Beruflich Dokumente
Kultur Dokumente
Riesgo Cardiovascular y Proteina de Soya PDF
Hochgeladen von
docneiraOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Riesgo Cardiovascular y Proteina de Soya PDF
Hochgeladen von
docneiraCopyright:
Verfügbare Formate
European Journal of Clinical Nutrition (2013) 67, 5863 & 2013 Macmillan Publishers Limited All rights reserved
0954-3007/13 www.nature.com/ejcn
ORIGINAL ARTICLE
Effect of soybean protein on novel cardiovascular disease risk factors: a randomized controlled trial
CM Rebholz1, K Reynolds1,2, MR Wofford3, J Chen1,4, TN Kelly1, H Mei1, PK Whelton1 and J He1,4 BACKGROUND/OBJECTIVES: Cardiovascular disease (CVD) is the leading cause of death in the United States and the world. Clinical trials have suggested that soybean protein lowers lipids and blood pressure. The effect of soybean protein on novel CVD risk factors has not been well studied. The objective of this study was to examine the effect of soybean protein on biomarkers of inammation, endothelial dysfunction and adipocytokines. SUBJECTS/METHODS: The effect of 8 weeks of 40 g of soybean protein supplement (89.3 mg isoavones), 40 g of milk protein supplement and 40 g of complex carbohydrate placebo was examined in a randomized, placebo-controlled, double-blind, threephase crossover trial among adults in New Orleans, Louisiana and Jackson, Mississippi. Plasma levels of inammation biomarkers (C-reactive protein, interleukin-6, tumor necrosis factor-a), endothelial dysfunction biomarkers (E-selectin, intercellular adhesion molecule-1, vascular cell adhesion molecule-1, thrombomodulin) and adipocytokines (high-molecular weight adiponectin, leptin, resistin) were measured at baseline and at the end of each intervention using immunoturbidimetric and enzyme-linked immunosorbent assay techniques. RESULTS: Soy protein supplementation resulted in a signicant mean net change (95% condence interval) in plasma E-selectin of 3.93 ng/ml ( 7.05 to 0.81 ng/ml; P 0.014) compared with milk protein, and in plasma leptin of 2089.8 pg/ml ( 3689.3 to 490.3 pg/ml; P 0.011) compared with carbohydrate. There were no signicant changes in any other risk factors. CONCLUSIONS: Soy protein supplementation may reduce levels of E-selectin and leptin. Further research is warranted to investigate the mechanisms through which protein may confer protective effects on novel CVD risk factors. European Journal of Clinical Nutrition (2013) 67, 5863; doi:10.1038/ejcn.2012.186; published online 28 November 2012 Keywords: adipokines; carbohydrates; clinical trial; inammation; milk proteins; soybean proteins
INTRODUCTION Cardiovascular disease (CVD) is the primary cause of mortality in the United States and the world.1,2 Epidemiologic studies have found that biomarkers of systemic inammation, endothelial dysfunction and adipocytokines are associated with an increased risk of CVD morbidity and mortality, independent of traditional CVD risk factors.35 Endothelial dysfunction is the initial detectable step in the process of developing atherosclerotic CVD, and the inammatory system is integral to facilitating further atherosclerosis lesion pathogenesis leading to clinical CVD events.6 Adipocytokines are thought to act through several pathways to realize cardio-metabolic effects, including mediating glucose and lipid metabolism, the inammatory response and endothelial function.7 Examining changes in biomarkers of the inammatory system, endothelial function and adipocytokines allows for the detection of early indications of change in CVD risk. Soybean protein is recommended as a healthy food for cardiovascular health based primarily on its favorable effect on cholesterol and blood pressure.810 The American Heart Association recommends daily consumption of 25 g or more of soy protein with phytoestrogens in a diet low in saturated fat and cholesterol to improve the lipid prole and reduce CVD risk.8 Some clinical studies have investigated the effect of soy protein
on inammatory biomarkers, endothelial dysfunction biomarkers and adipocytokines, as early markers of CVD risk.1116 However, the existing evidence is limited and inconsistent. Evaluating the impact of dietary interventions, such as soybean protein supplementation, on novel CVD risk factors may provide justication for widespread implementation of such interventions for the prevention and treatment of CVD and its related morbidity and mortality. The objective of this study was to examine the effect of soybean protein, milk protein and complex carbohydrate supplementation on plasma levels of biomarkers of inammation, endothelial dysfunction and adipocytokines. SUBJECTS AND METHODS Study design
This study was a randomized, double-blinded and placebo-controlled trial. This study utilized a three-phase crossover study design with a 2-week runin period and 3-week washout periods between interventions. Eligible participants were allocated to receive 40 g/day of soy protein (89.3 mg isoavones), 40 g/day of milk protein and 40 g/day of complex carbohydrate (placebo) in random order, each for 8 weeks. Written informed consent was obtained from each participant before the initial screening visit and before randomization. The institutional review boards at the Tulane University Health Sciences Center and the University of Mississippi Medical Center approved the study protocol.
