Beruflich Dokumente
Kultur Dokumente
Sturge Weber Syndrome
Hochgeladen von
Anumeha JindalCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Sturge Weber Syndrome
Hochgeladen von
Anumeha JindalCopyright:
Verfügbare Formate
Sturge-Weber Syndrome
Background: The Sturge-Weber syndrome (SWS), also called encephalotrigeminal angiomatosis, is a neurocutaneous disorder with angiomas involving the leptomeninges (leptomeningeal angiomas [LAs]) and skin of the face, typically in the ophthalmic (V1) and maxillary (V2) distributions of the trigeminal nerve. The cutaneous angioma is called a port-wine stain (PWS). In the brain, LAs demonstrated by structural neuroimaging may be unilateral or bilateral; unilateral angiomas are more common. Functional neuroimaging may demonstrate a greater area of involvement than structural neuroimaging. This is called a structural versus functional mismatch. The neurologic manifestations vary, depending on the location of the LAs, which most commonly are located in the parietal and occipital regions, and the secondary effects of the angioma. These include seizures, which may be intractable; focal deficits, such as hemiparesis and hemianopsia, both of which may be transient, called "strokelike episodes"; headaches; and developmental disorders, including developmental delay, learning disorders, and mental retardation. Developmental disorders are more common when angiomas are bilateral. Seizure control is thought to improve the neurologic outcome, and epilepsy surgery may be beneficial for refractory seizures. The primary complications involving the ipsilateral eye are buphthalmos and glaucoma, with treatment aimed at controlling the intraocular pressure (IOP) and preventing progressive visual loss and blindness. Cosmetic concerns are also important, and laser therapy is available for the PWS. Extracranial angiomas and soft-tissue overgrowth also may occur. Certain CNS malformations have been associated with the syndrome; other neurocutaneous disorders are included in the differential diagnosis. SWS is referred to as complete when both CNS and facial angiomas are present and incomplete when only 1 area is affected without the other. The Roach Scale is used for classification, as follows:
Type I - Both facial and leptomeningeal angiomas; may have glaucoma Type II - Facial angioma alone (no CNS involvement); may have glaucoma Type III - Isolated LA; usually no glaucoma
Pathophysiology: SWS is caused by residual embryonal blood vessels and their secondary effects on surrounding brain tissue. A vascular plexus develops around the cephalic portion of the neural tube, under ectoderm destined to become facial skin. Normally, this vascular plexus forms in the sixth week and
regresses around the ninth week of gestation. Failure of this normal regression results in residual vascular tissue, which forms the angiomata of the leptomeninges, face, and ipsilateral eye. Neurologic dysfunction results from secondary effects on surrounding brain tissue, which include hypoxia, ischemia, venous occlusion, thrombosis, infarction, or vasomotor phenomenon. From a review of pathologic specimens, Norman and Schoene thought that blood flow abnormalities in the LA caused increased capillary permeability, stasis, and anoxia. Garcia et al and Gomez and Bebin reported that venous occlusion might actually cause the initial neurologic event, either a seizure, transient hemiparesis, or both, thereby beginning the process. A "vascular steal phenomenon" may develop around the angioma, resulting in cortical ischemia. Therefore, recurrent seizures, status epilepticus, intractable seizures, and recurrent vascular events may aggravate this steal further, with an increase in cortical ischemia, resulting in progressive calcification, gliosis, and atrophy, which in turn increase the chance of seizures and neurologic deterioration. Disease progression and neurologic deterioration may occur in SWS. Although the actual LA is typically a static anatomic lesion, Reid et al, Maria et al, and Sujansky and Conradi have clearly documented the progressive nature of SWS. Seizure control, aspirin therapy, and early surgical treatment may prevent neurologic deterioration. The main ocular manifestations (ie, buphthalmos, glaucoma) occur secondary to increased IOP with mechanical obstruction of the angle of the eye, elevated episcleral venous pressure, or increased secretion of aqueous fluid. The etiology of SWS is unclear, although Huq et al reported evidence of somatic mosaicism in 4 patients with SWS. Two had skin biopsy from port-wine stains, and the other 2 had LAs from hemispherectomy. Inversion of chromosome arm 4q and trisomy 10 were seen in one patient each. Malformed cortical vessels in SWS have been reported to be innervated only by noradrenergic sympathetic nerve fibers, and increased endothelin-1 expression was also seen in malformed intracranial vessels. These findings may suggest increased vasoconstriction in these abnormal blood vessels, as endothelin-1 is a peptide associated with vasoconstriction. Fibronectin is a molecule important in regulating angiogenesis, maintenance of the blood-brain barrier, blood vessel structure and function, as well as brain tissue responses to seizures. Comi et al reported that, in patients with SWS, decreased expression of fibronectin was noted in the leptomeningeal blood
vessels while increased expression was noted in the parenchymal vessels. The leptomeningeal blood vessel circumference was decreased, while blood vessel density was increased in SWS. Overall, in SWS, a somatic mutation appears to cause alterations in regulation of the structure and function of blood vessels, innervation of the blood vessels, as well as expression of extracellular matrix and vasoactive molecules. Frequency:
In the US: According to Nelson's Textbook of Pediatrics, the incidence of SWS is estimated at 1 per 50,000. No regional differences have been identified. The inheritance is sporadic. The incidences of the major clinical manifestations of SWS are listed in Table 1. Table 1. Clinical Manifestations of Sturge-Weber Syndrome Risk of SWS with facial PWS SWS without facial nevus Bilateral cerebral involvement Seizures Hemiparesis Hemianopia Headaches Developmental delay and mental retardation Glaucoma Choroidal hemangioma 8% 13% 15% 72-93% 25-56% 44% 44-62% 50-75% 30-71% 40%
Mortality/Morbidity:
Neurologic and developmental morbidity includes seizures, weakness, strokes, headaches, hemianopsia, mental retardation, and developmental abnormalities. The development of seizures and the age of onset may correlate with the degree of neurologic involvement. Neurologic dysfunction increases with bilateral PWS. Patients may experience complications related to refractory seizures and anticonvulsants, visual
loss and blindness from glaucoma, cosmetic deformities, and other manifestations of soft-tissue involvement.
