipulation (e.g., after hydrotherapy and debridement). Same cardiovascular and respiratory system complications as in emergent phase may continue. Patient can become extremely disoriented, withdraw, or be combative. This is a transient state, lasting from a day to several weeks. Range of motion may be limited and contractures can occur. Paralytic ileus results from sepsis. Diarrhea and constipation may also occur. Management involves wound care with daily observation, assessment, cleansing, debridement, and dressing reapplication. Individualized and consistent pain assessment and care are essential. Note two kinds of pain: continuous, background pain existing throughout day and night, and treatment pain associated with dressing changes, ambulation, and rehabilitation activities. First line of treatment is pharmacologic. Then use nonpharmacologic strategies, such as relaxation tapes, visualization, hypnosis, guided imagery, and biofeedback. Rigorous physical therapy throughout recovery is imperative to maintain joint function. Nutritional therapy provides adequate calories and protein to promote healing.
REHABILITATION PHASE Begins when wounds have healed and patient is able to resume self-care activity. Phase occurs as early as 2 weeks or as long as 7 to 8 months after the burn.
Goals are to assist the patient in resuming a functional role in society and accomplish functional and cosmetic reconstructive surgery. Manifestations include new skin appearing flat and pink, then raised and hyperemic; itching occurs with healing. Complications are skin and joint contractures and hypertrophic scarring. Management includes positioning, splinting, and exercise to minimize contracture. Burned legs may be wrapped with elastic (e.g., tensor/Ace) bandages to assist the circulation to the leg graft and donor sites. Patient education and hands-on instruction need to be provided in dressing changes and wound care. Continuous exercise and physical/occupational therapy cannot be overemphasized. Encouragement and reassurance are necessary for patient morale, attaining independence, and returning to preburn activities.
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc.
Key Points
25-4
For patient with emotional needs, it is important that the nurse have understanding of circumstances of burn, family relationships, and prior coping experiences with stressful situations. Patient may experience fear, anxiety, anger, guilt, and depression.
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc.
Das könnte Ihnen auch gefallen
- Nursing care process in patients with chronic obstructive pulmonary diseaseVon EverandNursing care process in patients with chronic obstructive pulmonary diseaseNoch keine Bewertungen
- Nursing Management of Patient With BurnsDokument30 SeitenNursing Management of Patient With BurnsjsoalNoch keine Bewertungen
- 1 2 2012med Surg BurnsDokument2 Seiten1 2 2012med Surg BurnsIan RamaNoch keine Bewertungen
- Burn NotesDokument4 SeitenBurn NotesRiza Angela BarazanNoch keine Bewertungen
- Burns CH 25 n-7Dokument7 SeitenBurns CH 25 n-7Jessica VargasNoch keine Bewertungen
- NCM 109 Common Health Problems in TodddlersDokument9 SeitenNCM 109 Common Health Problems in TodddlersMantilla, Kristina Cassandra A.Noch keine Bewertungen
- Jeopardy Game - BurnsDokument42 SeitenJeopardy Game - BurnsPC NNoch keine Bewertungen
- BURNSDokument69 SeitenBURNS57- Kalanidhi mNoch keine Bewertungen
- Integumentary System Review - BurnsDokument52 SeitenIntegumentary System Review - BurnsmikErlhNoch keine Bewertungen
- Management of Burn Injuries: Dr. Lawal G.D Registrar, Dept. of Surgery, NHADokument53 SeitenManagement of Burn Injuries: Dr. Lawal G.D Registrar, Dept. of Surgery, NHAawesome0% (1)