1 Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA; 2Department of Research and Evaluation, Kaiser Permanente Southern California, Pasadena, CA, USA; 3Department of Medicine, University of Mississippi Medical Center, Jackson, MS, USA and 4Department of Medicine, Tulane University School of Medicine, New Orleans, LA, USA. Correspondence: Dr. J He, Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, 1440 Canal Street, Suite 2000, New Orleans, LA 70112, USA. E-mail: jhe@tulane.edu Received 6 June 2012; revised 21 October 2012; accepted 22 October 2012; published online 28 November 2012
Soy protein and novel cardiovascular risk factors CM Rebholz et al
59 Study participants
Study participants were men and women aged 22 years or older who had a mean systolic blood pressure from 120 to 159 mm Hg and a diastolic blood pressure from 80 to 95 mm Hg, based on the average of six readings at two screening visits. Individuals were excluded if they were taking antihypertensive medication, had a self-reported history of clinical CVD, cancer, chronic kidney disease (or a serum creatinine X1.7 mg/dl (150.3 mmol/l) for men and X1.5 mg/dl (132.6 mmol/l) for women), hypercholesterolemia (or serum total cholesterol X240 mg/dl (X6.2 mmol/l)), diabetes (or serum glucose X126 mg/dl (X7 mmol/l)), a body mass index X40 kg/m2, were pregnant or intended to become pregnant during the study, were consuming 414 alcoholic drinks per week, or were consuming X1.63 g/kg per day (85th percentile of dietary protein intake in the US general population) of dietary protein based on two 24-h dietary recalls. Study participants were recruited by mass mailing and work-site and community-based screenings in New Orleans, Louisiana and Jackson, Mississippi. Participant recruitment and the intervention occurred between October 2005 and April 2008. the samples were measured in duplicate. Plasma levels of all other biomarkers were measured using commercially available, sandwich enzyme-linked immunosorbent assay methods, with high-sensitivity assays for interleukin-6 (IL-6) and tumor necrosis factor-a (TNF-a) only (Quantikine human immunoassays, R&D Systems, Inc., Minneapolis, MN, USA). Optical density was measured using a microplate reader (ASYS Expert Plus microplate reader, Biochrom Ltd., Cambridge, UK). All samples that were measured with enzyme-linked immunosorbent assay methods were run in duplicate. A baseline questionnaire was administered to record demographic and lifestyle characteristics and medical history. Blood pressure, body weight, height and waist circumference were also measured at baseline. Computer software was used to calculate nutrient intakes from 24-h dietary recalls at baseline and at the end of each phase (Minnesota Nutrition Data System for Research, University of Minnesota, 2002). An overnight timed urine sample was collected at the baseline and termination visits to measure excretion of micronutrients. Side effects and compliance were assessed using a symptom questionnaire, counts of returned unconsumed packets and self-reported supplement calendar report.
Intervention
Study participants were randomly assigned to three sequences at a xed 1:1:1 allocation ratio. Randomization was stratied by clinic site, gender and hypertension status. We used a block size of six to ensure equal distribution of participants among the sequences. Randomization assignment was conducted centrally at the Data Coordinating Unit at Tulane University, employing a computer-generated assignment list, which could only be accessed by the data coordinator. All other research personnel and the study participants were unaware of treatment assignment. The soy protein, milk protein and complex carbohydrate supplements were provided by Solae, LLC (St Louis, MO, USA). Caloric and fat content was similar in all supplements. Milk protein supplements contained 10 mg of cholesterol, and soy protein supplements contained 89.3 mg of isoavones, which was not present in the other supplements. Supplement powders looked the same and were distributed in identical packets. Study participants were instructed to take the supplements twice per day; once in the morning and once in the evening in water or juice. Based on the participants two 24-h dietary recalls during screening visits, individualized recommendations were given in order for participants total energy intake to remain constant over the intervention periods.
Statistical analysis
The primary outcome of interest was the net change in biomarkers, which was calculated as the difference in biomarker levels at the end of each intervention/control phase. When duplicate measurements of samples were taken, the means of the two measurements were used for analysis. PROC MIXED of SAS version 9.2 (SAS Institute Inc., Cary, NC, USA) was used to obtain point estimates and standard errors of the treatment and sequence effects and to test for differences between treatments. An autoregressive correlation structure was used to account for within-subject correlation due to repeated measurements in the crossover study design. Mean levels of biomarkers according to intervention phase and net change in biomarkers according to all three comparisons between phases along with corresponding 95% condence intervals (CIs) were estimated with the LSMEANS statement. The carryover effect was assessed by testing the interaction between phase and treatment and the interaction was not statistically signicant. The intention-to-treat principle was used for all primary analyses. Sensitivity analyses were performed by (1) using logtransformed values, (2) restricting to those participants that completed all phases of the study and (3) those that consumed at least 85% of supplements based on returned packet counts. All tests are two-tailed and statistical signicance was assessed at an a level of 0.0167 (0.05/3 for the Bonferroni correction of multiple comparisons). For the power calculation, the standard deviations corresponding to net changes in biomarkers between phases were abstracted from previously published trials with a similar follow-up period as the present study.1820 With a pre-determined sample size and a Bonferroni-adjusted signicance level, the power for determining the difference in mean biomarkers in a crossover design study for two-tailed t tests was calculated. We estimated that it should be possible to recognize relatively small but important net changes in plasma levels of novel biomarkers with 80% statistical power.
Measurements
Study participants were instructed to fast for 10 h before their clinic visits for blood sample collection. Blood samples were promptly centrifuged at 3000 r.p.m. for 10 min at 4 1C. Serum and plasma were separated and aliquoted for different analyses at the clinical laboratory. Specimens were stored at 85 1C until analysis. Specimens from 102 study participants were available for this study. Blind duplicates of samples were collected, and biomarker levels were similar in the blind duplicates compared with the original samples. Plasma levels of C-reactive protein (CRP) were measured using a latex particle-enhanced, high-sensitivity immunoturbidimetric assay on the Olympus AU400e Analyzer (Beckman Coulter, Brea, CA, USA) with Kamiya reagents (Kamiya Biomedical Company, Seattle, WA, USA).17 Ten percent of
RESULTS The ow diagram summarizes study assignment according to randomization group and period (Figure 1). Conditional follow-up
Randomized (n=102)
Allocated to sequence A (n=32) Allocated to sequence B (n=35) Allocated to sequence C (n=35)
Completed soy protein (n=29)
Completed milk protein (n=34)
Completed carbohydrate (n=33)
Completed milk protein (n=23)
Completed carbohydrate (n=28)
Completed soy protein (n=27)
Completed carbohydrate (n=21)
Completed soy protein (n=27)
Completed milk protein (n=24)
Figure 1.
Flow diagram of study participant assignment and participation.