Of 60 patients in the combined series from Children's Hospital, Boston, 2 deaths (3.3%) have been reported (Erba and Cavazutti, 1990; Riviello et al, 1998). In earlier cases reported by Erba and Cavazutti, 1 death occurred in the postoperative period, after epilepsy surgery; in recent cases, 1 death occurred secondary to intractable seizures. Oakes reported 4 deaths in 30 patients (14%).
Race: No racial differences have been reported. Sex: Both sexes are affected equally. Age:
The typical patient presents at birth with facial angiomas; however, not all children with facial angiomas and PWS have SWS, which raises certain diagnostic and prognostic concerns. In the "incomplete" forms of SWS, CNS angiomas occur without cutaneous features (Type III, Roach Scale), and therefore, no suspicion of SWS arises until a seizure or other neurologic problem develops. Thus, the diagnosis of SWS is not always straightforward. Ocular manifestations, glaucoma and blindness
o
Glaucoma typically occurs in SWS only when the PWS involves the eyelids. The incidence ranges from 30-71%. Glaucoma may be present at birth but can develop at any age, even in adults. Treatment includes yearly examinations, looking for optic nerve damage (with measurement of IOP and visual fields) and corneal diameter and refractive changes in children. Glaucoma usually occurs only with an ipsilateral facial PWS, although it may be bilateral when facial involvement is bilateral. Contralateral glaucoma may develop, although rarely. Glaucoma also may occur without neurologic involvement (Type II, Roach Scale). Glaucoma in SWS is produced by mechanical obstruction of the angle of the eye, elevated episcleral venous pressure, or hypersecretion of fluid by either the choroidal hemangioma or ciliary body. The anterior chamber angle abnormality is consistently seen in the infantile glaucoma cases in SWS, while increased episcleral venous pressure may have a key role in late-onset glaucoma cases in SWS. Decreased vision and blindness result from untreated
glaucoma, with increased IOP leading to optic nerve damage. An acceptable range of IOP is 10-22 mm Hg.
Buphthalmos (hydrophthalmia): Enlargement of the eye occurs from the same mechanisms as glaucoma.
Physical:
PWS (see Picture 1) Macrocephaly Eye - Buphthalmos, heterochromia of iris, tomato-catsup color of the fundus (ipsilateral to the nevus flammeus) with glaucoma, possibility of choroidal angioma visible with an ophthalmoscope Soft-tissue hypertrophy Neurologic signs
o o o o o
Developmental delay/mental retardation Learning problems Attention deficit hyperactivity disorder Hemiparesis Visual loss
HemianopsiaOther Problems to be Considered: Headache, chronic Vascular malformations and hematomas of the brain PWS - May be isolated, occurring without SWS Arteriovenous malformation - May calcify Macrocephaly with SWS - Related to hydrocephalus or intracranial hypertension, secondary to the abnormal venous drainage Cyst of the posterior fossa with partial cerebellar agenesis in association with facial angiomas - Angioma flat or tuberous, lies in the territory of the first division of the trigeminal nerve; may be familial
Epilepsy with bilateral occipital calcifications - Incomplete SWS versus celiac disease Klippel-Trenaunay-Weber syndrome - Hemihypertrophy and hemangiomas; may occur with SWS; however, Klippel-Trenaunay-Weber associated with choroid plexus enhancement, atrophy, calcifications, and leptomeningeal enhancement Rendu-Osler-Weber syndrome - Hereditary hemorrhagic telangiectasia von Hippel-Lindau syndrome - Cerebellar or spinal hemangioma with retinal angioblastoma, pancreatic cysts, and renal cell carcinoma Wyburn-Mason syndrome - Retinal arteriovenous angioma Shapiro-Shulman syndrome - Bilateral facial nevi and abnormal venous drainage Divry-van Bogaert syndrome - Leptomeningeal angioma (noncalcifying) with diffuse sclerosis, progressive neurologic disorder, and livedo reticularis Bannayan-Zonna syndrome - Macrocephaly, lipomatosis, cutaneous hemangiomas Cobb syndrome - Cutaneomeningospinal angiomatosisLab Studies:
Cerebrospinal fluid (CSF) protein may be elevated, presumably secondary to microhemorrhage. Note that a major intracranial hemorrhage itself is rare in SWS, although microhemorrhage may be common.
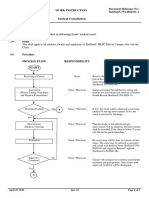
Imaging Studies:
Neuroimaging studies: Besides the clinical examination, these have been the procedures of choice to establish the diagnosis. Historically these are skull radiograph, angiography, CT scan, MRI, MRI with gadolinium, and functional imaging with SPECT or positron emission tomography (PET). Skull radiograph
o
The skull x-ray may show the classical "tram-line," or "tram-track" or "trolley-track," calcifications considered pathognomonic for SWS in the era prior to modern neuroimaging; however, these are often a late finding and may not be present initially. Wilms et al reported tram-track calcifications in tuberous sclerosis with calcification located in extensive cortical tubers; Borns and Rancier reported these in childhood leukemia.
