Beruflich Dokumente
Kultur Dokumente
Nursing Diagnosis For Seizure
Hochgeladen von
Kenneth ColeOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Diagnosis For Seizure
Hochgeladen von
Kenneth ColeCopyright:
Verfügbare Formate
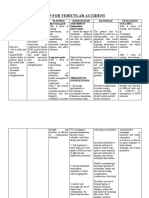
Nursing Diagnosis: Risk for Trauma/Suffocation Risk factors may include Weakness, balancing difficulties Cognitive limitations/altered consciousness
ss Loss of large or small muscle coordination Emotional difficulties Evidenced by [Not applicable; presence of signs and symptoms establishes an actual diagnosis.] Desired Outcomes Verbalize understanding of factors that contribute to possibility of trauma and/or suffocation and take steps to correct situation. Demonstrate behaviors, lifestyle changes to reduce risk factors and protect self from injury. Modify environment as indicated to enhance safety. Maintain treatment regimen to control/eliminate seizure activity. Identify actions/measures to take when seizure activity occurs. Nursing actions Rationale Alcohol, various drugs, and other stimuli (e.g., loss of sleep,flashing lights, prolonged television viewing) may increase brain activity, thereby increasing the potential for seizure activity. Enables patient to protect self from injury and recognize changes that require notification of physician/further intervention. Knowing what to do when seizure occurs can prevent injury/complications and decreases SOs feelings of helplessness.
Explore with patient the various stimuli that may precipitate seizure activity.
Discuss seizure warning signs (if appropriate) and usual seizure pattern. Teach SO to recognizewarning signs and how to care for patient during and after seizure. Keep padded side rails up with bed in lowest position, or place bed up against wall and pad floor if rails not available/appropriate.
Minimizes injury should seizures (frequent/generalized) occur while patient is in bed. Note: Most individuals seize in place and if in the middle of the bed, individual is unlikely to fall out of bed.
Encourage patient not to smoke except while supervised.
May cause burns if cigarette is accidentally dropped during aura/seizure activity. Use of helmet may provide added protection for individuals who suffer recurrent/severe seizures Reduces risk of patient biting and breaking glass thermometer or suffering injury if sudden seizure activity should occur. Patient may feel restless/need to ambulate or even defecate during aural phase, thereby inadvertently removing self from safe environment and easy observation. Understanding importance of providing for own safety needs may enhance patient cooperation Promotes patient safety. Helps maintain airway and reduces risk of oral trauma but should not be forced or inserted when teeth are clenched because dental and soft-tissue damage may result. Note: Wooden tongue blades should not be used because they may splinter and break in patients mouth. (Refer to ND: Airway Clearance/Breathing Pattern, ineffective, risk for Gentle guiding of extremities reduces risk of physical injury when patient lacks voluntary muscle control. Note: If attempt is made to restrain patient during seizure, erratic movements may increase, and patient may injure self or others.
Evaluate need for/provide protective headgear
Use tympanic thermometer when necessary to take temperature.
Maintain strict bed rest if prodromal signs/aura experienced. Explain necessity for these actions.
Stay with patient during/after seizure.
Turn head to side/suction airway as indicated. Insert plastic bite block only if jaw relaxed.
Cradle head, place on soft area, or assist to floor if out of bed. Do not attempt to restrain.
Document preseizure activity, presence of aura or unusual behavior, type of seizure activity (e.g., location/duration of motor activity, loss of consciousness, incontinence, eye activity, respiratory impairment/cyanosis), and frequency/recurrence. Note whether patient fell, expressed vocalizations, drooled, or had automatisms (e.g., lipsmacking, chewing, picking at clothes). Perform neurological/vital sign check after seizure, e.g., level of consciousness, orientation, ability to comply with simple commands, ability to speak; memory of incident; weakness/motor deficits; blood pressure (BP), pulse/respiratory rate.
Helps localize the cerebral area of involvement
Documents postictal state and time/completeness of recovery to normal state. May identify additional safety concerns to be addressed Patient may be confused, disoriented, and possibly amnesic after the seizure and need help to regain control and alleviate anxiety. May display behavior (of motor or psychic origin) that seems inappropriate/irrelevant for time and place. Attempts to control or prevent activity may result in patient becoming aggressive/combative. May be result of repetitive muscle contractions or symptom of injury incurred, requiring further evaluation/intervention.