European Journal of Clinical Nutrition (2013) 58 63
& 2013 Macmillan Publishers Limited
Soy protein and novel cardiovascular risk factors CM Rebholz et al
60 rates for the rst, second and third phases were 94.1, 81.3 and 92.3%, respectively. Overall follow-up during the entire study period was similar for the three interventions: 81.4% for soy protein, 79.4% for milk protein and 80.4% for carbohydrate. Supplement consumption was similar for all three interventions and all three periods. According to supplement calendar reports for all interventions combined, study participants consumed an average of 92.1% of supplements provided for each phase and 84.5% of participants consumed at least 85% of their supplements. Based on overall counts by study staff of returned and unconsumed supplement packets, study participants consumed an average of 90.5% of their supplements and 76.0% of participants consumed at least 85% of their supplements. The average level of overnight urinary excretion of urea nitrogen was signicantly increased during the soy protein (467.4 mg/l) and milk protein (484.0 mg/l) supplementation interventions compared with the carbohydrate supplementation intervention (376.9 mg/l; P 0.01). The urea:creatinine ratio was also increased during protein interventions (soy: 8.7, milk: 8.7, carbohydrate: 6.8; Po0.0001). Baseline characteristics of the 102 study participants are shown in Table 1 according to randomization group. For the total study population, mean age was 46 years, 67% were males, and 29% were African-American. At baseline, mean body mass index was 29.9 kg/m2, mean fasting glucose level was 96.1 mg/dl (5.3 mmol/l), mean systolic/diastolic blood pressure was 127.5/82.3 mm Hg and mean total cholesterol was 196.5 mg/dl (5.1 mmol/l). There were no statistically signicant differences in baseline
Table 1.
Baseline characteristics* of 102 trial participants Randomization groups A (n 35) Age, years Male, n (%) African-American, n (%) Some college education, n (%) Current smoking, n (%) Alcohol drinking, n (%) Physical activity X3 times/week, n (%) Body-mass index, kg/m2 Systolic blood pressure, mm Hg Diastolic blood pressure, mm Hg Total cholesterol, mmol/l Glucose, mmol/l Creatinine, mmol/l
*Mean (s.d.) or frequency (percentage).
characteristics by randomization sequence assignment. There appeared to be variation in age and college education by randomization group, but it was not statistically signicant. The daily dietary nutrient intake based on 24-h dietary recall is presented according to intervention phase in Table 2. Total dietary protein intake was signicantly higher by an average of 30.2 g/day due to the higher intake of vegetable protein (29.9 g/day) during the soy protein intervention compared with the carbohydrate intervention. During the milk protein intervention, total dietary protein was signicantly higher by 33.2 g/day due to the higher intake of animal protein (33.8 g/day) compared with the carbohydrate intervention. Dietary carbohydrate intake was lower by 36.7 g/day during the soy protein intervention and by 41.3 g/ day during the milk protein intervention compared with the carbohydrate intervention. Daily intake of other dietary nutrients was not signicantly different across intervention phases. Mean plasma levels of biomarkers at baseline and at the end of each intervention with corresponding CIs are presented in Table 3. During the study, the lowest level of several biomarkers, including CRP, IL-6, TNF-a, E-selectin, intercellular adhesion molecule-1 (ICAM-1) and leptin, were observed at the end of the soy supplementation intervention. The lowest levels of vascular cell adhesion molecule-1 (VCAM-1) and resistin were observed at the end of milk protein supplementation intervention. The mean plasma levels of E-selectin and resistin were statistically signicantly different by phase, after accounting for multiple comparisons. Mean plasma levels of all other biomarkers were not statistically signicantly different by phase.
B (n 32) 42.7 (11.7) 20 (62.5%) 9 (28.1%) 27 (84.4%) 4 (12.5%) 12 (37.5%) 23 (74.2%) 29.5 (3.8) 126.9 (8.5) 82.7 (4.8) 5.3 (0.6) 5.4 (0.5) 97.2 (17.7)
C (n 35) 47.6 (9.2) 23 (65.7%) 13 (37.1%) 26 (74.3%) 4 (11.4%) 14 (40.0%) 20 (58.8%) 29.7 (4.9) 128.4 (11.3) 82.7 (7.0) 5.1 (0.7) 5.3 (0.5) 97.2 (17.7)
P-value 0.08 0.73 0.42 0.07 0.30 0.90 0.16 0.71 0.79 0.67 0.13 0.85 0.87
48.2 (11.7) 25 (71.4%) 8 (22.9%) 33 (94.3%) 1 (2.9%) 15 (42.9%) 18 (51.4%) 30.4 (4.8) 127.0 (8.3) 81.6 (4.9) 4.9 (0.7) 5.3 (0.5) 88.4 (26.5)
Table 2.
Nutrient
Mean (s.d.) daily dietary nutrient intake according to intervention phase Baseline (n 102) 2021.8 87.3 61.4 25.7 234.2 79.4 25.0 16.5 31.0 320.8 1.0 1.1 (566.9) (29.5) (26.4) (12.3) (78.6) (27.8) (10.8) (7.4) (11.0) (185.9) (2.7) (3.3) Soy protein (n 83) 2102.7 114.3 59.7 54.4 231.4 77.0 24.9 14.3 30.2 317.5 0.9 1.1 (705.7) (30.9) (25.7) (16.2) (91.0) (34.6) (13.4) (6.9) (14.0) (168.4) (3.2) (4.1) Milk protein (n 81) 2099.8 117.3 93.2 24.0 226.8 78.0 25.2 15.8 30.0 341.9 0.9 0.9 (596.5) (32.2) (29.9) (10.7) (80.4) (28.7) (10.5) (6.8) (12.3) (193.8) (1.8) (2.0) Carbohydrate (n 82) 2113.2 84.1 59.4 24.5 268.1 77.8 25.5 15.7 29.8 300.2 1.1 1.2 (643.1) (30.4) (26.0) (10.9) (89.7) (32.5) (12.6) (7.3) (13.5) (184.9) (4.4) (4.5) P-value 0.99 o0.0001 o0.0001 o0.0001 0.005 0.98 0.95 0.29 0.98 0.35 0.92 0.92
Energy, kcal Protein, g Animal protein, g Vegetable protein, g Carbohydrate, g Fat, g Saturated fat, g Polyunsaturated fat, g Monounsaturated fat, g Cholesterol, mg Daidzein, mg Genistein, mg
European Journal of Clinical Nutrition (2013) 58 63
& 2013 Macmillan Publishers Limited
Soy protein and novel cardiovascular risk factors CM Rebholz et al
61
Table 3.