Angiography: Angiography does not show the angioma but demonstrates a lack of superficial cortical veins, nonfilling of dural sinuses, and abnormal, tortuous veins that course toward the vein of Galen. CT scan: CT scan may show calcifications in infants and even neonates; other findings include brain atrophy, ipsilateral choroid plexus enlargement, abnormal draining veins, and a breakdown of the bloodbrain barrier with seizures. In a study of CT scans in 14 children with SWS by Terdjman et al, cortical calcifications were present in 12 patients (see Picture 2), localized atrophy in 10 patients, and enlargement of the choroid plexus and abnormal veins in 7 patients each. MRI
o
Although MRI does not show calcifications, gadolinium enhancement may show pial angioma; therefore, MRI may permit early diagnosis of SWS, even in the newborn with a facial PWS. Sugama et al reported that the most characteristic finding of SWS on MRI is enhancement of LAs following gadolinium, which may show an LA not seen on CT scan or angiography (see Picture 3); however, Fischbein reported that gadolinium enhancement may not be seen in every case. Other MRI findings include accelerated myelination around the LA, a large choroid plexus whose size correlates with the extent of the LA, and progressive sinovenous occlusion on MR venography. Of note, Benedikt et al reported pial angiomatosis with adjacent cortical atrophy on MRI in 4 patients in whom unenhanced MRI or CT scan was normal or showed only nonspecific findings. Bernal and Altman reported abnormal activation patterns in the occipital areas on functional MRI in patients with SWS. Lin et al reported perfusion MRI findings compatible with impaired venous drainage in an early case of SWS with new-onset seizures. MR spectroscopy showed increased choline but no reduction in Nacetyl aspartate (NAA). Other reports of MR spectroscopy have shown decreased NAA; Cakirer et al showed decreased NAA and increased choline in a patient with SWS, while the abnormal area also showed increased apparent diffusion coefficient (ADC) on diffuse MRI. Regarding the MR spectroscopy findings in these studies, the decreased NAA was considered as neuronal loss of dysfunction, and the elevated choline as a lack of normal development. Mentzel et al reported that BOLD (blood-oxygen-level-dependent) MR venography may be sensitive in detecting early venous abnormalities in a case of SWS, earlier than conventional MRI sequences.
o o
Single-photon emission computed tomography
o
This measures cerebral blood flow, demonstrates underperfusion in the area of the pial angioma, and therefore may detect a latent angioma not seen with other studies (see Picture 4 and Picture 5). With SPECT, Reid et al demonstrated hypoperfusion before calcifications, anomalous drainage, or enhancement developed on either CT scan or MRI. Griffiths et al showed that MRI and SPECT together might reveal different areas of involvement. Namer et al demonstrated a steal phenomenon during seizures, causing ischemia in remote areas, with subtraction ictal SPECT coregistered to MRI (SISCOM). Pinton demonstrated that the cortex is hyperperfused during the first year of life before the first seizures, with the classic hypoperfusion appearing after 1 year of age, even in those without epilepsy. Maria et al reported that enlargement of the choroid plexus correlates with abnormalities seen with SPECT.
Positron emission tomography: In a pre-MRI study by PET scan, Chugani et al demonstrated metabolic abnormalities in the structurally affected hemisphere that extended beyond the anatomic abnormalities detected by CT scan. This result suggested that PET might help identify suitable candidates for hemispherectomy or focal cortical resection. Other modalities
o
Riela et al studied the xenon Xe 133 inhalation technique in 4 patients with SWS and demonstrated decreased regional perfusion in the area of the LA, with impaired vasomotor reactivity documented in 2 patients. Decreased flow was prominent in 2 younger patients with normal neurologic status, suggesting that the blood flow abnormality may actually precede neurologic symptoms and may therefore cause or at least contribute to the deterioration. Recently, with quantitative proton magnetic resonance spectroscopy, Moore et al demonstrated an ipsilateral reduction of N-acetyl-aspartate, a neuronal marker, suggesting neuronal loss.
Summary of neuroradiologic findings: The maximum extent of disease may require a combination of structural and functional neuroimaging, since a mismatch may exist among neuroimaging modalities. Each modality may demonstrate abnormalities not detected by the other. This is
especially important in the identification of the epileptogenic region when considering surgery for refractory seizures. Other Tests:
EEG is used for evaluation of seizures and for localization of seizure activity in refractory seizures when epilepsy surgery is considered.
o
Brenner and Sharbrough reported unilateral reduction of background amplitude as the most consistent finding, in both the waking and sleep states, with activation procedures (hyperventilation and photic driving) decreased on the involved side. EEG findings predated calcifications. Epileptiform activity was limited to the involved hemisphere. In a recent study, Sassower et al reported marked voltage attenuation in the region of the angioma in 13 of 14 patients; polymorphic delta activity (PDA) occurred in 12 of 14 patients; in those with PDA, it was unilateral in 6 and correlated with the angiomatosis, and none with unilateral PDA had mental retardation. In 6 with bilateral PDA, 4 had mental retardation despite a unilateral angioma. Interictal spikes occurred in only 2 patients and were bilateral in 1 patient with unilateral disease. Seizures were recorded in 4 patients, and the ictal activity came from the periphery of the lesion. The seizures were refractory to treatment in 6 of 14 patients. Erba and Cavazzuti reported that late in the course of the syndrome, epileptiform activity might occur from the contralateral cortex. In a study conducted at Toronto, the EEG was normal in only 4%, background suppression occurred in 74% (unilateral in 64% and bilateral in 10%), and epileptiform discharges occurred in 22%. Jansen et al reported asymmetry in beta activity before and after diazepam administration in brain regions that structurally appeared intact; they suggested that diazepam-enhanced EEG may provide information on functional involvement and monitor progression of the disease.
