Beruflich Dokumente
Kultur Dokumente
CMS Five Considerations Health Homes
Hochgeladen von
iggybauOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CMS Five Considerations Health Homes
Hochgeladen von
iggybauCopyright:
Verfügbare Formate
TECHNICAL ASSISTANCE TOOL
OCTOBER 2011
Five Key Considerations for Exploring the Medicaid Health Homes Opportunity
Medicaid programs are considering the option of M any submitting a state plan amendment (SPA) for health homes. Health home services comprehensive care management, care coordination, health promotion, care transitions, patient and family engagement, and social and community linkages can serve as the glue between effective delivery of clinical services and linked by health information technology, if feasible. As a state starts to explore this opportunity, following are five key considerations that can help a state identify whether it wants to invest in health homes.
Medicaid programs that are considering emerging health homes opportunities are faced with a variety of decisions in how to design new programs within the existing infrastructure of the states publicly financed care delivery system. This technical assistance tool outlines key considerations to help states determine
1. Educate partners about what health homes are whether to invest in health homes and and are not. The state should begin the process of how to get started in doing so. educating its internal and external partners about the health homes opportunity. The Medicaid agency should reach out to its sister agencies behavioral health, longterm care, etc. about the opportunity and what it could mean i.e., greater integration across primary, acute, behavioral, and long-term care which, in turn, would aim to reduce costly and otherwise avoidable services. The state should also inform its provider community about the opportunity being explored and what it could mean for those providers, i.e., a mechanism to provide the glue services to high cost, high needs Medicaid beneficiaries, and to raise the bar by integrating care more effectively and eliminating existing provider silos. Providers can offer valuable insights for planning, specifically the size of the gap between current care management activities and what would be demanded by health homes. 2. Identify potential building blocks for health home services. A state should consider what existing building blocks or infrastructure are already in place that health home services could be layered on or added to. Building blocks might include existing investments in care management capacity, either through a patient-centered medical home initiative, physical-behavioral health integration initiatives, chronic care management programs, or other vehicles. A state can also leverage existing infrastructure, such as health information technology or an existing provider learning collaborative or quality improvement program. Special consideration should be given to risk-based managed care plans that may currently provide some care management or care coordination services and what role they will play, if any, in the support for or delivery/administration of health home services.
This technical assistance resource was developed for the Centers for Medicare & Medicaid Services by the Center for Health Care Strategies and Mathematica Policy Research. For more information or technical assistance in developing health homes, visit http://www.Medicaid.gov.
3. Mine data to understand more about the eligible population. The state would also want to use claims data to identify the eligible beneficiary population as defined by Section 2703. Questions to answer include: How many beneficiaries would be eligible? Where are they currently receiving care? Do eligible beneficiaries cluster in a certain geographic area, around certain providers, or among specific chronic conditions? Among which population subsets do opportunities for reductions in avoidable emergency department and hospital utilization exist? Answering these questions can help the state strategically decide which eligible beneficiaries to enroll, what providers will be targeted, whether the program would be regional or statewide and how it might be phased in. 4. Consider requesting Medicaid funds for health home planning. States have the option to request a planning grant at their medical assistance service match rate to support health home program design. For some states, this match rate is higher than they would receive through administrative match, and therefore worthwhile to pursue. 5. Recognize the time-limited aspect of the enhanced federal-state reimbursement rate. On the effective date of the SPA, the state begins to receive an enhanced 90-10 federal-state match for health home services for eight consecutive quarters. However, after the eight quarters, the states regular medical match rate kicks back in. As states consider the design features and scale of their health home programs, they should keep in mind that the states contribution will increase down the road. Therefore, to ensure sustainability, states should consider which subpopulations may be most likely to benefit from health homes services, and what the potential payback of health homes investments might be in terms of reductions in acute care expenditures over time.
TECHNICAL ASSISTANCE TOOL: Five Key Considerations for Exploring the Medicaid Health Home Opportunity
Das könnte Ihnen auch gefallen
- AAFP Letter To Domestic Policy Council 6-10-2020Dokument3 SeitenAAFP Letter To Domestic Policy Council 6-10-2020iggybauNoch keine Bewertungen
- Boston Mayor Executive Order 6-12-2020Dokument3 SeitenBoston Mayor Executive Order 6-12-2020iggybauNoch keine Bewertungen