Mean (95% condence interval) plasma levels of biomarkers according to comparison phase Baseline 2.44 (1.81, 3.06) 2.29 (1.91, 2.66) 1.45 (1.28, 1.62) 49.91 (45.34, 54.48) 674.5 (612.3, 736.8) 254.4 (232.3, 276.5) 4457.4 (4204.5, 4710.6) 2830.3 (2126.6, 3533.9) 17 668 (14 092, 21 245) 10.92 (9.57, 12.28) Soy protein 2.33 (1.71, 2.95) 1.57 (1.22, 1.93) 1.20 (1.03, 1.37) 42.43 (37.75, 47.10) 746.0 (685.7, 806.3) 262.6 (240.2, 285.1) 4514.2 (4259.1, 4769.4) 3332.6 (2618.6, 4046.6) 17 538 (13 900, 21 176) 8.28 (7.08, 9.48) Milk protein 2.65 (2.03, 3.26) 1.69 (1.33, 2.04) 1.22 (1.05, 1.39) 46.36 (41.70, 51.01) 737.2 (677.4, 797.0) 268.2 (245.8, 290.6) 4589.0 (4335.5, 4842.5) 3202.0 (2489.1, 3914.9) 18 195 (14 564, 21 825) 7.57 (6.38, 8.76) Carbohydrate 2.54 (1.92, 3.15) 1.76 (1.41, 2.12) 1.22 (1.05, 1.38) 43.17 (38.53, 47.81) 760.4 (701.2, 819.8) 266.1 (243.9, 288.4) 4455.9 (4203.7, 4708.1) 3439.0 (2726.7, 4151.4) 19 628 (16 001, 23 255) 8.30 (7.11, 9.48) Pvalue 0.74 0.05 0.04 0.002 0.23 0.69 0.64 0.018 0.06 0.009
Biomarker C-reactive protein, mg/l Interleukin-6, pg/ml Tumor necrosis factor-a, pg/ml E-selectin, ng/ml Vascular cell adhesion molecule-1, ng/ml Intercellular adhesion molecule-1, ng/ml Thrombomodulin, pg/ml High-molecular weight adiponectin, ng/ml Leptin, pg/ml Resistin, ng/ml
To convert C-reactive protein to nmol/l, multiply by 9.524. To convert interleukin-6 to IU/ml, multiply by 0.124. To convert tumor necrosis factor-a to IU/ml, multiply by 0.086. To our knowledge, there is no conversion to International Units currently available for the remaining novel biomarkers.
Table 4.
Net change (95% condence interval) and P-value for plasma levels of biomarkers according to comparison phases Soy protein vs carbohydrate 0.21 0.19 0.01 0.74 14.44 ( 0.78, 0.36) 0.47 ( 0.55, 0.18) 0.31 ( 0.14, 0.11) 0.84 ( 3.79, 2.30) 0.63 ( 74.78, 45.89) 0.64 Milk protein vs carbohydrate 0.11 0.08 0.01 3.19 23.25 ( 0.47, 0.68) 0.71 ( 0.44, 0.29) 0.69 ( 0.12, 0.13) 0.93 (0.10, 6.27) 0.04 ( 84.29, 37.79) 0.45 Soy protein vs milk protein 0.32 0.11 0.02 3.93 8.81 ( 0.90, 0.26) 0.28 ( 0.48, 0.26) 0.55 ( 0.15, 0.11) 0.78 ( 7.05, 0.81) 0.014 ( 52.66, 70.27) 0.78
Biomarker C-reactive protein, mg/l Interleukin-6, pg/ml Tumor necrosis factor-a, pg/ml E-selectin, ng/ml Vascular cell adhesion molecule-1, ng/ml Intercellular adhesion molecule-1, ng/ml Thrombomodulin, pg/ml High-molecular weight adiponectin, ng/ml Leptin, pg/ml Resistin, ng/ml
3.47 ( 20.92, 13.97) 0.70 58.4 ( 155.7, 272.4) 0.59 106.4 ( 385.4, 172.5) 0.45 2089.8 ( 3689.3, 490.3) 0.011 0.02 ( 1.46, 1.42) 0.98
2.09 ( 15.57, 19.75) 0.82 113.2 ( 83.5, 349.8) 0.23 237.1 ( 519.9, 45.8) 0.10 1433.3 ( 3055.1, 188.4) 0.08 0.72 ( 2.17, 0.72) 0.33
5.56 ( 23.41, 12.29) 0.54 74.8 ( 293.6, 144.0) 0.50 130.6 ( 155.8, 417.0) 0.37 656.5 ( 2298.2, 985.3) 0.43 0.71 ( 0.74, 2.15) 0.34
To convert C-reactive protein to nmol/l, multiply by 9.524. To convert interleukin-6 to IU/ml, multiply by 0.124. To convert tumor necrosis factor-a to IU/ml, multiply by 0.086. To our knowledge, there is no conversion to International Units currently available for the remaining novel biomarkers.
