Beruflich Dokumente
Kultur Dokumente
BioLec - Circulatory
Hochgeladen von
JKCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
BioLec - Circulatory
Hochgeladen von
JKCopyright:
Verfügbare Formate
THE CIRCULATORY SYSTEM I.
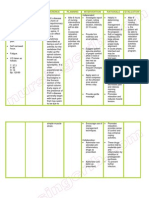
Functions - absorbs + transports nutrients (digestive system --> body cells) - delivers wastes (excretory --> outside) - gas transport (w/ respiratory system) - hormones transport from glands to target organs (endocrine system) - heat distribution (thermoregulation) - blood components as defense vs microorganisms (immune) - buffers in blood to maintain blood pH (7.35 - 7.45) CarbonateBicarbonate System Oxygen through lungs --> carried by blood --> CO2 exchange with O2 --> Nutrients from digestive system to liver (removal) --> Tissues load wastes for transport to kidneys --> Reabsorption --> Hormones + Heat Exchange II. Types of Circulation 1. Continuous w/ External environment - unicellular protozoans, sponges, cnidarians, flatworms - ciliary movements + pulsations + contraction of body wall = stirring of body fluid in coelom (no need for definite circ system) - nutrients & gases obtained easily because of size - Osculum/Ostium, Mouth/Anus, Pharynx 2. Discontinuous w/ External environment - need for specialized circ (due to size, activity, complexity) III. Types of Circulatory System 1. Open - nematodes (ascaris), arthropods (insect, spider, crab - dorsal heart, blood + body cavity fluid are one), mollusks (snail, oysters, clams) - relatively slow-moving except for arthropods (equipped w/ tracheal system -- direct pipeline) - Advantage: more even distribution of matls since cells swim in fluid - Disadvantage: slower circulation, low rates of O2 transport required by active animals 2. Closed - annelids (earthworm - blood separate from coelomic fluid), mollusk (SQUID only), vertebrates (fish, mammals) - blood enclosed in system of vessels, no contact w/ cells or interstitial fluid - movement of materials between blood & IF through thin capillaries designed for exchange (internal respiration)
- not necessarily more advanced - Advantages: faster circ, regulation of blood flow - Disadvantage: less even distribution IV. Blood - 4-5x thicker than water - temperature of 38 degrees - ph 7.35 - 7.45, isotonic at 0.85% NaCl - 5L in 60kg man (8% body weight, cardiac output of 5L/min) - Functions: A) Regulatory - Blood solutes affect water potential gradient (determined by plasma concentration of Na+ and plasma proteins) --> regulates water movement between blood and tissue - Water content of blood - regulation of body temp (heat transfer between thermogenic centers like liver, skeletal muscle and brown fat to heat sinks like skin, brain and kidney) - pH maintenance - blood buffer (hydrogencarbonate, phosphate equilibria; secondary role of hemoglobin) B) Protective - platelets, plasma proteins (fibrinogen), plasma factors (Ca2+) clotting vs blood loss and pathogen entry - Leucocytes - against toxins and potential pathogens (nonspecific phagocytosis + specific antibody production) C) TRANSPORT - Soluble products of digestion/absorption (glucose, amino acids, vit, min) from gut --> liver --> general circ ; fatty acids from gut to lymph to gen circ - Waste products (urea, creatinine, lactate) from prod site to liver/kidney - Hormones(insulin, a peptide, testosterone, steroid, adrenaline, catecholamine) from prod site to target organ - Respi gases from uptake to util (O2 - RBC, CO2 - plasma) - Plasma proteins from liver (fibrinogen - blood clotting; globulin specific transport of thyroxine, iron copper; albumin - bind plasma Ca2+) V. Blood Cells - Centrifugation: 2 layers (Serum - plasma of no more fibrinogen) - 55% plasma, 45% Cells - Blood cells originate from stem cells in bone marrow by haemopoiesis