Findings in the work-up of SWS are summarized in Table 3. Table 3. Summary of Work-up Findings in Sturge-Weber Syndrome CSF analysis Elevated protein
Skull x-ray Angiography
Tram-track calcifications Lack of superficial cortical veins Nonfilling dural sinuses Abnormal, tortuous vessels Calcifications, tram-track calcifications Cortical atrophy Abnormal draining veins Enlarged choroid plexus Blood-brain barrier breakdown (during seizures) Contrast enhancement Gadolinium enhancement of LA Enlarged choroid plexus Sinovenous occlusion Cortical atrophy Accelerated myelination Hyperperfusion, early Hypoperfusion, late Hypometabolism Reduced background activity Polymorphic delta activity Epileptiform features
CT scan
MRI
SPECT PET EEG
Endocrinologic tests: The Sturge-Weber Foundation notes increasing use of growth hormone in its members. Some have developed a body habitus similar to that in Cushing syndrome. This has occurred around the time of puberty.
Histologic Findings: The leptomeninges appear thickened and discolored by the LA, which fills the subarachnoid space, and abnormal venous structures are seen. Biopsies typically are not performed in SWS. However, pathologic specimens, such as those examined by Norman and Schoene, show calcium deposits in the cerebral vessel walls, in perivascular tissue and, rarely, within neurons, and neuronal loss and gliosis occur. These pathologic abnormalities may occur at a distance from the actual vascular lesion. Di Trapeni et al, from epilepsy surgery cases, reported a mucopolysaccharide substance with calcium in the connective tissue of the vessels early on, that later increases in size and migrates outside the vessels. They postulated that anoxia, necrosis, and variations in calcium concentrations act only as secondary factors.
Hoffman et al have shown aluminum within the calcium concretions. Simonati et al have reported 4-layered microgyria below the angiomatosis. In skin biopsies of the port-wine stain in SWS, dilated ecstatic thin-walled vessels are seen in the superficial vascular plexus, but with no increase in the number of blood vessels. In trabeculectomy specimens in patients with SWS, abnormal collagen depositions and abundant vessels in the intra-trabecular spaces have been seen morphological abnormalities in the Schlemm canal. Hemangiomas in the trabecular meshwork are characteristic of SWS.
TREATMENTMedical Care: This includes anticonvulsants for seizure control, symptomatic and prophylactic therapy for headache, glaucoma treatment to reduce the IOP, and laser therapy for PWS.
Seizures: Since the seizures are typically focal, an anticonvulsant with efficacy in focal seizures is preferable (see anticonvulsant medications). Glaucoma: The goal of treatment is control of IOP to prevent optic nerve injury (please see the articles on glaucoma in eMedicine Ophthalmology journal). Medications either decrease the production of aqueous fluid or promote the outflow of aqueous fluid. Beta-antagonist eye drops reduce the production of aqueous fluid, adrenergic eye drops and miotic eye drops reduce IOP by promoting drainage, and carbonic anhydrase inhibitors decrease IOP by decreasing production of aqueous fluid. Headaches: Recurrent headaches can be treated with symptomatic and prophylactic medications (see Migraine Headache). o Kossoff et al recently evaluated 68 patients with SWS regarding headaches, identified through the Sturge-Weber Foundation. Mean onset of the headaches was 8 years. Fifty-five of the 68 patients had epilepsy as well. Twenty-two of these patients perceived that the headaches were a more significant problem compared to their epilepsy. A positive family history of headaches was seen in 37 of these patients. o Most of the patients were using only abortive treatment, mainly acetaminophen and ibuprofen, while only 15 were tried on preventative agents, including gabapentin, valproate, and amitriptyline (none were on beta-adrenergic blockers). The authors suggested that the headaches may be undertreated.
Stroke-like events: Aspirin has been used for headaches and to prevent vascular disease, although it typically is used in patients who have had neurological progression or recurrent vascular events. Aspirin use needs to be with extreme caution in children, because of the concern about Reye syndrome, and the risks and benefits need to be carefully weighed. Thomas-Sohl, Vaslow, and Maria have recommended 3-5 mg/kg/day of aspirin for stroke-like events, and they also recommended varicella and yearly influenza immunizations, because of association of varicella and influenza infections in Reye syndrome. Maria et al reported a decreased incidence of stroke-like events in 20 patients who received aspirin; of 119 stroke-like events, 31 occurred in patients treated with aspirin, whereas 88 of these events occurred in those not treated with aspirin. The authors suggested further investigation of aspirin treatment in SWS. PWS: These need to be evaluated within the first week of life and differentiated from hemangioma.
o
PWS are treated with laser therapy, which should start as soon as possible, since multiple treatments are needed and earlier treatment may reduce the number needed. Also, the smaller the lesion initially, the fewer the laser flashes needed to remove the lesion. Troilius et al reported on the potential psychological benefits from early treatment of PWS. In a survey of patients with PWS, 75% reported that the PWS had affected their lives negatively, 62% were convinced that their lives would improve if the PWS were removed, 47% suffered low self-esteem, and 28% said that the PWS made their school life and education more difficult. No persistent pigmentation changes or posttreatment scarring were reported after laser therapy.
