Beruflich Dokumente
Kultur Dokumente
Nursing Diagnosis
Hochgeladen von
Mariya Mikaela Garcia SoledadOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Diagnosis
Hochgeladen von
Mariya Mikaela Garcia SoledadCopyright:
Verfügbare Formate
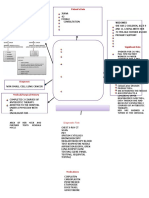
Nursing Diagnosis: Ineffective Airway Clearance Possible Etiologies: (Related to)
Goals/ Objectives: Short term goal: Client will demonstrate signs of patent airway and adequate oxygen
Nursing Actions 1. Assess respiratory status every hour during acute phase: lung sounds, respiratory rate and depth, presence and severity of wheezing, breathing pattern, use of accessory muscles. 2. Assist patient to assume
Rationale Outcome Criteria: 1. Some degree in bronchospasm is present with obstruction in airway and may be manifested with wheezing or absent breath sounds in severeasthma. Tachypnea is usually present to some degree and respiratory dysfunction is variable depending on underlying process such as allergic reaction. 2. Elevation of head of the bed facilitates respiratory function by use of gravity, however client in distress may seek position that most eases breathing. 3. Precipitators of allergic type of respiratory reactions that can trigger or exacerbate onset of acute episode. 4. Provides some means to cope with or control dyspnea and reduce air trapping. 5. Hydration helps thin secretions, facilitating expectoration and using warm liquids may decrease bronchospasm. Client will be able to identify and avoid potential allergens or stimuli that would triggerasthmaattack and be able to handle symptoms if recurrence comes, prompt follow up check up and to always bring or have the prescribed medication/s on hand in Client will verbalize reduction or absence in difficulty in breathing and feeling of chest constriction, respiration and cardiac rate within normal range, absence or reduction of inspiratory and expiratory wheezing, and ability to resume to activities.
Bronchospasm Increased production of secretions; retained secretions; thick, viscous secretions
exchange within 3 days.
Decreased energy/ fatigue
Long term goal: Client will demonstrate behaviours to improve or maintain airway clearance and identify potential complications and initiate appropriate actions.
to comfortable position, i.e. elevate head of bed, have client lean on overbed table or sit on the edge of bed. 3. Keep environmental pollution to a minimum according to individual situation. 4. Encourage and assist abdominal and pursed lipbreathing exercises. 5. Increase fluid intake to 3000ml/ day within cardiac tolerance. 6. Provide warm liquids and
Defining characteristics: (Evidenced by)
Statement of difficulty in breathing Feeling of chest constriction Changes in depth/ rate of respiration; tachypnea
Tachycardia Use of accessory muscles or marked respiratory effort
Abnormal breath sound, inspiratory and expiratory wheezing
recommend intake of fluids between meals, instead of during meals. 7. Administer medications as indicated. 8. Monitor side effects of bronchodilator (tremors/ tachycardia). 9. Provide supplemental humidification, e.g., neutralizer in respiratory treatments. 10. Monitor ABGs, pulse oximetry, chest x- ray.
6. Fluids during meals can increase gastric distension and pressure on the diaphragm. 7. Anticholinergic medications are the first line drugs for clients with this condition. 8. Humidity helps reduce viscosity of secretions, facilitating expectoration and may. 9. Breathing exercises help enhance diffusion,nebulizermedications can reduce bronchospasm and stimulate expectoration. 10. Establishes baseline for monitoring progression/ regression of disease process.
caseasthmaoccurs.
Cough (persistent), without sputum production
Prolonged expiration
Cardiovascular Nursing Management
Controlling cholesterol levels Oxygen therapy Encouraging mobility and independence or passive exercises as appropriate Tackling the factors that increase the risk of heart disease, such as smoking, poor diet and little physical exercise if appropriate Record duration of pain, amount of medication required to relieve ir, and accompanying symptoms. Cardiovascular Disease Pathophysiology
Ask the patient to grade the sverity of his pain on a scale 1 to 10. Monitor the patient for chest pain, hypotension, coronary artery spasm, and bleeding from the catheter site. Explain the cardiac catheterization to the patient. If the patient is scheduled for surgery, explain the procedure and events. Help the patient more effectively cope with stress and identify activities that precipitate pain. Stress the need to follow the prescribed drug regimen. Encourage the patient to maintain the prescribed diet. Encourage regular, moderate exercise.
BRONCHIAL ASTHMA IN ACUTE EXACERBATION PATHOPHYSIOLOGY
Predisposing Factors Gender, Age, Family History, Race (animal dander, dust, pollen, etc.)