Reorient patient following seizure activity.
Allow postictal automatic behavior without interfering while providing environmental protection.
Investigate reports of pain. Observe for status epilepticus, i.e., one tonic-clonic seizure after another in rapid succession. This is a life-threatening emergency that if left untreated could cause metabolic acidosis, hyperthermia, hypoglycemia, arrhythmias, hypoxia, increased intracranial pressure, airway obstruction,
and respiratory arrest. Immediate intervention is required to control seizure activity and prevent permanent injury/death. Note: Although absence seizures may become static, they are not usually life-threatening. Specific drug therapy depends on seizure type, with some patients requiring polytherapy or frequent medication adjustments. AEDs raise the seizure threshold by stabilizing nerve cell membranes, reducing the excitability of the neurons, or through direct action on the limbic system, thalamus, and hypothalamus. Goal is optimal suppression of seizure activity with lowest possible dose of drug and with fewest side effects. Cerebyx reaches therapeutic levels within 24 hr and can be used for nonemergent loading while waiting for other agents to become effective. Note: Some patients require polytherapy or frequent medication adjustments to control seizure activity. This increases the risk of adverse reactions and problems with adheren
Administer medications as indicated: Antiepileptic drugs (AEDs), e.g., phenytoin (Dilantin), primidone (Mysoline), carbamazepine (Tegretol), clonazepam (Klonopin), valproic acid (Depakene), divalproex (Depakote), acetazolamide (Diamox), ethotoin (Peganone), methsuximide (Celotin), fosphenytoin (Cerebyx);
Nursing Diagnosis: Risk for ineffective Airway Clearance/Breathing Pattern
Risk factors may include Neuromuscular impairment Tracheobronchial obstruction Perceptual/cognitive impairment Evidenced by [Not applicable; presence of signs and symptoms establishes an actual diagnosis.]
Desired Outcomes Respiratory Status: Ventilation Maintain effective respiratory pattern with airway patent/aspiration prevented. Rationale Nursing actions Encourage patient to empty mouth of dentures/foreign objects if aura occurs and to avoid chewing gum/sucking lozenges if seizures occur without warning. Place in lying position, flat surface; turn head to side during seizure activity. Loosen clothing from neck/chest and abdominal areas.
Reduces risk of aspiration/foreign bodies lodging in pharynx. Promotes drainage of secretions; prevents tongue from obstructing airway.
Facilitates breathing/chest expansion. If inserted before jaw is tightened, these devices may prevent biting of tongue and facilitate suctioning/respiratory support if required. Airway adjunct may be indicated after cessation of seizure activity if patient is unconscious and unable to maintain safe position of tongue. Reduces risk of aspiration/asphyxiation. Note: Risk of aspiration is low unless individual has eaten within the last 40 min. May reduce cerebral hypoxia resulting from decreased circulation/oxygenation secondary to vascular spasm during seizure. Note:Artificial ventilation during general seizure activity is of limited or no benefit because it is not possible to move air in/out of lungs during sustained contraction of respiratory musculature. As seizure abates, respiratory function will return unless a secondary problem
Insert plastic airway or soft roll as indicated and only if jaw is relaxed.
Suction as needed. Administer supplemental oxygen/bag ventilation as needed postictally.
exists (e.g., foreign body/aspiration). Prepare for/assist with intubation, if indicated. Presence of prolonged apnea postictally may require ventilatory support.