- Ns. Fetreo Negeo Putra, S.Kep.,M.KepDokument67 SeitenNs. Fetreo Negeo Putra, S.Kep.,M.KepAnggraini DarmawinantiNoch keine Bewertungen
- Note nsc432 Mod5 E4fhzhwemo2iupeDokument45 SeitenNote nsc432 Mod5 E4fhzhwemo2iupeBosede OjoNoch keine Bewertungen
- Case Pres PartDokument12 SeitenCase Pres PartJeannezelle Anne Mariz GazaNoch keine Bewertungen
- Burn Injury ManagementDokument26 SeitenBurn Injury Managementbackupuoload85Noch keine Bewertungen
- BurnsDokument106 SeitenBurnsShahini PrajapatiNoch keine Bewertungen
- Burns NotesDokument7 SeitenBurns NotesPsheen Pei WoeiNoch keine Bewertungen
- BurnsDokument55 SeitenBurnsMohammad Amjad KhanNoch keine Bewertungen
- BurnsDokument9 SeitenBurnsVincentus BinNoch keine Bewertungen
- Primary Care of BurnsDokument20 SeitenPrimary Care of BurnsNatalie AlcântaraNoch keine Bewertungen
- Physical ExamDokument43 SeitenPhysical Examapi-3726369Noch keine Bewertungen
- The White Army-BurnsDokument69 SeitenThe White Army-BurnsVishnu PriyaNoch keine Bewertungen
- Burn InjuryDokument19 SeitenBurn InjuryKristine Castillo100% (1)
- Nursing Care of Patients With BURNDokument21 SeitenNursing Care of Patients With BURNShuciee ImoedtsNoch keine Bewertungen
- Burn ManagementDokument13 SeitenBurn Managementhendra ciptaNoch keine Bewertungen
- CU. 9 BurnsDokument50 SeitenCU. 9 BurnsCechanNoch keine Bewertungen
- Acute Biologic Crisis - Hand OutDokument48 SeitenAcute Biologic Crisis - Hand OutLouis Carlos RoderosNoch keine Bewertungen
- Burn InjuryDokument32 SeitenBurn InjuryamosNoch keine Bewertungen
- Pre-Reading For VIHDokument10 SeitenPre-Reading For VIHMaria ClaraNoch keine Bewertungen
- Case Study Burn InjuryDokument9 SeitenCase Study Burn InjuryAmber Dawn MonteroNoch keine Bewertungen
- Management: Minor BurnsDokument3 SeitenManagement: Minor BurnsPatrick MangilinNoch keine Bewertungen
- Burn CmeDokument34 SeitenBurn CmeSyima MnnNoch keine Bewertungen
- Askep KGD Luka Bakar TeoriDokument43 SeitenAskep KGD Luka Bakar TeoriRiskaNoch keine Bewertungen
- Case Study Burn InjuryDokument9 SeitenCase Study Burn InjuryDoneva Lyn MedinaNoch keine Bewertungen
- Burns: Ashkay Anita Collins KennieDokument28 SeitenBurns: Ashkay Anita Collins KennierohitNoch keine Bewertungen
- Nursing - Burn InjuryDokument39 SeitenNursing - Burn Injuryamaracha2003Noch keine Bewertungen
- BurnsDokument33 SeitenBurnsErina Erichan Oto100% (1)
- AAAAAAAAAAAADokument21 SeitenAAAAAAAAAAAAM sajjad HaiderNoch keine Bewertungen
- Burn and Maangement NEW PDFDokument36 SeitenBurn and Maangement NEW PDFAshok SabalNoch keine Bewertungen
- Wound Infection: Julie Mae T. Ambay BSN 2-2Dokument14 SeitenWound Infection: Julie Mae T. Ambay BSN 2-2Julie Mae AmbayNoch keine Bewertungen
- Burn AsseessmentDokument3 SeitenBurn AsseessmentHCX dghhqNoch keine Bewertungen
- Adult NursingDokument100 SeitenAdult NursingAaron Wallace100% (1)
- Hospital Burn CareDokument9 SeitenHospital Burn CareAgung Rizka PratamaNoch keine Bewertungen
- Burns An Introduction To Burns and Basic Wound - 2023 - Physician Assistant CliDokument11 SeitenBurns An Introduction To Burns and Basic Wound - 2023 - Physician Assistant CliJose AnaconaNoch keine Bewertungen
- Case Study Burn Injury - 11Dokument15 SeitenCase Study Burn Injury - 11Evelyn MedinaNoch keine Bewertungen
- Care and Management of Burns Patients: March 2016Dokument3 SeitenCare and Management of Burns Patients: March 2016Meri Fitria HandayaniNoch keine Bewertungen
- BurnDokument3 SeitenBurnhameunjungNoch keine Bewertungen
- YankletterDokument2 SeitenYankletterGaurav DeshmukhNoch keine Bewertungen
- 1 Burn NCPDokument2 Seiten1 Burn NCPkingjoy100% (1)
- Key Points From Book Test 1Dokument8 SeitenKey Points From Book Test 1Hayden ShulerNoch keine Bewertungen
- Burn Injury: General Surgery Department, FKUI/RSCM, Jakarta, Indonesia, May 2011Dokument8 SeitenBurn Injury: General Surgery Department, FKUI/RSCM, Jakarta, Indonesia, May 2011DeVi K. NinGsihNoch keine Bewertungen