Net change in plasma levels of inammatory biomarkers along with CIs and P-values are provided for the three comparisons of interest in Table 4. Compared with milk protein, soy protein supplementation resulted in a signicant mean net change (95% CI) in plasma E-selectin of 3.93 ng/ml ( 7.05 to 0.81 ng/ml; P 0.014), even after correction for multiple comparisons. Compared with carbohydrate, soy protein supplementation resulted in a signicant mean net change (95% CI) in plasma leptin of 2089.8 pg/ml ( 3689.3 to 490.3 pg/ml; P 0.011), which attained statistical signicance even after adjusting for multiple comparisons. There were no statistically signicant net changes in plasma levels of CRP, IL-6, TNF-a, VCAM-1, ICAM-1, thrombomodulin, high-molecular weight (HMW) adiponectin, leptin or resistin. The magnitude and signicance of the mean levels and net change estimates were not different in the pre-specied sensitivity analyses which included using log-transformed values, when the analysis was restricted to participants who completed all phases and those who consumed at least 85% of their supplement packets. The frequency of side effects was similar for the soy protein, milk protein and carbohydrate supplementation interventions. The most commonly self-reported changes in symptoms were a change in appetite (29.6%), increased energy level (16.7%) and constipation (14.2%). Participants reported more belching during
& 2013 Macmillan Publishers Limited
the milk protein supplementation (18.0%) compared with soy protein (6.2%) and carbohydrate supplementation (6.2%; P 0.02). There was a slightly larger percentage of participants reporting improved mood during the soy protein supplementation (18.5%) compared with milk protein (7.7%) and carbohydrate supplementation (8.6%), although it was not statistically signicant (P 0.06). DISCUSSION This randomized controlled trial suggests that soy protein supplementation reduces plasma levels of E-selectin compared with milk protein and reduces plasma levels of leptin compared with carbohydrate. However, soy protein supplementation may not have a meaningful effect on plasma levels of CRP, IL-6, TNF-a, VCAM-1, ICAM-1, thrombomodulin, HMW adiponectin or resistin. These study ndings add to our understanding of the effects of soy protein, especially considering the paucity of rigorously designed and conducted soy protein clinical trials on novel CVD risk factors. The benecial effect of soy protein on traditional CVD risk factors, primarily lipids and blood pressure, has been demonstrated previously.9,10 The evidence for an association of dietary protein intake on novel CVD risk factors is less conclusive. Our ndings appear to be consistent with the majority of the few published soy protein clinical trials, demonstrating no statistically
European Journal of Clinical Nutrition (2013) 58 63
Soy protein and novel cardiovascular risk factors CM Rebholz et al
62 signicant change in the inammatory biomarkers, endothelial dysfunction biomarkers and adipocytokines.1116 The observed reduction in plasma levels of E-selectin after soy protein supplementation compared with milk protein supplementation in the present study was consistent with one other study.16 In a crossover study of 42 postmenopausal women with metabolic syndrome, an 8-week intervention on the soy nut diet (30 g/day soy protein and 102 mg/day isoavones) resulted in a 11.4% decrease (Po0.01) in E-selectin compared with 8 weeks on the control diet.16 In contrast, there was no effect of soy protein on E-selectin in three other studies.1315 The observed reduction in plasma leptin was documented in one other study of 90 overweight and obese men and women in which a 6-week intervention of two daily servings of a soy drink resulted in 18.2 ng/ml leptin reduction compared with 6.97 ng/ml in the control group (Po0.01).21 In contrast, six other soy protein clinical trials reported no signicant change in leptin levels.12,2226 To the best of our knowledge, the present study is one of the largest randomized trials to investigate the effect of protein supplementation on multiple biomarkers of inammation, endothelial dysfunction and adipocytokines, and is the second to report on thrombomodulin and resistin. Whereas the majority of previous studies have limited their participants to Caucasian females, our study population is more generalizable due to it representing men, women, Caucasians and African-Americans. It is well established that diet plays an important role in modifying CVD risk. Soy food products have several bioactive components and properties that could be responsible for improving cardiovascular health, including ber, polyunsaturated fatty acids and arginine.2729 Replacement of carbohydrate with dietary protein intake is thought to offer cardiovascular benet due to the lower glycemic index of protein and associated reduction of inammatory activity.30 A leading hypothesis for the postulated mechanism for an effect of soy protein on CVD risk factors is through the estrogen-like structure and biological activity of soy-derived isoavones.31,32 Isoavones, such as genistein, have been shown to improve endothelial function by increasing nitric oxide, causing smooth muscle relaxation, and subsequently resulting in vasodilation.3337 Genistein has also been shown to inhibit differentiation of fat cells, which secrete adipocytokines, through several pathways including expression of endothelial nitric oxide synthase, inhibition of p38 mitogenactivated kinase phosphorylation and inhibition of fatty acid synthase.3840 This randomized, double-blind, placebo-controlled trial had a high level of compliance, high rate of study completion, and limited variability in diet and lifestyle behaviors. The prolonged 3-week washout period limited the carryover effect, and there was no statistical evidence of carryover between periods. Blind duplicates of samples were measured for quality assurance, and the same laboratory technician and equipment was used throughout the study to minimize systematic error. Highsensitivity assay techniques were employed such that low levels of inammatory biomarkers could be detected. Random variability was decreased by using average values of duplicate measures in the analysis. The estimation of mean levels of biomarkers and mean net change in biomarkers was consistent in sensitivity analyses. Although our study has a relatively large sample size compared with previously published studies, this study still has insufcient statistical power to detect small changes in biomarkers due to the supplement interventions. However, the clinical signicance of small changes in these novel CVD risk factors is unknown. The contribution of participants was maximized with the crossover study design and mixed effects regression model. Another limitation is that the potential day-to-day variation in biomarker levels could have increased random error and variance estimates and therefore reduced statistical power. In our study, the 95% CI
European Journal of Clinical Nutrition (2013) 58 63
estimates of net changes in biomarkers were large, even for those that reached statistical signicance. Future studies should collect multiple blood samples on different days in order to assess and account for this potential source of variability. An additional limitation is the relatively short intervention duration of 2 months. However, the majority of soy protein clinical trials on novel CVD risk factors similarly have an intervention duration of 6 or 8 weeks.11,1316 In conclusion, this study suggests that soy protein may improve endothelial function by decreasing plasma levels of E-selectin compared with milk protein and may improve metabolic function by decreasing plasma levels of leptin compared with carbohydrate. This study suggests that soy protein may not signicantly impact plasma levels of CRP, IL-6, TNF-a, ICAM-1, VCAM-1, thrombomodulin, HMW adiponectin or resistin. A randomized controlled trial with a larger sample size, longer intervention duration and multiple measurements of biomarkers may be better suited to assess the impact of soy protein on novel CVD risk factors. A meta-analysis could be conducted to pool results from the few available clinical trials with small sample sizes in order to estimate the effect of soy protein on novel CVD risk factors with greater statistical power. This study provides moderate support for the role of soy protein as a healthy food for cardiovascular health through E-selectin and leptin reduction, which adds to the existing evidence for the cholesterol and blood pressure reducing effects of soy protein.