Surgical Care: Surgery is desirable for refractory seizures, glaucoma, and specific problems related to various associated disorders, such as scoliosis.
Seizures, refractory seizures
o
Surgical options are available for seizures refractory to medical treatment, especially for focal seizures. Surgical procedures include focal cortical resection, hemispherectomy, corpus callosotomy, and recently, vagal nerve stimulation (VNS). SWS is considered one of the catastrophic epilepsies which, according to Holmes, result in poor seizure control and developmental outcome if not controlled early; however, criteria for medical intractability should be fulfilled before considering surgery.
Early surgery has been advocated specifically in SWS to improve outcome and prevent refractory seizures, developmental delay, and hemiparesis. In the era prior to modern neuroimaging, Alexander and Norman and, later, Alexander suggested exploratory craniotomy and lobectomy if the diagnosis was confirmed, even before seizures started, because they found that early onset seizures were associated with mental retardation. Predictors of poor outcome include the extent of the LA, a refractory seizure disorder, and relapsing or permanent motor deficits. Factors predicting a poor outcome (or indicating surgery) include the following: Early seizure onset Extensive LA Medically refractive seizures Relapsing or permanent motor deficits Headaches or mild trauma associated with transient motor deficits Evidence of progressive neurologic damage Focal seizures with subsequent generalization Increasing seizure frequency and duration Increasing duration of postictal deficits Increasing focal or diffuse atrophy Progressive atrophy or calcifications Development of hemiparesis Deterioration in cognitive functioning (loss of intellectual abilities) The Toronto group suggested that hemispherectomy is more successful if done during infancy, since earlier seizure control helps to preserve the function of the normal hemisphere. They now perform a hemispherectomy, resulting in better neurologic recovery, even with some residual finger movement. Alternatively, if the patient is not a candidate for a limited resection or hemispherectomy, such as when disease is bilateral, corpus callosotomy can be done or VNS can be administered. VNS has been shown to be effective for focal seizures; its mechanism of action is a putative increase in CNS inhibitory activity. In order to address these issues, the Sturge-Weber Foundation recruited a task force to evaluate epilepsy surgery in SWS. The following is a summary of recommendations for surgery in SWS, modified to include VNS: Hemispherectomy should not be done in every patient with SWS solely because of the emphasis on increasingly early
o o
surgery. Surgery is appropriate only for medically refractory seizures. Patients with intractable seizures and very localized lesions should have a limited resection that preserves as much normal tissue as possible. Video EEG and both structural and functional neuroimaging should be used to define the extent of the lesion and the site of seizure origin. Corpus callosotomy is reserved for patients with intractable atonic or tonic seizures leading to secondary injury who are not candidates for more definitive surgery. Surgery should be done only in a center with an ongoing pediatric epilepsy surgery program. Although the benefit of surgery for refractory seizures is accepted generally, additional work is needed to evaluate the natural history of the syndrome and the potential benefits and risks of surgery. VNS can be done in those who are not candidates for other surgical procedures. Summary: Data on the natural history of the disease are not yet sufficient to advocate hemispherectomy unless refractory seizures occur.
Glaucoma surgery: If medications are unable to lower IOP, surgery may be beneficial. Trabeculectomy increases the release of aqueous fluid from the anterior chamber and opens the outflow pathway. Goniotomy is similar but is done through the eye. A Molteno valve can be placed (similar to a shunt), and cyclodestructive procedures with either freezing or laser decrease the production of aqueous fluid.
Consultations: Primary-care providers should be educated about SWS. Consultations are needed from a neurologist, an epileptologist (especially if seizures are intractable), a dermatologist, a plastic surgeon, a psychologist, a psychiatrist, a neuropsychologist, and a neuroendocrinologist. Diet: No special diet is needed. Activity: No restrictions are needed except as mandated by associated conditions.