- Week 2-BurnDokument53 SeitenWeek 2-BurnManal jNoch keine Bewertungen
- Burn NotesDokument2 SeitenBurn NotesRiza Angela BarazanNoch keine Bewertungen
- Burns Physiotherapy: Submitted By: Noor, Nisha, Nusrat, Saiha Submitted To: Dr. Aqsa Mujaddadi SUBMITTED ON: 16-03-2020Dokument48 SeitenBurns Physiotherapy: Submitted By: Noor, Nisha, Nusrat, Saiha Submitted To: Dr. Aqsa Mujaddadi SUBMITTED ON: 16-03-2020saihaNoch keine Bewertungen
- Burns in PaediatricDokument62 SeitenBurns in PaediatricMusa yohana75% (4)
- BurnsDokument53 SeitenBurnsAnonymous nPewb0gNoch keine Bewertungen
- Burn NursingDokument13 SeitenBurn NursingAndi sutandi50% (2)
- Total Scar Management: From Lasers to Surgery for Scars, Keloids, and Scar ContracturesVon EverandTotal Scar Management: From Lasers to Surgery for Scars, Keloids, and Scar ContracturesRei OgawaNoch keine Bewertungen
- Chapter 27Dokument20 SeitenChapter 27Ba LitNoch keine Bewertungen
- Airborne PrecautionDokument6 SeitenAirborne PrecautionBa LitNoch keine Bewertungen
- Turkey 1Dokument1 SeiteTurkey 1Ba LitNoch keine Bewertungen
- Turkey 2Dokument1 SeiteTurkey 2Ba LitNoch keine Bewertungen
- AND LET GO: HyskalDokument5 SeitenAND LET GO: HyskalBa LitNoch keine Bewertungen
- Turkey 3Dokument1 SeiteTurkey 3Ba LitNoch keine Bewertungen
- Pasta RecipeDokument1 SeitePasta RecipeBa LitNoch keine Bewertungen
- Forgive MeDokument1 SeiteForgive MeBa LitNoch keine Bewertungen
- Chapter 13Dokument25 SeitenChapter 13Ba LitNoch keine Bewertungen
- 15 Module15ShockLearningGuideDokument3 Seiten15 Module15ShockLearningGuideBa LitNoch keine Bewertungen
- BlooDokument1 SeiteBlooBa LitNoch keine Bewertungen
- EOL PaperDokument1 SeiteEOL PaperBa LitNoch keine Bewertungen
- Chapter 04Dokument21 SeitenChapter 04angelNoch keine Bewertungen
- QuestionsDokument1 SeiteQuestionsBa LitNoch keine Bewertungen
- Action of DrugDokument1 SeiteAction of DrugBa LitNoch keine Bewertungen
- Fried ChickenDokument1 SeiteFried ChickenBa LitNoch keine Bewertungen
- Chapter - 047 Renal Key PointsDokument7 SeitenChapter - 047 Renal Key PointsBa LitNoch keine Bewertungen
- Creamy Strawberry-Lemon SquaresDokument1 SeiteCreamy Strawberry-Lemon SquaresBa LitNoch keine Bewertungen
- BusinesslikeDokument2 SeitenBusinesslikeBa LitNoch keine Bewertungen
- PassDokument2 SeitenPassBa LitNoch keine Bewertungen
- Cosyntropin ( - Koe Sin TROE Pin) (Cortrosyn) : Given To Control Symptoms Such As Diarrhea or FlushingDokument2 SeitenCosyntropin ( - Koe Sin TROE Pin) (Cortrosyn) : Given To Control Symptoms Such As Diarrhea or FlushingBa LitNoch keine Bewertungen
- Cosyntropin ( - Koe Sin TROE Pin) (Cortrosyn) : Given To Control Symptoms Such As Diarrhea or FlushingDokument2 SeitenCosyntropin ( - Koe Sin TROE Pin) (Cortrosyn) : Given To Control Symptoms Such As Diarrhea or FlushingBa LitNoch keine Bewertungen
- Chapter 30Dokument16 SeitenChapter 30Ba LitNoch keine Bewertungen
- ReviewDokument1 SeiteReviewBa LitNoch keine Bewertungen
- BiosDokument1 SeiteBiosBa LitNoch keine Bewertungen
- LetterDokument1 SeiteLetterBa LitNoch keine Bewertungen
- Midterm2 SolDokument2 SeitenMidterm2 SolBa LitNoch keine Bewertungen
- Pulseless VT/VF Algorithm First Impression: Sick or Not Sick? Primary SurveyDokument9 SeitenPulseless VT/VF Algorithm First Impression: Sick or Not Sick? Primary SurveyBa LitNoch keine Bewertungen
- Ischemic Stroke ManagementDokument8 SeitenIschemic Stroke ManagementBa LitNoch keine Bewertungen
- Student Learning Guide For Obstructive Pulmonary DiseasesDokument9 SeitenStudent Learning Guide For Obstructive Pulmonary DiseasesBa LitNoch keine Bewertungen
- Fetal Intervetion - Abdelghaffarhelal2019Dokument20 SeitenFetal Intervetion - Abdelghaffarhelal2019Trần Ngọc BíchNoch keine Bewertungen