CONFLICT OF INTEREST
The authors declare no conict of interest.
ACKNOWLEDGEMENTS
This work was supported by a research grant (R01 HL68057) from the National Heart, Lung, and Blood Institute of National Institutes of Health, Bethesda, MD, USA, and the American Medical Association Foundation 2011 Seed Grant Research Program. The study supplements were provided by Solae, LLC. National Heart, Lung, and Blood Institute, American Medical Association Foundation, and Solae, LLC had no role in the design, data collection and analysis, decision to publish or preparation of the manuscript.
REFERENCES
1 Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367: 17471757. 2 Writing Group MembersRoger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation 2012; 125: e2e220. 3 Hwang SJ, Ballantyne CM, Sharrett AR, Smith LC, Davis CE, AM Gotto et al. Circulating adhesion molecules VCAM-1, ICAM-1, and E-selectin in carotid atherosclerosis and incident coronary heart disease cases: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 1997; 96: 42194225. 4 Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P et al. Low grade inammation and coronary heart disease: prospective study and updated metaanalyses. BMJ 2000; 321: 199204. 5 Lee SH, Ha JW, Kim JS, Choi EY, Park S, Kang SM et al. Plasma adiponectin and resistin levels as predictors of mortality in patients with acute myocardial infarction: data from infarction prognosis study registry. Coron Artery Dis 2009; 20: 3339. 6 Falk E. Pathogenesis of atherosclerosis. J Am Coll Cardiol 2006; 47: C7C12. 7 Tesauro M, Canale MP, Rodia G, Di Daniele N, Lauro D, Scuteri A et al. Metabolic syndrome, chronic kidney, and cardiovascular diseases: role of adipokines. Cardiol Res Pract 2011; 2011: 653182. 8 Erdman JW. AHA science advisory: Soy protein and cardiovascular disease: a statement for healthcare professionals from the Nutrition Committee of the AHA. Circulation 2000; 102: 25552559. 9 Reynolds K, Chin A, Lees KA, Nguyen A, Bujnowski D, He J. A meta-analysis of the effect of soy protein supplementation on serum lipids. Am J Cardiol 2006; 98: 633640.
& 2013 Macmillan Publishers Limited
Soy protein and novel cardiovascular risk factors CM Rebholz et al
63
10 Rebholz CM, Friedman EE, Powers LJ, Arroyave WD, He J, Kelly TN. Dietary protein intake and blood pressure: a meta-analysis of randomized controlled trials. Am J Epidemiol 2012; 176: S27S43. 11 Fanti P, Asmis R, Stephenson TJ, Sawaya BP, Franke AA. Positive effect of dietary soy in ESRD patients with systemic inammation--correlation between blood levels of the soy isoavones and the acute-phase reactants. Nephrol Dial Transplant 2006; 21: 22392246. 12 Charles C, Yuskavage J, Carlson O, John M, Tagalicud AS, Maggio M et al. Effects of high-dose isoavones on metabolic and inammatory markers in healthy postmenopausal women. Menopause 2009; 16: 395400. 13 Blum A, Lang N, Peleg A, Vigder F, Israeli P, Gumanovsky M et al. Effects of oral soy protein on markers of inammation in postmenopausal women with mild hypercholesterolemia. Am Heart J 2003; 145: e7. 14 Greany KA, Nettleton JA, Wangen KE, Thomas W, Kurzer MS. Consumption of isoavone-rich soy protein does not alter homocysteine or markers of inammation in postmenopausal women. Eur J Clin Nutr 2008; 62: 14191425. 15 Steinberg FM, Guthrie NL, Villablanca AC, Kumar K, Murray MJ. Soy protein with isoavones has favorable effects on endothelial function that are independent of lipid and antioxidant effects in healthy postmenopausal women. Am J Clin Nutr 2003; 78: 123130. 16 Azadbakht L, Kimiagar M, Mehrabi Y, Esmaillzadeh A, Hu FB, Willett WC. Soy consumption, markers of inammation, and endothelial function: a cross-over study in postmenopausal women with the metabolic syndrome. Diabetes Care 2007; 30: 967973. 17 Roberts WL, Moulton L, Law TC, Farrow G, Cooper-Anderson M, Savory J et al. Evaluation of nine automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications. Part 2. Clin Chem 2001; 47: 418425. 18 Huang Y, Cao S, Nagamani M, Anderson KE, Grady JJ, Lu LJ. Decreased circulating levels of tumor necrosis factor-alpha in postmenopausal women during consumption of soy-containing isoavones. J Clin Endocrinol Metab 2005; 90: 39563962. 19 Papadopoulos DP, Perrea D, Thomopoulos C, Sanidas E, Daskalaki M, Papazachou U et al. Masked hypertension and atherogenesis: the impact on adiponectin and resistin plasma levels. J Clin Hypertens 2009; 11: 6165. 20 Campbell CG, Brown BD, Dufner D, Thorland WG. Effects of soy or milk protein during a high-fat feeding challenge on oxidative stress, inammation, and lipids in healthy men. Lipids 2006; 41: 257265. 21 Konig D, Deibert P, Frey I, Landmann U, Berg A. Effect of meal replacement on metabolic risk factors in overweight and obese subjects. Ann Nutr Metab 2008; 52: 7478. 