Precipitating Factors Viral Respiratory Infections, Allergen Exposure Change in Weather, Smoking, Exercise
Exposure to different pathogens
Entry of the allergen
Release of immunoglobulin E (IgE)
Release of different chemical mediators
Mast cell degranulation
Release of the different inflammatory chemical mediators
Leukotrienes inflammatory mediators
Prostaglandins
Histamine, bradykinin, & other
Release of eosinophils (to combat allergen)
Opening of the mucosal inrtracellular junction
Inflammatory process
Mucus production vagal efferents
Increase vascular permeability
Direct stimulation of the
Mucosal edema
Bronchoconstriction
More release of other inflammatory mediators
Decrease ciliary function
Epithelial damage
Further edema
Mucus hypersecretion
Increased airway responsiveness
Wheezing, continuous coughing, feelings of chest tightness
dypnea, moist skin, tachypnea
fatigue, anxiety
View more pathophysiology and schematic diagrams at Nurseslabs.com
Das könnte Ihnen auch gefallen
- Sample SOAP NoteDokument6 SeitenSample SOAP NoteLorrie83% (6)
- Physical Examination Techniques and ManueversDokument160 SeitenPhysical Examination Techniques and ManueversMa-anJaneDiamosNoch keine Bewertungen
- Old Disease NamesDokument52 SeitenOld Disease NamesMuhammad Ata Ul MustafaNoch keine Bewertungen
- Pediatric Nursing Care Plan Impaired Physical MobilityDokument5 SeitenPediatric Nursing Care Plan Impaired Physical Mobilityapi-3077327050% (1)
- Status Epilepticus Case Study Kristopher Kirby.Dokument4 SeitenStatus Epilepticus Case Study Kristopher Kirby.KrisNoch keine Bewertungen
- SBAR Report To Physician About A Critical SitutionDokument3 SeitenSBAR Report To Physician About A Critical SitutionRandolph DjanieNoch keine Bewertungen
- HA - PA Findings Documentation (Head To Neck)Dokument9 SeitenHA - PA Findings Documentation (Head To Neck)Bianca SandovalNoch keine Bewertungen
- Nusing CareplanDokument3 SeitenNusing Careplanardec_143Noch keine Bewertungen
- Nursing Care Plan For Special ChildrenDokument2 SeitenNursing Care Plan For Special Childrenharas_dcsaisNoch keine Bewertungen
- Concept Map SepsisDokument4 SeitenConcept Map SepsisSavanna ChambersNoch keine Bewertungen
- Emergency Room Game: Self-Debriefing QuestionsDokument2 SeitenEmergency Room Game: Self-Debriefing QuestionsRyrey Abraham PacamanaNoch keine Bewertungen
- Gordon'sDokument2 SeitenGordon'sCham Rafaela ConeseNoch keine Bewertungen
- Herb II-5-Herbs That Tonify Qi & BloodDokument51 SeitenHerb II-5-Herbs That Tonify Qi & BloodEdison halimNoch keine Bewertungen
- Pneumonia Case StudyDokument12 SeitenPneumonia Case StudyCharisse Joy Cudal100% (7)
- Thyroid - History Taking: 1. Patient DetailsDokument5 SeitenThyroid - History Taking: 1. Patient DetailsNellayappan SivasubramanianNoch keine Bewertungen
- Puperium ComplicationDokument75 SeitenPuperium Complicationvarshasharma05100% (1)
- Physical AssessmentDokument3 SeitenPhysical AssessmentHyacinth ExmundoNoch keine Bewertungen
- Concept Map PEDokument3 SeitenConcept Map PERobert MariasiNoch keine Bewertungen
- Case AnalysisDokument25 SeitenCase AnalysisGerly LagutingNoch keine Bewertungen
- 1 Ineffective Airway ClearanceDokument8 Seiten1 Ineffective Airway ClearanceEsel Mae DinamlingNoch keine Bewertungen
- Valdez Reflective-Questions PDFDokument3 SeitenValdez Reflective-Questions PDFDexel Lorren ValdezNoch keine Bewertungen
- 8 Sample Care Plans For ACDFDokument11 Seiten8 Sample Care Plans For ACDFacasulla98Noch keine Bewertungen
- TCM DiagnosisDokument7 SeitenTCM DiagnosisravenadlerNoch keine Bewertungen