VI. Blood Composition A) Plasma - 55% - water (91-92%) - plasma proteins (albumin with high osmotic pressure and for delivery, serum globulin, fibrinogen) - regulatory + protective proteins (hormone, antibodies, enzymes) - organic (wastes + nutrients) - inorganic (Na, Cl, K,Ca, Mg, HCO3, Fe) - gas (O2, CO2, N2) B) Formed Elements - 45% 1. Erythrocytes / RBC - most numerous, 5 million per cubic mm of adult blood - CO2-O2 transfer, blood buffer - biconcave disc, no nucleus - red due to hemoglobin (adv in cells: keeps viscosity low, allows best arrangement of enzymes and solutes for hemoglobin function, prevents dramatic reduction in blood water potential) - typical lifespan: 127 days, destroyed in spleen - RBC (male = 5.4 +- 0.8M/cc; female = 4.8+-0.8M/cc) - Rouleux formation - Erythropoiesis: RBC formation 2M RBCs/sec (in hematopoietic organs like yolk sac, liver, myeloid tissue)
2. Platelets / Thrombocytes - fragments of cells, blood clots (disintegrate to release thromboblast), enucleated, derived from megakaryocytes, 10 day life span, 150,000-400,000 cc/blood, clotting 3. Leukocytes - no hemoglobin - with nuclei - 5000 - 9000 cells/cc; 9-12 days life span - agranulocyte (mono, lympho) - granulocyte (neutro, eosino, baso) A) Neutrophils - most abundant leukocyte (WBC) - short lived (12-72h) - non-staining granules, very active phagocytosis of microorganisms
- migrate from blood to tissues B) Monocytes - largest leucocyte - agranulocyte (no granules in cytoplasm) - large, bean shaped nucleus; 2-3 days in circ system before maturation into phagocytic macrophages in tissues C) Lymphocytes - 30% of circulating leukocytes - prod in bone marrow, develop in lymph node, thymus gland and spleen - specific immune response - B: produce anti-bodies - T: coordination of immune response, cell destruction - deeply staining nucleus, thin halo of clear cytoplasm D) Basophil - S-shaped nucleus, blue stain granules - large amounts of histamine (inflammation) + heparin (clot - not blood clot) E) Eosinophil - double lobe nucleus, red stain granules (w/ acid dye eosin) - controls allergic response (secrete enzymes to inactivate histamine) - increase during allergic reactions + parasitic infection (tape/hookworm) VII. Erythropoiesis in Bone Marrow - gradual appearance of hemoglobin, disappearance of RNA - progressive deterioration of nucleus, eventual extrusion - gradual loss of organelles (eg mitochondria) - reduction in cell size 1. Hemacytoblast (stem cell) 2. Rubricyte - synthesis of hemoglobin starts here 3. Metarubricyte - max hemoglobin, removal of nucleus and organelles 4. Erythrocyte - mature RBC 5. RBC goes to spleen, phagocytosis by macrophages 6. breakdown into Fe group (liver - storage; bone marrow - make new hemoglobin) 7. and heme group (Bilirubin - makes poop brown) Stimulus for Homeostatic Mechanism A) Hypoxia
- oxygen def in high altitude - Kidney Cells release Renal Erythropoietic Factor/Erythrogenin into blood --> activates plasma globulin inactive erythropoietinogen to erythropoietin --> erythropoietin hormone goes to bone marrow to initiate destruction B) Anemia - Nutritional (lack of Fe) - pernicious (intrinsic factor for B12 absorption packing - defect in stomach parietal cells) VIII. ABO Blood Grouping - antigen/agglutinogen presence on surface - whole blood transfusions - severe anemia or thrombocytopenia, blood loss (15-30%) - blood donor + anticoagulant + 4C (citrate and oxalate salts) - RBC - highly specific glycoprotein antigen --> AGGLUTINOGEN - preformed antibodies - agglutinins (act against RBC with antigens not on own person's RBC) Blood Group O (univ donor) A B AB (univ recipient) glycoprotein RBC Agglutinogen (molecule-like) None A B AB Plasma Agglutin (antibody/receptor) anti-A/anti-B anti-B anti-A none Blood Allowed O A, O B, O A, B, AB, O
Side Effects of Wrong Transfusions: Agglutination + Hemolysis - oxygen-carrying capacity of RBC disrupted - clumping in small vessels hinders blood flow - fever, chills, nausea, vomiting - hemoglobin > kidney blocks > renal breakdown - one time is okay - donor's blood too diluted in recipient blood, periodic transfusion may be fatal - WITTEBSKY: drug used in periodic transfusion as an immunosuppresant IX. Rh Blood Group