Das könnte Ihnen auch gefallen
- Herbal Recipes For AromatherapyDokument3 SeitenHerbal Recipes For AromatherapyAnumeha Jindal100% (4)
- The Chakras and Essential OilsDokument10 SeitenThe Chakras and Essential OilsAnumeha Jindal100% (4)
- Meditating With Essential OilsDokument2 SeitenMeditating With Essential OilsAnumeha JindalNoch keine Bewertungen
- Chapter 1 Part 1 Multiple ChoiceDokument4 SeitenChapter 1 Part 1 Multiple ChoiceArlanosaurusNoch keine Bewertungen
- From The Aromatherapy Recipe FilesDokument2 SeitenFrom The Aromatherapy Recipe FilesAnumeha JindalNoch keine Bewertungen
- Other Aromatherapy RecpiesDokument13 SeitenOther Aromatherapy RecpiesAnumeha JindalNoch keine Bewertungen
- Barry S. Fogel, Donna B. Greenberg-Psychiatric Care of The Medical Patient-Oxford University Press (2015) PDFDokument1.813 SeitenBarry S. Fogel, Donna B. Greenberg-Psychiatric Care of The Medical Patient-Oxford University Press (2015) PDFhalamadrid77100% (2)
- How To Apply Essential Oils For Chakra BalancingDokument2 SeitenHow To Apply Essential Oils For Chakra BalancingAnumeha Jindal100% (1)
- Enls V 4 0 Protocol Coma FinalDokument16 SeitenEnls V 4 0 Protocol Coma Finalsucipto suciptoNoch keine Bewertungen
- Essential Oil SubstitutesDokument13 SeitenEssential Oil SubstitutesAnumeha JindalNoch keine Bewertungen
- Facomatosis Pubmed PDFDokument8 SeitenFacomatosis Pubmed PDFKevin ChaucaNoch keine Bewertungen
- Kepaniteraan Klinik RSD Mardi Waluyo Blitar - FK Unisma: Pembimbing: Dr. Utchu Tedja Mulya SP.BDokument35 SeitenKepaniteraan Klinik RSD Mardi Waluyo Blitar - FK Unisma: Pembimbing: Dr. Utchu Tedja Mulya SP.BDada DoniNoch keine Bewertungen
- Neurocutaneous SyndromesDokument8 SeitenNeurocutaneous SyndromesvcNoch keine Bewertungen
- RetinaDokument82 SeitenRetinafebienaNoch keine Bewertungen
- Chapter 1 Nov. 24 RevisionDokument12 SeitenChapter 1 Nov. 24 RevisionOdessa Fortu LandichoNoch keine Bewertungen
- Essential Oil of The Month: SandlewoodDokument2 SeitenEssential Oil of The Month: SandlewoodAnumeha Jindal0% (1)
- Axial DeformityDokument58 SeitenAxial DeformitynishantsinghbmeNoch keine Bewertungen
- Essential Tremor Diagnosis and TreatmentDokument32 SeitenEssential Tremor Diagnosis and TreatmentAntony JebarajNoch keine Bewertungen
- Rule of 4 and Brainstem SyndromesDokument2 SeitenRule of 4 and Brainstem SyndromesTracie TanNoch keine Bewertungen
- Motor Neuron Disease 1Dokument95 SeitenMotor Neuron Disease 1La Ode Rinaldi100% (1)
- Disease of Nervous System Lect 2Dokument62 SeitenDisease of Nervous System Lect 2Monirul IslamNoch keine Bewertungen
- Spina Bifida OCCULTADokument1 SeiteSpina Bifida OCCULTArebelswanteddot_comNoch keine Bewertungen
- Trauma Medula SpinalisDokument33 SeitenTrauma Medula Spinalisintan rizka ndNoch keine Bewertungen
- Asking and Showing Rooms in A Hospital-1Dokument12 SeitenAsking and Showing Rooms in A Hospital-1VitaNoch keine Bewertungen
- The Hepatorenal SyndromeDokument26 SeitenThe Hepatorenal SyndromeWaraBawanaNoch keine Bewertungen
- Neurobehavior Disorder: Diatri Nari LastriDokument104 SeitenNeurobehavior Disorder: Diatri Nari LastriKurniati HatmiNoch keine Bewertungen
- Fenton Growth Chart Boy v1Dokument2 SeitenFenton Growth Chart Boy v1nurhapsari20100% (3)
- Intuitive Surgical JP Morgan PresentationDokument25 SeitenIntuitive Surgical JP Morgan PresentationmedtechyNoch keine Bewertungen
- SSEPDokument12 SeitenSSEPahippo100% (1)
- Nerve Examination-Leprosy 2Dokument52 SeitenNerve Examination-Leprosy 2Siska IxchaNoch keine Bewertungen
- Scoring BPSDDokument4 SeitenScoring BPSDayu yuliantiNoch keine Bewertungen
- Diagnosa & Tatalaksana DiabetesDokument46 SeitenDiagnosa & Tatalaksana DiabetesAdhelia Kusuma WardhaniNoch keine Bewertungen
- Infectious Disease Outbreak RRM PDFDokument75 SeitenInfectious Disease Outbreak RRM PDFmichlsy11Noch keine Bewertungen
- Karakteristik Gangguan Tidur Pada Penyakit Parkinson Berdasarkan Parkinson Disease SleepDokument8 SeitenKarakteristik Gangguan Tidur Pada Penyakit Parkinson Berdasarkan Parkinson Disease SleepAfifa NingrumNoch keine Bewertungen
- MiopatiDokument7 SeitenMiopatiMarco HutagaolNoch keine Bewertungen
- Motor Neuron DiseaseDokument22 SeitenMotor Neuron DiseaseNabin SimkhadaNoch keine Bewertungen
- k20 - Stroke IskemikDokument35 Seitenk20 - Stroke IskemikZikri Putra Lan LubisNoch keine Bewertungen
- MNJ ToastDokument4 SeitenMNJ ToastRichard SuherlimNoch keine Bewertungen