Das könnte Ihnen auch gefallen
- Hypertensive Crisis: - Alexter John C. Fajardo M.DDokument49 SeitenHypertensive Crisis: - Alexter John C. Fajardo M.DAlexter John Cabalonga FajardoNoch keine Bewertungen
- PathophysiologyDokument52 SeitenPathophysiologyVisalini Chandran67% (3)
- Therapeutic Apheresis Operator Competency Aug06Dokument43 SeitenTherapeutic Apheresis Operator Competency Aug06Jose Gregorio Riobueno BolivarNoch keine Bewertungen
- Proximal Humerus FracturesDokument4 SeitenProximal Humerus FracturesParidhi MittalNoch keine Bewertungen
- Ineffective Airway ClearanceDokument2 SeitenIneffective Airway ClearancePatrick Arvin Ballesteros BarcarseNoch keine Bewertungen
- HE Caregiving GR11 Q2 Module 4 FinalDokument19 SeitenHE Caregiving GR11 Q2 Module 4 FinalKenneth Cole75% (4)
- Hydrotherapy Indi ContraDokument71 SeitenHydrotherapy Indi Contrateam7MFkkOP YTNoch keine Bewertungen
- Nursing Management of PatientDokument32 SeitenNursing Management of PatientNoky KiaNoch keine Bewertungen
- Self Care DeficitDokument4 SeitenSelf Care DeficitEllaine RamirezNoch keine Bewertungen
- NCPDokument3 SeitenNCPranee diane0% (1)
- Nicu NCP (Neo - Pnia)Dokument3 SeitenNicu NCP (Neo - Pnia)lorence_cachoNoch keine Bewertungen
- Types of WoundsDokument20 SeitenTypes of Woundscrazyghost258100% (2)
- LM Caregiving G10Dokument248 SeitenLM Caregiving G10Kenneth Cole95% (20)
- NCPDokument7 SeitenNCPAbbie TantengcoNoch keine Bewertungen
- Checklist 17: Head-to-Toe Assessment Disclaimer: Always Review and Follow Your Hospital Policy Regarding This Specific Skill. Safety ConsiderationsDokument3 SeitenChecklist 17: Head-to-Toe Assessment Disclaimer: Always Review and Follow Your Hospital Policy Regarding This Specific Skill. Safety ConsiderationsKimberly Joy GregorioNoch keine Bewertungen
- Risk For Injury NCP SeizuresDokument2 SeitenRisk For Injury NCP Seizurestimie_reyes88% (8)
- Diabetes and It's Oral ManifestationsDokument28 SeitenDiabetes and It's Oral ManifestationsYashpreetsingh BhatiaNoch keine Bewertungen
- Crohn Vs ColitisDokument5 SeitenCrohn Vs Colitiswbarnes7Noch keine Bewertungen
- Nursing Care Plan 2Dokument2 SeitenNursing Care Plan 2Isabel Barredo Del MundoNoch keine Bewertungen
- NCP Activity Intolerance Related To Decreased in Oxygen SupplyDokument3 SeitenNCP Activity Intolerance Related To Decreased in Oxygen SupplyKyle Stephen TancioNoch keine Bewertungen
- NCP AlteredDokument3 SeitenNCP AlteredShaira TillahNoch keine Bewertungen
- Case Study: Christine Joy P. de Chavez, SNDokument23 SeitenCase Study: Christine Joy P. de Chavez, SNHELLONoch keine Bewertungen
- Nursing Care Plan For Low SelfDokument3 SeitenNursing Care Plan For Low SelfMarissa AsimNoch keine Bewertungen
- Activity IntoleranceDokument2 SeitenActivity Intoleranceayra_alegreNoch keine Bewertungen
- Gout N C P BY BHERU LALDokument1 SeiteGout N C P BY BHERU LALBheru LalNoch keine Bewertungen
- NCP Acute PainDokument3 SeitenNCP Acute PainSheene Lysethea Sioteco AguilosNoch keine Bewertungen
- Activity IntoleranceDokument2 SeitenActivity IntoleranceDiane AbanillaNoch keine Bewertungen
- Ortho NCPDokument1 SeiteOrtho NCPErjohn Vincent Lim100% (1)
- Inneffective Health Maintenence Care PlanDokument3 SeitenInneffective Health Maintenence Care PlanTammy Litzenberger-HarrisNoch keine Bewertungen
- NCP - Acute PainDokument1 SeiteNCP - Acute PainjsthrNoch keine Bewertungen
- Emj Cases : Questions For Case 1Dokument8 SeitenEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- Impaired Gas ExchangeDokument10 SeitenImpaired Gas ExchangeWardinatul ImanNoch keine Bewertungen