- Bostock v. Clayton County, Georgia DecisionDokument119 SeitenBostock v. Clayton County, Georgia DecisionNational Content DeskNoch keine Bewertungen
- S 3609 Coronavirus Immigrant Families Protection ActDokument17 SeitenS 3609 Coronavirus Immigrant Families Protection ActiggybauNoch keine Bewertungen
- HR 6437 Coronavirus Immigrant Families Protection AcfDokument16 SeitenHR 6437 Coronavirus Immigrant Families Protection AcfiggybauNoch keine Bewertungen
- S 3721 COVID-19 Racial and Ethnic Disparities Task ForceDokument11 SeitenS 3721 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNoch keine Bewertungen
- A Bill: in The House of RepresentativesDokument2 SeitenA Bill: in The House of RepresentativesiggybauNoch keine Bewertungen
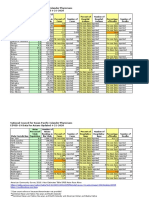
- Covid-19 Data For Asians Updated 4-21-2020Dokument2 SeitenCovid-19 Data For Asians Updated 4-21-2020iggybauNoch keine Bewertungen
- HR 6763 COVID-19 Racial and Ethnic Disparities Task ForceDokument11 SeitenHR 6763 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNoch keine Bewertungen
- HR 6585 Equitable Data Collection COVID-19Dokument18 SeitenHR 6585 Equitable Data Collection COVID-19iggybauNoch keine Bewertungen
- NCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020Dokument23 SeitenNCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020iggybauNoch keine Bewertungen
- SF StayHome MultiLang Poster 8.5x11 032620Dokument1 SeiteSF StayHome MultiLang Poster 8.5x11 032620iggybauNoch keine Bewertungen
- Doe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationDokument9 SeitenDoe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationiggybauNoch keine Bewertungen
- Doe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceDokument48 SeitenDoe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceiggybauNoch keine Bewertungen
- CDC Covid-19 Report FormDokument2 SeitenCDC Covid-19 Report FormiggybauNoch keine Bewertungen
- Exposing Corporate Profiteering From Immigration Detention and Enforcement September 2018Dokument16 SeitenExposing Corporate Profiteering From Immigration Detention and Enforcement September 2018iggybauNoch keine Bewertungen
- MACRA Quality Payment Program Year 2 Final RuleDokument662 SeitenMACRA Quality Payment Program Year 2 Final RuleiggybauNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Senator Robert Menendez - Public Letter of AdmonitionDokument4 SeitenSenator Robert Menendez - Public Letter of AdmonitionLegal InsurrectionNoch keine Bewertungen
- Private Duty NurseDokument2 SeitenPrivate Duty Nurserjavillar100% (1)
- Catalogo Libros Transfusion PDFDokument44 SeitenCatalogo Libros Transfusion PDFmeds1313Noch keine Bewertungen
- Dental EssayDokument3 SeitenDental Essayvaleriana calaniNoch keine Bewertungen
- MalpracticeDokument5 SeitenMalpracticeAntónio Ayrton WidiastaraNoch keine Bewertungen
- NURS FPX 6218 Assessment 4 Advocating For Lasting ChangeDokument7 SeitenNURS FPX 6218 Assessment 4 Advocating For Lasting ChangeEmma WatsonNoch keine Bewertungen
- Medicare Drug Plans in OhioDokument2 SeitenMedicare Drug Plans in OhioBetty Lin-FisherNoch keine Bewertungen
- Diya FoundationDokument5 SeitenDiya FoundationnehaNoch keine Bewertungen
- Scientific Programme (Tentative)Dokument2 SeitenScientific Programme (Tentative)DivyaDeepthi18Noch keine Bewertungen
- Med, Supp, Adv Script Live TransferDokument2 SeitenMed, Supp, Adv Script Live Transfereraj khan100% (1)
- Chapter 7 SinghDokument42 SeitenChapter 7 Singhmaa468Noch keine Bewertungen
- Osei Cassandra CVDokument2 SeitenOsei Cassandra CVCassieOseiNoch keine Bewertungen
- CC Terms and ConditionsDokument1 SeiteCC Terms and ConditionsZohra El GasmiNoch keine Bewertungen
- Nursing Home ChargesDokument67 SeitenNursing Home Chargesalmond2009Noch keine Bewertungen
- 2012 Alumni Times (Pgs. 5-8)Dokument5 Seiten2012 Alumni Times (Pgs. 5-8)monroecountybeaconNoch keine Bewertungen
- Family Support Interventions For Families of Adults With Intellectual and Developmental DisabilitiesDokument34 SeitenFamily Support Interventions For Families of Adults With Intellectual and Developmental DisabilitiesIntan HumaerohNoch keine Bewertungen
- Icd 10 Mental HealthDokument5 SeitenIcd 10 Mental Health733100% (2)
- Isaac Rodriguez Chronological Resume - Final MasterDokument2 SeitenIsaac Rodriguez Chronological Resume - Final Masterapi-366594193Noch keine Bewertungen
- Specialized Family Planning ClinicsDokument22 SeitenSpecialized Family Planning ClinicsKonstantinos KokorasNoch keine Bewertungen
- May 2019 Issue of Active LivingDokument20 SeitenMay 2019 Issue of Active Livingmgruender1100% (2)
- 01-31-2023 Medicare Advantage LetterDokument8 Seiten01-31-2023 Medicare Advantage LetterNBC MontanaNoch keine Bewertungen
- Pharmacoepidemiology Pharmacoepidemiology At3: Studies Using Automated Databases GDokument27 SeitenPharmacoepidemiology Pharmacoepidemiology At3: Studies Using Automated Databases GRuth Vargas GonzalesNoch keine Bewertungen
- Request of Document Issue and PledgeDokument2 SeitenRequest of Document Issue and PledgeCarlos Marove0% (1)
- Hospitals ReportDokument488 SeitenHospitals Reportrabiaw20Noch keine Bewertungen
- The Real Facts:: An Overview of Maine's Temporary Assistance For Needy Families ProgramDokument40 SeitenThe Real Facts:: An Overview of Maine's Temporary Assistance For Needy Families ProgramYuva Mahaneesh ChandraNoch keine Bewertungen
- 2016 Psych Directory Lawrence KansasDokument4 Seiten2016 Psych Directory Lawrence Kansasapi-284497736Noch keine Bewertungen
- Dental Insurance of IndiaDokument20 SeitenDental Insurance of IndiaMyuresh AgarwalNoch keine Bewertungen
- NDC FaqsDokument6 SeitenNDC FaqsSara E Alcantara RNoch keine Bewertungen
- Texas V United States ComplaintDokument33 SeitenTexas V United States ComplaintLaw&CrimeNoch keine Bewertungen