- Dasar-Dasar Membaca Elektroensefalografi - Gea Pandhita SDokument84 SeitenDasar-Dasar Membaca Elektroensefalografi - Gea Pandhita Sgea pandhita sNoch keine Bewertungen
- Corticospinal Tract - Pyramidal TractDokument52 SeitenCorticospinal Tract - Pyramidal TractdrgokuNoch keine Bewertungen
- Neurotoksikologi: DR - Sandi Lesmana, SP.SDokument48 SeitenNeurotoksikologi: DR - Sandi Lesmana, SP.Sdita anisya putriNoch keine Bewertungen
- Ohtahara Syndrome: Corticosteroids (Prednisolone or ACTH) Are Occasionally HelpfulDokument2 SeitenOhtahara Syndrome: Corticosteroids (Prednisolone or ACTH) Are Occasionally HelpfulidscribddotcomNoch keine Bewertungen
- Hubungan Antara Kualitas Tidur Dengan Keparahan StrokeDokument8 SeitenHubungan Antara Kualitas Tidur Dengan Keparahan StrokeadindaanjaniNoch keine Bewertungen
- 3rd Announcement Konas-IX PerdossiDokument30 Seiten3rd Announcement Konas-IX PerdossiA Hadid FirdiyanshahNoch keine Bewertungen
- MYELITISDokument8 SeitenMYELITISFebrina RamadhaniNoch keine Bewertungen
- PPDS I Kesadaran Dan MBODokument87 SeitenPPDS I Kesadaran Dan MBOThivyaroobiniNoch keine Bewertungen
- Anatomy of The Mental and Neurobehavior DisordersDokument57 SeitenAnatomy of The Mental and Neurobehavior DisordersiqiqiqiqiqNoch keine Bewertungen
- Kuesioner NandaDokument8 SeitenKuesioner NandaAnanda AsmaraNoch keine Bewertungen
- Neuroradiology: Sony Sutrisno Department of Radiology Krida Wacana Christian UniversityDokument46 SeitenNeuroradiology: Sony Sutrisno Department of Radiology Krida Wacana Christian UniversityPaulus AnungNoch keine Bewertungen
- Brain Abcess: Ahmad Usama Wali House Servant Medical 1Dokument28 SeitenBrain Abcess: Ahmad Usama Wali House Servant Medical 1Ahmad Talha WaliNoch keine Bewertungen
- SpondilodiscytisDokument16 SeitenSpondilodiscytischristinawiyaniputriNoch keine Bewertungen
- Neuroanatomi AriesDokument48 SeitenNeuroanatomi AriesAries Rahman HakimNoch keine Bewertungen
- Diagnosis Skdi Neuro NewDokument49 SeitenDiagnosis Skdi Neuro NewmerrykartikaNoch keine Bewertungen
- Neuroanatomi 2011Dokument51 SeitenNeuroanatomi 2011Farah MuthiaNoch keine Bewertungen
- Pendukung StrokeDokument202 SeitenPendukung StrokeNovita DuffNoch keine Bewertungen
- 1965 EchoencephalographyDokument4 Seiten1965 EchoencephalographyDaniela GasnașNoch keine Bewertungen
- BPPVDokument36 SeitenBPPVRizka AmaliaNoch keine Bewertungen
- Operasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarDokument10 SeitenOperasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarBlack Clover IdNoch keine Bewertungen
- Etiology, Classification, and Epidemiology of StrokeDokument33 SeitenEtiology, Classification, and Epidemiology of StrokeRenato VelitNoch keine Bewertungen
- DeliriumDokument21 SeitenDeliriumErnawati AfandiNoch keine Bewertungen
- 1.1.epidural or Extradural HematomaDokument5 Seiten1.1.epidural or Extradural HematomaCitrus Aurantifolia100% (1)
- BLOK 1.3 Jaras PenglihatanDokument43 SeitenBLOK 1.3 Jaras PenglihatanlenypsNoch keine Bewertungen
- Laporan Kasus - Buta KortikalDokument31 SeitenLaporan Kasus - Buta KortikalwadejackNoch keine Bewertungen
- Papilledema: Epidemiology, Etiology, and Clinical ManagementDokument11 SeitenPapilledema: Epidemiology, Etiology, and Clinical ManagementAita Utsukushi HyuugaNoch keine Bewertungen
- Gagal Ginjal Akut Dan Kronik: Divisi Ginjal & Hipertensi SMF/Lab - Ilmu Penyakit Dalam FK - UNS / RSUD DR - MoewardiDokument29 SeitenGagal Ginjal Akut Dan Kronik: Divisi Ginjal & Hipertensi SMF/Lab - Ilmu Penyakit Dalam FK - UNS / RSUD DR - MoewardiHabiby Habibaty QolbiNoch keine Bewertungen
- Diffuse Axonal InjuryDokument3 SeitenDiffuse Axonal InjuryAnirban GhoshNoch keine Bewertungen
- KKD NeuroDokument22 SeitenKKD NeuroFerdyNoch keine Bewertungen
- AspergillomaDokument20 SeitenAspergillomaFatur ReyhanNoch keine Bewertungen
- KortikospinalisDokument4 SeitenKortikospinalisAhmad SaifulNoch keine Bewertungen
- Kriteria Diagnostik McDonald 2017Dokument8 SeitenKriteria Diagnostik McDonald 2017SMF BEDAH SoebandiNoch keine Bewertungen
- Cerebral InfarctionDokument2 SeitenCerebral InfarctionMarie Aurora Gielbert MarianoNoch keine Bewertungen
- Congenital Glaucoma B4Dokument15 SeitenCongenital Glaucoma B4Prashantha VespanathanNoch keine Bewertungen
- Tugas Stase Saraf Dr. AsriDokument37 SeitenTugas Stase Saraf Dr. Asriluthfianisa azhariNoch keine Bewertungen
- Glaukoma UnilateralDokument11 SeitenGlaukoma UnilateralrenyNoch keine Bewertungen
