Beruflich Dokumente
Kultur Dokumente
Diabetes Increases The Risk of Periodontal Diseases
Hochgeladen von
Thalis BragaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diabetes Increases The Risk of Periodontal Diseases
Hochgeladen von
Thalis BragaCopyright:
Verfügbare Formate
Diabetes increases the risk of periodontal diseases, and biologically plausible mechanisms have been demonstrated in abundance.
Less clear is the impact of periodontal diseases on glycemic control of diabetes and the mechanisms through which this occurs. Inflammatory periodontal diseases may increase insulin resistance in a way similar to obesity, thereby aggravating glycemic control. Further research is needed to clarify this aspect of the relationship between periodontal diseases and diabetes. J Periodontol 2006;77:12891303.
Type 2 patients can be undiagnosed for many years because the hyperglycemia appears gradually and often without symptoms
when diabetic patients in this study were stratified according to their level of glycemic control, significantly greater gingival bleeding was seen in poorly controlled diabetic patients than in either well-controlled diabetic subjects or nondiabetic controls. The number of bleeding sites decreased as glycemic control improved
The preponderance of evidence suggests that diabetes also increases the risk of periodontitis. A thorough meta-analysis concluded that the majority of studiesdemonstrate a more severe periodontal condition in diabetic adults than in adults without diabetes. 18 These studies included over 3,500 diabetic adults and clearly demonstrated a significant association between periodontitis and diabetes. Diabetes has been associated with an increased risk of periodontitis even at a young age. In a group of 263 type 1 diabetic patients compared to 59 nondiabetic siblings and 149 non-diabetic unrelated controls, periodontitis was not seen among any of the subjects under the age of 12.21 However, between 13 and 18 years of age, 13.6% of the diabetic individuals had periodontitis, and the prevalence increased to 39% among those aged 19 to 32 years. By comparison, the prevalence in non-diabetic control subjects was <3%.
Longitudinal research has also shown an increased risk of progressive periodontal destruction in people with diabetes. In a study of the Pima Indians, the incidence and prevalence of periodontal disease were determined in 2,273 subjects 15 years of age or older.38 The prevalence of periodontitis was 60% in subjects with diabetes and 36% in those without diabetes.
In a large epidemiologic study in the United States, adults with poorly controlled diabetes had a 2.9-fold increased risk of having periodontitis compared to non-diabetic adult subjects; conversely,well-controlled diabetic subjects had no significant increase in the risk of periodontitis
O Diabetes inspido, que decorrente da insuficiente quantidade de hormnios antidiurticos produzidos pelo hipotlamo, causa a eliminao de muito lquido atravs da urina e desperta muita sede. Nesse tipo de diabetes, no h alterao no metabolismo do acar Alteraes no ambiente subgengival, tais como aumento dos nveis da glicose e uria no fluido crevicular gengival, favorecem o crescimento de algumas espcies bacterianas7. As alteraes vasculares apresentadas pelo doente descompensado tm estreita relao com a instalao e progesso da doena periodontal6 O fator causal primrio de desenvolvimento das alteraes vasculares no diabtico a prolongada exposio hiperglicemia. Essas alteraes impedem a difuso do oxignio, a eliminao de metablitos, a migrao de leuccitos e a difuso de fatores imunes (quimiocinas, por exemplo), contribuindo para o agravamento da periodontite no diabtico7,8. A funo fagocitria deficiente pode msnifestar-se pelo fato de certo nmero de enzimas serem insulino-dependentes. Nos diabticos mal controlados h uma diminuio da resposta imune infeco, observada pela presena de hiperglicemia e cetoacidose, que alteram a fagocitose dos macrfagos e a quimiotaxia dos polimorfonucleares2,3,7,9. O espessamento dos vasos do periodonto dificulta o transporte de elementos nutritivos intimidade dos tecidos, fazendo-os mais vulnerveis aos produtos de agresso microbiana e a maior severidade da enfermidade periodontal8. Desta forma, a associao entre as alteraes vasculares da doena diabetes e a doena periodontal pode ser assim estabelecida: Diabetes ? alterao vascular ? alteraes do fluido crevicular e do tecido conjuntivo gengival ? resposta imunolgica do hospedeiro alterada ? Doena periodontal? liberao crnica de citocinas pr-inflamatrias ? ao diminuda da insulina ? agravamento das alteraes metablicas
O diabetes compromete a produo da matriz ssea pelos osteoblastos, diminui a sntese de colgeno pelos fibroblastos gengivais, alm de aumentar a atividade da colagenase gengival. O difcil controle da cicatrizao tecidual no diabtico decorre da presena de hiperglicemia, microangiopatias, acidez metablica, fagocitose ineficaz pelos polimorfonucleares e macrfagos A colaborao entre o cirurgio-dentista e o endocrinologista indispensvel para o bom andamento do tratamento dos pacientes diabticos8.
Os pacientes diabticos insulinodependentes apresentaram gengivite com maior freqncia do que os pacientes saudveis. Embora a gengivite raramente evolua para periodontite, a inflamao gengival evidente nestes pacientes8,10; mesmo em quantidades pequenas de placas, h uma grande tendncia de ocorrer gengivite em diabticos descompensados, quando comparado com no-diabticos. Entretanto, crianas com um bom controle metablico no diferem das crianas saudveis. Se os parmetros clnicos do diabetes juvenil estiveram sob controle, a doena no exacerbar a inflamao gengival em crianas e adolescentes7.