Das könnte Ihnen auch gefallen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Control of Pandemic Infectious Disease Procedure - Landkap - Gitt 00Dokument25 SeitenControl of Pandemic Infectious Disease Procedure - Landkap - Gitt 00ahar85Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Deeper Trial - Asco 2021Dokument26 SeitenDeeper Trial - Asco 2021Vuong Dinh Thy HaoNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Zybio Company Profile 20211109CDokument46 SeitenZybio Company Profile 20211109CĐức Hòa100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- OME Video DurationsDokument7 SeitenOME Video DurationsLucas RiosNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Dermoscopy ReviewDokument28 SeitenDermoscopy ReviewMarwa RagabNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Stress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.Dokument94 SeitenStress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.sorbariNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Wadsworth Publishing Critical Reasoning 6thDokument468 SeitenWadsworth Publishing Critical Reasoning 6thprabindra100% (1)
- Diagnostic TestDokument4 SeitenDiagnostic TestrizabesmonteNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Ozone Unsung Hero by Navy Captain - Ajit VadakayilDokument153 SeitenOzone Unsung Hero by Navy Captain - Ajit Vadakayilsudhir shahNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Day Cream: Material Safety Data SheetDokument2 SeitenDay Cream: Material Safety Data SheetRachmawati AfridaNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Contact Lens Complications and ManagementDokument10 SeitenContact Lens Complications and Managementstrawberry8832850% (2)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Meiosis GizmosDokument9 SeitenMeiosis GizmosShaylee TorresNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Subcutaneous Mycoses: Presenter: DR Pranay Reddy Moderator: DR Tonita MNDokument81 SeitenSubcutaneous Mycoses: Presenter: DR Pranay Reddy Moderator: DR Tonita MNSandipNoch keine Bewertungen
- Assis 2017Dokument19 SeitenAssis 2017widyadariNoch keine Bewertungen
- Knee Dry NeedlingDokument24 SeitenKnee Dry NeedlingJavi EgeaNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Bioassay For AntidiabetesDokument39 SeitenBioassay For AntidiabetesNita TriadistiNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Gold Awards: Organization Name Title of InnovationDokument10 SeitenGold Awards: Organization Name Title of Innovationchek86351Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- From Outrage To Courage: The Unjust and Unhealthy Situation of Women in Poorer Countries and What They Are Doing About It PDFDokument97 SeitenFrom Outrage To Courage: The Unjust and Unhealthy Situation of Women in Poorer Countries and What They Are Doing About It PDFNadine Avila100% (2)
- K2 - Strongyloides StercoralisDokument16 SeitenK2 - Strongyloides StercoraliswirputNoch keine Bewertungen
- Kakawate Dog Soap ThesisDokument55 SeitenKakawate Dog Soap ThesisArturo Roman100% (4)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Neurology & Pupils (No 467)Dokument231 SeitenNeurology & Pupils (No 467)Mohamed GaberNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- Seatone InfoDokument7 SeitenSeatone InfoJugal ShahNoch keine Bewertungen
- IMNCIDokument13 SeitenIMNCIJayalakshmiullasNoch keine Bewertungen
- CHON Lecture PDFDokument25 SeitenCHON Lecture PDF2d HoehoeNoch keine Bewertungen
- Nursing Care Plan Pott's DiseaseDokument2 SeitenNursing Care Plan Pott's Diseasederic95% (21)
- Latin Root Words ListDokument4 SeitenLatin Root Words ListrbalakrNoch keine Bewertungen
- HWC (SC) Nqas ChecklistDokument79 SeitenHWC (SC) Nqas Checklistqa100% (1)
- Mental Disorder Due To AlcoholDokument18 SeitenMental Disorder Due To AlcoholAnonymous Oj5JCpO5xNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Endodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentDokument28 SeitenEndodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentardeleanoanaNoch keine Bewertungen
- FWD Medical Rider enDokument12 SeitenFWD Medical Rider enKhairul HMSBNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)