- Index - : Professor Yasser MetwallyDokument11 SeitenIndex - : Professor Yasser MetwallyDrhikmatullah SheraniNoch keine Bewertungen
- Ocular Ischemic Syndrome Survey OphthalmologyDokument33 SeitenOcular Ischemic Syndrome Survey OphthalmologyamaiacNoch keine Bewertungen
- Age Related Macular DegenerationDokument21 SeitenAge Related Macular DegenerationAnumeha JindalNoch keine Bewertungen
- Micronutrients and AgeDokument9 SeitenMicronutrients and AgeAnumeha JindalNoch keine Bewertungen
- Flower Blossom Massage Oil RecipeDokument1 SeiteFlower Blossom Massage Oil RecipeAnumeha JindalNoch keine Bewertungen
- Exquisite Sandalwood Massage OilDokument1 SeiteExquisite Sandalwood Massage OilAnumeha JindalNoch keine Bewertungen
- Insomnia Relief Massage Oil RecipeDokument1 SeiteInsomnia Relief Massage Oil RecipeAnumeha JindalNoch keine Bewertungen
- The Third Eye (Brow) Chakra and Essential OilsDokument2 SeitenThe Third Eye (Brow) Chakra and Essential OilsAnumeha JindalNoch keine Bewertungen
- Lemon and Pomegranate Refresher RecipeDokument2 SeitenLemon and Pomegranate Refresher RecipeAnumeha JindalNoch keine Bewertungen
- Mexican Tres Leche Cake RecipeDokument2 SeitenMexican Tres Leche Cake RecipeAnumeha JindalNoch keine Bewertungen
- Cinnamon Vanilla Massage RecpieDokument1 SeiteCinnamon Vanilla Massage RecpieAnumeha JindalNoch keine Bewertungen
- Fruit 'N' Juice Breakfast Shake RecipeDokument1 SeiteFruit 'N' Juice Breakfast Shake RecipeAnumeha JindalNoch keine Bewertungen
- Lemon Beer Punch 1960s) RecipeDokument2 SeitenLemon Beer Punch 1960s) RecipeAnumeha JindalNoch keine Bewertungen
- Jell-O Fruit Juice Squares RecipeDokument2 SeitenJell-O Fruit Juice Squares RecipeAnumeha JindalNoch keine Bewertungen
- Clinical - Approach - To - The - Diagnosis IEM PDFDokument15 SeitenClinical - Approach - To - The - Diagnosis IEM PDFVictor Lage de AraujoNoch keine Bewertungen
- Soal Uts BikDokument7 SeitenSoal Uts Bikfitriani simanjuntakNoch keine Bewertungen
- Anaesthesia & Intensive Care Medicine Volume 11 Issue 4 2010 (Doi 10.1016/j.mpaic.2009.12.013) Ben Shelley Nick Sutcliffe - Total Intravenous AnaesthesiaDokument3 SeitenAnaesthesia & Intensive Care Medicine Volume 11 Issue 4 2010 (Doi 10.1016/j.mpaic.2009.12.013) Ben Shelley Nick Sutcliffe - Total Intravenous AnaesthesiamikhatiarNoch keine Bewertungen
- Suprarenal GlandDokument19 SeitenSuprarenal GlandKay BristolNoch keine Bewertungen
- MSK IV: Upper Limb and Shoulder: Brachial PlexusDokument7 SeitenMSK IV: Upper Limb and Shoulder: Brachial PlexusKevin Yixi RenNoch keine Bewertungen
- Electric Hot Water Bag IncidentDokument2 SeitenElectric Hot Water Bag IncidentKmt_AeNoch keine Bewertungen
- Essentials of Orthognathic Surgery, 2nd Edition: Book ReviewsDokument1 SeiteEssentials of Orthognathic Surgery, 2nd Edition: Book ReviewsPae Anusorn AmtanonNoch keine Bewertungen
- Cardiovascular MedicineDokument50 SeitenCardiovascular MedicineCarlos HernándezNoch keine Bewertungen
- Glustitch PDFDokument1 SeiteGlustitch PDFRossnani Juaing100% (1)
- WI-HSD-01 MALVAR Medical ConsultationDokument2 SeitenWI-HSD-01 MALVAR Medical ConsultationVictor BaluyotNoch keine Bewertungen
- DeshpandeDokument17 SeitenDeshpandedeekshithNoch keine Bewertungen
- Notice No. 152 - 2022 INICET Tentative Seat PositionDokument9 SeitenNotice No. 152 - 2022 INICET Tentative Seat PositionVetrivel TamizhNoch keine Bewertungen
- Master ListDokument100 SeitenMaster ListAris GonzalesNoch keine Bewertungen
- 2008 Article 29Dokument3 Seiten2008 Article 29Dea LeeteukNoch keine Bewertungen
- 666 CDR - Scale PDFDokument10 Seiten666 CDR - Scale PDFIkanpaus Di BlogspotNoch keine Bewertungen
- Fisiologi Saraf OtonomDokument32 SeitenFisiologi Saraf OtonomNiaNoch keine Bewertungen
- Non GAMCA Medical Check Up FormDokument1 SeiteNon GAMCA Medical Check Up FormNurman Hidayat100% (1)
- The Exorcist 2ooo: Dialogue ListDokument73 SeitenThe Exorcist 2ooo: Dialogue ListJunior TribbianiNoch keine Bewertungen
- AIIMSDokument7 SeitenAIIMSPrakash PandaNoch keine Bewertungen
- Reviews: Case Reports in Pediatric DentistryDokument1 SeiteReviews: Case Reports in Pediatric DentistryYaser JasNoch keine Bewertungen
- Defense of Learning Capstone Blood DriveDokument20 SeitenDefense of Learning Capstone Blood Driveapi-194147189Noch keine Bewertungen
- Cavernous Malformations, Venous Malformations, and Capillary TelangiectasiasDokument28 SeitenCavernous Malformations, Venous Malformations, and Capillary TelangiectasiasGilang PramanayudhaNoch keine Bewertungen