22 Christie DR, Grant J, Darnell BE, Chapman VR, Gastaldelli A, Sites CK. Metabolic effects of soy supplementation in postmenopausal Caucasian and African American women: a randomized, placebo-controlled trial. Am J Obstet Gynecol 2010; 203: 153.e1153.e9. 23 Maskarinec G, Steude JS, Franke AA, Cooney RV. Inammatory markers in a 2-year soy intervention among premenopausal women. J Inamm 2009; 6: 9. 24 Phipps WR, Wangen KE, Duncan AM, Merz-Demlow BE, Xu X, Kurzer MS. Lack of effect of isoavonic phytoestrogen intake on leptin concentrations in premenopausal and postmenopausal women. Fertil Steril 2001; 75: 10591064. 25 Takahira M, Noda K, Fukushima M, Zhang B, Mitsutake R, Uehara Y et al. Randomized, double-blind, controlled, comparative trial of formula food containing soy protein vs. milk protein in visceral fat obesity. -FLAVO study-. Circ J 2011; 75: 22352243. 26 Wu AH, Stanczyk FZ, Martinez C, Tseng CC, Hendrich S, Murphy P et al. A controlled 2-mo dietary fat reduction and soy food supplementation study in postmenopausal women. Am J Clin Nutr 2005; 81: 11331141. 27 King DE. Dietary ber, inammation, and cardiovascular disease. Mol Nutr Food Res 2005; 49: 594600. 28 Finot PA. Proteins and cardiovascular problems. Bibl Nutr Dieta 1992; 49: 8392. 29 Esposito K, Giugliano D. Diet and inammation: a link to metabolic and cardiovascular diseases. Eur Heart J 2006; 27: 1520. 30 Qi L, Hu FB. Dietary glycemic load, whole grains, and systemic inammation in diabetes: the epidemiological evidence. Curr Opin Lipidol 2007; 18: 38. 31 Pike AC, Brzozowski AM, Hubbard RE, Bonn T, Thorsell AG, Engstrom O et al. Structure of the ligand-binding domain of oestrogen receptor beta in the presence of a partial agonist and a full antagonist. EMBO J 1999; 18: 46084618. 32 Shimizu H, Shimomura Y, Nakanishi Y, Futawatari T, Ohtani K, Sato N et al. Estrogen increases in vivo leptin production in rats and human subjects J Endocrinol 1997; 154: 285292. 33 Catania MA, Crupi A, Firenzuoli F, Parisi A, Sturiale A, Squadrito F et al. Oral administration of a soy extract improves endothelial dysfunction in ovariectomized rats. Planta Med 2002; 68: 11421144. 34 Jiang F, Jones GT, Husband AJ, Dusting GJ. Cardiovascular protective effects of synthetic isoavone derivatives in apolipoprotein e-decient mice. J Vasc Res 2003; 40: 276284. 35 Squadrito F, Altavilla D, Crisafulli A, Saitta A, Cucinotta D, Morabito N et al. Effect of genistein on endothelial function in postmenopausal women: a randomized, double-blind, controlled study. Am J Med 2003; 114: 470476. 36 Walker HA, Dean TS, Sanders TA, Jackson G, Ritter JM, Chowienczyk PJ. The phytoestrogen genistein produces acute nitric oxide-dependent dilation of human forearm vasculature with similar potency to 17beta-estradiol. Circulation 2001; 103: 258262. 37 Beavers DP, Beavers KM, Miller M, Stamey J, Messina MJ. Exposure to isoavonecontaining soy products and endothelial function: a Bayesian meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis 2012; 22: 182191. 38 Harmon AW, Harp JB. Differential effects of avonoids on 3T3-L1 adipogenesis and lipolysis. Am J Physiol Cell Physiol 2001; 280: C807C813. 39 Park HJ, Della-Fera MA, Hausman DB, Rayalam S, Ambati S, Baile CA. Genistein inhibits differentiation of primary human adipocytes. J Nutr Biochem 2009; 20: 140148. 40 Zhang M, Ikeda K, Xu JW, Yamori Y, Gao XM, Zhang BL. Genistein suppresses adipogenesis of 3T3-L1 cells via multiple signal pathways. Phytother Res 2009; 23: 713718.
& 2013 Macmillan Publishers Limited
European Journal of Clinical Nutrition (2013) 58 63
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Marc Lobliner - Fat Loss Factor BookDokument77 SeitenMarc Lobliner - Fat Loss Factor Bookcleudimartins100% (2)
- AP Economy in BriefDokument77 SeitenAP Economy in Briefdarimadugu100% (1)
- A Nutty Way To Measure CaloriesDokument2 SeitenA Nutty Way To Measure CaloriesDavid PhamNoch keine Bewertungen
- Copper Kettle Catering 2Dokument4 SeitenCopper Kettle Catering 2t4thilini100% (2)
- Ultimate Guide To Marathon Running 2nd Edition PDFDokument164 SeitenUltimate Guide To Marathon Running 2nd Edition PDFJordi LopezNoch keine Bewertungen
- Aspartame 2012 Final PDFDokument10 SeitenAspartame 2012 Final PDFdocneiraNoch keine Bewertungen
- Thimerosal y ASDDokument12 SeitenThimerosal y ASDdocneiraNoch keine Bewertungen
- Asian Pac. J. Allergy Immunol. 2013 Amarasekera PDFDokument10 SeitenAsian Pac. J. Allergy Immunol. 2013 Amarasekera PDFdocneiraNoch keine Bewertungen
- Respiracion y Control Metabolico y Oxidativo PDFDokument3 SeitenRespiracion y Control Metabolico y Oxidativo PDFdocneiraNoch keine Bewertungen