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Nutrisi - Prof. Dr. Dr. Askandar, SP - PD-FINASIM - Dr. Sri Murtiwi, SP - PD-FINASIMDokument23 SeitenNutrisi - Prof. Dr. Dr. Askandar, SP - PD-FINASIM - Dr. Sri Murtiwi, SP - PD-FINASIMroviancahyaNoch keine Bewertungen
- December 2018 Ophthalmic PearlsDokument2 SeitenDecember 2018 Ophthalmic PearlsFathirNoch keine Bewertungen
- Chapter 3. Invitro Growth of Oocyte and Oocyte Maturation Đã Chuyển ĐổiDokument49 SeitenChapter 3. Invitro Growth of Oocyte and Oocyte Maturation Đã Chuyển ĐổiGia HoàngNoch keine Bewertungen
- Banana Leaf ScanningDokument24 SeitenBanana Leaf ScanningFatima Dela Cruz LascanoNoch keine Bewertungen
- RESEARCH (Edited)Dokument6 SeitenRESEARCH (Edited)Navarrete, AliceNoch keine Bewertungen
- Health Grade 8: Department of EducationDokument10 SeitenHealth Grade 8: Department of EducationGenesis SarengoNoch keine Bewertungen
- Unicef in IndiaDokument22 SeitenUnicef in IndiaNamita Kothari100% (1)
- PTBD 2Dokument4 SeitenPTBD 2Alcntara AllenNoch keine Bewertungen
- NCM 114-A Module 4Dokument8 SeitenNCM 114-A Module 4Aycee ElardoNoch keine Bewertungen
- Cardiovascular Diagnostic Tests and ProceduresDokument27 SeitenCardiovascular Diagnostic Tests and ProceduresSajjal JohnsonNoch keine Bewertungen
- Removing Contaminated Gown and Gloves ChecklistDokument3 SeitenRemoving Contaminated Gown and Gloves ChecklistFar Ri NaNoch keine Bewertungen
- Nucleus Arthroplasty Volume IIDokument55 SeitenNucleus Arthroplasty Volume IIHelifunoNoch keine Bewertungen
- JPediatrCritCare2167-4903094 133710Dokument18 SeitenJPediatrCritCare2167-4903094 133710brajendra singhNoch keine Bewertungen
- Logistics HandbookDokument196 SeitenLogistics Handbooknikolaos13100% (1)
- Motion Is LotionDokument2 SeitenMotion Is LotionQing JyulyanNoch keine Bewertungen
- Urinesamplesand Urinalysis 2007Dokument5 SeitenUrinesamplesand Urinalysis 2007Catharina Christie HWNoch keine Bewertungen
- Unit 3 - Transudates and Exudates IIIDokument17 SeitenUnit 3 - Transudates and Exudates IIIRubina KhatunNoch keine Bewertungen
- MCQs VTEDokument7 SeitenMCQs VTEMUHAMMADNoch keine Bewertungen
- Persistent Cough in ChildrenDokument6 SeitenPersistent Cough in Childrenyujin KimNoch keine Bewertungen
- AHA18HyperPocketGuidePRINT3FINAL APPROVED PDFDokument2 SeitenAHA18HyperPocketGuidePRINT3FINAL APPROVED PDFAmanda JulianaNoch keine Bewertungen
- Balance, Posture and Body AlignmentDokument6 SeitenBalance, Posture and Body AlignmenthahahahaaaaaaaNoch keine Bewertungen
- Internal Medicine 1, Conrad FischerDokument35 SeitenInternal Medicine 1, Conrad Fischerdukelist566100% (3)
- Immunological Lab Diagnosis of TuberculosisDokument38 SeitenImmunological Lab Diagnosis of TuberculosisRasha EmadNoch keine Bewertungen
- HIV SeminarDokument45 SeitenHIV SeminarDelphy VargheseNoch keine Bewertungen
- Geriatric ...... Dental CareDokument39 SeitenGeriatric ...... Dental CareDelvine AderoNoch keine Bewertungen
- Pathology Lec 1Dokument16 SeitenPathology Lec 1hamadNoch keine Bewertungen
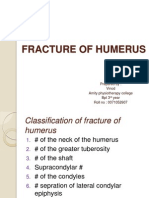
- Fracture of HumerusDokument56 SeitenFracture of HumerusDr. Vinod Gupta100% (2)
- Garcia, Nehemiah B. BSN 2Y2-2A: Ncma 219 Rle Course Task # 2Dokument3 SeitenGarcia, Nehemiah B. BSN 2Y2-2A: Ncma 219 Rle Course Task # 2Mushy_ayaNoch keine Bewertungen
- Beta BlockersDokument2 SeitenBeta BlockersmetkosdNoch keine Bewertungen
- Asbestos Awareness Quiz #1: AnswersDokument2 SeitenAsbestos Awareness Quiz #1: AnswersMichael NcubeNoch keine Bewertungen