- King Abdulaziz University Hospital Surgical Safety ChecklistDokument1 SeiteKing Abdulaziz University Hospital Surgical Safety ChecklistdrshwethanaikNoch keine Bewertungen
- M3 CiaDokument2 SeitenM3 CiaApplePi SimpNoch keine Bewertungen
- IHDDokument34 SeitenIHDAyeshah IlyasNoch keine Bewertungen
- Daftar Pustaka Case CephalgiaDokument3 SeitenDaftar Pustaka Case Cephalgiakatherine rinovaNoch keine Bewertungen
- BP PGD CausticDokument36 SeitenBP PGD Causticasni_rahayu9020Noch keine Bewertungen
- Lra 181458 Non Operating Room Anesthesia Patient Selection and SpecialDokument9 SeitenLra 181458 Non Operating Room Anesthesia Patient Selection and SpecialEric Aguilar SantiagoNoch keine Bewertungen
- Ventric Ul Omega LyDokument40 SeitenVentric Ul Omega LyErliana FaniNoch keine Bewertungen
- Krista L Switzer ResumeDokument2 SeitenKrista L Switzer Resumeapi-247358875Noch keine Bewertungen
- Fundamentals of Nursing SummaryDokument58 SeitenFundamentals of Nursing SummaryJa Dimas100% (2)
- 1 - Introduction of CytopathologyDokument41 Seiten1 - Introduction of CytopathologyAyu Rizky Fitriawan AyuNoch keine Bewertungen
- Hormones of The Anterior PituitaryDokument21 SeitenHormones of The Anterior PituitaryRed MistNoch keine Bewertungen
- Recommended Standards For Newborn ICU DesignDokument40 SeitenRecommended Standards For Newborn ICU DesignCarol HNoch keine Bewertungen
- Orthodontic Case PresentationDokument21 SeitenOrthodontic Case PresentationEman Nazzal100% (1)
- Biohiorizons Catalog L01029 PDFDokument28 SeitenBiohiorizons Catalog L01029 PDFTomas LopezNoch keine Bewertungen
- Code Team Training and Assessment Best Practices From The Floor UCM - 486059Dokument34 SeitenCode Team Training and Assessment Best Practices From The Floor UCM - 486059JoaoNoch keine Bewertungen
- Understanding Corrected AgeDokument2 SeitenUnderstanding Corrected Ages_ton77Noch keine Bewertungen
- NOTICE (Revised Syllabi) : (WRITTEN TEST & SYLLABI For The Posts - Advt. No. 01, 02 and 03 of 2016)Dokument123 SeitenNOTICE (Revised Syllabi) : (WRITTEN TEST & SYLLABI For The Posts - Advt. No. 01, 02 and 03 of 2016)wani ashNoch keine Bewertungen
- 1AA17AT009 - Trauma Centre by Ananya KulkarniDokument43 Seiten1AA17AT009 - Trauma Centre by Ananya KulkarniSakshi RangnekarNoch keine Bewertungen
- Terapi Pijat English PDFDokument6 SeitenTerapi Pijat English PDFari dwiNoch keine Bewertungen
- @. Massive TrasfussionDokument12 Seiten@. Massive TrasfussionYoomiif BedadaNoch keine Bewertungen
- Scars & Devices in Paces 4th Edition PDFDokument132 SeitenScars & Devices in Paces 4th Edition PDFKaleem Ullah Bhatti100% (2)
- Instrumentar LaparoscopieDokument3 SeitenInstrumentar LaparoscopieMarius NenciuNoch keine Bewertungen
- Table : Number of Population, Hospitals and Beds in All Over JordanDokument8 SeitenTable : Number of Population, Hospitals and Beds in All Over JordanjNoch keine Bewertungen
- Trabalhoavaliativo Ingles Simple Present e ContinuousDokument4 SeitenTrabalhoavaliativo Ingles Simple Present e ContinuousMarcelo RochaNoch keine Bewertungen
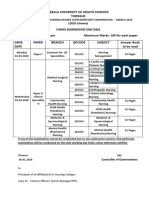
- Kerala University of Health Sciences Thrissur: (2010 Scheme)Dokument1 SeiteKerala University of Health Sciences Thrissur: (2010 Scheme)subiNoch keine Bewertungen
- Circulatory System TurtleDokument32 SeitenCirculatory System TurtleVillamorchardNoch keine Bewertungen
- 3 The Health Care Delivery SystemDokument5 Seiten3 The Health Care Delivery SystemMikhaela Andree Mariano100% (1)
- LaaabbbbsssDokument3 SeitenLaaabbbbsssshiva lakshmiNoch keine Bewertungen
- Early Initiation of Breast-Feeding in Ghana: Barriers and FacilitatorsDokument7 SeitenEarly Initiation of Breast-Feeding in Ghana: Barriers and Facilitatorsafifah nurul zahraNoch keine Bewertungen