- Aspartamo y Obesidad PDFDokument7 SeitenAspartamo y Obesidad PDFdocneiraNoch keine Bewertungen
- Carne Roja y MortalidadDokument9 SeitenCarne Roja y MortalidaddocneiraNoch keine Bewertungen
- Chinese Herbal Mixture y Cancer PDFDokument7 SeitenChinese Herbal Mixture y Cancer PDFdocneiraNoch keine Bewertungen
- Ajo y Neumonía Por Bacteria Multiresistente PDFDokument2 SeitenAjo y Neumonía Por Bacteria Multiresistente PDFdocneiraNoch keine Bewertungen
- Ajo y Efecto Antibiótico PDFDokument6 SeitenAjo y Efecto Antibiótico PDFdocneiraNoch keine Bewertungen
- Cerebro y Meditacion PDFDokument18 SeitenCerebro y Meditacion PDFdocneiraNoch keine Bewertungen
- Meditacion y RM Cerebral PDFDokument7 SeitenMeditacion y RM Cerebral PDFdocneiraNoch keine Bewertungen
- Isoflavonas y Cancer de Prostata PDFDokument4 SeitenIsoflavonas y Cancer de Prostata PDFdocneiraNoch keine Bewertungen
- Meditacion y Autismo PDFDokument11 SeitenMeditacion y Autismo PDFdocneiraNoch keine Bewertungen
- Autismo y Vacunacion PDFDokument15 SeitenAutismo y Vacunacion PDFdocneiraNoch keine Bewertungen
- Cancer Otto Warburg 00Dokument7 SeitenCancer Otto Warburg 00Harish BorraNoch keine Bewertungen
- Vacuna Hepatitis B y Autismo PDFDokument14 SeitenVacuna Hepatitis B y Autismo PDFdocneiraNoch keine Bewertungen
- The Toxic Truth About SugarDokument3 SeitenThe Toxic Truth About SugarfatoldfartNoch keine Bewertungen
- SBS Instalment Plans at 0% Markup : Alfalah Credit CardsDokument2 SeitenSBS Instalment Plans at 0% Markup : Alfalah Credit CardsSyeda SeeratNoch keine Bewertungen
- English 4 Q4 Week 1Dokument82 SeitenEnglish 4 Q4 Week 1Pia PrenroseNoch keine Bewertungen
- 历年托福词汇题汇总440题Dokument54 Seiten历年托福词汇题汇总440题harry yangNoch keine Bewertungen
- IELTS Practice TestDokument4 SeitenIELTS Practice TestDániel KreiszNoch keine Bewertungen
- Eyesight Self Correction Instructions 2Dokument19 SeitenEyesight Self Correction Instructions 2Brad YantzerNoch keine Bewertungen
- Dietary Intake, Nutrient Status, and Growth Parameters in Children With Autism SpectrumDokument8 SeitenDietary Intake, Nutrient Status, and Growth Parameters in Children With Autism Spectrumguilherme augusto paroNoch keine Bewertungen
- Rewrite The Following Sentences Into Active VoiceDokument2 SeitenRewrite The Following Sentences Into Active VoiceTamara GonzalezNoch keine Bewertungen
- Lincoln County School District # 2 Elementary Lunch Menu January-11Dokument1 SeiteLincoln County School District # 2 Elementary Lunch Menu January-11anon-579447Noch keine Bewertungen
- Jack-Large Mouth BassDokument2 SeitenJack-Large Mouth Basslbrinson1Noch keine Bewertungen
- Fun Butterfly SnacksDokument5 SeitenFun Butterfly Snacksapi-637009748Noch keine Bewertungen
- Final Exam in PE and Health 10Dokument1 SeiteFinal Exam in PE and Health 10Mary Grace Palis-MaulionNoch keine Bewertungen
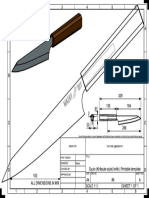
- 06 Gyuto Knife DRWDokument1 Seite06 Gyuto Knife DRWPeter IlievNoch keine Bewertungen
- Birthday Celeb Madam MarlynDokument3 SeitenBirthday Celeb Madam MarlynEric PascuaNoch keine Bewertungen
- In Partial FulfillmentDokument17 SeitenIn Partial FulfillmentHarvey Jansen JrNoch keine Bewertungen
- Level Test EnglishDokument6 SeitenLevel Test EnglishCelia Romero MateoNoch keine Bewertungen
- Gastronomic Tourism, A New Trend For Contemporary Tourism??: Georgică Gheorghe, Petronela Tudorache, Puiu NistoreanuDokument10 SeitenGastronomic Tourism, A New Trend For Contemporary Tourism??: Georgică Gheorghe, Petronela Tudorache, Puiu NistoreanuMuhammad RojaliNoch keine Bewertungen
- IFRJ 2017, Sri Winarti, Colonic MicrobiotaDokument8 SeitenIFRJ 2017, Sri Winarti, Colonic MicrobiotaSri WinartiNoch keine Bewertungen
- Pengaruh Sp-36 Dan Asam Humat Terhadap Pertumbuhan Dan Produksi Tanaman Kedelai (Glycine Max L)Dokument6 SeitenPengaruh Sp-36 Dan Asam Humat Terhadap Pertumbuhan Dan Produksi Tanaman Kedelai (Glycine Max L)Alif FazariNoch keine Bewertungen
- Differences Between Trends and FadsDokument19 SeitenDifferences Between Trends and FadsRhea Carillo100% (3)
- Natural Glow BookDokument112 SeitenNatural Glow Bookalejandra9roper9cond100% (1)
- Let's Be HealthyDokument4 SeitenLet's Be HealthygizlealvesNoch keine Bewertungen
- A Restaurant Review and RubricDokument2 SeitenA Restaurant Review and Rubricandres aponteNoch keine Bewertungen
- Flexible Dieting 1Dokument11 SeitenFlexible Dieting 1SamirNoch keine Bewertungen
- NG T Đi V I Gi I T - Phrasal VerbsDokument13 SeitenNG T Đi V I Gi I T - Phrasal VerbsĐỗ Thị Hồng NguyênNoch keine Bewertungen
- The Triumph of Surgery Notes Class 10 NCERT EnglishDokument4 SeitenThe Triumph of Surgery Notes Class 10 NCERT EnglishRudar SharmaNoch keine Bewertungen
- Semester I Lesson 1 FamilyDokument60 SeitenSemester I Lesson 1 FamilyPuspita Purnama SariNoch keine Bewertungen