- Nursing DiagnosisDokument16 SeitenNursing DiagnosisSi Bunga JonquilleNoch keine Bewertungen
- Exam HaadDokument10 SeitenExam HaadNiggaNoch keine Bewertungen
- Inspiratory Muscle TrainingDokument15 SeitenInspiratory Muscle Trainingulfapanjaitan100% (2)
- The Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseVon EverandThe Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseNoch keine Bewertungen
- Head To Toe Assessment (Elder)Dokument2 SeitenHead To Toe Assessment (Elder)ZnarfNoch keine Bewertungen
- Exam Questions HAAD-RN: HAAD Licensure Examination For Registered NursesDokument5 SeitenExam Questions HAAD-RN: HAAD Licensure Examination For Registered NursesGreeshma victorNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care PlanMarielle SorianoNoch keine Bewertungen
- Asthma Nanda DiagnosesDokument4 SeitenAsthma Nanda DiagnosesZinya RobinsonNoch keine Bewertungen
- Nursing Care PlanllDokument5 SeitenNursing Care Planllbbarnes0912Noch keine Bewertungen
- Careplan Week 8Dokument3 SeitenCareplan Week 8api-353681121Noch keine Bewertungen
- Health Assessment 51-100 QuestionnaireDokument27 SeitenHealth Assessment 51-100 QuestionnairetflorenzNoch keine Bewertungen
- Guaifenesin Drug CardDokument1 SeiteGuaifenesin Drug CardJessie JenningsNoch keine Bewertungen
- Nursing Care PlansDokument5 SeitenNursing Care PlansMa Liezel M Camba100% (1)
- NCP Proper CholecystectomyDokument2 SeitenNCP Proper CholecystectomyGail Lian SantosNoch keine Bewertungen
- Nursing Care Plan Impaired Gas ExchangeDokument1 SeiteNursing Care Plan Impaired Gas ExchangeKarylle PetilNoch keine Bewertungen
- Nursing Care PlanDokument2 SeitenNursing Care PlanAl RizkyNoch keine Bewertungen
- ASTHMADokument9 SeitenASTHMAmildred alidonNoch keine Bewertungen
- Ex LapDokument2 SeitenEx LaprebeljeromeNoch keine Bewertungen
- TCP HeartburnDokument12 SeitenTCP HeartburnArlene NicomedezNoch keine Bewertungen
- Code Green Introduction Reviewer - RedDokument4 SeitenCode Green Introduction Reviewer - RedJamieNoch keine Bewertungen
- Heart Failure Care Plan LippincottDokument62 SeitenHeart Failure Care Plan LippincottDyllano100% (1)
- Nursing Care PlansDokument6 SeitenNursing Care PlansRoxanne MariÑas Delvo0% (1)
- NCPDokument2 SeitenNCPMelissa David100% (1)
- Careplan For Sickle Cell DiseaseDokument21 SeitenCareplan For Sickle Cell DiseaseEcaroh Hew SmailliwNoch keine Bewertungen
- Urinary IncontinenceDokument5 SeitenUrinary IncontinencefakrulnersmudaNoch keine Bewertungen
- NANDA Nursing DiagnosesDokument8 SeitenNANDA Nursing DiagnosesShreejana PrajapatiNoch keine Bewertungen
- Nursing Care PlansDokument6 SeitenNursing Care PlansMichelle Danica Vicente PaswickNoch keine Bewertungen
- Careplan 5 MedsurgDokument8 SeitenCareplan 5 Medsurgapi-509642710Noch keine Bewertungen
- PleuritisDokument8 SeitenPleuritisshielamaygo05Noch keine Bewertungen
- Risk For Bleeding - Cirrhosis NCPDokument2 SeitenRisk For Bleeding - Cirrhosis NCPPaula AbadNoch keine Bewertungen
- Nursing Careplan - Rectal CancerDokument5 SeitenNursing Careplan - Rectal CancerdrugcardrefNoch keine Bewertungen
- Peds Nursing Care PlanDokument9 SeitenPeds Nursing Care Planapi-327793284100% (1)
- Nursing Care Plan Renal FailureDokument18 SeitenNursing Care Plan Renal FailureKundan KumarNoch keine Bewertungen
- Nursing DiagnosisDokument4 SeitenNursing DiagnosisLouren Marie DavidNoch keine Bewertungen
- Concept Map 360Dokument6 SeitenConcept Map 360api-273469220Noch keine Bewertungen
- Nursing Care PlanDokument7 SeitenNursing Care PlanRhitzle Ann100% (1)