- Biopsy: Assessment Diagnosis Planning Intervention Rationale EvaluationDokument5 SeitenBiopsy: Assessment Diagnosis Planning Intervention Rationale EvaluationDan HizonNoch keine Bewertungen
- Discharge Plan For AppendectomyDokument1 SeiteDischarge Plan For AppendectomyMyra AtuleNoch keine Bewertungen
- NCPDokument10 SeitenNCPNefre Dayap DarrocaNoch keine Bewertungen
- Risk For AspirationDokument1 SeiteRisk For Aspirationmmcgee01Noch keine Bewertungen
- Ineffective Health MaintenanceDokument1 SeiteIneffective Health Maintenancedragon3466Noch keine Bewertungen
- NCP For Acute PainDokument4 SeitenNCP For Acute PainimnasNoch keine Bewertungen
- CELINDokument9 SeitenCELINaikoestrellaNoch keine Bewertungen
- NCP Set 1Dokument18 SeitenNCP Set 1Augene Toribio50% (2)
- NCPDokument4 SeitenNCPyasayayasay yasayNoch keine Bewertungen
- NCPDokument1 SeiteNCPTalTal Balcera Beniten100% (1)
- Gordon'S Functional Health Pattern I. Health Perceptual PatternDokument2 SeitenGordon'S Functional Health Pattern I. Health Perceptual Patternjoyrena ochondraNoch keine Bewertungen
- NCP CarpioDokument7 SeitenNCP CarpioFrancis Polycarp DiazNoch keine Bewertungen
- NCP 1Dokument7 SeitenNCP 1Roldan VidadNoch keine Bewertungen
- Generic Name Mechanism of Action Indications Contraindication Side Effects Nursing ResponsibilitiesDokument2 SeitenGeneric Name Mechanism of Action Indications Contraindication Side Effects Nursing ResponsibilitiestaekadoNoch keine Bewertungen
- Why Do Human Cells Rely Far More On Glucose and Fat For The Energy Than On ProteinDokument4 SeitenWhy Do Human Cells Rely Far More On Glucose and Fat For The Energy Than On ProteinHamda HassanNoch keine Bewertungen
- NCP Close Complete Fracture Knowledge DeficitDokument2 SeitenNCP Close Complete Fracture Knowledge DeficitArt Christian Ramos0% (1)
- NCP 3Dokument2 SeitenNCP 3Richson Bacay100% (1)
- Impaired Physical MobilityDokument2 SeitenImpaired Physical MobilityJayson OlileNoch keine Bewertungen
- Discharge PlanningDokument1 SeiteDischarge PlanningzbestgurlNoch keine Bewertungen
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDokument2 SeitenNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaNoch keine Bewertungen
- BSN 215 Reflection Essay - LagoDokument2 SeitenBSN 215 Reflection Essay - LagoAlliahkherzteen LagoNoch keine Bewertungen
- NCP For Ruptured AppendicitisDokument2 SeitenNCP For Ruptured AppendicitisJansen Arquilita RiveraNoch keine Bewertungen
- NCPDokument2 SeitenNCPVince John SevillaNoch keine Bewertungen
- OB Nursing Care PlanDokument3 SeitenOB Nursing Care PlanLiza Marie Cayetano AdarneNoch keine Bewertungen
- Assessment Nursing Diagnosis Rationale Desired Outcome Interventions Justification EvaluationDokument7 SeitenAssessment Nursing Diagnosis Rationale Desired Outcome Interventions Justification EvaluationPJNoch keine Bewertungen
- AnxietyDokument3 SeitenAnxietyJenny Pearl Pasal100% (1)
- Ineffective Breathing PatternDokument3 SeitenIneffective Breathing PatternErickson OcialNoch keine Bewertungen
- Case IcuDokument5 SeitenCase IcuTrisha SuazoNoch keine Bewertungen
- BFC NCPDokument2 SeitenBFC NCPMonica Melo HernandezNoch keine Bewertungen
- Pharmacologic Class: Contraindications: CNS: Headache, BeforeDokument4 SeitenPharmacologic Class: Contraindications: CNS: Headache, BeforeGwyn RosalesNoch keine Bewertungen
- As Needed.: Environmental Stimuli 6Dokument4 SeitenAs Needed.: Environmental Stimuli 6Nicole GumolonNoch keine Bewertungen
- NCPDokument3 SeitenNCPJoevelyn LaynoNoch keine Bewertungen
