Beruflich Dokumente
Kultur Dokumente
RESUME Keperawatan B.inggris
Hochgeladen von
Ahmad Gelegar PersadaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
RESUME Keperawatan B.inggris
Hochgeladen von
Ahmad Gelegar PersadaCopyright:
Verfügbare Formate
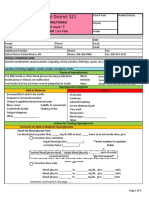
Nama : M.Nur Hidayatullah NIM : 11.
040
RESUME Nursing care in Tn. S with Diabetes Mellitus
Name Age Address education Job
: Tn. S : 57 Th : Pacitan : SLTP : Swasta
No. Reg Dx. Medis Date of Assessment
: 103067 : Diabetes Mellitus : 03 November 2011 Time 11.00 am
subjective: Clients say fatigue, frequent urinating at night, thirst, and frequent sleepiness. objective: o Client looks sleepy o Mucosal dry lips o GDS: 230 mg / dl o TTV: BP: 110/90 mmHg N: 88 x / min S: 36.6 0 C RR: 24 x / min
B1 (Breath) - Chest symmetric - No nostril breathing - Regular breathing rhythm - Not installed 02 B2 (Blood) - Heart sound s1, s2 single - No additional noise - No noise B3 ( Brain) - Awareness: composmentis - GCS: 4-5-6 B4 ( Bladder) - The color yellow is rather concentrated urine - Not attached catheter
Assasement: 1. Disorders of fluid balance and is associated with increased osmolarity electolyte secondary to hyperglycemia 2. Break the pattern of sleep disturbances associated with gangrene of the leg wound 3. Changes in nutrition less than body requirements related to insulin insufficiency Planning: Disorders of fluid balance and is associated with increased osmolarity electolyte secondary to hyperglycemia
Plan of Action: 1. Observation and record vital signs every 4 hours R /: Knowing the early occurrence of wound infection 2. Give fluids at least 2500 cc / hr R /: Maintaining hydration and circulation volume. 3. Measure BB every day R /: Preventing the spread and limit the spread of infection or cross contamination widespread 4. Monitor and record the input and expenditure BJ Urine
R /: Provides forecasts the need for fluid replacement, renal function, and the effectiveness of a given therapy 5. Note things such as nausea, abdominal pain, vomiting, gastric distention R /: Lack of fluid and electrolyte alter gastrointestinal motility, which will often cause vomiting and potentially will lead to lack of fluids or electrolytes
Implementation: 1. Observe and record vital signs every 4 hours 2. Giving fluids at least 2500 cc / hr 3. Measure BB every day 4. Monitor and record the input and expenditure BJ Urine 5. Record things like nausea, abdominal pain, vomiting, gastric distention evaluation: subjective: Clients say his body has not limp anymore objective: TTV: BP: 110/90 mmHg N: 88 x / min S: 36.6 0 C RR: 88 x / mnt:
Bibliography
Wartonah and tarwoto. , 2006. Basic human needs and the nursing process 3rd edition. Jakarta: Salemba Medika Carpenito, Lynda Juall.2007.Buku pocket keperawatan.Jakarta diagnosis: EGC Doengos, Marlyn E.1999. Nursing Care Plan for Issue 3. Jakarta: EGC
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Postpartum QuestionsDokument2 SeitenPostpartum QuestionsRayMendez100% (4)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Nursing Care Plan Peptic UlcerDokument2 SeitenNursing Care Plan Peptic UlcerMichael Joaquin0% (2)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Immobilization Splints: Presented by Siti Nur Rifhan KamaruddinDokument15 SeitenImmobilization Splints: Presented by Siti Nur Rifhan KamaruddinsnfhanNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Pre-Diabetes:: Don't Let It Lead To Type-2Dokument1 SeitePre-Diabetes:: Don't Let It Lead To Type-2ARIA MINDNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Carpal Tunnel SyndromeDokument3 SeitenCarpal Tunnel SyndromeAnonymous uTEAEbugNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- NCP For AnaphylacticDokument3 SeitenNCP For AnaphylacticRommar Romero67% (3)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hemo PathDokument2 SeitenHemo PathanadiguptaNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Geeky Medics DocumentationDokument3 SeitenGeeky Medics DocumentationGus LionsNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Istilah Kedokteran in JapaneseDokument8 SeitenIstilah Kedokteran in JapaneseYusrina AdaniNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Herpetic Keratitis: Jenan GhaithDokument8 SeitenHerpetic Keratitis: Jenan GhaithJenan GhaithNoch keine Bewertungen
- UPDRS-8 Robert Hauser MD 5-7-12Dokument1 SeiteUPDRS-8 Robert Hauser MD 5-7-12Robert A. Hauser, MDNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Comm NCPDokument3 SeitenComm NCProgeletteNoch keine Bewertungen
- Bell's PalsyDokument37 SeitenBell's Palsywahyu_sitaNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Diabetes Hyperglycemia Emergency Care PlanDokument2 SeitenDiabetes Hyperglycemia Emergency Care Planapi-405196113Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Acute PancreatitisDokument11 SeitenAcute PancreatitisChoirina QomariahNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- A 49Dokument2 SeitenA 49Daffaa' MahardikaNoch keine Bewertungen
- Barotrauma HTMLDokument5 SeitenBarotrauma HTMLKatarinaNoch keine Bewertungen
- Therapeutic EquivalenceDokument2 SeitenTherapeutic EquivalenceyuppierajNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Veritas Health Low Back Pain Exercise Guide PDFDokument6 SeitenVeritas Health Low Back Pain Exercise Guide PDFvipinTHOTNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Lynn13 4Dokument2 SeitenLynn13 4Harley Justiniani Dela CruzNoch keine Bewertungen
- IPL Client History v1 - 7Dokument8 SeitenIPL Client History v1 - 7Karen Dodd100% (1)
- ParonychiaDokument1 SeiteParonychiaFaishal HusniNoch keine Bewertungen
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokument6 SeitenAssessment Diagnosis Planning Intervention Rationale EvaluationBalloonsRus PHNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Coba PDFDokument2 SeitenCoba PDFAnton RyanNoch keine Bewertungen
- DokumenDokument4 SeitenDokumenFkep2015Noch keine Bewertungen
- 37 - Acute Rheumatic FeverDokument1 Seite37 - Acute Rheumatic FevernasibdinNoch keine Bewertungen
- Prader Willi SyndromeDokument14 SeitenPrader Willi Syndromeapi-471834071Noch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- CaseDokument3 SeitenCasebLessy_july16Noch keine Bewertungen
- Deep Vein Thrombosis: Causes Treatment Complications PreventionDokument5 SeitenDeep Vein Thrombosis: Causes Treatment Complications PreventionRaghav Suri100% (2)
- Oswestry Chronic Low BackDokument2 SeitenOswestry Chronic Low BackimurtonNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)