- Psych Final ContentsDokument51 SeitenPsych Final ContentsFrancis Peter Abear LahoraNoch keine Bewertungen
- BronchitisDokument129 SeitenBronchitisMark Norriel CajandabNoch keine Bewertungen
- CNO. Ethical Framework - StudentDokument42 SeitenCNO. Ethical Framework - StudentdanushaNoch keine Bewertungen
- Disharge Plan Patient'S Outcome Criteria Nursing OrderDokument2 SeitenDisharge Plan Patient'S Outcome Criteria Nursing OrderDianne Loregas SanchezNoch keine Bewertungen
- Care PlanDokument2 SeitenCare PlanLorina Lynne ApelacioNoch keine Bewertungen
- 51 100Dokument18 Seiten51 100Jaessa Feliciano100% (1)
- Imbalanced Nutrition: Less Than Body RequirementDokument10 SeitenImbalanced Nutrition: Less Than Body RequirementDangz SkiiNoch keine Bewertungen
- Careplan PneumoniaDokument3 SeitenCareplan PneumoniaJénny Ann100% (1)
- NCP TetanusDokument2 SeitenNCP TetanusSugar Capule - Manuel0% (1)
- Renal CalculiDokument28 SeitenRenal Calculihailleyann33% (3)
- Status Asthmaticus CASE PRESDokument18 SeitenStatus Asthmaticus CASE PRESNessa Layos MorilloNoch keine Bewertungen
- Activity Intolerance Care Plan For CFDokument8 SeitenActivity Intolerance Care Plan For CFapi-314197645Noch keine Bewertungen
- Managemant Copd CPG MsiaDokument67 SeitenManagemant Copd CPG MsiaNur Anis ZarimeNoch keine Bewertungen
- Practice Exam in Nursing Set FDokument44 SeitenPractice Exam in Nursing Set FAna Rose Dela CruzNoch keine Bewertungen
- Prosedur Occlusive DressingDokument4 SeitenProsedur Occlusive DressingRopita SariNoch keine Bewertungen
- Modern Nursing Cardiogenic Pulmonary Edema Seminar HARKIT SugiyonoDokument43 SeitenModern Nursing Cardiogenic Pulmonary Edema Seminar HARKIT SugiyonoeffitaNoch keine Bewertungen
- B Inggris Halim NCP Asma BronchialDokument28 SeitenB Inggris Halim NCP Asma BronchialAbdul HlmNoch keine Bewertungen
- PolycythemiaDokument3 SeitenPolycythemiaSaraNoch keine Bewertungen
- Respiratory Disorders Lnu 2018 HandoutDokument58 SeitenRespiratory Disorders Lnu 2018 HandoutSamatha SamathaNoch keine Bewertungen
- Case Study On Children With Cardiac DisordersDokument3 SeitenCase Study On Children With Cardiac DisordersAlyNoch keine Bewertungen
- Northwell Direct - Respirator Medical Evaluation QuestionnaireDokument5 SeitenNorthwell Direct - Respirator Medical Evaluation QuestionnaireFaithNoch keine Bewertungen
- PE 12 Chapter 3Dokument16 SeitenPE 12 Chapter 3Ayisha AlamNoch keine Bewertungen
- Advanced Ventilation ManagementDokument3 SeitenAdvanced Ventilation ManagementAnka EremiaNoch keine Bewertungen
- Is Physical Activity and Diet Having A Spot in Periodontal and Respiratory Health A ReviewDokument7 SeitenIs Physical Activity and Diet Having A Spot in Periodontal and Respiratory Health A ReviewAthenaeum Scientific PublishersNoch keine Bewertungen
- Cabergoline PDFDokument2 SeitenCabergoline PDFBebel MantaliNoch keine Bewertungen
- NPDADokument52 SeitenNPDAAlondra MangandogNoch keine Bewertungen
- BPUDDokument26 SeitenBPUDIvanNoch keine Bewertungen
- Pathophysiology Patient's DataDokument3 SeitenPathophysiology Patient's DataKristian Karl Bautista Kiw-isNoch keine Bewertungen
- Nursing Care Plan FinalDokument9 SeitenNursing Care Plan FinalJny SthaNoch keine Bewertungen
- Exercise COPD-342-355 SeparadoDokument14 SeitenExercise COPD-342-355 SeparadoKuririn matiasNoch keine Bewertungen
- Pulmonary Tuberculos IS: PGI Aquino Ruel Aldrin PGI Andaman Greg JinichiDokument79 SeitenPulmonary Tuberculos IS: PGI Aquino Ruel Aldrin PGI Andaman Greg JinichiIggs AndamanNoch keine Bewertungen