- JM CarbocisteineDokument1 SeiteJM CarbocisteineKatrina MagtalasNoch keine Bewertungen
- Nursing Care Plan Orthopedic Philipine CenterDokument4 SeitenNursing Care Plan Orthopedic Philipine CenterAnonymous NZTQVgjaNoch keine Bewertungen
- NCP For StokeDokument5 SeitenNCP For StokeMemedNoch keine Bewertungen
- BETAXOLOLDokument2 SeitenBETAXOLOLjulieNoch keine Bewertungen
- Nursing Care Plan: Fluid Volume DeficitDokument2 SeitenNursing Care Plan: Fluid Volume DeficitGenEsis CarandangNoch keine Bewertungen
- ThyroidectomyDokument11 SeitenThyroidectomySherina W. EddingNoch keine Bewertungen
- Nadja Assignment CompleteDokument3 SeitenNadja Assignment CompleteNadja JamilahNoch keine Bewertungen
- Department of Education: Republic of The PhilippinesDokument3 SeitenDepartment of Education: Republic of The PhilippinesKenneth ColeNoch keine Bewertungen
- Just ForDokument1 SeiteJust ForKenneth ColeNoch keine Bewertungen
- Cancer of The Larynx ComDokument10 SeitenCancer of The Larynx ComKenneth ColeNoch keine Bewertungen
- Case Report: Perioperative Management of A Patient With Secreting Paraganglioma Undergoing Cesarean SectionDokument3 SeitenCase Report: Perioperative Management of A Patient With Secreting Paraganglioma Undergoing Cesarean SectionYolanda FitrianiNoch keine Bewertungen
- Oral PathologyDokument31 SeitenOral PathologyAnonymous GyqTkXMwMNoch keine Bewertungen
- Phcist Letter Sept 2006Dokument52 SeitenPhcist Letter Sept 2006MichelNoch keine Bewertungen
- Stridor, Aspiration, and Cough in ChildrenDokument41 SeitenStridor, Aspiration, and Cough in ChildrenArif Rahman DmNoch keine Bewertungen
- 04 GTTDokument15 Seiten04 GTTAshish TuraleNoch keine Bewertungen
- Caso 2Dokument78 SeitenCaso 2Khairul ScNoch keine Bewertungen
- Spanish Medical Words and PhrasesDokument22 SeitenSpanish Medical Words and PhrasesAnushkaNoch keine Bewertungen
- A A To Raco AbdominalDokument64 SeitenA A To Raco AbdominalYgor AlbuquerqueNoch keine Bewertungen
- Aortic Regurgitation PathophysiologyDokument1 SeiteAortic Regurgitation Pathophysiologydana100% (1)
- AceDokument14 SeitenAceJustice Ace DaprozaNoch keine Bewertungen
- UCDokument6 SeitenUCapiv2010_808955526Noch keine Bewertungen
- MeningomyeloceleDokument34 SeitenMeningomyelocelerajan kumarNoch keine Bewertungen
- FLCCC Alliance MATHplus Protocol ENGLISHDokument3 SeitenFLCCC Alliance MATHplus Protocol ENGLISHJhonn BlackNoch keine Bewertungen
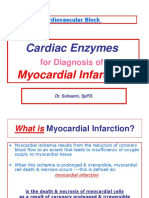
- Cardiac Enzymes - KulDokument39 SeitenCardiac Enzymes - KulAnonymous J1iWk2xNoch keine Bewertungen
- CPG DyslipidemiaDokument26 SeitenCPG DyslipidemiaRenzy SalumbreNoch keine Bewertungen
- Brooder PneumoniaDokument27 SeitenBrooder PneumoniaMohammad Rizwan SaeedNoch keine Bewertungen
- Þ" Hospital: Clinical and Scientific Rationale For The "MATH Treatment Protocol For COVID-19Dokument22 SeitenÞ" Hospital: Clinical and Scientific Rationale For The "MATH Treatment Protocol For COVID-19Doménica SánchezNoch keine Bewertungen
- Initial Antimicrobial Management of Sepsis: Review Open AccessDokument11 SeitenInitial Antimicrobial Management of Sepsis: Review Open AccessblanquishemNoch keine Bewertungen
- 14 - UveitisDokument4 Seiten14 - UveitisSpislgal PhilipNoch keine Bewertungen
- New Laboratory TestsDokument35 SeitenNew Laboratory TestsCar SadNoch keine Bewertungen
- Oceanic Question Bank Year 4Dokument358 SeitenOceanic Question Bank Year 4maryNoch keine Bewertungen
- Prevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenDokument10 SeitenPrevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenRiszki_03Noch keine Bewertungen